Abstract
OBJECTIVE
To determine the frequency of potentially inappropriate colonoscopy in Medicare beneficiaries in Texas and examine variation across providers and geographic regions.
METHODS
This retrospective cohort study used 100% Medicare claims data for Texas and a 5% sample from the U.S. from 2000–2009. We identified Medicare beneficiaries aged ≥ 70 who received a colonoscopy from 10/01/2008–9/30/2009. A colonoscopy was classified as screening in the absence of diagnoses suggesting an indication for the procedure. A screening colonoscopy was considered potentially inappropriate on the basis of age of the patient or occurrence too soon after a normal colonoscopy. The percentage of patients undergoing a potentially inappropriate screening colonoscopy was estimated for each colonoscopy provider and Hospital Service Area.
RESULTS
A large percentage of colonoscopies performed in older adults were potentially inappropriate: 23% for the overall Texas cohort, 10% in adults aged 70–75, 39% in adults aged 76–85, and 25% in adults aged ≥ 86. There was considerable variation across the 797 providers in the percent of colonoscopies performed that were potentially inappropriate. In a multilevel model including patient sex, race/ethnicity, comorbidity, education, and urban/rural residence, 73 providers had percentages significantly above the mean (24%), ranging from 29%–45% and 119 providers had percentages significantly below the mean, ranging from 7%–19%. The providers with percentages significantly above the mean were more likely to be surgeons, graduates of U.S. medical schools, medical school graduates before 1990, and higher volume providers compared to those significantly below the mean. Provider rankings were fairly stable over time (2006–07 vs. 2008–09). There was also geographic variation across Texas and the U.S., with percentages ranging from 13.3% to 34.9% in Texas.
CONCLUSIONS
Many of the colonoscopies provided to older adults may be inappropriate. Receipt of potentially inappropriate colonoscopy depends in part on where patients live and what provider they see.
Keywords: aged, colonoscopy, mass screening, Medicare
INTRODUCTION
Colonoscopy has become the dominant modality for colorectal cancer screening.1 Underuse of colonoscopy screening has been well-documented;1–3 however, there is also growing evidence of overuse.4–7 We found that 23.5% of Medicare patients who had a negative screening colonoscopy underwent a repeat screening examination fewer than 7 years later.7 Repeat colonoscopy within 10 years after a negative examination represents overuse based on current guidelines.8, 9 Screening colonoscopy performed in the oldest age groups also may represent overuse according to guidelines from the US Preventive Services Task Force (USPSTF) and American College of Physicians (ACP).8, 9
Complications from colonoscopy are increased in older populations.10 Moreover, competing causes of mortality with advancing age shift the balance between life-years gained and colonoscopy risks.11, 12 Colonoscopy screening capacity is limited,13, 14 and the overuse of screening colonoscopy drains resources that could otherwise be used for the unscreened at-risk population.15
The decision to undergo colonoscopy screening is ultimately up to the patient. However, providers and health care systems may exert considerable influence on patient decision-making and adherence to screening recommendations.1, 16–18 Provider preferences and practice setting may influence colorectal screening rates.19, 20 State-level variation has been reported in the use of colorectal cancer screening procedures, suggesting the presence of local practice patterns.21
The purpose of this study was to determine the frequency of potentially inappropriate screening colonoscopy in Medicare beneficiaries. We selected beneficiaries who had a colonoscopy in 2008–2009 and classified the procedure as screening or diagnostic. A screening colonoscopy was considered inappropriate on the basis of age of the patient or occurrence too soon after a previous normal colonoscopy. The use of 100% Texas Medicare data allowed us to examine variation among providers and across geographic regions.
METHODS
Data
The primary data source for this study was the 100% Medicare claims and enrollment files for Texas (2000–2009). The Denominator File contained patients’ demographic and enrollment characteristics. The Outpatient Standard Analytic Files and the Carrier Files were used to identify outpatient facility services and physician services. Inpatient hospital claims data were identified in the Medicare Provider Analysis and Review Files. We built a crosswalk between National Provider Identifier (NPI) (2008–2009) and Unique Provider Identification Number (2006–2007) on Medicare claims and linked to the American Medical Association (AMA) Physician File to obtain physician data. Medicare claims were linked to 2000 U.S. Census data to obtain zip code-level aggregate information on area education.
We also used claims and enrollment data from a 5% random national sample of Medicare beneficiaries to examine geographic variation across the United States. Cohort selection criteria and variable definitions were identical to those for Texas data.
Cohort
We identified Medicare beneficiaries aged 70 and older who received a complete colonoscopy between 10/01/2008 and 9/30/2009 (n=119,477). We limited the index procedures to patients age 70 and older to allow for at least 5 years of Medicare claims data to identify prior colonoscopies. Colonoscopies were identified by the following Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes: CPT 44388–89, 44392–94, 45378, 45380, 45382–85; HCPCS G0105, G0121; ICD-9-CM 45.23, 45.25, 45.27, 45.41–43, 48.36. Colonoscopies with CPT modifier codes of 52 and 53 were considered incomplete and excluded.
We excluded beneficiaries who without continuous enrollment in parts A and B or who were enrolled in an HMO in the previous seven years (n=21,976). We excluded beneficiaries with a history of colon cancer, inflammatory bowel disease, or colon resection in the seven years preceding the colonoscopy (n=6,553). We also excluded colonoscopies performed during an inpatient hospital admission or the same day as an emergency room visit (n=9,410). Finally, we restricted the cohort to Texas residents who received a colonoscopy from a Texas provider, yielding a final sample of 74,681 beneficiaries. We constructed a second cohort of beneficiaries who received colonoscopy from 10/1/2006–9/30/2007, in order to examine the stability over time in estimates of the provider-level performance. That cohort was constructed exactly like the 2008/2009 cohort and included 73,922 beneficiaries.
