Abstract
Hazards in the urban built environment can create barriers to mobility among older adults aging in place. We investigated the relationship between urban built environment characteristics and 15-month trajectories of mobility disability in a sample of 1,188 older adults living in Detroit, MI, a city that has undergone rapid economic and structural decline. Data come from the Michigan Minimum Data Set for Home Care (2001–2008), an enumerative database of older adults in Michigan who qualify for federal or state-funded home and community-based long-term care through a Medicaid waiver program. Standardized assessments are made at intake and every 90 days by case managers. Built environments were assessed with a virtual audit using the “Street View” feature of Google Earth. A summary accessibility score was created for each block based on a count of the number of accessible features (e.g., continuous barrier-free sidewalks and proximity of public transportation). Using growth mixture models, two latent trajectories of outdoor mobility were identified: one capturing occasional outdoor mobility (representing 83 % of the sample) and one capturing almost no mobility outside the home. Controlling for sociodemographic and health risk factors, individuals living in more accessible environments had a 18 % higher odds of being in the more mobile group (OR = 1.18, 95 % CI = 1.01, 1.41). These findings emphasize the importance of the built environment for mobility among urban-dwelling older adults.
Keywords: Aging, Mobility, Built environment
Introduction
Outdoor mobility is critical for healthy aging.1 In fact, the most common type of moderate physical activity chosen by older adults is walking,2 which provides health benefits that contribute to the maintenance of functional ability.3–8 In a pivotal article entitled “Just Get out the Door!”, Simonsick and colleagues9 found that walking outdoors, even just two blocks per day on average, prevents physical decline in functionally limited older women. Yet, only 25 % of older adults walk outdoors on a regular basis.10
While a host of studies have focused on the role of individual factors for encouraging or preventing outdoor mobility (e.g., functional status, self-efficacy, outcome expectations),11–14 considerably less research has examined the importance of the urban built environment for older adults aging in place. Urban environmental barriers subjectively reported by older adults include poor access to public transportation, discontinuous or uneven sidewalks, curbs, and inadequate lighting.15,16 Pedestrian-oriented designs (e.g., continuous, barrier-free sidewalks, four-way stop signals, and pedestrian amenities) and access to recreational facilities have been shown to be positively associated with mobility in older adults.17–25 Poor street conditions, heavy traffic, and excessive noise have been shown to be associated with the onset of mobility impairments 1 to 3 years later.26,27
One study in the city of Chicago found that older adults with movement-related impairments had a fourfold higher odds of reporting severe difficulty walking when living in neighborhoods with streets in poor condition (e.g., cracks, broken curbs, potholes) compared to those living in neighborhoods with streets in good condition.28 Another study of older adults living in the Houston area found that curb cuts and bus shelters were non-existent in the vast majority (75 %) of respondent neighborhoods and fewer than 10 % of respondents used public transportation even though close to half of these adults lived within two blocks of a bus stop.16 Curb cuts, smooth pavement, and barrier-free sidewalks are just some of the many environmental factors that can enhance independence and social participation in older adults at greatest risk, such as those who are socially isolated, prone to falling, or those with underlying weakness in movement-related functions and balance. Without accessible built environments, older adults can find it difficult to care for their daily needs (e.g., shopping, banking) or their health (access health care facilities or a pharmacy), with subsequent risks for isolation,15 institutionalization,29–31 and even death.16 Qualitative work from a study in central North Carolina15 found that older adults specifically identified poor-quality and inconsistent sidewalks as contributing to their inability to walk independently outside their homes. They mentioned that some sidewalks were too high to negotiate, and others lacked curb cuts. One person commented “you can go a stretch and there is a sidewalk but then all of a sudden you are either walking in grass, or mud or on the road” (p. 21). These findings highlight the importance of the urban context as a consequential factor in the degree to which limitations in physical functioning translate into actual difficulty in activities outside the home.
