Abstract
This study examined the effect of syringe exchange program setting on the injection practices, health status, and health service utilization patterns of injection drug users (IDUs) recruited from a public urban hospital. One hundred sixty-six participants were randomized to either community– or hospital–based syringe exchange services. Poisson regression models were used to compare service utilization between groups. In both conditions, risky drug use practices decreased, and physical health functioning improved over time. Hospital–based syringe exchange program (SEP) attendees had 83% more inpatient admissions (p < .0001) and 22% more ambulatory care visits (p < .0001) than those assigned to the community–based SEP condition. Syringe exchange services that are integrated into public hospital settings may serve as a valuable strategy to engage hard to reach IDU populations in behavioral interventions designed to reduce HIV risk transmission behaviors and increase access to, or engagement in, the use of secondary and tertiary preventive medical care.
Syringe exchange programs (SEPs) reduce the transmission of HIV and other blood-borne pathogens through the provision of free sterile injection equipment, disposal of used syringes, and referrals to HIV testing and drug treatment. Increasing the availability of sterile syringes through SEPs, pharmacies, and other outlets reduces unsafe injection practices, such as needle sharing, and reduces the spread of HIV infection (Des Jarlais et al., 1996; Hagan & Thiede, 2000; MacDonald, Law, Kaldor, Hales, & Dore, 2003; Valente, Foreman, Junge, & Vlahov, 2001; Vlahov et al., 1997). Moreover, SEPs are a cost–effective HIV prevention strategy (Laufer, 2001).
Despite the effectiveness of SEPs, questions about how to operate these programs remain unanswered. Factors such as SEP location, syringe distribution policies, number of hours of operation, days of the week and time of day of operation, ancillary services offered, harm reduction philosophy of staff, law enforcement practices and cultural appropriateness of staff may affect risk behaviors and patterns of SEP use (Bluthenthal, Kral, Lorvick, & Watters, 1997; Kral & Bluthenthal, 2003; Riley et al., 2000; Rockwell, Des Jarlais, Friedman, Perlis, & Paone, 1999). The influence of these factors on the effectiveness of SEPs requires further study.
Although SEPs and health care facilities share the mission of preventing or reducing complications of injection drug use, they usually operate independently of one another. In addition, although hospital–based SEPs have been instituted in other countries, including Australia, Canada, and the United Kingdom, this approach has not gained widespread general acceptance in the United States (Commonwealth Department of Health and Ageing, 2002; Hankins, 1998; Parsons et al., 2002). In the United States SEPs are usually freestanding. Integration with the health care system may have advantages, but without further study it remains unclear whether SEPs can be effectively integrated into the traditional continuum of the health care system and, if successful integration were achieved, whether or not added benefits would be gained. Several benefits do seem reasonable. Injection drug users (IDUs) use public emergency departments as a regular source of care; this setting would afford the opportunity to identify active IDUs and engage them in HIV risk reduction efforts. Furthermore, because referral to off–site services impedes service delivery to IDUs (Umbricht–Schneiter, Ginn, Pabst, & Bigelow, 1994), syringe exchange services on site in health care facilities may expedite the delivery of less costly services (Perlman et al., 2001).
In this randomized controlled trial, SEPs in two different settings were compared. The first were typical free-standing community–based SEPs, and the second was a hospital–based SEP, which was enhanced by education on safe self–injection practices. We sought to examine whether the setting in which the SEP resides has a differential impact on injection practices and health outcomes. We did not, however, expect one setting to have across–the–board advantages over the other. Both settings may have their advantages and disadvantages. For example, for some clients, community–based SEPs may be more easily accessible, increasing the frequency of use. On the other hand, many IDUs need medical care for untreated acute and chronic illnesses, and the hospital–based SEP may have the advantage of increasing IDUs’ access to less costly outpatient services and to primary care services, which may improve physical health. Determining the extent to which SEP setting impacts HIV risk behaviors and adverse health outcomes can assist public health policy planners in making decisions about where to locate SEPs in their communities to optimize HIV prevention efforts.
METHODS
PARTICIPANTS
Participants were recruited from the emergency department, outpatient clinics, and inpatient wards at San Francisco General Hospital (SFGH). SFGH is the primary treatment site for the city’s low–income and indigent population, and as such, the hospital provides treatment to many substance users. Research staff made weekday recruitment visits to the emergency department and inpatient and outpatient units of SFGH as well as responded to referrals from medical staff. Study inclusion criteria were (a) at least 18 years of age; (b) from the Diagnostic and Statistical Manual of Mental Disorders (4th ed.) criteria for a drug dependence disorder; (c) current injection drug use; (d) not interested in receiving drug abuse treatment; and (e) residents of the Mission District in San Francisco, which ensured easy access to SFGH.
A total of 830 people were screened during a 2–year period. Out of those screened, 234 were eligible, and 166 people enrolled in the study. Five hundred ninety-six people were not eligible. Ineligible people could not participate in the study for the following reasons: 19% (115) received substance abuse treatment within the past 30 days, 23% (140) were not IDUs, 6% (36) were interested in substance abuse treatment, 25% (149) did not live in the Mission District, 1% (6) were experiencing active psychosis, 1% (5) were planning to leave the area within a year, 1% (5) were recently released from psychiatric emergency services, 5% (29) were already enrolled in a different research study, and 19% (111) were ineligible because they fell into more than one of the categories above, or were ineligible for other reasons.