Variables
Inappropriate Colonoscopy
We classified the 2008/2009 colonoscopy as inappropriate if it was: 1) an early repeat colonoscopy without clear indication in subjects aged 70–75 or 2) contrary to USPSTF age-based screening recommendations. The USPSTF recommends against routine screening in adults aged 76–85 years and against any screening in adults older than 85 years.8 In the USPSTF suggestions for practice, physicians are counseled to provide screening to 76–85 year olds only if other considerations support providing the service in an individual patient, and physicians are counseled to discourage screening in patients older than 85 years.8
The identification of screening colonoscopy is complicated by the fact that few colonoscopies are submitted using the screening code.7, 22 It is estimated that approximately two-thirds of colonoscopies are performed for colorectal cancer screening purposes;22 however, only 14.6% of all Medicare colonoscopies in 2007–2008 included a screening code on the claim. Consistent with prior research,7 we examined the diagnoses on the colonoscopy claim and on inpatient and outpatient claims in the 3 months prior to the procedure to determine whether the colonoscopy was performed without clear indication other than screening. We reasoned that a diagnostic colonoscopy would produce relevant diagnoses on the colonoscopy claim or on claims in the 3 months prior to the procedure. Patients who did not have any indications for a diagnostic colonoscopy were considered to have had a screening colonoscopy.
The following were considered indications for diagnostic colonoscopy: (1) a claim for barium enema or abdominal CT in the 3 months prior to colonoscopy; or (2) a diagnosis on the colonoscopy claim and on any inpatient or outpatient claim in the prior 3 months for: anemia, gastrointestinal bleeding, constipation, diarrhea, abdominal pain, ischemic bowel disease, irritable bowel syndrome, bowel habits change, hemorrhoid, weight loss, or other conditions where a colonoscopy might plausibly be indicated (see Appendix for full list).7
Colonoscopies that did not meet the above criteria for a diagnostic procedure were considered screening colonoscopies and labeled as ‘potentially inappropriate’ if performed in adults aged 76 and older. We modified criterion 2 of the above algorithm to require a diagnosis consistent with an indication for colonoscopy on either the colonoscopy claim or any claim in the prior 3 months. Colonoscopies that did not meet these modified criteria for a diagnostic procedure were labeled as ‘probably inappropriate’ screening colonoscopies if performed in adults aged 76 and older.
To define early repeat colonoscopy in subjects aged 70–75, we examined Medicare claims data from 01/01/2001 to 9/30/2008 to identify previous procedures. If beneficiaries had multiple previous colonoscopies, we selected the latest procedure. Beneficiaries who had undergone a negative colonoscopy23 and who did not have any indications for colonoscopy in 2008/2009 were classified as having had an early repeat colonoscopy. These colonoscopies were labeled as ‘potentially inappropriate’ or ‘probably inappropriate’ based on the above algorithms. Early repeat colonoscopies in those with a family history of colorectal cancer (ICD-9 diagnosis of V16.0) were classified as appropriate.
Colonoscopy Provider
We linked patients to the performing provider using the NPI on the colonoscopy claim. Medicare Health Care Financing Administration provider specialty codes were used to categorize physician specialty as gastroenterology, generalist, surgery, and other.
Provider Volume
For each physician, we calculated the volume of colonoscopies performed on Medicare enrollees from 10/1/2008–9/30/2009. Physician volume was stratified into quartiles: < 65, 65–115, 116–175, and >175.
Patient Characteristics
Patient demographics obtained from the Denominator file included age, sex, and race. A Charlson comorbidity score was estimated using inpatient and outpatient claims files from the year prior to the 2008/2009 colonoscopy.24 The percentage of residents in the zip code with fewer than 12 years of education was used as a surrogate for patient education. Area of residence was classified as metropolitan, non-metropolitan, or rural. Place of service was classified as hospital-based facility, office, or ambulatory surgical center.
Geographic Area
Hospital Service Areas (HSAs), described in the Dartmouth Atlas of Health Care,25 were used to assess geographic variation across 208 areas in Texas. Hospital referral regions25 (HRRs) were used to assess geographic variation across 306 regions in the United States.
Analysis
Descriptive statistics were used to describe the percent of colonoscopies performed in Medicare patients in 2008/2009 that were potentially or probably inappropriate, stratified by patient and provider characteristics. Two-level hierarchical generalized linear models (HGLM) adjusted for patient and provider characteristics and clustering of patients within provider were used to identify independent predictors of potentially inappropriate colonoscopy.
Two-level HGLMs provided estimates for each provider of the percent of colonoscopies performed that were potentially inappropriate, after adjusting for patient sex, race/ethnicity, comorbidity, education, urban/rural, and place of service. The percent of Medicare beneficiaries whose colonoscopy was potentially inappropriate was estimated for each HSA in Texas using an unconditional two-level HGLM with HSA as a random effect, and for each HRR in the U.S. using an unconditional two-level HGLM with HRR as a random effect.