Socioeconomically disadvantaged older adults are more vulnerable to environmental barriers because of their greater need to access social services, such as a community meal programs and senior centers.16 Women, minority, and low-income seniors are especially vulnerable because of their greater propensity to live alone in socially and economically disadvantaged areas without the language, education, or economic resources to negotiate or even improve their environment. Yet, the majority of studies on the built environment and older adult mobility have come from cross-sectional studies with generally healthy or well-functioning older adults. Little is known about the factors related to long-term profiles of outdoor mobility among more physically and socioeconomically vulnerable elders who are struggling to age in place. A better knowledge of the built environment factors that constrain long-term mobility in frail older adults is critical because this is the population at greatest risk for physical decline and institutionalization.31,32
The purpose of this work was to examine 15-month trajectories of outdoor mobility in a socioeconomically and physically vulnerable population of community-dwelling elderly living in central Detroit, a densely populated, yet medically underserved urban area that has experienced rapid socioeconomic and structural change since the 1950s. We examine the role of urban built environment characteristics in shaping the pattern of mobility trajectories in this population, focusing specifically on the conditions in the proximate environment such as sidewalk quality and access to public transit. We hypothesize that there may be differences in the trajectory patterns of this population, and that environmental risk factors will play a critical role in determining the probability of having a particular trajectory. Because independent mobility is not just dependent on characteristics in the outdoor environment but also whether someone can simply go out their front door, it is important to also consider barriers within (unsafe flooring, steep stairs), or leading up to (unsafe front porch) the home when investigating barriers to outdoor mobility. Evidence indicates that low-income and minority older adults are more likely to live in substandard housing with a decaying front porch or inaccessible front steps.15,16 We therefore consider both indoor hazards as well as outdoor environmental barriers in our models.
Methods
Data
Data are drawn from the Michigan Minimum Data Set for Home Care (MDS-HC), an enumerative database of persons in the State of Michigan who qualify for federal or state-funded home and community-based long-term care through a Medicaid waiver program. The program is funded jointly by the State and Federal governments to help older adults remain in their homes by providing home-based services (e.g., personal care, nursing), acting as an alternative to nursing home placement.33,34 Clients must have functional needs and meet a low-income cutoff to be eligible for this program.
The MDS-HC database contains data for almost 500,000 individuals (collected since 2001 and up to 2008 in this analysis), and we focus on a subsample of 1,188 vulnerable older adults (age 55+) living in central Detroit, an area with a high proportion of older adults in poverty. Clients are assessed at intake and every 90 days by trained nursing/social worker care management teams. We focus on assessments over a 15-month period, corresponding to a maximum of six assessment visits for each individual.
On behalf of the state, the University of Michigan maintains a data archive (Michigan Master Data Archive, MMDA) including longitudinal assessments for all MDS-HC participants, and researchers within the University of Michigan community may use the MMDA with permission of the MMDA Oversight Committee and the Michigan Department of Community Health (MDCH). All projects require a data use agreement from MDCH and must obtain IRB approval from the University’s IRB and the State IRB at MDCH. This project received IRB approval from both bodies.
Individual Measures
All data in the MDS-HC are collected using the Resident Assessment Instrument for Home Care,34 a standardized comprehensive assessment instrument incorporating multiple clinical and functional domains important for care planning. More than 200 variables are collected on each client including physical functioning, sensory limitations, cognition, medication use, and disease diagnoses. All possible sources of information are used in the assessment, including clients, caregivers, direct observation, and any medical records. Assessments are made every 90 days by case managers (nurses or social workers) who are trained in the use of the instrument, which has demonstrated inter-rater reliability.33
The outcome of interest, outdoor mobility, is rated at every assessment according to the number of days the client goes outside in a typical week (range, 0–7). In addition, case managers document whether the client limits going outdoors due to a fear of falling and whether there are home barriers at the entry of the residence that make it difficult to enter or leave (e.g., unstable front stairs, or a client lives in a multi-story building in which the elevator is often broken). Analyses control for key sociodemographic factors, including age (in years), gender, race (African American vs. White), marital status [not married (including widowed, divorced/separated) vs. married], and living arrangements (lives alone vs. lives with others). Other covariates include a summary index of the number of medically diagnosed chronic health conditions (e.g., diabetes, hypertension, heart problems, arthritis), and a measure of vision impairment (even with glasses) ranging from 0 (no impairment) to 4 (severely impaired). A measure of difficulty with seven self-care activities of daily living (bathing, dressing, eating, grooming, transferring, toileting, and indoor locomotion) is rated on a scale from 0 (independent) to 5 (total dependence) and averaged across all seven activities. Finally, a measure of mobility impairment is based on the client’s difficulty walking, which ranges from 0 (walks without help) to 5 (severe difficulty walking even with help). These variables are documented at baseline (client intake) and are modelled as time invariant characteristics.
