Abstract
Purpose:
To identify pre-operative variables affecting the outcome of posterior open globe (zone III) injuries. Secondary objective was to re-look at the definition or landmarks for zone III injury and its clinical significance for predicting visual prognosis following open globe injury.
Materials and Methods:
Retrospective review of medical records of all hospitalized patients with surgical repair of open globe injury over last 10 years at a tertiary referral eye care center in Singapore. Out of 172 eyes with open globe injury, 28 eyes (16.3%) with zone III injury was identified and reviewed further. Pre-operative visual acuity (VA) and other variables, extent of scleral wound in reference to rectus insertion, relative afferent pupillary defect (RAPD) and final vision outcome were recorded.
Results:
Median age was 37 years with male predilection (92.9%). Mean follow-up was 12.9 months. Pre-operative VA was no light perception (NLP) in 16 (57.1%) eyes. Final VA remained NLP in 14 eyes (50.0%). The factors contributing to poor post-operative vision based on univariate regression analysis were the presence of RAPD, poor pre-operative VA, blunt trauma, extent of trauma, associated traumatic cataract, hyphema, vitreous loss and associated vitreo-retinal trauma. Further on, zone III injuries with scleral wound limited anterior to rectus insertion (6 eyes) had better vision outcome than those with injuries extending beyond rectus insertion (22 eyes).
Conclusion:
Initial VA, blunt ocular trauma, visual axis involvement, loss of light perception, presence of RAPD, traumatic cataract, hyphema, vitreous loss were the important determinants for final visual outcome in patients with zone III injury. Wound extending posterior to rectus insertion has poorer outcome as those limited anterior to rectus insertion. We suggest that there may be a need to relook at zone III injuries with reference to rectus insertion for prognostic significance, and further studies are warranted.
Keywords: Posterior open globe injuries, posterior to rectus insertion, zone III open globe injuries
Ocular trauma is a leading cause of visual morbidity world-wide.[1] It accounts for about 50% of all eye casualties admitted in developed countries.[2] It impacts not only the individual, but also the country's healthcare system and community.[3,4]
The Ocular Trauma Classification group classified mechanical injuries of the eye into open globe and closed globe injuries.[5] The classification system was based on four specific variables that have been of prognostic significance for final visual outcome: Type of injury, grade of injury (based on visual acuity (VA) at the initial examination), presence of relative afferent pupillary defect (RAPD) and the zone of injury. The zone of injury was defined by the location of the most posterior aspect of the globe opening [Fig. 1]. Zone I injuries occur when the break in the globe was isolated to the cornea or corneoscleral limbus [Fig. 1]. Zone II injuries are those that involved anterior 5 mm of the sclera-5 mm extension into the sclera is chosen as a landmark as it has been hypothesized that wounds located in this zone would not extend posteriorly beyond the pars plana [Fig. 1]. Zone III injuries are those that extended full thickness into the sclera more than 5 mm posterior to the corneoscleral limbus [Fig. 1]. Though, the zone of injury was often determined at the time of the initial examination, the exact extent of the injury may be more accurately determined during the time of surgical intervention.[5]
Figure 1.
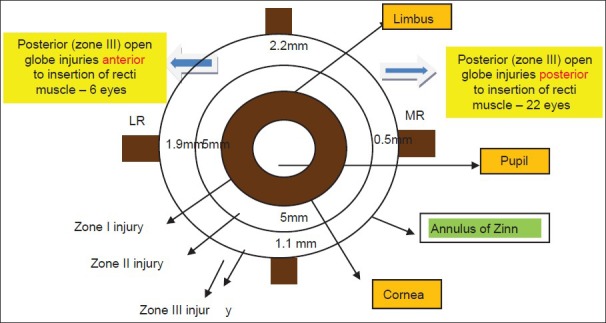
Diagramatic representation of the extent of wound in relation to recti insertion
Zone III injuries have been reported to be associated with poorer outcomes. However, there is limited literature on pre-operative variables affecting final anatomical and vision outcome in patients with zone III injuries.[6] We aimed to evaluate the pre-operative variables affecting the final vision outcome following surgical repair of posterior open globe injuries. The hypothesis of zone III injuries leading to poorer final vision outcome was also tested in this study.