RESULTS
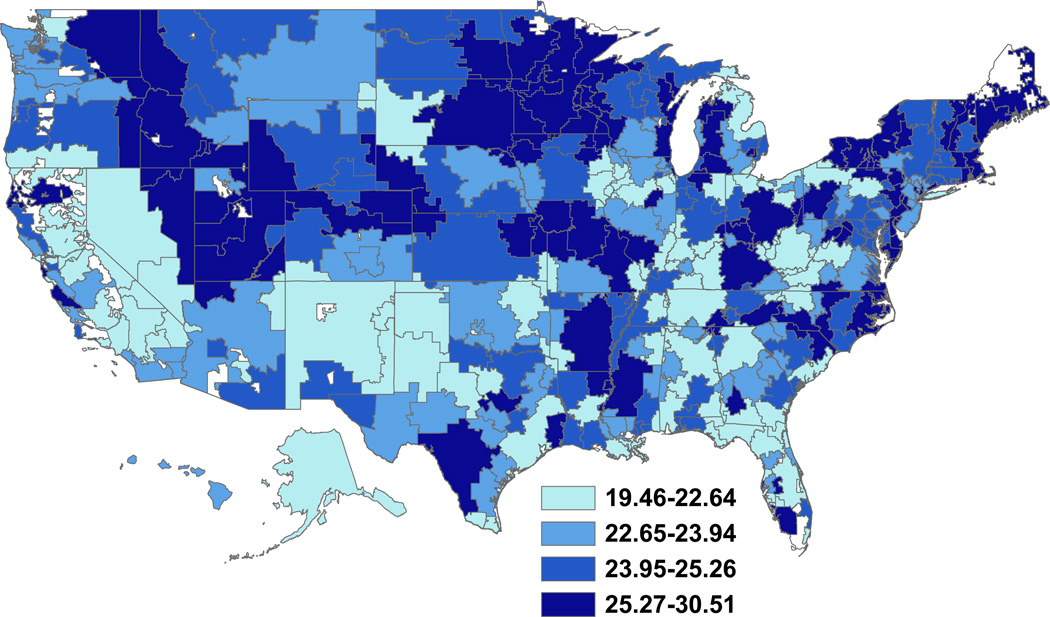
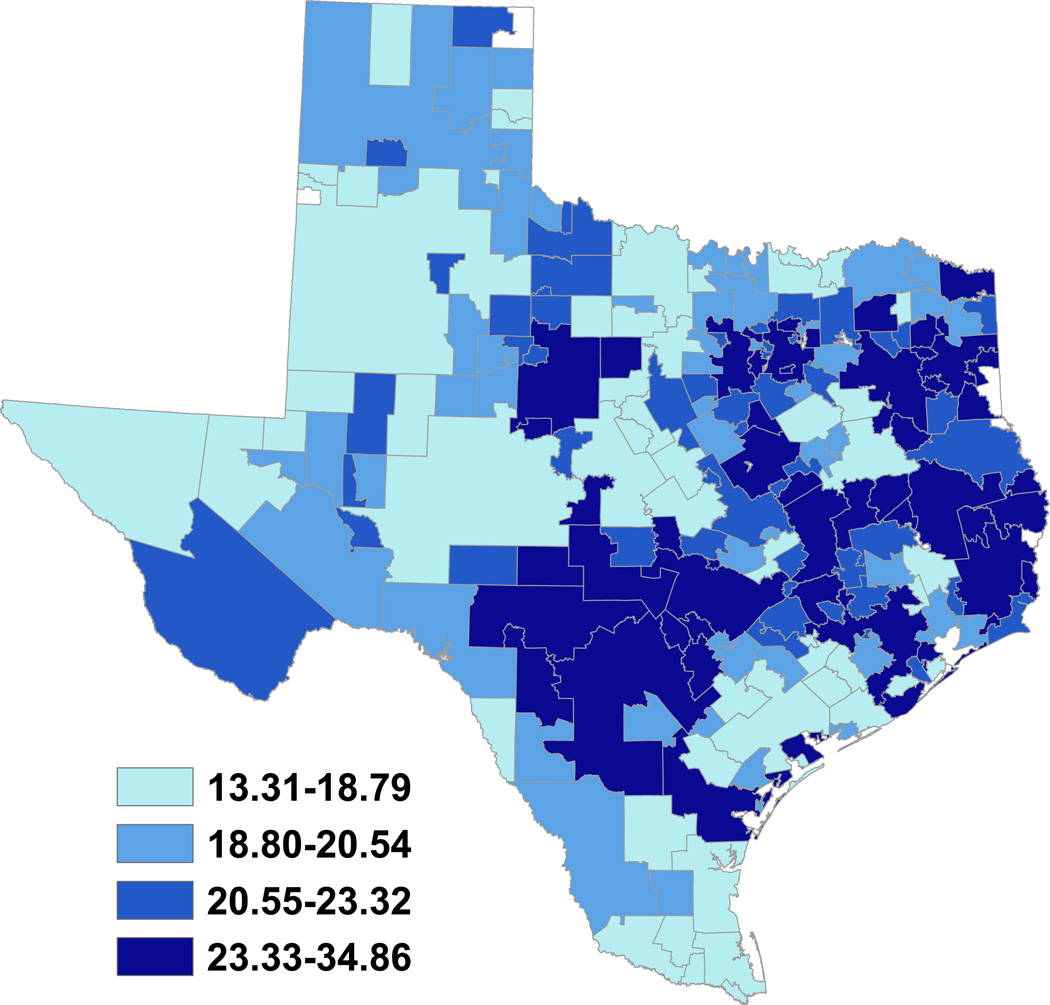
Figure 1 is a map presenting the percentage of potentially inappropriate colonoscopies in a 5% sample of Medicare recipients 70 and older (n = 56,566) nationally by HRR. The overall percent for the U.S. was 23.5%, and varied from 19.5% to 30.5% by HRR. Figure 2 shows similar variations across HSAs in Texas. The overall percent for Texas was 23.4%, and varied from 13.3% to 34.9% of colonoscopies. An analysis using the algorithm for ‘probably inappropriate’ colonoscopy produced similar results for both maps (not shown).
Figure 1.
For each of the 306 Hospital Referral Regions in the United States, the percent of colonoscopies performed in Medicare beneficiaries aged 70 and older in 2008/2009 that were potentially inappropriate. Results based on 5% national Medicare claims data.
Figure 2.
For each of the 208 Hospital Service Areas in Texas, the percent of colonoscopies performed in Medicare beneficiaries aged 70 and older in 2008/2009 that were potentially inappropriate. Results based on 100% Texas Medicare claims data.
We next examined the role of the colonoscopy provider in inappropriate colonoscopy. We restricted our analyses to 100% Medicare data for Texas, because 100% data allows for substantial number of colonoscopies for each provider and stable estimates.