Community Measures
Data on characteristics of the surrounding local environment were obtained from a “virtual audit” using Google Street View images in Google Earth from 2007 to 2009. A virtual audit has been shown to provide reliable indicators of land use, recreational facilities, and the local food environment at a fraction of the cost of an in-person audit.35,36 All subject addresses were geocoded, and a trained rater conducted a virtual audit of all four streets in each subject’s block using a standardized instrument. A summary urban accessibility score was calculated for each street by summing the number of mobility-enhancing features37: (1) sidewalks in place on both sides of the street; (2) continuous sidewalks; (3) smooth/flat/unbroken sidewalks; (4) free from obstructions; (5) wide enough to allow two people to pass comfortably; and (6) a public transportation stop on the street. A mean score was calculated by averaging summary scores across the four streets in each subject’s block such that a higher score indicates greater accessibility.
Statistical Analysis
We used a statistical methodology that is specifically designed to capture heterogeneity in long-term trajectories of mobility by empirically identifying distinct sub-populations of trajectories over time, and modeling differences in the characteristics of subjects across these groups. Rather than assuming that there is a single underlying population trajectory of outdoor mobility, we seek to capture subtle but significant differences in trajectory patterns that may exist in the frail elderly population. A generalized growth mixture model was used to model the number of days a client goes outside in a typical week. By using latent trajectory classes (categorical latent variables), the growth mixture model allows different classes of individuals to vary around different mean growth curves.38 Because the trajectory of interest in this paper is a count variable, we used a Poisson growth model with a log-link function in our analyses.
The measurement part of the model captures the growth factors (intercept and slope) as measured by multiple indicators of outdoor mobility over time. A linear growth model is first specified with equidistant time points, but we also test the fit of a nonlinear form by using quadratic terms. The structural part of the model incorporates the growth model within a larger latent variable model by relating the growth factors to other observed and latent variables. Of particular interest is the latent trajectory class variable, which represents the unobserved subpopulation of membership for respondents. This allows a separate growth model for each of the latent classes. Of key interest is whether the urban accessibility variable predicts class membership in a multinomial logistic regression, controlling for sociodemographic characteristics, home barriers, and health status.
Model building proceeded in a sequential process by first specifying the measurement model and then incrementally increasing the number of latent classes. While substantively based theory is used as the primary means to determine the best fitting model, good fitting models are characterized by (1) a low value for the Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC); (2) a statistically significant (low p value) Lo–Mendell–Rubin likelihood ratio test; and (3) distinct posterior probabilities for individual class membership.38 All models are estimated in Mplus Version 6.12 using full information maximum likelihood with robust standard errors. Multiple random starts are used to minimize local optimal in the likelihood.
Results
Table 1 presents the sociodemographic and health characteristics for the analytic sample at baseline (client intake). The average age was 78.7 years, 71 % were female, 78 % were African-American, 71 % were not currently married, but only 35 % lived alone. On average, clients had three underlying chronic health problems and had minor difficulty seeing even when wearing glasses. The average self-care difficulty and mobility impairment scores were 1.6 and 2.4, respectively, which indicates that the average subject needed some assistance with self-care activities, and had moderate difficulty walking. During the course of follow-up, 56 % died and 10 % were transferred to a nursing home, making them ineligible for further follow-up. On average, subjects were followed for 6 months (corresponding to three case manager visits).
Table 1.
Subject characteristics at baseline (program intake) Michigan Minimum Data Set for Home Care: Detroit residents age 55+ (n = 1,188)
| Mean (S.D.) or N (%) | |
|---|---|
| Sociodemographic characteristics | |
| Age | 78.7 (10.0) |
| Female | 842 (71 %) |
| African-American | 921 (78 %) |
| Not married | 843 (71 %) |
| Lives alone | 419 (35 %) |
| Health status | |
| Number of chronic health conditions | 3.3 (1.8) |
| Vision impairment (0 = none, 4 = severe) | 0.9 (0.9) |
| Mean self-care difficulty score (0 = independent, 5 = total dependency) | 1.6 (1.1) |
| Mobility impairment (0 = none, 5 = severe) | 2.4 (1.8) |
| Reports fear of falling outdoors | 665 (56 %) |
| Outdoor mobilitya | |
| Goes outdoors at least once a week | 1,752 (67.8 %) |
| Number of days out per week | 1.6 (1.7) |
| Home environment | |
| Barriers at entry | 232 (23 %) |
| Urban residential environment | |
| Sidewalks in place on both sides of street | 986 (83 %) |
| Continuous unbroken sidewalks | 807 (68 %) |
| Smooth sidewalk surfaces | 641 (54 %) |
| Sidewalks free from obstructions | 760 (64 %) |
| Sidewalks wide enough for two people to pass | 807 (68 %) |
| Public transit stop on the block | 368 (31 %) |
| Urban accessibility score (range, 0–6) | 3.5 (1.2) |
aPresented for baseline; modeled as time-varying
Roughly two thirds of subjects (67.8 %) reported going outside at least once in a typical week (Table 1). Fear of falling, which may prevent subjects from venturing outside, was reported by over half of these subjects, and about one quarter of clients lived in homes where there were barriers to entry or exit. The average sidewalk accessibility score was 3.5 (±1.2) on a scale of 0 to 6. Sidewalks were generally in place on both sides of the street surrounding each client’s residential block, but the condition of the sidewalks was variable (Table 1). Less than a third of these older adults had a public transit stop on their residential block.