Materials and Methods
A retrospective review of medical records of all consecutive patients who underwent surgical repair of open globe injuries over 10 years from 2000 to 2009 at a tertiary referral eye care center in Singapore was carried out after local ethics board approval. Medical records of all the patients were grouped into 3 zones based on the extent of injury measured during surgical repair as defined by the Ocular Trauma Classification [Fig. 1].[5] Medical records of eyes with zone III injuries were further analyzed in detail. Data collected included patient demographics and clinical data including laterality, mode and mechanism of injury, pre-operative VA, presence of RAPD, location and extent of the injury, ocular structures involved in the injury and number of surgeries. Final post-operative VA and duration of follow-up were also documented.
Pre-operative and final post-operative Snellen VA was divided into five categorical groups for statistical analysis: group 1 (≤6/12), group 2 (6/18-6/36), group 3 (6/60 to counting finger [CF]), group 4 (hand movements [HM] to perception of light) and group 5 (no light perception). All patients in this study underwent primary repair within 24 h of emergency consultation. The final post-operative best corrected VA was the outcome measured at 6 months follow-up. All patients had a minimal follow-up of 6 months.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (version 14, SPSS Inc., Chicago, IL, USA). Fisher's exact test was applied to study the factors affecting final vision outcome individually. Multivariate analysis and logistic regression analysis were applied to define the association between final post-operative VA and those factors found to be significant on univariate analysis. The significance level for all tests was set as 0.05.
Results
Out of 172 eyes with open globe injuries there were 28 eyes of 28 patients with posterior open globe injuries involving zone III. The detailed demographics and findings are tabulated in Table 1a and b. The mean age was 37.7 years, (median age: 37 years, range 19-74 years) and median follow-up was 6.5 months (mean follow-up: 12.9 months, range 6-60 months). There was a male predominance (92.9%). Eleven (39.3%) patients had open globe injury following penetrating trauma while remaining patients had globe rupture secondary to blunt trauma. Pre-operative VA was as listed in Table 1a and was divided into five categorical groups as described above. Associated hyphema and visual axis involvement were seen in 24 (85.7%) eyes. Vitreous loss with vitreous hemorrhage was seen in 20 (71.4%) eyes. Traumatic cataract occurred in 18 (64.3%) eyes and retinal detachment in 50% of eyes. There were 4 (14.3%) eyes with associated intraocular foreign bodies. All 28 eyes underwent wound exploration and primary surgical repair within 24 h of injury. Fourteen (50%) of eyes underwent a second surgery for retinal detachment and 3 required a further third surgical procedure. All 14 eyes underwent combined pars plana vitreo-retina surgery with or without cataract extraction and 3 patients had additional silicone oil injection with encirclage. Final VA in correlation with initial VA is cross tabulated in Table 2. Univariate analysis was performed for different pre-operative variables affecting final VA outcome. Pre-operative variables that were found to be statistically significant are shown in Table 3. However, multivariate analysis using multinomial logistic regression analysis did not show any single factor significantly affecting final VA.
Table 1a.