The cohort included 74,681 Medicare beneficiaries aged 70 and older who underwent a colonoscopy in Texas in 2008/2009. Table 1 presents the percentages of the colonoscopies that were potentially or probably inappropriate, stratified by patient and provider characteristics. Overall, 23.4% of colonoscopies were potentially inappropriate and 18.9% were probably inappropriate. Approximately 10% of colonoscopies performed on patients aged 70–75 were potentially inappropriate, which for this age group indicates an early repeat colonoscopy. Notably, around 39% of colonoscopies performed on patients aged 76–85 and 25% performed on those aged 86 and older were potentially inappropriate. This means that of the 1,042,790 Medicare beneficiaries in Texas, approximately 0.9% of adults aged 70–75, 2.7% of adults aged 76–85, and 0.6% of adults aged 86 and older underwent a potentially inappropriate colonoscopy in 2008/2009.
Table 1.
Characteristics of Texas Medicare patients aged 70 and older who underwent colonoscopy in 2008–2009
| Variables | Number of patients | Percent with potentially inappropriate colonoscopy* |
Percent with probably inappropriate colonoscopy** |
|---|---|---|---|
| Total cohort | 74,681 | 23.4 | 18.9 |
| Age at time of 2008/2009 colonoscopy | |||
| 70–75 | 37,710 | 9.9 | 7.9 |
| 76–85 | 32,947 | 38.8 | 31.7 |
| 86 and older | 4, 024 | 24.9 | 17.3 |
| Sex | |||
| Male | 32,745 | 25.5 | 21.2 |
| Female | 41,936 | 21.9 | 17.1 |
| Race/ethnicity | |||
| White | 66,795 | 23.9 | 19.2 |
| Black | 4,213 | 20.0 | 16.0 |
| Hispanic | 2,432 | 18.9 | 14.2 |
| Other | 1,241 | 21.5 | 17.7 |
| Number of comorbidities | |||
| 0 | 14,638 | 28.3 | 23.6 |
| 1 | 19,215 | 27.4 | 22.3 |
| 2 | 16,384 | 25.3 | 20.5 |
| ≥ 3 | 24,444 | 16.2 | 12.3 |
| Education (% of residents in zip code with > 12 years) | |||
| < 9 | 18,762 | 26.3 | 21.8 |
| 9–18 | 16,686 | 24.9 | 20.0 |
| 18–26 | 18,627 | 23.0 | 18.6 |
| ≥ 26 | 16,885 | 19.8 | 15.3 |
| Urban/rural | |||
| Metropolitan | 58,320 | 24.0 | 19.4 |
| Non-metropolitan | 14,944 | 21.4 | 16.9 |
| Rural | 1,412 | 22.4 | 18.1 |
| Place of service | |||
| Hospital-based facility | 43,545 | 21.1 | 16.2 |
| Ambulatory surgical center | 30,404 | 26.7 | 22.6 |
| Office | 732 | 26.7 | 22.5 |
| Specialty of colonoscopist | |||
| Gastroenterology | 59,116 | 23.2 | 18.8 |
| Generalist | 3,655 | 22.2 | 16.5 |
| Surgery | 11,106 | 25.0 | 20.2 |
| Other | 804 | 22.5 | 14.1 |
| Volume of colonoscopist† | |||
| 1– 64 | 19,052 | 19.1 | 14.5 |
| 65–115 | 18,531 | 22.8 | 18.4 |
| 116–175 | 18,592 | 23.9 | 19.2 |
| 175–366 | 18,506 | 28.1 | 23.6 |
| Training | |||
| U.S. trained | 48,172 | 25.9 | 21.2 |
| Trained outside U.S. | 20,821 | 19.2 | 14.8 |
For adults ages 70–75, inappropriate colonoscopy was defined as an early repeat colonoscopy without clear diagnostic indication. For adults ages 76–85 and 86 and older, inappropriate colonoscopy was defined as any colonoscopy without a clear diagnostic indication.
Defined based on an algorithm that required relevant diagnoses on the colonoscopy claim and in the prior 3 months
Defined based on an algorithm that required relevant diagnoses on the colonoscopy claim or in the prior 3 months
For each physician, volume was calculated as the total number of colonoscopies performed on Medicare enrollees from 10/1/2008–9/30/2009
In the multivariate model in Table 2, female sex, black race, increased comorbidity, higher education, and residence in a non-metropolitan or rural area were associated with lower odds of potentially inappropriate colonoscopy. Patients who received a colonoscopy in an ambulatory surgical center or office setting had higher odds of potentially inappropriate colonoscopy. Patients who received a colonoscopy from higher volume providers, generalists or surgeons, and U.S. trained physicians had higher odds of potentially inappropriate colonoscopy. A multivariate model using ‘probably inappropriate’ colonoscopy as the outcome produced substantively equivalent results (not shown).
Table 2.
