Abstract
Despite being a relatively effective and safe treatment, the clinical management of alcohol abuse/dependence by oral naltrexone can be compromised due to the patient's non-compliance with daily use of this medication. Over the past decade an increasing body of research has suggested that the use of sustained release depot naltrexone preparations can overcome this issue and deliver improved clinical outcomes. However, at the same time, research findings from diverse areas of pharmacogenetics, neurobiology and behavioural psychology have also been converging to identify variables including genetic markers, patient psychosocial characteristics and drug use history differences, or clusters of these variables that play a major role in mediating the response of alcohol abuse/dependent persons to treatment by naltrexone. While this article does not attempt to review all available data pertaining to an individual alcohol dependent patient's response to treatment by naltrexone, it does identify relevant research areas and highlights the importance of data arising from them. The characterization of clinical markers, to identify those patients who are most likely to benefit from naltrexone and to tailor a more individual naltrexone treatment, will ultimately provide significant benefit to both patients and clinicians by optimizing treatment outcome.
Keywords: alcoholism, clinical subtypes, naltrexone maintenance, oral naltrexone, pharmacogenetics, pharmacokinetics, predictors of treatment outcomes
“No animal ever invented anything so bad as drunkenness – or so good as drink” [1].
Introduction
Alcoholism is a serious issue worldwide, having a negative impact on the health and welfare of the drinker as well as their community. According to the World Health Organization (WHO), globally, around 2.5 million deaths each year result from harmful alcohol use [2]. Alcohol is the underlying cause of more than 30 conditions (e.g. cancer, diabetes, neuropsychiatric diseases, cardiovascular diseases, liver and pancreas diseases and unintentional and intentional injury) and a contributing factor to many more conditions [3]. Alcohol is the leading risk factor for the burden of disease in the Western Pacific and the Americas, the second largest in Europe and the third largest globally [2]. In the United Kingdom, using the population attributable fractions from WHO's Global Burden of Disease Project, it is estimated that alcohol consumption was directly responsible for around 31 000 deaths in 2005, and cost the National Health Service £3.0 billion in 2005–2006, due to increased mortality and morbidity [4]. Including other less tangible costs such as premature deaths, loss of productivity, violence and crime, the cost of alcohol to the Australian community was estimated to be $15.3 billion [3].
Patients with problem alcohol use can present anywhere along a continuum from early stage problems, such as ‘recreational’ or binge use, to severe alcohol dependence with major psycho-social or major and/or multiple health problems. End stage persons in this group commonly have negligible non-alcohol using social support and require intensive intervention, usually with the objective of reconstructing a low alcohol or abstinence lifestyle. Psychopharmacology based programmes have become the cornerstone for treatment of this group. Three oral pharmacotherapies (acamprosate, disulfiram and naltrexone) are commonly used for the management of alcohol abuse or dependence.
Oral naltrexone
Naltrexone is an opioid antagonist which primarily, but not exclusively, targets the μ-opioid receptor. Naltrexone likely exerts its actions by blockade of the high concentration of μ-opioid receptors located in areas of the brain that have been implicated in the reward pathway associated with alcohol. Oral naltrexone is relatively safe and has a moderate to good clinical efficacy in the management of persons with alcohol dependence [5, 6]. Meta-analysis studies have concluded that the use of naltrexone is most appropriate where controlled drinking is the desired outcome [7, 8]. Another study suggests that the treatment efficacy of naltrexone is greater during active alcohol consumption and depends on aversive side effects [9]. Naltrexone is also associated with significant improvements on a number of other clinical measures including increased time to alcohol relapse, number of drinks per drinking day, improved liver function indicators (γ-glutamyl transferase (GGT), aspartate aminotransferase) and reduction in alcohol craving [10]. An evaluation of the comparative cost of treating alcohol dependence with either cognitive behavioural therapy (CBT) alone or CBT combined with oral naltrexone over a 12 week treatment programme showed that the addition of naltrexone significantly improved abstinence rates (36.1% CBT, 62.6% CBT + naltrexone) and, although adding 54% to treatment costs, was found to be the most effective treatment option [11]. Despite the aforementioned there are few data on oral naltrexone treatment beyond 12 weeks and limited long term follow-up data [10]. Therefore, it is speculative to generalize to ‘real world’ utility.