Patients with posterior open globe (zone III) injuries
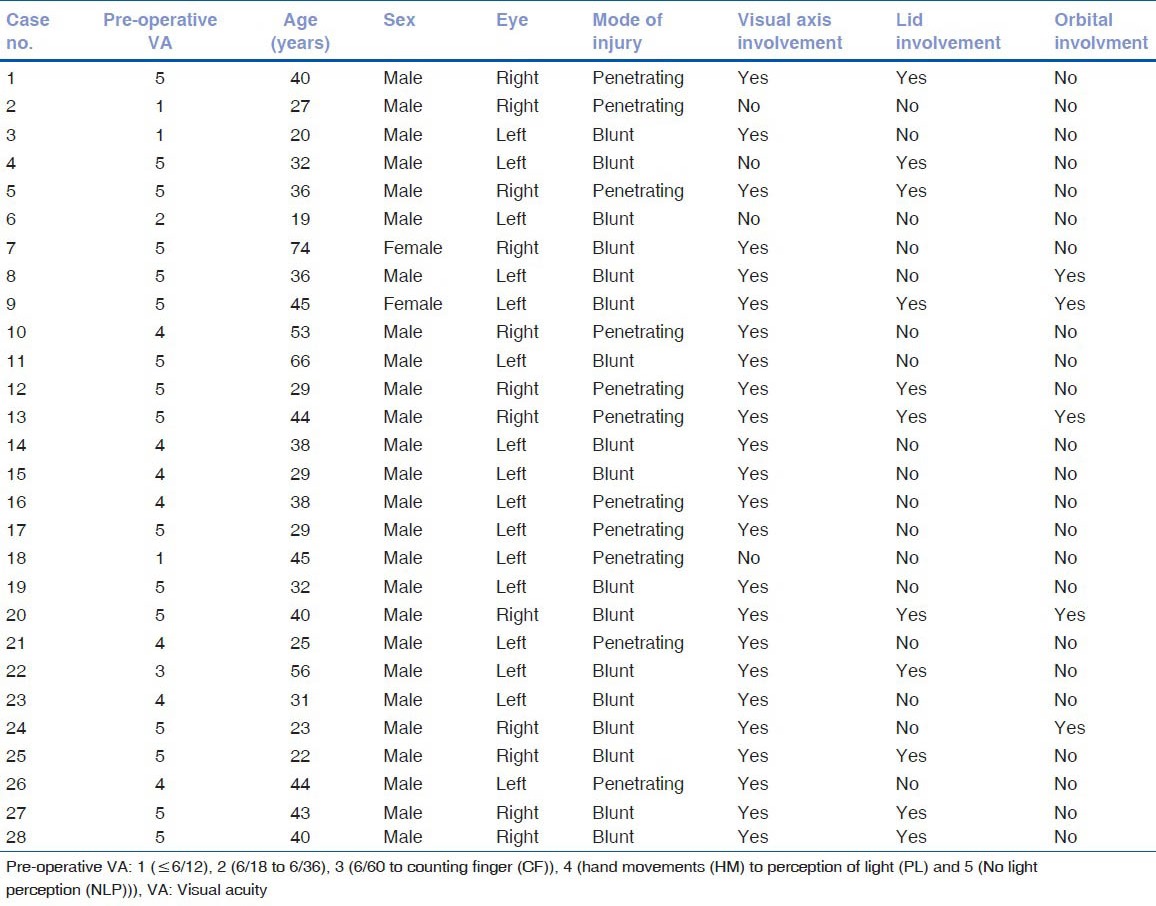
Table 1b.