Multilevel multivariate logistic regression analyses of patient and provider characteristics associated with potentially inappropriate colonoscopy, 100% Texas Medicare claims, 2008–2009*
| Model 1 (n = 65,553) | ||
|---|---|---|
| Variables | Adjusted odds ratio |
95% CI |
| Sex | ||
| Male | (ref) | |
| Female | 0.85 | 0.82, 0.88 |
| Race/ethnicity | ||
| White | (ref) | |
| Black | 0.91 | 0.83, 0.99 |
| Hispanic | 1.08 | 0.96, 1.22 |
| Other | 0.92 | 0.79, 1.07 |
| Number of comorbidities | ||
| 0 | (ref) | |
| 1 | 0.99 | 0.94, 1.05 |
| 2 | 0.91 | 0.86, 0.96 |
| ≥ 3 | 0.54 | 0.51, 0.57 |
| Education (% of residents in zip code with > 12 years) | ||
| < 9 | (ref) | |
| 9–18 | 0.95 | 0.90, 1.01 |
| 18–26 | 0.91 | 0.86, 0.97 |
| ≥ 26 | 0.87 | 0.82, 0.93 |
| Urban/rural | ||
| Metropolitan | (ref) | |
| Non-metropolitan | 0.86 | 0.81, 0.91 |
| Rural | 0.83 | 0.72, 0.96 |
| Place of service | ||
| Hospital-based facility | ||
| Ambulatory surgical center | 1.22 | 1.15, 1.29 |
| Office | 1.58 | 1.21, 2.06 |
| Volume of colonoscopist† | ||
| <65 | (ref) | |
| 65–115 | 1.23 | 1.13, 1.35 |
| 116–175 | 1.35 | 1.22, 1.49 |
| >175 | 1.63 | 1.45, 1.82 |
| Specialty of colonoscopist | ||
| Gastroenterology | (ref) | |
| Generalist | 1.27 | 1.10, 1.47 |
| Surgery | 1.27 | 1.15, 1.39 |
| Other | 0.86 | 0.59, 1.25 |
| Training | ||
| U.S. trained | (ref) | |
| Trained outside U.S. | 0.78 | 0.72, 0.84 |
‘Potentially inappropriate’ defined based on an algorithm that required relevant diagnoses on the colonoscopy claim and in the prior 3 months. For adults ages 70–75, inappropriate colonoscopy was defined as an early repeat colonoscopy without clear diagnostic indication. For adults ages 76–85 and 86 and older, inappropriate colonoscopy was defined as any colonoscopy without a clear diagnostic indication. An analysis using the algorithm for ‘probably inappropriate’ colonoscopy produced similar results.
For each physician, volume was calculated as the total number of colonoscopies performed on Medicare enrollees in 2008–2009; analyses were restricted to providers with ≥ 20 colonoscopies.
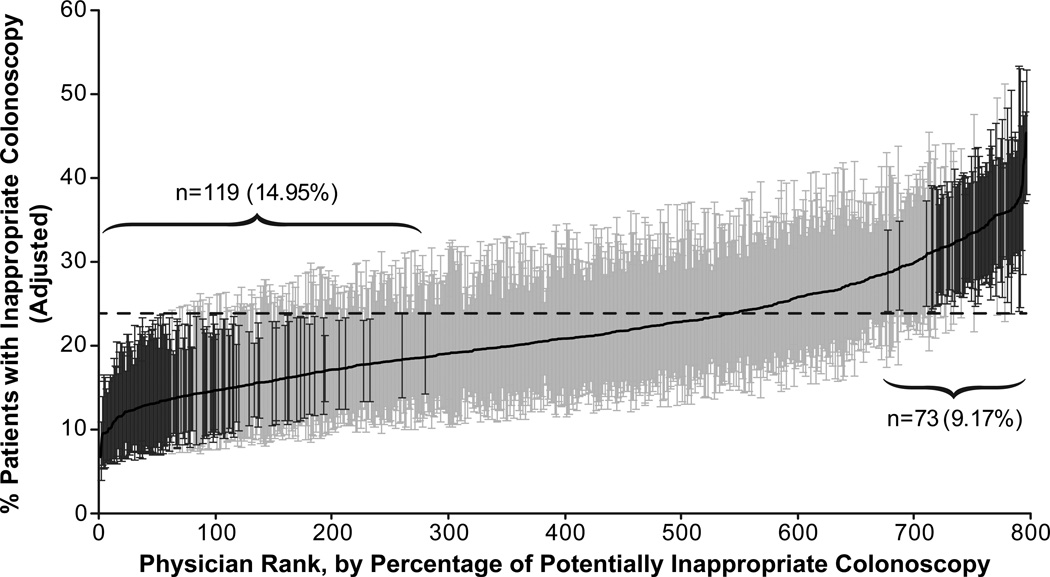
Figure 3 presents a cumulative ranking of providers by percent of colonoscopies performed that were potentially inappropriate, generated from a multilevel model adjusting for patient characteristics. The Intraclass Correlation Coefficient (ICC) for this model was 6.0%, indicating that 6.0% of the variance in whether a patient undergoing colonoscopy received a potentially inappropriate colonoscopy was explained by the provider. Seventy-three providers had percentages significantly above the mean (23.9%), ranging from 28.7%–45.5% and 119 providers that had percentages significantly below the mean, ranging from 6.7%–18.6%. The high and low percentage providers differed, with the high percentage group containing more surgeons, more U.S. medical school graduates, and fewer recent graduates (Table 3). The volume of colonoscopies performed per year was significantly higher among providers with a high percentage of inappropriate colonoscopy (175.5 vs. 99.2, p < 0.0001). A model using ‘probably inappropriate’ colonoscopy as the outcome produced an ICC of 7.6%. In addition, the results for Figure 3 and Table 3 were very similar to those reported above.
Figure 3.
For each of the 797 Texas colonoscopy providers, the adjusted percent of colonoscopies performed in Medicare beneficiaries aged 70 and older in 2008/2009 that were potentially inappropriate. The analysis was restricted to providers with ≥ 20 colonoscopies. The estimates were adjusted for patient sex, race/ethnicity, comorbidity, education, and urban/rural residence in a multilevel model. 95% confidence intervals are shown, and colonoscopists with adjusted percentages significantly different from the mean are indicated by a dark line. 119 colonoscopists were significantly below the mean, and 73 were significantly above the mean.
Table 3.
Comparison of characteristics of colonoscopy providers with high and low percentages of potentially inappropriate colonoscopy
| Variables | Physicians with low percentage of inappropriate colonoscopy (n = 119)* |
Physicians with high percentage of inappropriate colonoscopy (n=73)* |
P value |
|---|---|---|---|
| Sex | |||
| Male | 94 (87.8) | 69 (97.2) | 0.03 |
| Female | 13 (12.2) | 2 (2.8) | |
| Specialty | |||
| Gastroenterology | 95 (89.6) | 55 (77.5) | 0.04 |
| Surgery | 9 (8.5) | 15 (21.1) | |
| Generalist | 2 (1.9) | 1 (1.4) | |
| Year of medical school graduation | |||
| <1980 | 15 (14.3) | 22 (28.2) | <0.0001 |
| 1980–<1990 | 16 (15.2) | 27 (34.6) | |
| 1990–<2000 | 43 (41.0) | 27 (34.6) | |
| 2000+ | 31 (29.5) | 2 (2.6) | |
| Location of medical school | |||
| United States | 57 (53.3) | 66 (93.0) | <0.0001 |
| Outside of United States | 50 (46.7) | 5 (7.0) | |
| Colonoscopy volume (mean, s.d.) | 99.2 ± 59.1 | 175.5 ± 81.1 | <0.0001 |
Note: Physician information was available from the American Medical Association file for 107 physicians in the low group and 71 physicians in the high group.
