Abstract
Objective:
The objective of this study is to examine the effect of a cognitive, behavioral stress management module of Sudarshan Kriya (SK) and P on levels of serum cortisol and pain among the women suffering from advanced stage breast cancer.
Materials and Methods:
Participants (n = 147) were screened and randomized to receive standard care (n = 69) versus standard along with SK and Pranayam (P) intervention (n = 78) imparted in one 18 hrs workshop spread during 3 days. Participants were expected to practice it at home 20 min daily as adjuvant to standard pharmacological treatment for pain.
Results:
There was a significant difference in blood cortisol levels after 3 months of practice of SK and P. Mean blood levels in the intervention arm were 341.2 ng/ml against 549.2 ng/ml in the control arm (P ≤ 0.002). Pain perception in comparison to control arm reduced by 3 points in SK and P arm on 0-10 verbal scale of pain.
Conclusion:
SK and P is an effective intervention in reducing stress and pain among advance stage patients of breast cancer.
Keywords: Cancer, Pain, Pranayam, Stress, Sudarshan kriya, Yoga
INTRODUCTION
Data derived from the National Cancer Registry Program of India, other Indian registries, the International Agency for Research on Cancer, and the United states National Cancer Institute Surveillance, Epidemiology, and End Results Program show average annual cancer incidence rates in India ranged from 7.2/100,000/year to 31.3/100,000/year for female breast. Comparative rates in the US for female breast cancer are 86.6 for blacks and 96.4 for whites. Overall, about 50-55% of breast cancer cases are detected in late (III and IV) stage in India; in contrast to the US where 15% cancer is diagnosed at late stage.[1]
In late stages, pain and stress become imperative symptom in most of the breast cancer patients. Most of the modern treatment modalities used to manage pain and stress in such terminal cases are less than satisfactory. There is neurophysiological basis for the modulating effect of the central nervous system on the perception of pain with a clearly identified somatic origin.[2] Apart from theoretical consideration, experimental behavioral stress management module (CBSM) have been evaluated in pain management and evidence shows the effectiveness of Yoga (Y), psychotherapy, and relaxation techniques. A number of studies have recently been published that identified the association between neuropathic pain and health-related quality-of life. The findings have important implications and suggest that a biopsychosocial (as opposed to a primarily biomedical) approach would be appropriate for understanding and treating neuropathic pain.[3]
A study analyzed the risk factors that predispose women to chronic symptoms related breast cancer. A questionnaire was sent to 569 women who had undergone modified radical mastectomies with axillary evacuation or breast resection with axillary evacuation. Pain, paresthesias and strange sensations were reported by half of the patients. The chronic pain slightly affected the daily lives of about 50% of the patients and moderately or more of about 25% of the patients. Patients with chronic pain were significantly younger and had larger primary tumors. The highest incidence of pain was reported by patients who had had both radio- and chemotherapy. Surgical complications and post-operative radiotherapy and chemotherapy increase the risk of chronic pain and other symptoms. Modifications in the treatment protocol and preclusion are recommended by this study from Finland in order to minimize chronic treatment-related symptoms.[4],[5]
Another study which reported symptom profile after 1 year of surgery finds 80% of the women had treatment-related symptoms in the breast scar region and virtually all patients had symptoms. Several studied have provided positive impact of yoga meditation modulating perception of pain with a clearly identified somatic origin; however, such studies are lacking from India.[5]
As part of Detect Clinical Epidemiological Study in USA, the frequency and associated problem of co morbid depression with a wide range of somatic illness were studied (n = 51,000) in patients seeking primary care. The association of depression with pain related chronic disorder (odd ratio [OR]: 1.5) was pronounced. Since, there has been demonstrable link of pain depression and stress in chronic disorders. It is the hypothesis whether by altering psychological component; somatic components of pain can be estimated using biologic markers. Hence, this study evaluated standardized set of regimen of Sudarshan Kriya (SK) and Pranayam (P).