Patients with posterior open globe (zone III) injuries
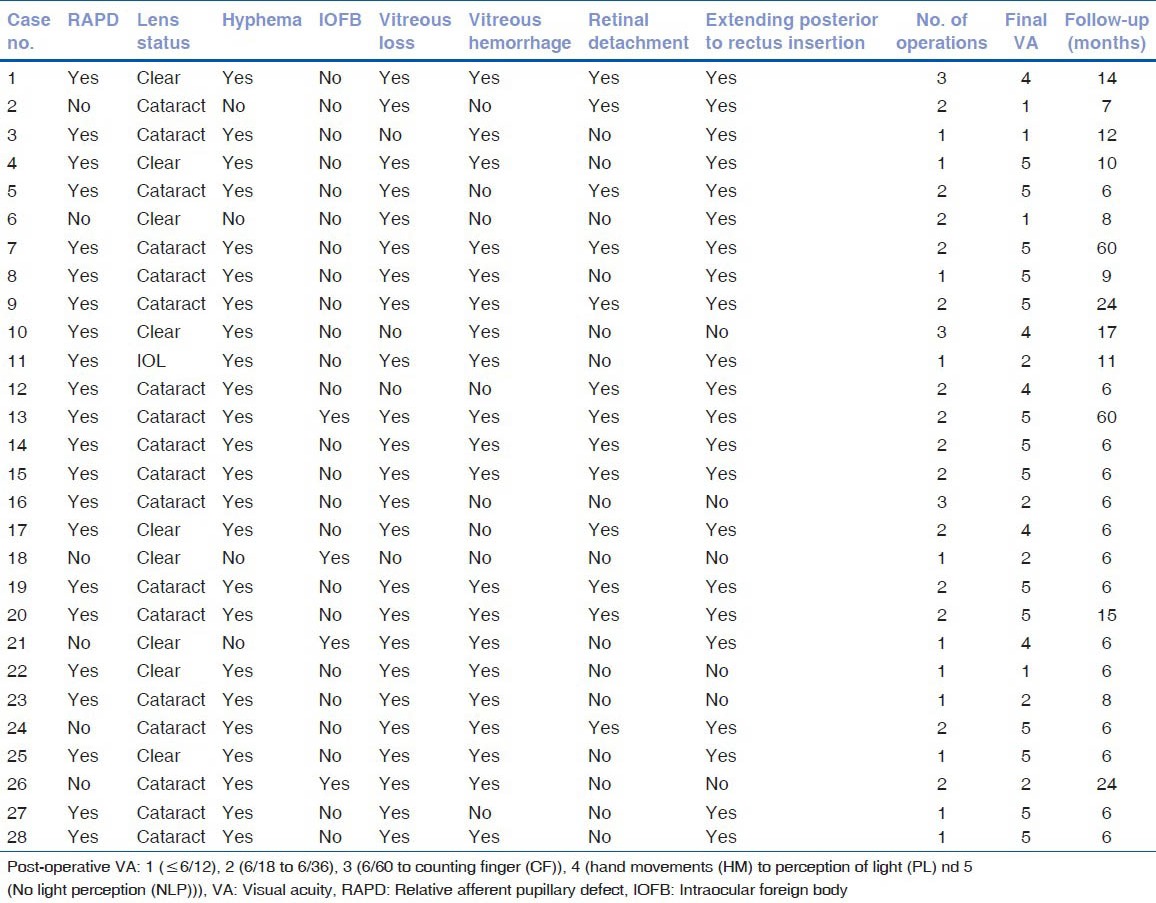
Table 2.
Cross tabulation of pre-operative versus postoperative visual acuity
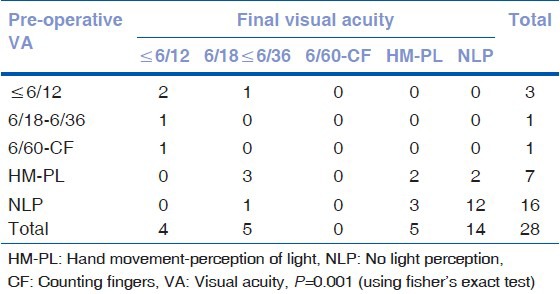
Table 3.