‘Potentially inappropriate’ defined based on an algorithm that required relevant diagnoses on the colonoscopy claim and in the prior 3 months. For adults ages 70–75, inappropriate colonoscopy was defined as an early repeat colonoscopy without clear diagnostic indication. For adults ages 76–85 and 86 and older, inappropriate colonoscopy was defined as any colonoscopy without a clear diagnostic indication.
Analyses restricted to providers with ≥ 20 colonoscopies from 10/1/2008–9/30/2009
We also examined the stability over time of colonoscopist rankings in percentage of potentially inappropriate colonoscopies performed. We identified 687 colonoscopists who performed colonoscopies in two time periods: 10/1/2008–9/3/2009, and 10/1/2006–9/30/2007. We then ranked them by the percent of potentially inappropriate colonoscopies performed in each period. The rankings were fairly stable over time (Spearman’s rho = 0.69, p <0.0001). For example, of the 174 colonoscopists in the highest quartile of percentage of inappropriate colonoscopies in 2006–07, 89.1% of them were in the highest (63.2%) or second highest (25.9%) quartiles in 2008–09. Similarly, of those 169 colonoscopists in the lowest quartile in 2006–07, 85.2% were in the lowest (58.6%) or next lowest (26.6%) quartile in 2008–09. Similar results were observed when using ‘probably inappropriate’ colonoscopy as the outcome.
DISCUSSION
Overall, 23% of colonoscopies performed in Medicare beneficiaries ages 70 and older in 2008/2009 in Texas and across the U.S. were potentially inappropriate due to age-based screening recommendations or previous screening. We observed geographic and provider-level variation in potentially inappropriate colonoscopy. For some physicians, more than 30% of the colonoscopies they performed on Medicare patients in 2008/2009 were potentially inappropriate. Physician rankings were relatively stable over time. Approximately 6.0% of the variation in our outcome was attributable to the physician. Previous studies examining the role of the provider in explaining variations in practice behavior have generally reported comparable ICCs.26–29
Throughout this report we have used the terms “potentially inappropriate” and “probably inappropriate” colonoscopy. It is impossible using claims data to determine whether any given colonoscopy on a specific patient was appropriate or inappropriate. What claims data can provide is an analysis of patterns, how the level of potentially inappropriate colonoscopies varies by provider and geographic region. We made the assumption that colonoscopies performed without clear diagnostic indication were done for screening purposes rather than for evaluating symptoms. We reasoned that a diagnostic colonoscopy would produce relevant diagnoses on the colonoscopy claim and in the three months prior to the procedure. An alternative approach would be to identify patients with a charge for screening colonoscopy as opposed to diagnostic colonoscopy. However, only 14.6% of all Medicare colonoscopies in 2007–2008 included a screening code on the claim, even though it is estimated that nearly two-thirds of colonoscopies are performed for screening purposes.22
The USPSTF colorectal cancer screening guidelines specify age limits for routine screening based on a targeted systematic evidence review12 and decision analytic modeling analysis11 showing that screening in adults older than 75 years produced a gain in life-years that was small compared to the risks of screening. The ACP also recently issued a guidance statement recommending that clinicians stop screening in adults over 75 years old.30 The American College of Gastroenterology, American Cancer Society, US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology do not address age limits for discontinuing screening.31
Surgeons were overrepresented in the group of providers with significantly higher percentages of potentially inappropriate colonoscopies. It is possible that surgeons were actually performing surveillance colonoscopies on colon cancer survivors, and that those were misclassified as inappropriate screening colonoscopies. However, our look-back period searching for any diagnoses or procedures indicative of colon cancer was 5–7 years in all cases. Colonoscopy accounts for 25% of clinical time and total charges in the practices of colorectal surgeons,32 and it is estimated that surgeons perform one-third of screening colonoscopies in the United States.14
Physician recommendation is a key factor affecting patient adherence to screening guidelines.1, 18, 33–35Colonoscopists often recommend screening colonoscopy and polyp surveillance at shorter intervals than stipulated in national guidelines.15, 36–38 Legitimate clinical considerations and patient or referring physician request may prompt colonoscopists to perform colonoscopy at shorter intervals. The evidence supporting a 10-year interval is substantial but indirect.39 There is evidence that the progression of neoplasia to colorectal cancer may occur more quickly in older patients.40 Other reasons for potentially inappropriate colonoscopy screening may include poor communication between colonoscopists and primary care physicians,17 disagreement with recommended guidelines, ignorance about the findings of prior endoscopy, and financial incentives. Finally, misperceptions regarding cancer screening by patients and physicians may lead to inappropriate use of colonoscopy.41, 42
Considerable geographic variation in rates of colonoscopy and flexible sigmoidoscopy has also been reported at the state level in the United States21 and in Canada.43 Local physician practice patterns or supply may contribute to geographic variation in screening rates.2, 3 Regional variations in Medicare spending and medical practice have been well-documented in the United States, and evidence suggests that variations are due to the quantity of medical services, rather than differences in population health or socioeconomic status.44
The cohort of providers in this study was limited to Texas. We needed 100% Medicare data to assess variation among providers, and we cannot obtain that for the entire country. Texas is a state with recognized geographic variation in health care costs and outliers in utilization patterns;45 therefore, results may not be generalizable to other states or the nation as a whole. However, we also found geographic variation throughout the country when we examined 5% national Medicare data (Figure 1). Using administrative data, we were unable to determine the appropriateness of screening for any individual patient. This limitation is most relevant to adults aged 76–85 because other considerations may have supported providing the service in these patients. Patient preference also may influence the use of screening colonoscopy in this age group. We limited the cohort to patients age 70 and older to allow for at least 5 years of Medicare claims data. We were unable to capture any colonoscopies performed prior to Medicare eligibility at age 65; therefore, our estimates of early repeat colonoscopy are underestimates for the 70–75 age group. We were also unable to determine whether patients had a procedure to remove adenomatous polyps prior to 2000 or prior to age 65.