Despite these positive outcomes associated with oral naltrexone treatment, non-compliance with oral naltrexone formulae has been a major impediment to achieving positive clinical outcomes for a significant number of patients. A meta-analysis found that 37% of patients discontinue daily oral naltrexone use by 12 weeks (placebo 43%) [12], with other data indicating more than 80% of patients discontinued use by 6 months [13]. Non-compliance is often associated with a patient's withdrawal from treatment, return to alcohol abuse/dependence [14] and greater use of costly health care services, i.e. emergency departments and hospitals [15]. A US survey showed that 80% of physicians indicated that their decision to prescribe oral naltrexone, albeit for opiate dependence, was based on their opinion about whether the patient would comply with medication [16]. A study comparing combined efficacy of behavioural treatment and naltrexone found a doubling in the effect size of the oral naltrexone by therapy interactions when the analysis was performed only on the subgroup of oral naltrexone compliant patients [17]. Clearly, if naltrexone treatment for alcohol dependence is to have ‘real world’ clinical utility, attention must be focused on ways to improve medication compliance.
Long acting preparations of naltrexone
An alternative method of naltrexone maintenance delivery involves the injection or surgical insertion of a sustained release preparation of naltrexone. This approach removes the need for patients to use daily oral naltrexone. Sustained release preparations have commonly involved using compressed naltrexone or naltrexone/polymer/co-polymer base formulations administered subcutaneously or intramuscularly [18].
The concept of sustained release preparations of naltrexone is not new. In 1980, the US National Institute of Health called for the development of a ‘naltrexone sustained-release parenteral drug delivery system’ for the management of substance abuse. In addition to providing therapeutically relevant blood concentrations for extended periods, they noted that products should be clinically effective, biodegradable, biocompatible and easy to administer [19]. Beginning in the mid-1970s, a number of depot naltrexone formulations were developed. While showing promising naltrexone release patterns, most had unacceptable tissue compatibility. For example, Chiang et al. [20] subcutaneously implanted naltrexone-copolymer (90% L-lactic acid and 10% glycolic acid) beads in normal, healthy volunteers. While naltrexone plasma concentrations were relatively constant (0.3–0.5 ng ml−1) for up to 1 month following an initial burst of release, this formulation was not biocompatible, with two of the three human subjects having them removed at approximately 3 to 4 weeks due to marked inflammatory reactions or other local tissue irritation [21].
Newer formulations of sustained-release naltrexone have proved more promising. An increasing body of literature, particularly arising from randomized trials in the US, strongly suggests that depot sustained release formulations of naltrexone which commonly maintain therapeutic blood naltrexone concentrations of above 1–2 ng ml−1 for approximately 4 weeks can, in the short to medium term, optimize treatment outcomes [22–24]. For example an intramuscular depot formulation of naltrexone manufactured by Drug Abuse Sciences (USA) was tested in a large cohort of 158 alcohol abuse/dependent persons, with another 157 patients receiving placebo [24]. Injections were given monthly for 3 months with significant benefits of increased time to first drinking day and total abstinence rate for the naltrexone group, despite approximately 25% of the naltrexone group failing to return for their third injection. The blood naltrexone concentrations were not reported in this study, but an earlier pilot study using the same naltrexone formulation, noted a peak plasma concentration of less than 6 ng ml−1 on day 1, falling to about 2 ng ml−1 on day 3. Mean plasma naltrexone concentrations remained above 1 ng ml−1 for 21 days but they noted that reductions in heavy drinking days were sustained for 8 weeks [25]. A pharmacokinetic and safety trial of the same depot preparation (n = 16) showed mean blood concentrations peaked at 2.04 ng ml−1 falling to 0.58 ng ml−1 by 6 weeks [22].
A 30 day injectable naltrexone formulation (Vivitrex®) has now been approved by the US's Federal Food & Drug Administration for the management of alcohol dependence (N.B. ‘Vivitrex’ has been renamed ‘Vivitrol’ as part of an application for FDA product registration). Johnson and colleagues conducted a pilot evaluation involving 25 participants who received an active (400 mg) treatment (Vivitrex®) and five people who received a placebo injection. Treatment consisted of four injections at 28 day intervals. At 28 days the mean blood naltrexone concentration was 1.23 ng ml−1 and this dosing regimen resulted in an average blood naltrexone concentration of 1.33 ng ml−1 over the study. The small sample size meant that significant outcomes were not obtained, but there were trends in the predicted direction for both alcohol consumption and liver enzyme (GGT) measures. However, 32% of the active treatment group failed to complete the 4 monthly study injections [26].