Univariate analysis of pre-operative variables affecting final vision outcome in eyes with posterior (zone III) open globe injuries
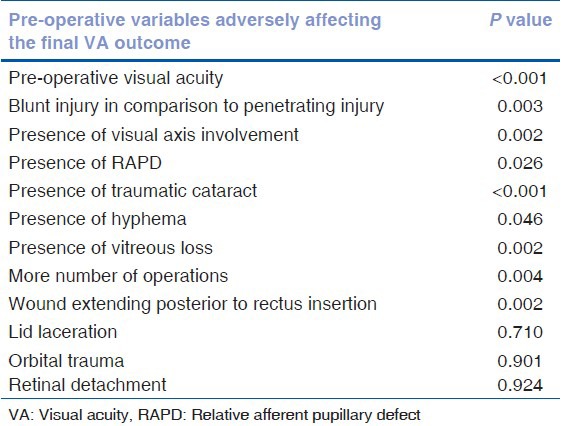
Length of laceration or radial extent of scleral wound was found to be significantly affecting the final vision outcome based on the univariate analysis. In eyes with zone III injury, those eyes with scleral wounds extending posterior to rectus insertion having poorer outcomes than those with scleral wounds limited anterior to rectus insertion (P = 0.002). The number of eyes with wound extending anterior or posterior in relation to rectus insertion is as shown in Fig. 1.
Discussion
There are significant number of studies on preoperative variables affecting final visual outcome in patients with open globe injuries.[7,8,9,10,11,12,13] To out of the numerous factors affecting final vision outcome, posteriorly extended open globe injury has been indicated to be one of the poor prognostic indicator.[7,8,9,10,11,12,13] There are, however limited studies on factors affecting the outcome in posterior open globe injuries (zone III injuries).[6] In our study, we attempted to identify factors affecting final vision outcome in patients specifically with zone III injuries and also analyzed zone III injuries as a prognostic indicator for final VA outcome.
Knyazer et al. identified 21 patients with zone III injury in a series of open globe injury patients and identified pre-operative VA, eyelid injury, iris deformity, lens damage, ocular hypotonia, and retinal detachment as prognostic indicators associated with final vision outcome. Depending on the site and extent of retinal detachment and amount of vitreous loss, the final vision outcome will be affected.[6] In our study, poor initial VA correlated with poorer visual outcome, and this was statistically significant on univariate logistic regression analysis. Patients who had a pre-operative vision of CF or better had improvement in the final VA, whereas the majority of patients with initial VA of HM or worse had poorer final vision outcome. In our study, vitreo-retinal operations performed for retinal detachment, proliferative vitreo-retinopathy and vitreous hemorrhage resulted in improvement in final vision outcome. The number of operations was found to be statistically significant for a poorer visual outcome on univariate logistic regression analysis. This was consistent clinically as second or subsequent operations were usually performed for associated vitreo-retinal injury, which had a poorer prognostic outcome. Conversely, in cases where only scleral wound repair was required, visual outcome was more favorable because of less collateral damage requiring second or subsequent surgeries.
We had no cases of post-traumatic or post-operative endophthalmitis in our study. This could be due to the presence of an intact conjunctiva covering the break in the globe as seen in blunt injuries (60.7% eyes) and early intervention within 24 h of injury in all the eyes. Penetrating injuries due to the high velocity impact such as fragments from hammering were also less likely to lead to endophthalmitis as high velocity leads to generation of heat and hence a relative sterile surface upon penetration. The presence of vegetative and iron intraocular foreign bodies and delay in surgical repair and initiation of antibiotics have been reported to be more likely to result in endophthalmitis.[14,15,16]
The significant factor, which was noted from this study was the extent of wound affecting the final vision outcome and its correlation with insertion of the rectus muscle or “spiral of Tillaux or annulus of Zinn.” The radial scleral lacerations extending beyond recti insertion were often associated with poorer outcome because of co-morbid factors such as retinal detachment, vitreous traction and significant vitreous loss. Cases with zone III injuries not extending beyond “annulus of Zinn” as highlighted in Fig. 1 were associated with good outcome. The possible explanation for adverse outcome in injuries extending beyond “annulus of Zinn” is because of significant vitreo-retinal trauma associated with posteriorly extending scleral laceration. International Ocular trauma classification group have defined zone III injuries as those extending beyond 5 mm of limbus.[5] Based on the justification given by ocular trauma classification group, they have arbitrarily taken it as 5 mm as injuries in that zone may not extend into pars plana. However, based on literature search, the anteroposterior length of the ciliary body and hence the position of the pars plana varies considerably with the length of the eye. It is always longer on the temporal side and longest inferotemporally, the most expanded quadrant of the eye [Fig. 2].[17,18,19] Temporally it is 5.6-6.3 mm in length, and nasally 4.6-5.2 mm.[18] Of importance surgically is the distance from the external corneoscleral limbus to the end of the ciliary body at the ora serrata which marks the beginning of the pars plana. This may be roughly estimated as 7 mm temporally and 6 mm nasally since in 200 autopsy eyes the slightly shorter distance from Schwalbe's line internally to the end of the ciliary body at the ora serrata averaged 6.53 mm temporally, 5.73 mm nasally, 6.14 mm superiorly, and 6.20 mm inferiorly.[20] This distance of ora serrata from corneoscleral limbus almost coincides and overlaps with Spiral of Tillaux, the imaginary line along the insertion of all rectus muscle [Fig. 2].[19]
Figure 2.