For the sixty–eight people who were eligible but did not enroll, demographic characteristics were as follows: 40% (27) were female, 54% (37) were male, and 6% (4) did not indicate their gender. Regarding their ethnic background, 53% (36) were White, 18% (12) were African American, 10% (7) were Hispanic, 1% (1) were Native American, 3% (2) were mixed/other, and 15% (10) did not report their ethnicity. The mean age of those who were eligible but did not enroll was 38 years old. Those who were eligible, but declined to participate did not differ from those who agreed to participate with respect to age, or race/ethnicity, but those who were eligible and did not enroll were more likely to be female (42% vs. 18%; p = 006).
PROCEDURES
IDUs who met eligibility criteria and gave informed consent participated in a baseline interview, which lasted approximately 90 minutes, and included questions regarding personal background characteristics, housing and employment histories, health and psychological problems, drug and alcohol use, HIV risk behaviors, history of attendance at SEPs, and past health service utilization. All participants were offered HIV and hepatitis B and C viruses (HBV and HCV) testing and pretest and posttest counseling, which included a discussion of the risks of contaminated needles and use of one sterile syringe for every injection (HBV and HCV, respectively). Blood samples were tested for HIV antibodies using enzyme immunoassay (EIA) and confirmatory Western blot and for HBV and HCV antibodies using EIA. Certified HIV counselors conducted pretest counseling at the time that phlebotomy was performed. Because women are underrepresented among substance using populations, we stratified participants on gender before randomization. The randomization scheme was based on computer-generated random numbers, and each new research participant was assigned to an intervention group by opening sealed envelopes. Following the completion of the baseline interview, and after HIV and hepatitis testing, participants were randomly assigned to receive community (n = 83) or hospital–based (n = 83) SEP services. Follow–up assessments were conducted at 6 and 12 months after the baseline visit.
Participants returned for their HIV, HBV, and HCV test results and posttest counseling 2 weeks after the baseline visit. Standard HIV counseling and testing procedures were followed, including risk reduction counseling in accordance with guidelines from the Centers for Disease Control and Prevention (2001). Participants who were found to test positive for HIV, HCV, or active HBV were referred for further medical evaluation. Those who were susceptible to HBV were referred for vaccination.
This study was approved by the University of California, San Francisco Committee on Human Research and a federal certificate of confidentiality was obtained to further protect the privacy and confidentiality of research participants. Participants received $20 for completing the baseline interview, $25 for the 6–month interview, and $30 for the 12–month interview. Additionally, those participants randomized to the hospital-based SEP received a $20 incentive for participating in an additional risk reduction education session. Participant recruitment and follow–up is illustrated in Figure 1.
FIGURE 1.
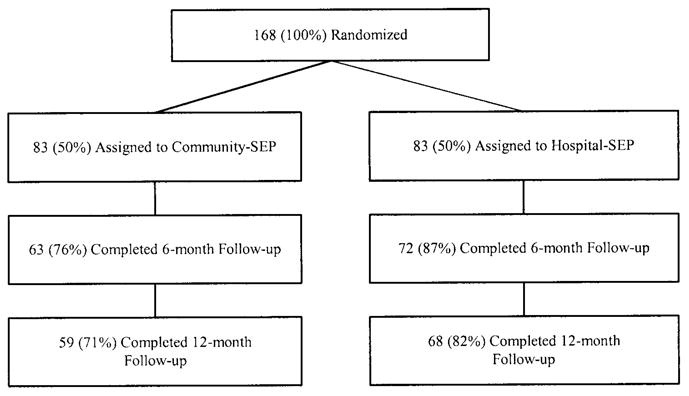
Participant assignment to intervention group and attrition
STUDY GROUPS
Community SEP
After completing the baseline interview, participants who were assigned to the community–SEP condition were given a pamphlet describing the 12 locations and hours of operation of these SEPs in the city and county of San Francisco that were operated by San Francisco AIDS Foundation HIV Prevention Project. In addition to providing sterile syringes, the community SEPs provided other HIV prevention supplies (i.e., bleach, distilled water, cotton, latex tourniquets, alcohol wipes, antibacterial cream, “cookers,” and condoms), and additional educational materials. Community SEPs gave 10 syringes as a starter kit and then a one–for–one exchange with no upper limit on the number of syringes that could be exchanged per visit. Community SEPs, however, did not provide education classes or referrals to SFGH for in-patient and outpatient services. In general, the community SEPs were open Monday through Saturday between 10 A.M. and noon and 7 P.M. to 9 P.M.
Hospital SEP
The hospital–based SEP was begun as a collaborative research program between the San Francisco AIDS Foundation HIV Prevention Project and researchers at the University of California, San Francisco. The San Francisco AIDS Foundation HIV Prevention Project also coordinated and performed the syringe exchange services, but in contrast to community SEPs, the hospital SEP was located at SFGH. In addition to the usual SEP activities, an additional HIV risk reduction education session and referrals to inpatient and outpatient services were provided. One week after the baseline interview, participants returned to the hospital for an additional HIV/AIDS education session. A research assistant, certified as an HIV counselor, conducted the 1–hour risk reduction educational session with each participant. The educational program covered (a) information on HIV disease and how it is transmitted; (b) behavioral strategies to avoid exposure to HIV; and (c) detailed instructions on safe self–injection practices including information on preparation for injection, choosing an injection site (hierarchy of safety for choosing injection sites), rotating injection sites, skin cleaning, use of a new syringe for every injection, use of clean water from a reliable source to prepare drugs, use of a new disinfected container (“cooker”) and a new filter (“cotton”) to prepare drugs, avoiding sharing of syringes, water, or drug preparation equipment. Hands–on demonstration on safe self–injection practices and printed educational materials were used in this session. In addition, the HIV counselor provided standardized instructions regarding the use of syringes (e.g., syringes are only intended for onetime single use, and that the use of sterile syringes is safer than reusing syringes). They were also issued an identification card to be presented during SEP visits.