The impact of SK and P has been evaluated in various chronic medical conditions like Diabetes, addiction, depression, anxiety, and stress.[6],[7],[8],[9],[10],[11] However, somatic symptom like pain has been tested for its impact for the first time. SK and P have been shown enhancing beta and alpha waves on electroencephalography indicating relaxed alertness,[12] increasing natural killer cells in cancer patients,[13] lowering blood lactate levels,[7] boost antioxidant defense, inducing relaxation, lowering anxiety and also to alter the gene expression by up-regulation of anti-apoptotic genes and pro-survival genes.[10]
MATERIALS AND METHODS
The study take account of stress biochemical marker serum cortisol and verbal scale of pain in a randomized clinical trial in which blinding is performed at program level since independent team generated random allocation numbers, separate staff imparted allocation in to control versus intervention arm by opening opaque envelopes containing allocation information in the subsequent recruitments. Blinding is followed at the blood sample collection, processing, testing, and analysis levels. Separate team worked on these components and used only codes, which were broken at the time of the final analysis by statistician team.
Sample size was determined on the basis of studies,[14],[15] showing depression and pain relationship (odd ratio 4.8). Considering 90% of advance stage cancer patients complain pain and assuming 20% lost to follow-up and non-compliance, standard sample size formula on N query package found 75 participants in each arm (total 150 participants) to get 30% difference in outcome measures. After getting ethical approval from institutional ethical committee and registering trial, recruitment of the staff, and training of staff took place. Training was given on randomization, data collection methods, entry in EPI-6tm package, collection of blood samples, and delivery of samples to laboratory, processing, standardization of processes under expert supervision. Role and duties of all stakeholders were defined.
Inclusion criteria
Women who are suffering from breast cancer stage IIb, III and IV, completed standard treatment of cancer by radiotherapy, chemotherapy, and surgery and now in the follow-up period for pain management, age ranging from 35 years to 60 years, Karnofsky score is above 70. Out of 185 participants screened 38 were excluded for various reasons (severe mental illnesses such as Catatonic/melancholic depression, n = 2, schizophrenia or hysteria, n = 1, using other form of alternative medicine/process of yogdhyan (n = 8) and Karnofsky score below 70, n = 17, unable to comply for a follow-up visit schedule/do not provide consent, n = 10). Data collection was started in April, 2011 and continued until January 2013. Comorbid condition other than severe mental illness were not excluded; hence 15% (n = 22) of the patients had high blood pressure, diabetes spread equally in control and intervention arm.
Weekly follow-up was carried out for enhancing regular practice. Weekly phone reminders, E-mails were used. Participants were asked to record practice, their time and day when they have any complaints did the practice of intervention. This information was retrieved for pre-coded performa during 3 monthly visits of the patients.
RESULTS
A total of 147 participants fulfilled the inclusion criteria, provided informed consent and underwent randomization into two arms. Arm-A (SK and P level-1) along with regular treatment while Arm B was on regular treatment. World Health Organization ladder of Nonsteroidal anti-inflammatory drugs (first, second generation) and morphine group of medicines with and without surgical intervention and counseling were part of regular treatment in both arms.
Under the intervention arm, adjuvant SK and P training components included teachings for self-awareness, how to do Ujjayi breath and Bhastrika parnayama, rhythmic breathing of SK under the supervision of trained yoga teachers. After the 18 h contact program spread in 3 days’ time, participants in the Arm A were narrated 20 min package of these steps for routine practice at home on a daily basis. One of the family members was imparted responsibility to look after the regularity of practice and report problems to the research team, if any.
After recruitment, the intervention in the form of 18 h workshop was organized once the group of 20-25 participants was cumulated.