A larger 6 month trial of Vivitrol® (205 received 380 mg injections, 210 received 190 mg injections and 209 received placebo injections, with all being offered psychosocial intervention) which was used to support its registration with the FDA also reported a reduction of 25% (P = 0.03) in heavy drinking days in the 380 mg naltrexone and 17% (P = 0.07) in the lower 190 mg dose compared with placebo recipients. Although those seeking complete abstinence had a greater reduction in alcohol use, the injectable naltrexone also showed benefits for those only seeking to reduce their consumption. Overall, the drug was well-tolerated. However 36% of patients failed to complete the 6 month course of monthly injections, with the majority lost to follow-up after 60 days [23]. These authors cited a 14.1% discontinuation due to adverse events in participants receiving the 380 mg naltrexone injection. Notably, this pivotal study did not include a treatment group who received the standard existing pharmacotherapy, such as oral naltrexone.
Two sets of post hoc analyses based on the data from this large trial were subsequently conducted to examine the efficacy of Vivitrol® in patients who abstained at baseline [27] and patients' early treatment response [28]. O'Malley and colleagues found that among patients who abstained for at least 4 days prior to treatment, compared with placebo treatment, the 380 mg injection demonstrated ‘robust and clinically meaningful improvements’, with time to first drink increasing three-fold, time to first heavy drink increasing nine-fold, and the number of heavy drinking days per month 10 times less [27]. Ciraulo and associates noted a rapid onset of therapeutic effect of the 380 mg injection in the first 2 days of treatment, which was maintained throughout the 24 week study duration [28].
An additional potential advantage of sustained release naltrexone products is that they avoid the gastro-intestinal route and hence may produce less gastro-intestinal side effects (e.g. nausea), compared with oral formulations. Avoidance of first-pass hepatic metabolism also means that only a small monthly dosage (e.g. 380 mg injection vs. 1500 mg based on 50 mg day−1 dosing) and a significantly higher ratio of naltrexone (the active primary agent) to 6β-naltrexol (the principal metabolite) in blood can be attained [29]. Further, they provide more constant blood naltrexone concentrations, thereby avoiding the peaks and troughs in 6β-naltrexol concentrations that have been associated with adverse side-effects of treatment [30]. The one small study (n = 20) that compared side-effects for sustained release and oral naltrexone found a fall in iatrogenic effects with sustained release naltrexone [mean 1.80 (SD 1.82) vs. 1.33 (SD 1.95)] [25].
In summary, data show that extended naltrexone formulations overcome the daily medication non-compliance issues associated with oral naltrexone, and produce good treatment outcomes. However, the requirement that patients return for re-treatment every 30 days is associated with high attrition rates post 60 days (25–36%) and limits clinical efficacy [23, 24, 26]. It follows that treatment with a longer acting naltrexone preparation that reduces the frequency of re-treatments over any given period is likely to be associated with reduced relapse and produce more stable patient outcomes over time.
Recently a subcutaneously implantable formulation of naltrexone was developed which can maintain blood naltrexone for approximately 4 to 6 months [31]. Although no direct comparison has been undertaken with the FDA registered Vivitrol® published blood profile data can be used to compare a single treatment with implant naltrexone compared with that of monthly injection with Vivitrol®.
Figure 1 depicts the (raw) data on blood (serum) naltrexone concentrations over time from a single treatment with a 2.2 g naltrexone implant (n = 24). Statistical modelling has shown that this implant can sustain blood naltrexone concentrations at or above 2 ng ml−1 for approximately 136 (95% CI 114, 158) days, taking into account potential confounding effect of body weight, gender and age of the sampled population [31]. Also shown on the graph (heavy dotted line) are the mean blood (plasma) naltrexone concentrations from repeated (every 4 weeks) dosing of a 380 mg Vivitrol injection in a clinical trial (n = 12) [32]. Concentrations following doses 2 and 3 are not available from the referenced paper. They are interpolated from doses 1 and 4 concentrations, with the 13% accumulative effect of repeated dosing also taken into account.
Figure 1.