Table 2 reports the results and fit statistics for a systematic progression of growth mixture models. The first column presents the results for the single class model. Because the Poisson model uses a log-link function, the coefficients can be interpreted by taking the antilog of the parameter estimates. At baseline (program intake), clients reported going outdoors about 1 day per week on average (e−.018 = .98), and over the 15-month period of follow-up the expected number of days outdoors declined at a rate of 2 % per visit (100[e−.023−1] = −2.27 %). However, this rate of decline was not significantly different from zero.
Table 2.
Generalized growth mixture model results: Poisson regression coefficients for trajectories of outdoor mobility Michigan Minimum Data Set for Home Care: Detroit residents age 55+ (n = 1,188)
| Single-class model | Two-class model | |||
|---|---|---|---|---|
| Linear | Quadratic | Class 1 (17 %) (almost never goes out) | Class 2 (83 %) (occasionally goes out) | |
| Intercept | −.018 | .004 | −1.64*** | .40*** |
| Slope (visit) | −.023 | −.066**** | −.65 | .08** |
| Quadratic | .099 | −1.60**** | −.013** | |
| Goodness of fit | BIC = 10,046.317 | BIC = 10,064.73 | BIC = 9,881.576 | |
| AIC = 10,021.714 | AIC = 10,020.44 | AIC = 9,832.370 | ||
BIC Bayesian Information Criterion, AIC Akaike Information Criterion
**p < .01; ***p < .001; ****p < .10 (two-tailed tests)
Adding a quadratic term to the single class model did not suggest any improvement in fit, but a two-class model with a quadratic curve showed a substantial improvement in fit over the single class model (second and third columns of Table 2). The change in the BIC and AIC values, coupled with a significant Lo–Mendel–Rubin Likelihood ratio test (p < .001, not shown in Table 2), suggests that a two-class solution is preferable to a single class model. Membership in each class showed good classification quality with individuals most likely to belong to their predicted class [posterior probability is markedly higher (>0.90) than for the other class]. Adding a third class (model not shown) did not result in any improvement in model fit, and the posterior probabilities did not differentiate class membership well.
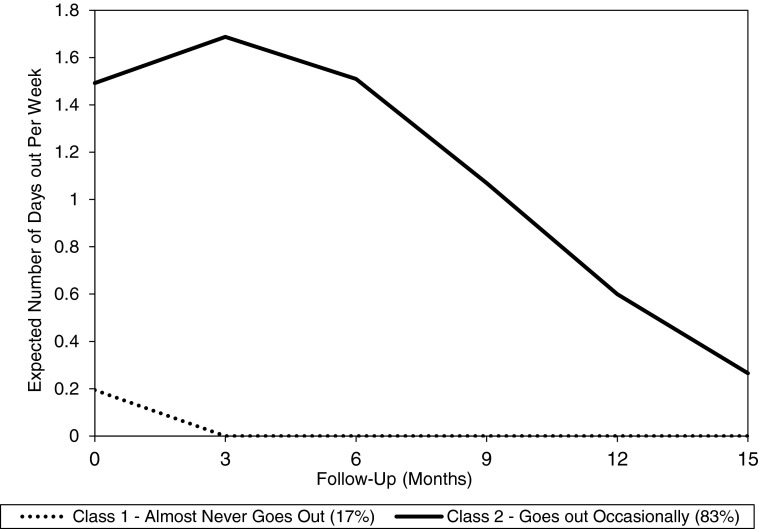
Figure 1 shows the estimated trajectories of going outside according to the two-class solution. The two curves represent two distinct trajectories of outdoor mobility over the 15-month follow-up period. Class 2 (with 83 % of the sample) represents the majority of the sample who go out occasionally in the first 3 months of follow-up (about 1.5 days per week on average at client intake, increasing to about 1.7 days per week after 90 days of follow-up); but the frequency of outdoor mobility declines rapidly over the next 12 months. In contrast, individuals in Class 1 (17 % of the sample) almost never go outdoors (the expected number of days out averaged 0.2 at baseline and fell to zero days outdoors by the third month of follow-up).