Baseline information for both groups was collected before any intervention [Figure 1]. It was on income, education, occupation, social support, and transport and was collected in the predesigned and pre-tested questionnaire. Interpretation of pain perception was filled on verbal pain scale. For blood samples, the morning fasting 10 ml venous blood in the supine position for routine hemogram, liver, and kidney function tests and specific testes related to study-Serum Cortisol was collected and processed same morning. The samples were collected on the same time of the day in all the participants at 8.00 am-9.00 am after fasting overnight, since Cortisol levels tend to change according to diurnal variation. Samples were stored at-80 degree until slot of 30 samples was available to run standard tests to estimate serum cortisol levels.[16]
Figure 1.
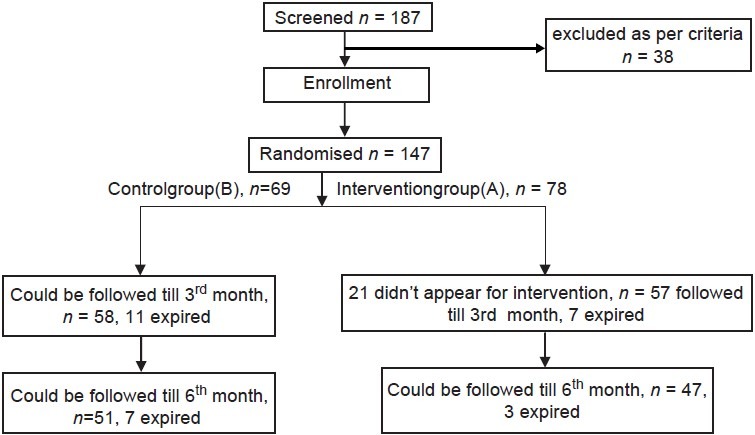
Experimental design, flow diagram
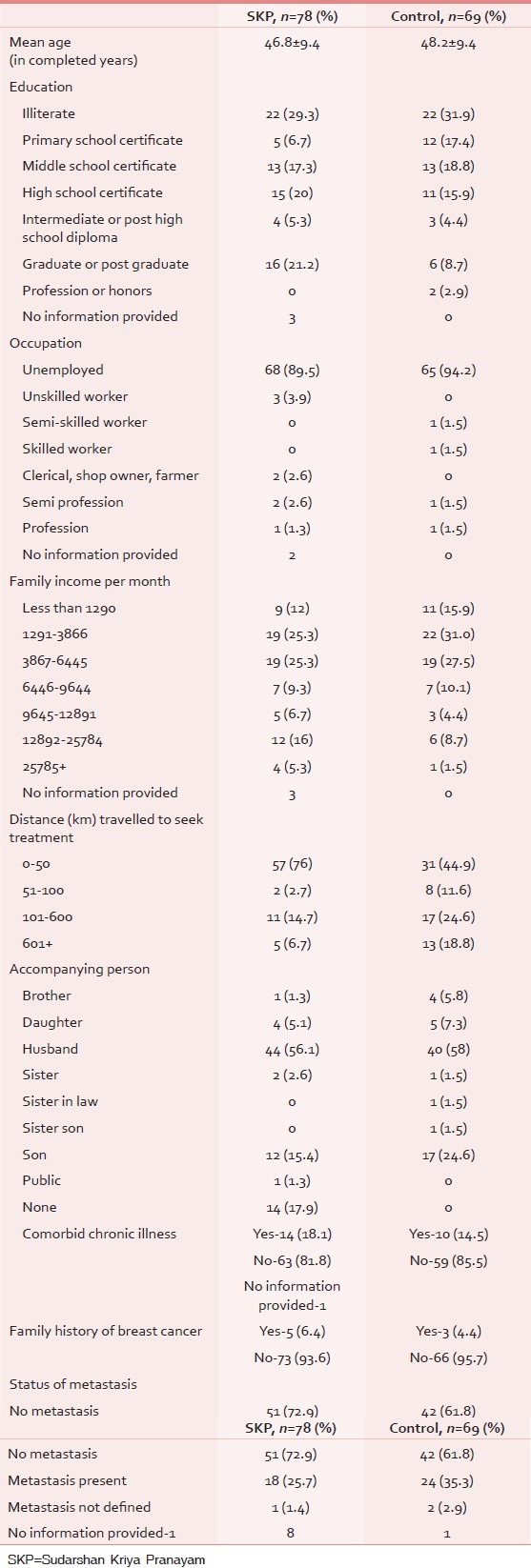
Demographic profile of the participants from education, occupation and family income point of view was found distributed equally with minor differences in few categories. Like more graduates (21.2 %) in intervention arm in comparison to 8.7% graduates in control arm. Family income wise slight more high income was observed in intervention arm. For the distance travelled to seek treatment it was found more in control arm. Accompanying person in both the group were majorly spouses of the patients. Co-morbidities like blood pressure, gastritis were found similar in both the arms at baseline. Family history of breast cancer was present in 4.4 to 6.4% of all the participants. Metastasis in bone was present in 35.3% of control and 25.7% of intervention arm [Table 1].