Referrals to drug abuse treatment programs, medical care, and social service programs were also provided. The hospital SEP was open on Saturdays between noon and 2 P.M. Because of space and funding limitations of the hospital SEP, operation was restricted to one session per week. Research participants assigned to this condition received syringe exchange services for a 1–year period.
MEASURES
Participants were assessed with the Addiction Severity Index (McLellan et al., 1992), Texas Christian University (TCU) HIV/AIDS Risk Assessment (Camacho, Bartholomew, Joe, & Simpson, 1997), and Medical Outcomes Study SF–36 (Ware, 1996) at baseline and at 6- and 12-month follow-up. We also collected information on self–reported use of syringe exchange services in the past 30 days.
Addiction Severity Index (ASI)
The ASI is a widely used standardized instrument that provides assessments of problem severity in areas commonly affected by alcohol and drug abuse, including medical status, employment/financial support, alcohol and drug abuse, family/social functioning, legal problems, and psychiatric status (McLellan et al., 1992).
Texas Christian University AIDS Risk Assessment (TCU/ARA)
The TCU/ARA is a 40–item self–report instrument that assesses drug use and sexual risk behaviors as well as HIV testing history and attitudes and concerns about AIDS (Camacho et al., 1997).
MOS SF–36 Short–Form Health Survey (SF–36)
The SF–36 is a 36–item inventory designed to assess general health status. The multi–item scales measure eight areas of functioning: physical functioning, role limitations owing to physical health problems, bodily pain, general health, vitality (energy/fatigue), social functioning, role limitations owing to emotional problems, and mental health (psychological distress and psychological well–being) (Ware, 1996).
Scales are scored from 0 to 100, with higher scores indicating more positive health. Two summary measures, the Physical Component Summary (PCS) and Mental Component Summary (MCS) can be derived. The summary scores are reported as T scores, with a mean of 50 and standard deviation of 10 in the general U.S. population (Ware, Kosinski, & Keller, 1994).
SEP Use
At each follow up assessment participants’ self–reported SEP use, including use of the hospital and any other SEPs in the past 30 days was collected. We also separately tracked dates of hospital SEP use.
MEDICAL CARE UTILIZATION
Utilization of medical services was obtained from a review of computerized records from the SFGH’s administrative database. Medical service data were collected from baseline through the 12–month follow up. This electronic database provided information on the utilization of emergency, inpatient, and ambulatory care services received by the study participants from the San Francisco Department of Public Health Community Health Network, including services provided by SFGH. Emergency department and ambulatory care service use data included the service date, the clinic where the service was provided, International Classification of Diseases, (9th Rev.), Clinical Modification (ICD–9–CM) coded diagnoses, and the Common Procedural Terminology (CPT–4) codes of the services provided. For each inpatient admission, information was collected on the date of admission, length of stay, ICD–9–CM coded diagnoses, and which inpatient unit the patient was admitted to for each hospitalization. We examined three service utilization outcome variables: emergency department visits, inpatient admissions, and ambulatory care clinic visits. For each of the three service utilization variables, the total number of services (visits or admissions) received across the 12 months of the study was computed for each participant.
DATA ANALYSIS
In the first set of analyses, we examined the main outcome variables including injection practices, health status, and self–reported SEP use. We examined change between baseline and 12 months and whether or not these changes across time varied between study conditions. Specifically, we looked for significant intervention by time interactions. These differences were tested with a mixed-effects analysis of variance model using SAS PROC–MIXED.
In a second analysis, we sought to identify independent predictors of hospital SEP attendance (i.e., whether or not participants assigned to the hospital SEP attended at least one session) using logistic regression. Predictor variables were age, gender, ethnicity, needle risk index in the past 30 days, self–reported HIV status, SF–36 Physical and Mental Component Summary scales, and homelessness. Before building the final logistic regression models, we conducted exploratory analysis with univariate Pearson chi–square tests, and eliminated variables from consideration that did not meet a criterion of p ≤ .25, as suggested by Mickey and Greenland (1989). A model building strategy was used to arrive at parsimonious, final models. Specifically, variables were excluded if they did not contribute to the fit of the model according to log likelihood ratio statistics. Odds ratios (ORs) and 95% confidence intervals are reported for all variables included in the final model.
In a third analysis, Poisson regression models were used to examine the influence of SEP setting on service use outcome variables (i.e., frequency of emergency department visits, inpatient admissions, and ambulatory care visits). These regression equations also examined the influence of secondary variables as described above. Poisson regression models were used because the service utilization variables are counts, which are relatively rare events that tend to cluster around the value of 0 or 1, thus producing a positively skewed distribution. Poisson regression is more appropriate than least squares regression for this type of variable. The Poisson model estimates the relationship between the natural log of the count (visits or admissions) and the independent variables. Predictor variables were dichotomized (continuous variables were dichotomized at their median), and thus, the exponents of the parameters represent the percentage difference, compared to the reference group. For all statistical analyses we used SAS software, Version 8.0.