FIGURE 1.
Predicted number of days outdoors based on two-class Poisson growth mixture model. Michigan Minimum Data Set for Home Care: Detroit residents age 55+ (n = 1,188).
The next step in the modeling process adds the covariates to the model, regressing sociodemographic characteristics, health status, home barriers, and the urban accessibility score on class membership. Table 3 reports the results from the logistic regression for class membership [adjusted odds ratios (OR) and 95 % confidence intervals (CI)] using Class 2 (occasionally goes out doors) as the reference group. Compared to those who go out on an occasional basis individuals in the group that almost never goes outdoors tended to be older, to have more difficulty with basic self-care activities, and to have greater difficulty with mobility and vision. Each unit increase in the self-care difficulty measure increased the odds of being in the homebound group by almost 60 % (OR = 1.58, 95 % CI = 1.2, 2.0; Table 3). Living arrangements and marital status were not related to class membership and are not included in Table 3.
Table 3.
Logistic regression for latent class membership: Michigan Minimum Data Set for Home Care: Detroit residents age 55+ (n = 1,188)
| Latent Class 1c (almost never goes out) | ||
|---|---|---|
| Coefficient | OR (95 % CI) | |
| Age (years) | .03* | 1.03 (1.01, 1.05) |
| Femalea | −.09 | 0.91 (0.55, 1.52) |
| African-Americanb | −.18 | 0.84 (0.31, 2.28) |
| Self-care difficulty | .46*** | 1.58 (1.24, 2.01) |
| Mobility impairment | .25** | 1.29 (1.09, 1.51) |
| Chronic health conditions | −.06 | 0.95 (.82, 1.09) |
| Vision impairment | .28* | 1.32 (1.06, 1.66) |
| Barriers at entry to home | .40**** | 1.49 (.93, 2.47) |
| Urban accessibility score | −.16* | 0.85 (0.71, .99) |
OR adjusted odds ratio, CI confidence interval
*p < .05; **p < .01; ***p < .001; ****p < .10 (two-tailed tests)
aReference group is Male
bReference group is White
cLatent Class 2 (occasionally goes outdoors) is the reference class
After controlling for these individual risk factors, there was evidence that barriers in the home and urban environment were important for outdoor mobility. Individuals living with barriers at the entry to their home, which made it difficult to enter or leave, had almost 50 % higher odds of being in the homebound group (although this was only approaching statistical significance in two-tailed tests). Conversely, living in a more accessible urban environment was associated with a reduced odds of being in the homebound group. Each unit increase in the urban accessibility measure was associated with a 15 % lower odds of being in the homebound group (adjusted OR = .85, 95 % CI = .71, .99; Table 3).
The model also captures latent class-specific effects of the covariates on the growth factors. No significant effects were found for the covariates on the slope, but effects on the intercept are presented in Table 4 for each latent class. Table 4 includes the unstandardized regression coefficients (with standard errors) for the effects of the covariates on the outdoor mobility intercept for each of the two latent classes. Within the homebound group (Class 1, almost never goes out), women and those with greater mobility impairment were expected to have even fewer days outdoors at baseline (lower intercept) than others in this latent class. Moreover, a fear of falling drastically reduced the expected number of days out at baseline among those who almost never go out (Latent Class 1, Table 4). Among those who go out more frequently (occasionally go out, Class 2), a fear of falling is also associated with fewer days out at baseline. In addition, those with greater difficulty with self-care activities and with walking go out somewhat less frequently than others in this class (Class 2, Table 4).
Table 4.