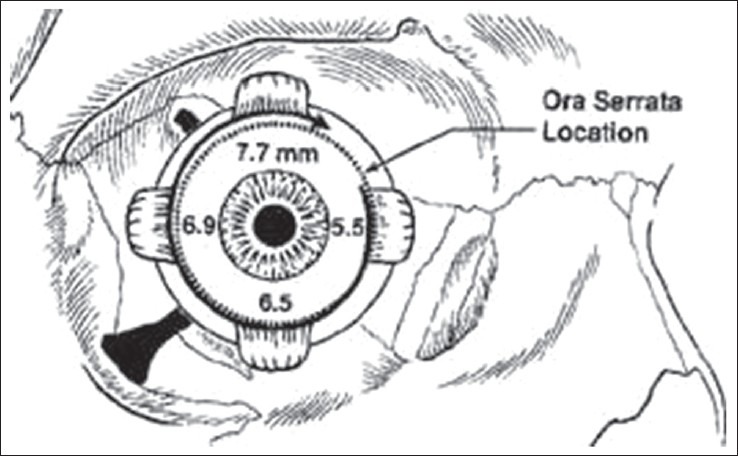
Anterior view of the right globe: Spiral of tillaux is shown with superimposed location of the ora serrata
We suggest we should look at the landmark of zone III injury, and for the same, we may need larger prospective multicentric studies and the hypothesis, which needs to be tested is the prognostic significance of zone III injuries. From the current study with very small sample size, it's indicated that zone III injuries should rather be defined for those injuries extending beyond “annulus of Zinn” i.e. beyond rectus insertion, which is not necessarily 5 mm from limbus and varies with each rectus muscle for prognostic importance.
We acknowledge that the current study has several limitations including the small sample size which obviously is too small to comment on new classification system by itself for this form of rare injury. Although this is a retrospective case series, the most important visual and ophthalmic parameters were collected as routine assessment. However, despite this limitation, we identified several parameters as potential predictive factors.