RESULTS
A total of 166 participants were randomized to the two intervention groups, community SEP (n = 83) and hospital SEP (n = 83). Table 1 displays summary statistics of the participants at study entry. The majority were White men who were unemployed and homeless. The mean age of participants was 40 (SD = 9.8), with a range of 19 to 63 years. Seventy percent of participants reported that heroin use was their major illicit drug use problem. At the 6–month follow–up, 81% (135) were assessed, and at the 12–month follow–up 78% (129) were assessed. Participant flow through the study is illustrated in Figure 1. Follow–up rates between conditions did not differ significantly at six (p = .07) or 12 months (p = .10). We also compared groups on their sociodemographic, substance use, and physical and mental health characteristics at baseline, and found no statistically significant differences.
TABLE 1.
Participant Characteristics by Group Assignment
| Variable | Community–SEP % (n = 83) | Hospital–SEP % (n = 83) |
|---|---|---|
| Gender—male | 77 | 77 |
| Ethnicity | ||
| White | 60 | 55 |
| African American | 20 | 23 |
| Latino/a | 16 | 18 |
| Other | 4 | 4 |
| Marital Status—married | 11 | 13 |
| Education—high school or less | 72 | 71 |
| Employed (full or parttime) | 11 | 5 |
| Yearly income less than $10,000 | 70 | 66 |
| Homeless | 66 | 69 |
| Mean (SD) | Mean (SD) | |
|
| ||
| Age (years) | 41 (8.99) | 40 (10.54) |
| ASI Medical | 0.6 (0.34) | 0.6 (0.30) |
| ASI Drug | 0.3 (0.12) | 0.3 (0.11) |
| ASI Psychiatric | 0.3 (0.28) | 0.3 (0.29) |
| SF–36 Physical Component Summary | 38.5 (11.29) | 39.4 (11.31) |
| SF–36 Mental Health Component Summary | 43.5 (13.56) | 44.9 (12.53) |
Note. SEP = syringe exchange program; ASI = Addiction Severity index; SF–36 = Short–Form Health Survey.
PRIMARY OUTCOMES
SEP condition did not influence risk behaviors, health status, or self–reported SEP program use. For these variables, there were no differences between conditions, and no statistically significant Intervention × Time interactions. More specifically, self–reported drug use risk behaviors did not differ between SEP conditions. Drug use risk behaviors reported by participants decreased over time, regardless of condition, F (2, 260) = 65.84, p < .0001. SF–36 scores increased over time for both conditions, F(2, 419) = 7.29, p < .001. Self–reported frequency of SEP use did not differ between conditions. From another perspective, no significant differences were found in the proportion of those reporting SEP use in the past 30 days by study condition. At the 6–month assessment point, 59% of participants assigned to the hospital–based SEP reported using syringe exchange in the past 30 days, whereas 52% of those assigned the comparison arm reported SEP use (p = .61). Similarly, the proportion of those reporting SEP use did not differ between the hospital SEP and community SEP groups at the 12–month assessment point (47% vs. 46%; p = .11).
PREDICTORS OF HOSPITAL SEP SERVICES
Table 2 presents distributions for service utilization variables. One hundred and two participants (61%) were treated in the emergency department during the 1–year follow up period. Thirty–four percent had at least one inpatient admission during the 12–month follow up and 99% were seen at least once in ambulatory care clinics.
TABLE 2.
Medical Service Use
| Types of Medical Care | 0 Visits | 1 Visit | 2–3 Visits | 4–5 Visits | 6–7 Visits | 8 or More Visits |
|---|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| Emergency department | 64 (39) | 30 (18) | 33 (20) | 14 (8) | 6 (3) | 19 (12) |
| Inpatient | 110 (66) | 27 (16) | 21 (13) | 5 (3) | 0 (0) | 3 (2) |
| Ambulatory | 1 (1) | 10 (6) | 24 (15) | 16 (10) | 14 (8) | 101 (60) |
We examined demographic and substance use–related characteristics associated with participation in the hospital SEP among those assigned to the hospital SEP. In univariate analyses, characteristics associated with using the hospital SEP were White race (p = .006), homelessness (p = .001), and risky drug use (p = .02), but in a multivariate analysis only homelessness significantly predicted syringe exchange program use: Persons who had housing were 5.03 times more likely to attend the hospital SEP (confidence interval [CI] = 1.84, 15.26).
PREDICTORS OF MEDICAL SERVICE USE
Table 3 presents the results of Poisson regression models estimating the effect of a number of demographic and substance use–related variables on emergency department use. HIV-positive participants had 61% fewer emergency department visits than those who were HIV-negative (CI = −75%, −38%). Participants with higher physical functioning had 24% fewer emergency department visits than those with lower functioning (CI = −37%, −8%).
TABLE 3.
Factors Associated with Medical Service Use Among Study Participants
| Coefficient | Standard Error | |
|---|---|---|
| Emergency department | ||
| HIV–positive | −0.943**** | 0.235 |
| SF–36 Physical Healtha | −0.269** | 0.097 |
| Inpatient | ||
| Male | 0.759** | 0.242 |
| Whiteb | −0.481** | 0.169 |
| Needle Risk Indexc | 0.476** | 0.171 |
| HIV–positive | −0.888* | 0.393 |
| SF–36 Physical Health | −1.354**** | 0.206 |
| SF–36 Mental Healthd | −0.446** | 0.169 |
| Study condition | 0.606**** | 0.178 |
| Ambulatory | ||
| Age (years)d | 0.360**** | 0.044 |
| Male | 0.232**** | 0.053 |
| White | −0.214**** | 0.041 |
| Homelesse | −0.281**** | 0.041 |
| Needle Risk Index | −0.145**** | 0.040 |
| HIV–positive | −0.645**** | 0.084 |
| SF–36 Physical Health | −0.357**** | 0.039 |
| SF–36 Mental Health | −0.279**** | 0.039 |
| Study condition | 0.198**** | 0.039 |
Note. SF–36 = MOS SF–36 Short–From Health Survey.