Table 1.
Demographic profile at baseline
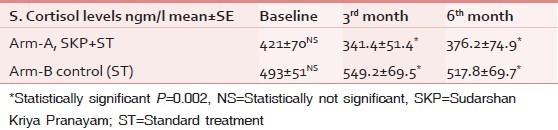
The S. Cortisol fasting levels in both the arms were found with non significant statistical difference at baseline for both intervention and control arms respectively (421 ± 70 vs 493 ± 51 nmg/l). It was found significantly reduced in the intervention arm in the serum of participants at 3rd month's visit (341.4 ± 51.4 vs. 549.2 ± 69.5 nmg/l) and 6th month's visit (376.2 ± 74.9 vs. 517.8 ± 69.7 nmg/l) in comparison to control arm [Table 2].
Table 2.
Status of cortisol levels at baseline, 3rd and 6th months of the follow-up
Regarding compliance, all the participants were complaint in their visits on scheduled date, however only 78% of intervention group showed regular practice at home for what was taught in SK&P training workshop.
Pain perception on verbal scale of 0-10 showed increasing pains with time, but the average weighted line demonstrated the difference of 3 points at 3rd month visit and 6th month visit in SKP intervention arm [Figure 2].
Figure 2.
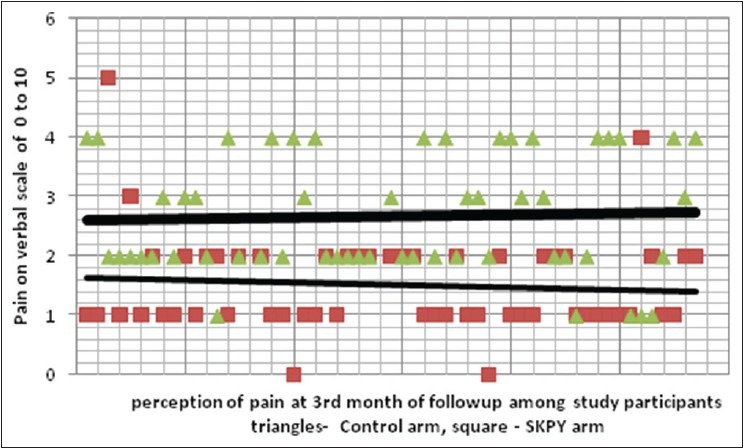
Verbal pains scale on 0-10 scale: showed average 2 point difference at 3rd month of follow-up in control versus Sudarshan Kriya and Pranayam yoga arm. (Upper thick line = control arm verbal pain scales, lower thin line = Sudarshan Kriya and Pranayam verbal pain scale)
DISCUSSION
A study performed in University of Miami,[17] has studied breast cancer report that women encounter a number of burdens, including anxiety about treatment and prognosis, adjuvant therapy, and disruptions in daily living.[14] Evidence suggests cancer-related stress has a negative impact on health, possibly via neuroendocrine pathways. Cortisol, a steroid hormone secreted by the adrenal cortex, is used to assess hypothalamic-pituitary-adrenal axis function and is a reliable measure of physiological stress.[18] Cortisol affects multiple physiological processes, including metabolic and immune responses (e.g., suppressing T lymphocyte functions and natural killer cell cytotoxicity). Women living with breast cancer have higher cortisol levels as compared to healthy women, and higher cortisol levels are associated with greater disease severity in women with breast cancer. Neuroendocrine regulation of cortisol and other adrenal hormones may contribute to cancer progression and health outcomes through multiple mechanisms. There is evidence that breast cancer is associated with greater plasma cortisol, which increases during a behavioral challenge reactivity task. If women with breast cancer are hyper responsive to stressful challenges, it also has been shown that they may show decreases in cortisol levels if they are taught stress management techniques. The pain experiences of 86 women with metastatic carcinoma of the breast were systematically evaluated over a period of 1 year in a study in University of California. 56% of the sample reported experiencing pain, and the intensity of pain was not significantly related to the site of metastasis. Multiple regression analysis revealed that 50% of the variance in the pain experience was accounted for by: (1) the amount of mood disturbance as measured by the Profile of Mood States. These data document the significance of psychological factors in accounting for differences in pain experience and document the interaction between pain and mood disturbance. These findings suggest that treatment of metastatic pain should include attention to the patient's mood and adjustment skills to the illness.[19]