In conclusion, pre-operative variables such as initial VA, RAPD, extent of wound posterior to recti insertion, retinal detachment, hyphema, lens involvement, vitreous loss affect the final vision outcome in posterior open globe injuries which is very similar to those shown in previous similar studies. However, landmark of zone III injuries may be redefined to “annulus of Zinn” instead of conventional 5 mm from limbus is the important recommendation for further consideration from the current study.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 2.Chiapella AP, Rosenthal AR. One year in an eye casualty clinic. Br J Ophthalmol. 1985;69:865–70. doi: 10.1136/bjo.69.11.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong TY, Klein BE, Klein R. The prevalence and 5-year incidence of ocular trauma. The Beaver Dam Eye Study. Ophthalmology. 2000;107:2196–202. doi: 10.1016/s0161-6420(00)00390-0. [DOI] [PubMed] [Google Scholar]
- 4.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 5.Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, Bridges WZ, Jr, Capone A, Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–31. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 6.Knyazer B, Levy J, Rosen S, Belfair N, Klemperer I, Lifshitz T. Prognostic factors in posterior open globe injuries (zone-III injuries) Clin Experiment Ophthalmol. 2008;36:836–41. doi: 10.1111/j.1442-9071.2009.01922.x. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9. doi: 10.1016/j.ophtha.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 8.De Juan E, Jr, Sternberg P, Jr, Michels RG. Penetrating ocular injuries. Types of injuries and visual results. Ophthalmology. 1983;90:1318–22. doi: 10.1016/s0161-6420(83)34387-6. [DOI] [PubMed] [Google Scholar]
- 9.Groessl S, Nanda SK, Mieler WF. Assault-related penetrating ocular injury. Am J Ophthalmol. 1993;116:26–33. doi: 10.1016/s0002-9394(14)71739-8. [DOI] [PubMed] [Google Scholar]
- 10.Cruvinel Isaac DL, Ghanem VC, Nascimento MA, Torigoe M, Kara-José N. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5. doi: 10.1159/000073075. [DOI] [PubMed] [Google Scholar]
- 11.Karlson TA, Klein BE. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol. 1986;104:1473–6. doi: 10.1001/archopht.1986.01050220067028. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert CM, Soong HK, Hirst LW. A two-year prospective study of penetrating ocular trauma at the Wilmer Ophthalmological Institute. Ann Ophthalmol. 1987;19:104–6. [PubMed] [Google Scholar]
- 13.Abrams GW, Knighton RW. Falsely extinguished bright-flash electroretinogram. Its association with dense vitreous hemorrhage. Arch Ophthalmol. 1982;100:1427–9. doi: 10.1001/archopht.1982.01030040405005. [DOI] [PubMed] [Google Scholar]
- 14.Brinton GS, Topping TM, Hyndiuk RA, Aaberg TM, Reeser FH, Abrams GW. Posttraumatic endophthalmitis. Arch Ophthalmol. 1984;102:547–50. doi: 10.1001/archopht.1984.01040030425016. [DOI] [PubMed] [Google Scholar]
- 15.Thompson WS, Rubsamen PE, Flynn HW, Jr, Schiffman J, Cousins SW. Endophthalmitis after penetrating trauma. Risk factors and visual acuity outcomes. Ophthalmology. 1995;102:1696–701. doi: 10.1016/s0161-6420(95)30807-x. [DOI] [PubMed] [Google Scholar]
- 16.Schmidseder E, Miño de Kaspar H, Klauss V, Kampik A. Post-traumatic endophthalmitis after penetrating eye injuries. Risk factors, microbiological diagnosis and functional outcome. Ophthalmologe. 1998;95:153–7. doi: 10.1007/s003470050254. [DOI] [PubMed] [Google Scholar]
- 17.Barker-Griffith AE, Streeten BW, Fikhman M, Gutman J. The Ciliary Body. In: Tasman W, Jaeger EA, editors. Duane's Foundations of Clinical Ophthalmology. Chap 13. I. Philadelphia, PA: Lippincott, Williams and Wilkins; 2011. [Google Scholar]
- 18.Straatsma BR, Landers MB, Kreiger AE. The ora serrata in the adult human eye. Arch Ophthalmol. 1968;80:3–20. doi: 10.1001/archopht.1968.00980050005002. [DOI] [PubMed] [Google Scholar]
- 19.Sherman DD, Lemke BN. Orbital anatomy and its clinical applications. In: Tasman W, Jaeger EA, editors. Duane's Clinical Ophthalmology. Ch. 21. Vol. 2. Philadelphia: Lippincott Raven; 1997. pp. 13–20. [Google Scholar]
- 20.Salzmann M. Chicago: University of Chicago Press; 1912. The Anatomy and Histology of the Human Eyeball; p. 107. [Google Scholar]