Inappropriate use of colonoscopy results in higher Medicare expenditures, involves unnecessary risk for older patients, and represents a substantial proportion of endoscopist workload, consuming resources that could be used more effectively. Public education campaigns on appropriate screening colonoscopy may reduce unnecessary testing and increase available screening capacity.
ACKNOWLEDGMENT
This research was supported by the following: RP101207 CPRIT (Cancer Prevention and Research Institute of Texas) Comparative Effectiveness Research on Cancer in Texas (CERCIT), K05-CA134923, K07 CA130983, and UL1TR000071- UTMB Clinical and Translational Science Award.
Footnotes
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Dr. Sheffield had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors have no conflicts of interest or financial disclosures.
REFERENCES
- 1.Holden DJ, Harris R, Porterfield DS, et al. Enhancing the use and quality of colorectal cancer screening. Evid Rep Technol Assess (Full Rep) 2010 Feb;(190):1–195. v. [PMC free article] [PubMed] [Google Scholar]
- 2.Benarroch-Gampel J, Sheffield KM, Lin YL, Kuo YF, Goodwin JS, Riall TS. Colonoscopist and Primary Care Physician Supply and Disparities in Colorectal Cancer Screening. Health Serv Res. 2012 Jun;47(3):1137–1157. doi: 10.1111/j.1475-6773.2011.01355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singal AK, Lin YL, Kuo YF, Riall T, Goodwin JS. Primary Care Physicians and Disparities in Colorectal Cancer Screening in the Elderly. Health Serv Res. 2012 Jun 20; doi: 10.1111/j.1475-6773.2012.01433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walter LC, Lindquist K, Nugent S, et al. Impact of age and comorbidity on colorectal cancer screening among older veterans. Ann Intern Med. 2009 Apr 7;150(7):465–473. doi: 10.7326/0003-4819-150-7-200904070-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher DA, Galanko J, Dudley TK, Shaheen NJ. Impact of comorbidity on colorectal cancer screening in the veterans healthcare system. Clin Gastroenterol Hepatol. 2007 Aug;5(8):991–996. doi: 10.1016/j.cgh.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Fisher DA, Judd L, Sanford NS. Inappropriate colorectal cancer screening: findings and implications. Am J Gastroenterol. 2005 Nov;100(11):2526–2530. doi: 10.1111/j.1572-0241.2005.00322.x. [DOI] [PubMed] [Google Scholar]
- 7.Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF. Overuse of Screening Colonoscopy in the Medicare Population. Arch Intern Med. 2011 May 9; doi: 10.1001/archinternmed.2011.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Screening for colorectal cancer. U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008 Nov 4;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 9.Qaseem A, Denberg TD, Hopkins RH, Jr, et al. Screening for colorectal cancer: a guidance statement from the American College of Physicians. Ann Intern Med. 2012 Mar 6;156(5):378–386. doi: 10.7326/0003-4819-156-5-201203060-00010. [DOI] [PubMed] [Google Scholar]
- 10.Warren JL, Klabunde CN, Mariotto AB, et al. Adverse events after outpatient colonoscopy in the Medicare population. Ann Intern Med. 2009 Jun 16;150(12):849–857. W152. doi: 10.7326/0003-4819-150-12-200906160-00008. [DOI] [PubMed] [Google Scholar]
- 11.Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008 Nov 4;149(9):659–669. doi: 10.7326/0003-4819-149-9-200811040-00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008 Nov 4;149(9):638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]
- 13.Seeff LC, Manninen DL, Dong FB, et al. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the United States? Gastroenterology. 2004 Dec;127(6):1661–1669. doi: 10.1053/j.gastro.2004.09.052. [DOI] [PubMed] [Google Scholar]
- 14.Brown ML, Klabunde CN, Mysliwiec P. Current capacity for endoscopic colorectal cancer screening in the United States: data from the National Cancer Institute Survey of Colorectal Cancer Screening Practices. Am J Med. 2003 Aug 1;115(2):129–133. doi: 10.1016/s0002-9343(03)00297-3. [DOI] [PubMed] [Google Scholar]
- 15.Krist AH, Jones RM, Woolf SH, et al. Timing of repeat colonoscopy: disparity between guidelines and endoscopists' recommendation. Am J Prev Med. 2007 Dec;33(6):471–478. doi: 10.1016/j.amepre.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 16.Klabunde CN, Lanier D, Breslau ES, et al. Improving colorectal cancer screening in primary care practice: innovative strategies and future directions. J Gen Intern Med. 2007 Aug;22(8):1195–1205. doi: 10.1007/s11606-007-0231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheridan SL, Harris RP, Woolf SH. Shared decision making about screening and chemoprevention. a suggested approach from the U.S. Preventive Services Task Force. Am J Prev Med. 2004 Jan;26(1):56–66. doi: 10.1016/j.amepre.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 18.Subramanian S, Klosterman M, Amonkar MM, Hunt TL. Adherence with colorectal cancer screening guidelines: a review. Prev Med. 2004 May;38(5):536–550. doi: 10.1016/j.ypmed.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA. 2005 Jul 27;294(4):473–481. doi: 10.1001/jama.294.4.473. [DOI] [PubMed] [Google Scholar]
- 20.O'Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage: gaps in colorectal cancer screening among Medicare beneficiaries. Arch Intern Med. 2005 Oct 10;165(18):2129–2135. doi: 10.1001/archinte.165.18.2129. [DOI] [PubMed] [Google Scholar]