Entered in analyses as >46 versus ≤=46.
Entered in analyses as White versus all other ethnic groups.
Entered in analyses as high versus low risk.
Entered in analyses as >39 versus ≤=39.
Entered in analyses as homeless versus housed (i.e., house, apartment, halfway house, or residence in a therapeutic community, single room occupancy hotel, motel, jail, hospital).
p <.05.
p< .01.
p< .001.
p<.0001.
We also examined the correlation between demographic and substance use–related variables on inpatient medical admissions. Men had 114% more inpatient admissions than women (CI = 33%, 243%). Participants with higher risky needle use had 61% more inpatient admissions than those with lower risky needle use (CI = 15%, 125%). Persons assigned to the hospital SEP had 83% more inpatient admissions than those assigned to community SEPs (CI = 29%, 160%). White participants had 38% fewer inpatient admissions than non–White participants (CI = −56%, −14%). HIV-positive participants had 59% fewer inpatient admissions than HIV-negative participants (CI = −81%, −11%). Participants with higher physical health functioning had 74 % fewer inpatient admissions than those with lower functioning (CI = −83%, −62%). Similarly, participants with higher mental health functioning had 36% fewer inpatient admissions than those with lower functioning (CI = −54%, −11%).
In an analysis of ambulatory care visits, persons who were older than 40 years had 43% more ambulatory care visits than those who were younger (CI = 31%,56%). Men had 26.% more ambulatory care visits than women (CI = 14%,40%). Finally, those who were assigned to the hospital SEP had 22% more ambulatory care visits than those assigned to the Community SEPs (CI = 13%,32%). White participants had 19% fewer ambulatory care visits than non–White participants (CI = −25%, −13%). Homeless participants made 25% fewer ambulatory care visits compared to participants with stable housing (CI = −30%, −18%). Persons with higher risky drug use scores had 14% fewer ambulatory care visits than those with lower scores (CI = −20%, −16%). HIV-positive participants had 48% fewer ambulatory care visits than HIV-negative participants (CI = −56%, −38%). Those with higher physical health functioning had 30% fewer ambulatory care visits than those with lower functioning (CI = −35%, −24%). Persons who had higher mental health functioning demonstrated 24% fewer ambulatory care visits than those with lower functioning (CI = −30%, −18%).
DISCUSSION
This randomized trial compared the effectiveness of two syringe exchange program delivery models on injection practices and health outcomes. Participants reduced risky drug use in both conditions over time, suggesting that engagement or participation in syringe exchange programs may have been associated with reductions in risky drug use. These findings are consistent with previous studies showing that active participation in syringe exchange programs significantly reduces sharing of syringes and injection equipment (Hagan & Thiede, 2000; Vlahov et al., 1997). In addition, we did not find differences in the frequency of syringe exchange program use between settings, suggesting that the hospital SEP was not less convenient than community SEPs and that high rates of retention in hospital-based SEPs can be achieved. Despite differences in the hours of operation between programs, syringe exchange program participants used SEP services at comparable levels.
In both groups, we found that physical health functioning improved over time. Thus, syringe exchange program setting did not appear to differentially influence the health of these out–of–treatment IDUs. Regarding the impact of syringe exchange program setting on health service utilization, hospital SEP attendees used inpatient and ambulatory care services more frequently than those assigned to the community–SEP condition. One possibility is that the groups differed in health status in ways not detected by the SF–36. An alternative explanation for this finding is that the proximity of the hospital SEP to medical services may have reduced barriers to receiving needed care. The hospital SEP was located on hospital grounds, allowing participants to easily walk to outpatient clinics. In some cases study participants were escorted to outpatient clinics by SEP staff. Previous research has demonstrated that onsite delivery of health care is instrumental in increasing use of medical services as compared to referral to off-site care in community settings (Umbricht–Schneiter et al., 1994). Hence, health service delivery models that increase accessibility to health care services through co–located services may reduce obstacles in the decision to seek care.
A number of sociodemographic and substance use–related characteristics were significantly correlated with health service use among syringe exchange program attendees. Characteristics positively correlated with inpatient admissions were male gender and risky drug use. Men were admitted to inpatient services more frequently than women. It is possible that men were more likely to have chronic medical conditions that necessitated care. Alternatively, women may have been more likely to experience barriers to health care, and delayed seeking medical treatment because of these barriers. Women may be more reluctant to seek treatment when they are caring for children or ill family members because they may perceive these responsibilities as more important (Davidson et al., 1998). In other instances, drug-using women who have chronic medical conditions such as HIV or HCV may hide their disease as long as possible to protect their children against stigmatization (Davidson et al., 1998).
We also found that those engaging in higher risky drug use practices were admitted to inpatient care more frequently than those with lower risk scores. Illicit drug users who engage in risky drug use practices are at especially high risk for HIV and other injection drug use–related medical problems (Friedman, Jose, Deren, Des Jarlais, & Neaigus, 1995; Kerr et al., 2004; Masson et al., 2002). In fact, for the participants in this study, treatment of skin and soft–tissue infections accounted for the majority of their service use. Consistent with our findings for inpatient services, we found that men used ambulatory care services more frequently than women. Given that men made more contacts with ambulatory care clinics than women, strategies to engage women who are drug users in secondary and tertiary preventive health care may be needed. Policies that attempt to increase access to health care, enhance patients’ integration into the health care system, and engagement in longitudinal prevention services may lead to reductions in the use of high-cost emergency health care among illicit drug users (Laine, Lin, Hauck, & Turner, 2005). Additionally, persons who were over 40 years old used ambulatory care services more frequently than persons who were younger. Within injection drug-using populations, studies have shown that older people use more nonemergency health care than younger people (Fleishman et al., 2005). Future studies might compare health service use patterns of injection drug-using men and women, while considering characteristics of IDU populations as well as characteristics of the health service delivery system. Such findings might help to inform the broader issues of health care access among IDUs.