Another study assessing pain, neurological symptoms, edema in arm, anxiety and depression occurring in women treated surgically for breast cancer, the impact of these symptoms on daily life and how they evolved during the follow-up. 1 year after surgery, 80% of the women had treatment-related symptoms in the breast scar region and virtually all patients had symptoms in the ipsilateral arm.[4]
In the current study, the higher level of serum cortisol in the control arm in comparison to the intervention arm were evident with significant statistical margins and correlate well with pain scores in the intervention arm. Raised serum cortisol has been reported as an indicator of clinical stage of the disease also.[18] One more study confirms high rates of behavioral symptoms in breast cancer survivors, particularly those treated with chemotherapy and indicates a role for tumor necrosis factor-α signaling as a contributor to post-chemotherapy fatigue. Results also suggest that fatigue, sleep disturbance, and depression may stem from distinct biologic processes in post-treatment survivors, with inflammatory signaling contributing relatively specifically to fatigue.[20]
Though many CBSM strategies,[21],[22],[23],[24] have reported a reduction of perception of pain and increased stress coping ability, decreased cortisol after intervention, however, intervention applied in this study has been considered very efficient, in terms of cost effectiveness (1 time workshop expenditure and weekly phone reminders was the expenditure incurred on the part of the research team, nothing spent from participant's side). This has been easily doable despite requiring physical exercise in the intervention; physically handicapped patients after breast surgery who had a problem of hand movement, 88% of them could do bhastrika paranayam and three stages P properly. This helps them to improve margin of movements in the arms. This unique combination of physical movement, rhythmic breathing and meditation imparted relaxed looks after intervention. The intervention is unique in the sense that it is uniformly followed across the countries, irrespective of cast creed; module remains the same, so chances of heterogeneity in practice and impact evaluation are minimal.
One lacunae identified during execution of the study was that due to distance many patients were providing their part of practice details on the phone only and physical verification of that doing practice could not be validated. To some extent, patients were informed about their nearest center to be regular in their practice, but only 12% could physically be verified of doing practice, Rest were relied on their version of doing SK and P practice on the phone and what their relatives and they themselves told on 3 monthly meetings of follow-up. Future research should provide provision of travel cost inbuilt in research grant, so physical verification is more intensified.
Further research is also required to address the underlying mechanism by in-depth analysis of findings, especially genetic component, to look whether these changes affect gene also. Since, this study imparted level-1 SKP Y module in the intervention arm, level-2 (more of meditation less in physical exercise) impact is hypothesized to be more intense and should be estimated for benefits of patients and researchers.