Regressing growth parameter (intercept) on health and sociodemographic characteristics by latent class of outdoor mobility Michigan Minimum Data Set for Home Care: Detroit residents age 55+ (n = 1,188)
| Latent Class 1 (almost never goes out) | Latent Class 2 (occasionally goes out) | |||
|---|---|---|---|---|
| Coefficient | Standard error | Coefficient | Standard error | |
| Age | .02 | .02 | −.01**** | .003 |
| Femalea | −1.21* | .51 | −.02 | .07 |
| African-Americanb | −.90 | .62 | .09 | .34 |
| Chronic health conditions | .13 | .17 | −.03 | .02 |
| Vision impairment | −.39 | .31 | .01 | .04 |
| Fear of falling | −1.49** | .53 | −.40*** | .07 |
| Self-care difficulty | .12 | .26 | −.11* | .04 |
| Mobility impairment | −.45* | .19 | −.05* | .02 |
*p < .05; **p < .01; ***p < .001; ****p < .10 (two-tailed tests)
aReference group is Male
bReference group is White
Discussion
This study examined trajectories of outdoor mobility in a socioeconomically and physically vulnerable population of older adults living in the city of Detroit, a medically underserved urban area that has experienced rapid socioeconomic and structural change since the mid-twentieth century. In recent decades, there has been a growing interest in developing interventions to help older adults remain in their own homes and communities and out of long-term care institutions. Multiple studies suggest that maintaining outdoor mobility is an important step in preventing disability and institutionalization.9,13,31 However, most of this research is limited to cross-sectional studies or samples of non-frail older adults. As a result, we have much more restricted knowledge of the factors related to outdoor mobility in the physically and socioeconomically vulnerable community-dwelling elderly, precisely those at greatest risk for physical decline and institutionalization. We advance this area of research by examining both individual and environmental factors in the urban setting that shape patterns of long-term trajectories of outdoor mobility in community-dwelling frail elderly.
We found evidence of two distinct latent trajectories of outdoor mobility over a 15-month period. A small minority were essentially homebound, almost never venturing outdoors over time. However, a sizable majority of these frail elderly reported some outdoor mobility, going outdoors at least once a week over the first 3 months of follow-up, but steadily declining in their outdoor mobility throughout the subsequent year. While these results emphasize the very frail nature of this population, they nonetheless highlight heterogeneity in this group that would be masked in a model using a single underlying population trajectory. By modeling multiple latent trajectory classes, our results were able to identify meaningful subpopulations of outdoor mobility in the frail elderly.
Consistent with the existing literature,7,8,13 individual health and sociodemographic risk factors were associated with membership in the different latent trajectories. Not surprisingly, older adults experiencing greater difficulty with self-care activities and with mobility were more likely to be in the homebound group, while greater independence in these critical life activities increased the odds greater outdoor mobility. But even controlling for these individual risk factors we found non-trivial effects of the surrounding urban environment for membership in the different latent classes of outdoor mobility. Older adults living on a block with accessible sidewalks and a public transit stop were significantly more likely to be in the more mobile group.
Although only approaching statistical significance, older adults with home entry barriers were more likely to be homebound than those with more accessible entryways. Accessible urban environments are only meaningful for older adults if they can get out their front door. Our results suggest that home-entry conditions, such as an unsafe front porch or an apartment elevator that rarely works, are critical to consider when examining the role of community or environmental factors for outdoor mobility.
While research is increasingly focused on understanding the individual (and more rarely the environmental) factors that relate to aging in place,39 comparatively less research has considered the unique needs of socieconomically and physically frail older adults struggling to remain in their communities. Due to its rapid socioeconomic and structural decline, the city of Detroit presents unique challenges for frail community-dwelling elders. Vacant lots, overgrown vegetation, broken sidewalks, heightened criminal activity, and loose dogs that roam the city are just some of the conditions that make it difficult for older adults to be mobile in their community.40 We attempted to examine the effect of this structural deterioration by modeling the effect of urban accessibility in the form of walkable, barrier-free sidewalks and access to public transportation. This work was based on the premise that the urban environment is a potential source of variability in outdoor mobility, particularly among the vulnerable and frail elderly. Results suggest that other studies should consider including environmental factors in addition to individual factors when examining outdoor mobility in physically frail older adults.
Limitations
This study was subject to limitations in both study design and methodology. First, there was a temporal mismatch between the individual data (2001–2008) and the data collected on the urban environment (2007–2009). While the environmental features we assessed (e.g., sidewalk characteristics) were unlikely to have changed dramatically since 2001, the temporal mismatch may have contributed to some misspecification in our models and constrained the ability to detect stronger effects in the urban accessibility measure. Moreover, information on seasonal variation in sidewalk accessibility was not available, but is likely to be of considerable relevance for walking among older adults.40 Second, a measure of going outside does not necessarily equal outdoor mobility, but it may act as a proxy or important prerequisite for mobility and other related outcomes.9,31
Nonetheless, in spite of these limitations, the results of this study identify individual and environmental factors related to long-term profiles of outdoor mobility among a population of physically and socioeconomically vulnerable older adults who are struggling to age in place. Going outside is an important way in which older adults can stay connected to their communities and remain independent. Attention to sidewalk quality in urban areas with a high proportion of older adults can be a critical, yet modifiable factor, facilitating aging in place.