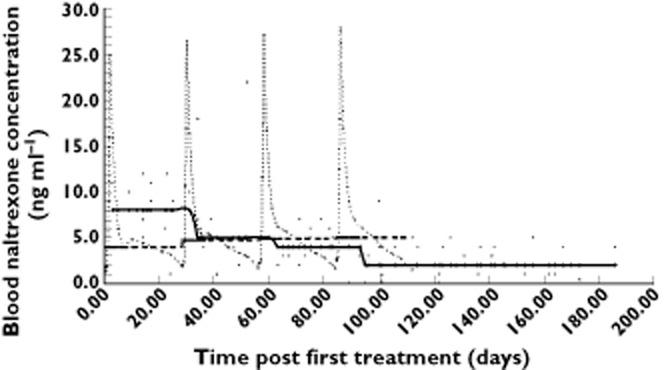
Bloon naltrexone concentration from a single 2.2 g implant vs. repeated Vivitrol injection.  , Vivitrol – Dose 1;
, Vivitrol – Dose 1;  , Vivitrol – Dose 2;
, Vivitrol – Dose 2;  , Vivitrol – Dose 3;
, Vivitrol – Dose 3;  , Vivitrol – Dose 4;
, Vivitrol – Dose 4;  , 2.2 g implant – observed;
, 2.2 g implant – observed;  , median naltrexone concentration per Vivitor dose;
, median naltrexone concentration per Vivitor dose;  , median naltrexone concentration per month from 2.2 g implant
, median naltrexone concentration per month from 2.2 g implant
Data indicate this naltrexone implant is biocompatible [33], biodegradable [34] and clinically safe [35–37]. In an assessment for the treatment of heroin dependence a single implant was shown to be superior to daily oral naltrexone on many outcome measures to 6 months, including relapse to heroin [38] or regular heroin use [39]. Further patients treated with this naltrexone implant had a significantly lower risk of returning to regular heroin use than patients who complied with daily oral naltrexone use [38]. This suggests that, in addition to overcoming the non-compliance issue associated with oral naltrexone, implant naltrexone may also improve clinical outcomes, possibly by delivering a more constant concentration of naltrexone (than the oral formula).
Naltrexone implant and alcohol dependence treatment
To date there has been no randomized controlled trial (RCT) to assess the effectiveness of this naltrexone implant (or a similarly long acting sustained release naltrexone formulation) as a treatment for alcohol dependence. Nevertheless, case series clinical outcome data were reviewed in 47 alcohol dependent persons treated with naltrexone implants. Thirty-six of these patients had treatment outcome data at 6 months, with 22 (60%) not drinking. Overall those reviewed showed lower levels of alcohol use and improved quality of life post- compared with pre-treatment (Author's unpublished data). Additionally, a review of hospital or emergency department admissions and use of mental health services utilizing State Health Department records of 124 alcohol dependent persons treated with this implant showed a decrease in hospital or emergency department admissions and use of mental health services compared with pre-treatment levels (Author's unpublished data). Issues of patient acceptability of naltrexone implant treatment for alcohol dependence, which requires a surgical procedure compared with monthly injection with depot products, can only be resolved when both treatment options are made widely available.
Pharmacokinetics of naltrexone and their predictive role in treatment outcomes
Only limited research has assessed the significance of blood naltrexone and 6β-naltrexol concentrations in predicting alcoholism treatment outcomes. In a study of 23 heavy drinkers, McCaul et al. [40] found that higher serum 6β-naltrexol was strongly associated with lower ratings of alcohol liking and effect. These authors also found a significant positive relationship between 6β-naltrexol concentrations and ratings of sedation before drinking (P = 0.002). Pharmacokinetic data indicate that standard oral naltrexone treatment (50 mg), which has shown moderate to good clinical efficacy in the management of alcohol dependence [5, 6], is likely to result in peak blood concentrations of approximately 8.5 ng ml−1 and trough concentrations of less than 0.2 ng ml−1 within 12 h [41]. However, higher doses of oral naltrexone (150 mg day−1) have been shown to reduce significantly alcohol consumption (percentage of drinking days, P < 0.0001 and number of drinks per drinking day, P < 0.0001) among those with strong craving, without significant adverse effects [42]. Nevertheless, these authors did not report pharmacokinetic data. Further, the depot naltrexone Vivitrol (delivered at 380 mg) had greater clinical efficacy than a 190 mg Vivitrol dose [23]. Collectively, these data suggest that different blood naltrexone concentrations associated with oral or depot preparations likely produce a dose−response difference in clinical outcomes for the management of alcohol dependence. As such, they raise the question of the optimum naltrexone dosing.
Despite the variety of naltrexone release profiles provided by different sustained release products or oral naltrexone dosing, there is no consensus on blood naltrexone concentrations required to provide effective management of problem alcohol use or to direct the development of new more effective products. This contrasts with increasing knowledge of effective blood concentrations for the management of heroin dependence where blood naltrexone concentrations between 1 and 2 ng ml−1 have been generally cited to provide therapeutic coverage against the effect of heroin [18]. Further, data from the author's recent RCT have shown the odds of returning to weekly or more frequent heroin use to increase 2.5 times when blood naltrexone concentrations dropped below 0.5 ng ml−1 [38]. The same study also found an increment of 1 ng ml−1 in blood naltrexone concentration was associated with 35% reduction in odds of return to use. Clearly studies to assess the pharmacokinetic profile of naltrexone and its predictive role in alcohol treatment outcomes are urgently required.