- 21.Cooper GS, Koroukian SM. Geographic variation among Medicare beneficiaries in the use of colorectal carcinoma screening procedures. Am J Gastroenterol. 2004 Aug;99(8):1544–1550. doi: 10.1111/j.1572-0241.2004.30902.x. [DOI] [PubMed] [Google Scholar]
- 22.Chao A, Connell CJ, Cokkinides V, Jacobs EJ, Calle EE, Thun MJ. Underuse of screening sigmoidoscopy and colonoscopy in a large cohort of US adults. American Journal of Public Health. 2004 Oct;94(10):1775–1781. doi: 10.2105/ajph.94.10.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh A, Kuo YF, Riall TS, Raju GS, Goodwin JS. Predictors of Colorectal Cancer Following a Negative Colonoscopy in the Medicare Population. Digest Dis Sci. 2011 Nov;56(11):3122–3128. doi: 10.1007/s10620-011-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Wennberg JE, Cooper MM. The Dartmouth Atlas of Health Care 1998. Chicago, IL: American Hospital Publishing, Inc.; 1998. [PubMed] [Google Scholar]
- 26.Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician "report cards" for assessing the costs and quality of care of a chronic disease. JAMA. 1999 Jun 9;281(22):2098–2105. doi: 10.1001/jama.281.22.2098. [DOI] [PubMed] [Google Scholar]
- 27.Sixma HJ, Spreeuwenberg PM, van der Pasch MA. Patient satisfaction with the general practitioner: a two-level analysis. Med Care. 1998 Feb;36(2):212–229. doi: 10.1097/00005650-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Cowen ME, Strawderman RL. Quantifying the physician contribution to managed care pharmacy expenses: a random effects approach. Med Care. 2002 Aug;40(8):650–661. doi: 10.1097/00005650-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Beaulieu MD, Blais R, Jacques A, Battista RN, Lebeau R, Brophy J. Are patients suffering from stable angina receiving optimal medical treatment? QJM. 2001 Jun;94(6):301–308. doi: 10.1093/qjmed/94.6.301. [DOI] [PubMed] [Google Scholar]
- 30.Qaseem A, Denberg TD, Hopkins RH, et al. Screening for Colorectal Cancer: A Guidance Statement From the American College of Physicians. Annals of Internal Medicine. 2012 Mar 6;156(5) doi: 10.7326/0003-4819-156-5-201203060-00010. 378-U209. [DOI] [PubMed] [Google Scholar]
- 31.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008 May;134(5):1570–1595. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Kann BR, Margolin DA, Brill SA, et al. The importance of colonoscopy in colorectal surgeons' practices: results of a survey. Dis Colon Rectum. 2006 Nov;49(11):1763–1767. doi: 10.1007/s10350-006-0654-7. [DOI] [PubMed] [Google Scholar]
- 33.Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult U.S. population. Cancer. 2004 May 15;100(10):2093–2103. doi: 10.1002/cncr.20276. [DOI] [PubMed] [Google Scholar]
- 34.Wee CC, McCarthy EP, Phillips RS. Factors associated with colon cancer screening: the role of patient factors and physician counseling. Prev Med. 2005 Jul;41(1):23–29. doi: 10.1016/j.ypmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Coughlin SS, Thompson T. Physician recommendation for colorectal cancer screening by race, ethnicity, and health insurance status among men and women in the United States, 2000. Health Promot Pract. 2005 Oct;6(4):369–378. doi: 10.1177/1524839905278742. [DOI] [PubMed] [Google Scholar]
- 36.Saini SD, Nayak RS, Kuhn L, Schoenfeld P. Why don't gastroenterologists follow colon polyp surveillance guidelines?: results of a national survey. J Clin Gastroenterol. 2009 Jul;43(6):554–558. doi: 10.1097/MCG.0b013e31818242ad. [DOI] [PubMed] [Google Scholar]
- 37.Rossi F, Sosa JA, Aslanian HR. Screening colonoscopy and fecal occult blood testing practice patterns: a population-based survey of gastroenterologists. J Clin Gastroenterol. 2008 Nov-Dec;42(10):1089–1094. doi: 10.1097/MCG.0b013e3181599bfc. [DOI] [PubMed] [Google Scholar]
- 38.Lieberman D. Progress and challenges in colorectal cancer screening and surveillance. Gastroenterology. 2010 Jun;138(6):2115–2126. doi: 10.1053/j.gastro.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 39.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009 Mar;104(3):739–750. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 40.Brenner H, Hoffmeister M, Stegmaier C, Brenner G, Altenhofen L, Haug U. Risk of progression of advanced adenomas to colorectal cancer by age and sex: estimates based on 840,149 screening colonoscopies. Gut. 2007 Nov;56(11):1585–1589. doi: 10.1136/gut.2007.122739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wegwarth O, Schwartz LM, Woloshin S, Gaissmaier W, Gigerenzer G. Do physicians understand cancer screening statistics? A national survey of primary care physicians in the United States. Annals of Internal Medicine. 2012 Mar 6;156(5):340–349. doi: 10.7326/0003-4819-156-5-201203060-00005. [DOI] [PubMed] [Google Scholar]
- 42.Schwartz LM, Woloshin S, Fowler FJ, Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004 Jan 7;291(1):71–78. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- 43.Schultz SE, Vinden C, Rabeneck L. Colonoscopy and flexible sigmoidoscopy practice patterns in Ontario: a population-based study. Can J Gastroenterol. 2007 Jul;21(7):431–434. doi: 10.1155/2007/817810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003 Feb 18;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 45.Gawande A. The cost conundrum: What a Texas town can teach us about health care. The New Yorker. 2009 [Google Scholar]