Acknowledgments
This research was supported in part by Grant Number K01EH000286-01 from the Centers for Disease Control and Prevention (CDC). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the sponsors.
References
- 1.Ettinger WH. Physical activity and older people: a walk a day keeps the doctor away. J Am Geriatr Soc. 1996;44(2):207. doi: 10.1111/j.1532-5415.1996.tb02442.x. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Patterns and trends in physical activity. Physical Activity and Health: A Report of the Surgeon General. Atlanta: GA; Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. p.175–185.
- 3.Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48(4):445–469. doi: 10.1016/S0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 4.Wong CH, Wong SF, Pang WS, Azizah MY, Dass MJ. Habitual walking and its correlation to better physical function: implications for prevention of physical disability in older persons. J Gerontol A Biol Sci Med Sci. 2003;58(6):M555–M560. doi: 10.1093/gerona/58.6.M555. [DOI] [PubMed] [Google Scholar]
- 5.Pahor M. Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 6.Guralnik JM. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137(8):845–857. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 7.Fried LP, Bandeen-Roche K, Chaves PHM, Johnson BA. Preclinical mobility disability predicts incident mobility disabilityin older women. J Gerontol A Biol Sci Med Sci. 2000;55(1):M43–M52. doi: 10.1093/gerona/55.1.M43. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simonsick EM, Guralnik JM, Volpato S, Balfour J, Fried LP. Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the Women's Health and Aging Study. J Am Geriatr Soc. 2005;53(2):198–203. doi: 10.1111/j.1532-5415.2005.53103.x. [DOI] [PubMed] [Google Scholar]
- 10.Le Masurier GC, Bauman AE, Corbin CB, Konopack JF, Umstattd RM, Van Emmerik REA. Assessing walking behaviors of selected subpopulations. Med Sci in Sports & Exercise. 2008;40(7):S594–S602. doi: 10.1249/MSS.0b013e31817c68b1. [DOI] [PubMed] [Google Scholar]
- 11.Asano M, Miller WC, Eng JJ. Development and psychometric properties of the ambulatory self-confidence questionnaire. Gerontology. 2007;53(6):373–381. doi: 10.1159/000104830. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher N, Clarke P, Loveland-Cherry C, Ronis D, Nyquist L, Gretebeck KE. Environmental and psychosocial influences on neighborhood walking in older adults with and without mobility limitations. Res Gerontol Nurs. 2012;5:238–250. doi: 10.3928/19404921-20120906-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.M221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simonsick EM, Newman AB, Visser M, et al. Mobility limitation in self-described well-functioning older adults: importance of endurance walk testing. J Gerontol A Biol Sci Med Sci. 2008;63(8):841–847. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Debnam K, Harris J, Morris I, Parikh S, Shirey L. Durham County socially isolated older adults: an action-oriented community diagnosis. University of North Carolina at Chapel Hill School of Public Health, Department of Health Behavior and Health Education; 2002.