HIV-positive persons used fewer emergency, inpatient, and ambulatory care services than those who were negative. As a group, HIV-infected IDUs are less likely to be engaged in HIV primary care than non–IDUs and less likely to receive effective highly active antiretroviral therapy (HAART) (Solomon et al., 1998). An explanation for the less frequent use of ambulatory care services may be that IDUs are not engaged in HIV primary care because of clinicians concerns regarding nonadherence to HAART. On the other hand, the lower levels of service use among HIV-infected persons may reflect their decision to delay treatment. Other factors that may have influenced service use patterns among HIV-positive IDUs in this study include poor knowledge of available treatments, lack of belief in efficacy of antiretroviral therapy, and severe mental illnesses such as major depressive disorder, which may have reduced their motivation to seek needed medical care. It has been well established that much of the disparity in the health benefits of HAART among IDUs has been a consequence of decreased access to and receipt of potent antiretroviral combination therapies (Cunningham et al., 2000). This finding highlights the importance of identifying strategies to reduce health disparities attributed to lack of receipt of HAART among IDUs. Strategies to increase access to and utilization of HAART have included entry into drug treatment, abstinence, community outreach and referral, and provision of medical care at nontraditional sites such as syringe exchange (Molitor et al., 2005). For example, Altice, Springer, Buitrago, Hunt, and Friedland (2003) provided HAART to out–of–treatment IDUs using a mobile van at SEP sites and found that by 6 months the proportion whose HIV–1 RNA was below the limits of detection was 85%; 77% had no detectable levels by 9 months. Findings from this study demonstrate that health services linked to nontraditional settings such as SEPs may enhance access to HAART among out–of–treatment HIV-infected IDUs.
Within the hospital SEP condition, those who had stable housing were significantly more likely to use the hospital SEP. Homeless populations have a number of un-met service needs and frequent subsistence difficulty, which act as barriers to the receipt of regular health care (Gallagher, Andersen, Koegel, & Gelberg, 1997). Therefore, it is reasonable to suggest that conflicts between competing priorities and health care needs, a lack of transportation, the hospital SEP’s limited hours of operation, or other characteristics of the single site hospital SEP may have made it more difficult for homeless persons to participate in the program.
Limitations to these findings are also noted. First, participants in this study may differ from IDUs receiving services in other syringe exchange program settings in unknown ways. Subjects were recruited in the hospital emergency department and therefore may not be fully representative of all IDUs who might benefit from syringe exchange services. However, although most IDUs are not engaged in longitudinal preventive health care, most active injectors do in fact seek health care episodically in emergency departments facilitating generalizability to the majority of IDUs (French, McGeary, Chitwood, & McCoy, 2000; Laine et al., 2001). Our finding that fewer eligible women enrolled in the study than did eligible men may limit generalizabililty of the findings to women drug users; however, this finding highlights the need to develop effective strategies to engage female as well as male drug users in risk reducing interventions. The fact that most syringe exchange program attendees are not enrolled in substance abuse treatment at any given time enhances the generalizability of the study’s findings (Heimer, 1998). Furthermore, this study was conducted in a city that permitted syringe exchange programs to operate legally, thus increasing the generalizability of our findings to similar settings (e.g., New York, Seattle, WA). Second, this study focused on medical service use obtained through the public sector. It is generally recognized that this population obtains the vast majority of health care through the public health care system. We found that use of services outside of the public health care system was extremely limited; thus, medical service utilization data used in the present study likely reflect actual resource utilization. Third, the sample scored significantly lower than the normative sample on the physical and mental health functioning summary scales (Ware et al., 1994). These extremely low scores may explain the lack of group differences on these outcome measures. Alternatively, the lack of group differences may be due to insensitivity of the study instruments. Clinical observations of health status to supplement the interview data might have produced different results. Finally, it is possible that community–SEP participants received additional HIV risk reduction counseling from other settings, which may have accounted for the lack of group differences on risky injection drug use practices. It is also possible that the additional one session safe self–injection class that was provided for the hospital SEP group may not have been sufficient to change risk behaviors. Another possibility is that education alone may not be sufficient to change risky drug use behaviors (Madray & van Hulst, 2000). Therefore, more intensive interventions that both provide education and are demonstrated to result in risk reducing behavior change are needed.
IMPLICATIONS
The SEP setting did not influence the injection drug use practices or health status of this sample of out–of–treatment IDUs. However, participants enrolled in the hospital SEP used more ambulatory care services suggesting that the setting increased accessibility to needed outpatient services. Syringe exchange services alone are unlikely to eliminate risky drug use behaviors or related adverse health consequences. Providing linkages to needed services, such as active referrals to drug treatment may increase the likelihood that needed psychosocial services are received (Heimer, 1998). Additionally, providing primary care or specialty care at SEPs, such as treatment of skin and soft–tissue infections, may address unmet medical care needs and provide opportunities to engage these individuals in longitudinal preventive care services (Grau, Arevalo, Catchpool, & Heimer, 2002). Syringe exchange services that are integrated into public hospital settings may serve as a valuable strategy to engage hard to reach IDU populations in preventive care. Future studies should explore enhancements to hospital SEPs and their impact on drug use, health, and other psychosocial outcomes.