A meta-analysis from Germany retrieved 198 studies (covering 22,238 patients) that report 218 treatment-control comparisons. Significant small-to-medium effects were observed for individual and group psychotherapy and psychoeducation. These effects were sustained, in part, in the medium term (≤6 months) and long-term (<6 months). Short-term effects were evident for relaxation training. Studies that pre-selected participants according to increased distress produced large effects at post-treatment. A moderator effect was found for the moderator variable “duration of the intervention,” with longer interventions producing more sustained effects. Indicators of study quality were often not reported. Small-sample bias indicative of possible publication bias was found for some effects, particularly with individual psychotherapy and relaxation training.[25] This randomized controlled trial has used precaution (ample sample size, blinding, long follow-up, identified indicators) to address caution under this met analysis.
Though survival benefit of such interventions in advance stage cancer patients is also reported, this study recorded only marginal difference. The survival of 86 patients with metastatic breast cancer was studied prospectively in a study in which 1 year intervention consisted of weekly supportive group therapy with self-hypnosis for pain. Both treatment (n = 50) and control groups (n = 36) had routine oncological care. At 10 year follow-up, only 3 of the patients were alive, and death records were obtained for the other 83. Survival from time of randomization and onset of intervention was a mean 36.6 (SD 37.6) months in the intervention group compared with 18.9 (10.8) months in the control group, a significant difference. Survival plots indicated that divergence in survival began at 20 months after entry or 8 months after the intervention ended.[26] This type of long follow-up was not planned in this study; however, this study cohort may be followed to record overall long-term survival effect.
ACKNOWLEDGMENTS
Department of AYUSH, CCRYN, Ministry of Health and Family Welfare, Government of India is gratefully acknowledged for financial support to carry out this clinical trial.
Footnotes
Source of Support: AYUSH, Ministry of Health.
Conflict of Interest: None declared.
REFERENCES
- 1.Hebert JR, Ghumare SS, Gupta PC. Stage at diagnosis and relative differences in breast and prostate cancer incidence in India: Comparison with the United States. Asian Pac J Cancer Prev. 2006;7:547–55. [PubMed] [Google Scholar]
- 2.Brawley OW, Smith DE, Kirch RA. Taking action to ease suffering: Advancing cancer pain control as a health care priority. CA Cancer J Clin. 2009;59:285–9. doi: 10.3322/caac.20030. [DOI] [PubMed] [Google Scholar]
- 3.Jensen MP, Chodroff MJ, Dworkin RH. The impact of neuropathic pain on health-related quality of life: Review and implications. Neurology. 2007;68:1178–82. doi: 10.1212/01.wnl.0000259085.61898.9e. [DOI] [PubMed] [Google Scholar]
- 4.Tasmuth T, von Smitten K, Hietanen P, Kataja M, Kalso E. Pain and other symptoms after different treatment modalities of breast cancer. Ann Oncol. 1995;6:453–9. doi: 10.1093/oxfordjournals.annonc.a059215. [DOI] [PubMed] [Google Scholar]
- 5.Tasmuth T, von Smitten K, Kalso E. Pain and other symptoms during the first year after radical and conservative surgery for breast cancer. Br J Cancer. 1996;74:2024–31. doi: 10.1038/bjc.1996.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of sudarshan kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 7.Sharma H, Sen S, Singh A, Bhardwaj NK, Kochupillai V, Singh N. Sudarshan kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol. 2003;63:281–91. doi: 10.1016/s0301-0511(03)00071-1. [DOI] [PubMed] [Google Scholar]