- 16.Markham JP, Gilderbloom JI. Housing quality among the elderly: a decade of changes. Int J Aging Hum Dev. 1998;46(1):71–90. doi: 10.2190/A6EQ-FY4C-F4CF-18G9. [DOI] [PubMed] [Google Scholar]
- 17.Humpel N, Owen N, Leslie E. Environmental factors associated with adults' participation in physical activity. Am J Prev Med. 2002;22:188–199. doi: 10.1016/S0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- 18.Addy CL, Wilson DK, Kirtland KA, Ainsworth BE, Sharpe P, Kimsey D. Associations of perceived social and physical environmental supports with physical activity and walking behavior. Am J Public Health. 2004;94:440–443. doi: 10.2105/AJPH.94.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Booth ML, Owen N, Bauman A, Clavisi O, Leslie E. Social-cognitive and perceived environment influences associated with physical activity in older Australians. Prev Med. 2000;31(1):15–22. doi: 10.1006/pmed.2000.0661. [DOI] [PubMed] [Google Scholar]
- 20.Patterson PK, Chapman NJ. Urban form and older residents' service use, walking, driving, quality of life, and neighborhood satisfaction. Am J Heal Promot. 2004;19:45–52. doi: 10.4278/0890-1171-19.1.45. [DOI] [PubMed] [Google Scholar]
- 21.Fisher KJ, Li F, Michael Y, Cleveland M. Neighborhood-level influences on physical activity among older adults: a multilevel analysis. J Aging Phy Activity. 2004;11:45–63. doi: 10.1123/japa.12.1.45. [DOI] [PubMed] [Google Scholar]
- 22.Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the built environment with physical activity and obesity in older persons. Am J Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michael Y, Beard T, Choi D, Farquhar S, Carlson N. Measuring the influence of built neighborhood environments on walking in older adults. J Aging Phy Activity. 2006;14:302–312. doi: 10.1123/japa.14.3.302. [DOI] [PubMed] [Google Scholar]
- 24.Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J Epidemiol Community Health. 2005;59(7):558–564. doi: 10.1136/jech.2004.028399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li F, Fisher KJ. A multilevel path analysis of the relationship between physical activity and self-rated health in older adults. J Phys Act Heal. 2004;1:398–402. [Google Scholar]
- 26.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155:507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 27.Schootman M, Andresen EM, Wolinsky FD, Malmstron TK, Miller JP, Miller DK. Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans. Am J Epidemiol. 2006;163:450–458. doi: 10.1093/aje/kwj054. [DOI] [PubMed] [Google Scholar]
- 28.Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility disability and the urban built environment. Am J Epidemiol. 2008;168(5):506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gill TM, Allore HG, Han L. Bathing disability and the risk of long-term admission to a nursing home. J Gerontol A Biol Sci Med Sci. 2006;61A:821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- 30.Cohen MA, Tell EJ, Wallack SS. Client-related risk factors of nursing home entry among elderly adults. J Gerontol. 1986;41:785–792. doi: 10.1093/geronj/41.6.785. [DOI] [PubMed] [Google Scholar]
- 31.Jette AM, Branch LG, Sleeper LA, Feldman HR, Sullivan LM. High-risk profiles for nursing home admission. Gerontologist. 1992;32:634–640. doi: 10.1093/geront/32.5.634. [DOI] [PubMed] [Google Scholar]
- 32.Alexander NA, Goldberg A. Common gait disturbances: a clinical overview. In: Hausdorff JM, Alexander NB, editors. Gait Disorders: Evaluation and Management. Boca Raton: FL: Taylor & Francis Group; 2005. pp. 1–18. [Google Scholar]
- 33.Morris JN, Fries BE, Steel K, Ikeggami N, Bernabei R, Carpenter GI. Comprehensive clinical assessment in community setting: applicability of the MDS-HC. J Am Geriatr Soc. 1997;45:1017–1024. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- 34.Fries BE, Shugarman LR, Morris JN, Simon SE, James M. A screening system for Michigan's home- and community-based long-term care programs. Gerontologist. 2002;42:462–474. doi: 10.1093/geront/42.4.462. [DOI] [PubMed] [Google Scholar]
- 35.Clarke P, Ailshire J, Melendez R, Bader M, Morenoff J. Using Google Earth to conduct a neighborhood audit: reliability of a virtual audit instrument. Health & Place. 2010;16(6):1224–1229. doi: 10.1016/j.healthplace.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rundle AG, Bader MDM, Richards CA, Neckerman KM, Teitler JO. Using Google Street View to audit neighborhood environments. Am J Prev Med. 2011;40(1):94–100. doi: 10.1016/j.amepre.2010.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Michael YL, Keast EM, Chaudhury H, Day K, Mahmood A, Sarte AFI. Revising the senior walking environmental assessment tool. Prev Med. 2009;48(3):247–249. doi: 10.1016/j.ypmed.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muthen BO. Latent variable analysis: growth mixture modelling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Newbury Park: Sage; 2004. pp. 345–368. [Google Scholar]
- 39.Lehning AJ. City governments and aging in place: community design, transportation and housing innovation adoption. Gerontologist. 2012;52(3):345–356. doi: 10.1093/geront/gnr089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gallagher N, Gretebeck K, Robinson J, Torres E, Murphy S, Martyn K. Neighborhood factors relevant for walking in older, urban, African American adults. J Aging Phys Activity. 2010;18(1):99–115. doi: 10.1123/japa.18.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]