Acknowledgments
This work was supported by Grants K01DA00408 and P50DA09253 from the National Institute on Drug Abuse. The authors extend their thanks to the staff at the San Francisco AIDS Foundation HIV Prevention Project, San Francisco General Hospital Volunteer Center, San Francisco General Hospital clinical and research staff, and research participants for their participation in this project.
Contributor Information
Carmen L. Masson, Department of Psychiatry, University of California, San Francisco at San Francisco General Hospital
James L. Sorensen, Department of Psychiatry, University of California, San Francisco at San Francisco General Hospital
David C. Perlman, Department of Medicine, Beth Israel Medical Center, New York; the Center for Drug Use & HIV Research, National Development and Research Institutes Inc., New York; and Baron Edmond de Rothschild Chemical Dependency Institute, Beth Israel Medical Center, New York
Michael S. Shopshire, Department of Psychiatry, University of California, San Francisco at San Francisco General Hospital
Kevin L. Delucchi, Department of Psychiatry, University of California, San Francisco
TeChieh Chen, Department of Psychiatry, University of California, San Francisco at San Francisco General Hospital.
Karl Sporer, Department of Medicine, University of California, San Francisco at San Francisco General Hospital, San Francisco, CA.
Don Des Jarlais, Center for Drug Use & HIV Research, National Development and Research Institutes Inc., New York; and Baron Edmond de Rothschild Chemical Dependency Institute, Beth Israel Medical Center, New York.
Sharon M. Hall, Department of Psychiatry, University of California, San Francisco
References
- Altice F, Springer S, Buitrago M, Hunt D, Friedland G. Pilot study to enhance HIV care using needle exchange–based health services for out–of–treatment injecting drug users. Journal of Urban Health. 2003;80:416–426. doi: 10.1093/jurban/jtg053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Medical Anthropology. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Camacho LM, Bartholomew NG, Joe GW, Simpson DD. Maintenance of HIV risk reduction among injection opioid users: A 12 month posttreatment follow–up. Drug and Alcohol Dependence. 1997;47:11–18. doi: 10.1016/s0376-8716(97)00056-2. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Revised guidelines for HIV counseling, testing, and referral. Morbidity and Mortality Weekly Report. 2001;50:1–58. [PubMed] [Google Scholar]
- Commonwealth Department of Health and Ageing. Return on investment in needle and syringe programs in Australia. Canberra, Australia: Commonwealth of Australia, Publications Production Unit; 2002. [Google Scholar]
- Cunningham W, Markson L, Andersen RM, Crystal S, Fleishman J, Golin C, et al. Prevalence and predictors of highly active antiretroviral therapy use in patients with HIV infection in the United States. Journal of Acquired Immune Deficiency Syndromes. 2000;25:115–123. doi: 10.1097/00042560-200010010-00005. [DOI] [PubMed] [Google Scholar]
- Davidson AJ, Bertram SL, Lezotte DC, Marine W, Rietmeijer CA, Hagglund BB, et al. Comparison of health status, socioeconomic characteristics, and knowledge and use of HIV–related resources between HIV–infected women and men. Medical Care. 1998;36:1676–1684. doi: 10.1097/00005650-199812000-00005. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Marmor M, Paone D, Titus S, Shi Q, Perlis T, et al. HIV incidence among injecting drug users in New York City syringe–exchange programmes. The Lancet. 1996;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- Fleishman JA, Gebo KA, Reilly ED, Conviser R, Christopher MW, Todd KP, et al. Hosptial and outpatient health services utilization among HIV–infected adults in care 2000–2002. Medical Care. 2005;43(9 Suppl):40–52. doi: 10.1097/01.mlr.0000175621.65005.c6. [DOI] [PubMed] [Google Scholar]
- French MT, McGeary KA, Chitwood DD, McCoy CB. Chronic illicit drug use, health services utilization and the cost of medical care. Social Science and Medicine. 2000;50:1703–1713. doi: 10.1016/s0277-9536(99)00411-6. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Jose B, Deren S, Des Jarlais DC, Neaigus A. Risk factors for human immunodeficiency virus seroconversion among out–of–treatment drug injectors in high and low seroprevalence cities. American Journal of Epidemiology. 1995;142:864–874. doi: 10.1093/oxfordjournals.aje.a117726. [DOI] [PubMed] [Google Scholar]
- Gallagher TC, Andersen RM, Koegel P, Gelberg L. Determinants of regular source of care among homeless adults in Los Angeles. Medical Care. 1997;35:814–830. doi: 10.1097/00005650-199708000-00007. [DOI] [PubMed] [Google Scholar]
- Grau LE, Arevalo S, Catchpool C, Heimer R. Expanding harm reduction services through a wound and abscess clinic. American Journal of Public Health. 2002;92:1915–1917. doi: 10.2105/ajph.92.12.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan H, Thiede H. Changes in injection risk behavior associated with participation in the Seattle Needle–Exchange Program. Journal of Urban Health. 2000;77:369–382. doi: 10.1007/BF02386747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankins CA. Syringe exchange in Canada: Good but not enough to stem the HIV tide. Substance Use and Misuse. 1998;33:1129–1146. doi: 10.3109/10826089809062211. [DOI] [PubMed] [Google Scholar]