- 8.Jyotsna VP, Joshi A, Ambekar S, Kumar N, Dhawan A, Sreenivas V. Comprehensive yogic breathing program improves quality of life in patients with diabetes. Indian J Endocrinol Metab. 2012;16:423–8. doi: 10.4103/2230-8210.95692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma H, Datta P, Singh A, Sen S, Bhardwaj NK, Kochupillai V, et al. Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I-Neurophysiologic model. J Altern Complement Med. 2005;11:4. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 10.Sharma H, Datta P, Singh A, Sen S, Bhardwaj NK, Kochupillai V, et al. Gene expression profiling in practitioners of sudarshan kriya. J Psychosom Res. 2008;64:213–8. doi: 10.1016/j.jpsychores.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Dhruva A, Miaskowski C, Abrams D, Acree M, Cooper B, Goodman S, et al. Yoga breathing for cancer chemotherapy-associated symptoms and quality of life: Results of a pilot randomized controlled trial. J Altern Complement Med. 2012;18:473–9. doi: 10.1089/acm.2011.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatia M, Kumar A, Kumar N, Pandey RM, Kochupillai V, EEG study, et al. Electrophysiologic evaluation of sudarshan kriya: An EEG, BAER, P300 study. Indian J Physiol Pharmacol. 2003;47:157–63. [PubMed] [Google Scholar]
- 13.Kochupillai V, Kumar P, Singh D, Aggarwal D, Bhardwaj N, Bhutani M, et al. Effect of rhythmic breathing (sudarshan kriya and pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005;1056:242–52. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- 14.Williams LS, Jones WJ, Shen J, Robinson RL, Weinberger M, Kroenke K. Prevalence and impact of depression and pain in neurology outpatients. J Neurol Neurosurg Psychiatry. 2003;74:1587–9. doi: 10.1136/jnnp.74.11.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II - Clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 16.Vogeser M, Zachoval R, Jacob K. Serum cortisol/cortisone ratio after Synacthen stimulation. Clin Biochem. 2001;34:421–5. doi: 10.1016/s0009-9120(01)00251-x. [DOI] [PubMed] [Google Scholar]
- 17.Phillips KM, Antoni MH, Lechner SC, Blomberg BB, Llabre MM, Avisar E, et al. Stress management intervention reduces serum cortisol and increases relaxation during treatment for nonmetastatic breast cancer. Psychosom Med. 2008;70:1044–9. doi: 10.1097/PSY.0b013e318186fb27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernabé DG, Tamae AC, Miyahara GI, Sundefeld ML, Oliveira SP, Biasoli ÉR. Increased plasma and salivary cortisol levels in patients with oral cancer and their association with clinical stage. J Clin Pathol. 2012;65:934–9. doi: 10.1136/jclinpath-2012-200695. [DOI] [PubMed] [Google Scholar]
- 19.Spiegel D, Bloom JR. Pain in metastatic breast cancer. Cancer. 1983;52:34–345. doi: 10.1002/1097-0142(19830715)52:2<341::aid-cncr2820520227>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 20.Bower JE, Ganz PA, Irwin MR, Kwan L, Breen EC, Cole SW. Inflammation and behavioral symptoms after breast cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517–22. doi: 10.1200/JCO.2011.36.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruess DG, Antoni MH, McGregor BA, Kilbourn KM, Boyers AE, Alferi SM, et al. Cognitive-behavioral stress management reduces serum cortisol by enhancing benefit finding among women being treated for early stage breast cancer. Psychosom Med. 2000;62:304–8. doi: 10.1097/00006842-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Schedlowski M, Jung C, Schimanski G, Tewes U, Schmoll HJ. Effects of behavioral intervention on plasma cortisol and lymphocytes in breast cancer patients: An exploratory study. Psychooncology. 1994;3:181–7. [Google Scholar]
- 23.Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, et al. How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psychol. 2006;74:1143–52. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antoni MH, Wimberly SR, Lechner SC, Kazi A, Sifre T, Urcuyo KR, et al. Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry. 2006;163:1791–7. doi: 10.1176/ajp.2006.163.10.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-analysis. J of Clinical Oncology. 2011;40:8922. doi: 10.1200/JCO.2011.40.8922. [DOI] [PubMed] [Google Scholar]
- 26.Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888–91. doi: 10.1016/s0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]