- Heimer R. Can syringe exchange serve as a conduit to substance abuse treatment? Journal of Substance Abuse Treatment. 1998;15:183–191. doi: 10.1016/s0740-5472(97)00220-1. [DOI] [PubMed] [Google Scholar]
- Kerr T, Wood E, Grafstein T, Ishida T, Shannon K, Lai C, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. Journal of Public Health. 2004;27:62–66. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- Kral AH, Bluthenthal RN. What is it about needle and syringe exchange programmes that make them effective for preventing HIV transmission? International Journal of Drug Policy. 2003;14:361–363. [Google Scholar]
- Laine C, Hauck WW, Gourevitch MN, Rothman J, Cohen A, Turner BJ. Regular outpatient medical and drug abuse care and subsequent hospitalization of persons who use illicit drugs. Journal of the American Medical Association. 2001;285:2355–2362. doi: 10.1001/jama.285.18.2355. [DOI] [PubMed] [Google Scholar]
- Laine C, Lin Y, Hauck WW, Turner BJ. Availability of medical care services in drug treatment clinics associated with lower repeated emergency department use. Medical Care. 2005;43:985–995. doi: 10.1097/01.mlr.0000178198.79329.89. [DOI] [PubMed] [Google Scholar]
- Laufer FN. Cost–effectiveness of syringe exchange as an HIV prevention strategy. Journal of Acquired Immune Deficiency Syndromes. 2001;28:273–278. doi: 10.1097/00042560-200111010-00012. [DOI] [PubMed] [Google Scholar]
- MacDonald M, Law M, Kaldor J, Hales J, Dore GJ. Effectiveness of needle exchange and syringe exchange programmes for preventing HIV transmission. International Journal of Drug Policy. 2003;14:353–357. [Google Scholar]
- Madray H, van Hulst Y. Reducing HIV/AIDS high–risk behavior among injection drug users: peers vs. education. Journal of Drug Education. 2000;30:205–211. doi: 10.2190/1DWM-D9WA-22R1-70Q0. [DOI] [PubMed] [Google Scholar]
- Masson CL, Sorensen JL, Batki SL, Okin RL, Delucchi KL, Perlman DC. Medical service use and financial charges among opioid users at a public hospital. Drug and Alcohol Dependence. 2002;66:45–50. doi: 10.1016/s0376-8716(01)00182-x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mickey J, Greenland S. A study of the impact of confounder selection criteria on effect estimation. American Journal of Epidemiology. 1989;129:125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- Molitor F, Kuenneth C, Waltermeyer J, Mendoza M, Aguirre A, Brockmann K, et al. Linking HIV–infected persons of color and injection drug users to HIV medical and other services: The California Bridge Project. AIDS Patient Care and STDs. 2005;19:406–412. doi: 10.1089/apc.2005.19.406. [DOI] [PubMed] [Google Scholar]
- Parsons J, Hickman M, Turnbull PJ, McSweeney T, Stimson GV, Judd A, et al. Over a decade of syringe exchange: Results from 1997 UK survey. Addiction. 2002;97:845–850. doi: 10.1046/j.1360-0443.2002.00128.x. [DOI] [PubMed] [Google Scholar]
- Perlman D, Gourevitch M, Trinh C, Salomon N, Horn L, Des Jarlais D. Cost–effectiveness of tuberculosis screening and observed preventive therapy for active drug injectors at a syringe exchange program. Journal of Urban Health. 2001;78:550–567. doi: 10.1093/jurban/78.3.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley ED, Safaeian M, Strathdee SA, Marx MA, Huettner S, Beilenson P, et al. Comparing new participants of a mobile versus a pharmacy–based needle exchange program. Journal of Acquired Immune Deficiency Syndromes. 2000;24:57–61. doi: 10.1097/00126334-200005010-00010. [DOI] [PubMed] [Google Scholar]
- Rockwell R, Des Jarlais DC, Friedman SR, Perlis TE, Paone D. Geographic proximity, policy and utilization of syringe exchange programmes. AIDS Care. 1999;11:437–442. doi: 10.1080/09540129947811. [DOI] [PubMed] [Google Scholar]
- Solomon L, Stein M, Flynn C, Schuman P, Schoenbaum E, Moore J, et al. Health services use by urban women with or at risk for HIV–1 infection: The HIV epidemiological research study (HERS) Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998;17:253–261. doi: 10.1097/00042560-199803010-00011. [DOI] [PubMed] [Google Scholar]
- Umbricht–Schneiter A, Ginn DH, Pabst KM, Bigelow GE. Providing medical care to methadone clinics: Referral vs onsite care. American Journal of Public Health. 1994;84:207–210. doi: 10.2105/ajph.84.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW, Foreman RK, Junge B, Vlahov D. Needle–exchange participation, effectiveness, and policy: Syringe relay, gender, and the paradox of public health. Journal of Urban Health. 2001;78:340–349. doi: 10.1093/jurban/78.2.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Junge B, Brookmeyer R, Cohn S, Riley E, Armenian H, et al. Reductions in high–risk drug use behaviors among participants in the Baltimore needle exchange program. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1997;16:400–406. doi: 10.1097/00042560-199712150-00014. [DOI] [PubMed] [Google Scholar]
- Ware JE. The MOS 36–item short–form health survey (SF–36) In: Dickey LISB, editor. Outcomes assessment in clinical practice. Baltimore: Williams & Wilkins; 1996. p. xxx. [Google Scholar]
- Ware JE, Kosinski M, Keller SD. SF–36 physical and mental health summary scales: A user’s manual. Boston: New England Medical Center, Health Assessment Lab; 1994. [Google Scholar]