Psychiatric morbidity and naltrexone
A growing body of research has sought to evaluate mental health outcomes of patients following naltrexone pharmacotherapy treatment, both those with a history of psychiatric morbidity, and the emergence of psychiatric morbidity in those without previous mental health morbidity. Specifically, concern has been raised of a possible increase in the incidence of depression or dysphoric mood disorder following treatment with naltrexone, due to its antagonistic effect on endogenous opioid receptors [43–45]. However, the evidence for this has been mixed, with some investigators reporting mild dysphoria in ‘healthy, drug free’ persons following administration of naltrexone [43, 46], while others have reported no change in incidence of depression [44] or an improvement in depressive symptoms among depressed alcoholics [47, 48].
Data on mental health outcomes associated with sustained release naltrexone are limited. As noted earlier, a review of 124 alcohol dependent patients treated with naltrexone implant showed a significant reduction in mental health admissions (64.1%) in the 12 months post- compared with pre-treatment (Author's unpublished data). Given the high prevalence of mental health disorders amongst persons with problem alcohol use there is an urgent need to determine mental health following naltrexone implant treatment for alcohol.
Treatment for a non-homogenous population
A major challenge for clinicians when prescribing any pharmacotherapy is determining which patients are most likely to benefit from any particular treatment. This is especially true when there are a number of treatment alternatives available and when the therapeutic effects are perceived as marginal as is the case with pharmacotherapies for alcohol dependence [16]. Persons seeking treatment for problem alcohol use are not a homogenous population. Alcohol use disorders have a highly variable phenotypic expression and are now understood to be the product of a complex interaction of genetic and environmental influences. Inter-individual variation occurs in personal genetic, environmental and clinical characteristics and pathways to dependence, such as family history of substance use disorders, the co-use of other drugs and presence of mental illness. Variation in response to treatment may manifest as adverse drug reactions and other side-effects of treatment, poor metabolism of treatment drugs resulting in different dosage requirements and lack of therapeutic efficacy. A number of different approaches have been taken by those seeking to understand why some people respond to treatment and others do not. These include but are not restricted to (i) identification of individual characteristics at treatment entry that predict treatment outcome, (ii) clusters of characteristics that identify clinical subtypes which may be associated with different treatment outcomes and (iii) identification of genes which affect treatment outcomes.
Identification of patient characteristics at treatment entry that predict treatment outcome
A number of individual variables have been found to moderate the effects of naltrexone on clinical outcomes in alcohol abuse/dependence treatment. These include high baseline craving for alcohol [49, 50], increased density of familial alcohol problems [49, 51–53], early onset of alcohol problems [53, 54], the co-use of other drugs [54] and compliance with oral naltrexone treatment [17]. Similarly, several factors have been identified as mediating compliance with oral naltrexone including recent diagnosis, younger age at treatment, less stable employment status, lower socio-economic status [15] and frequency of gastro-intestinal adverse event (i.e. nausea [52, 55] or fatigue [52]). Differing personal genetic characteristics and their possible impact on naltrexone treatment outcomes for alcohol dependence will be discussed in greater detail later in this paper.
Identification of clusters of characteristics to identify clinical subtypes
Researchers in the field of alcohol dependence have attempted to classify clinical subtypes based on a variety of indicators such as onset age, chronicity of problems, familial history, personality factors and patterns of substance abuse [56–58]. Using multivariate analysis, clusters of symptoms and traits are identified to produce substance dependence typologies which comprise more homogenous subsets of patients. The identification of clinical subtypes may improve diagnostic classification, facilitate clinical decision-making and improve the allocation of patients to different modalities and intensities of treatment services. This hypothesis is supported by evidence from the recent European Acamprosate Trials [59]. With particular reference to the Austrian Acamprosate double-blind, placebo-controlled trial, 260 patients were grouped according to the Lesch alcoholism topology, which took into account social, psychic and somatic factors. Type I (the ‘Allergy’ group, n = 94) is characterized by severe withdrawal syndromes, including also convulsions and psychotic symptoms. Type II (the ‘Conflict’ group, n = 64) is marked by conflicts and anxiety and/or personality disorders, as well as featuring aggression outbreaks under the influence of alcohol. Type III (the ‘Self-treatment’ group, n = 58) patients usually display pre-alcohol problems with mood, motivation, sleep or health, for which the patients often attempt to self-medicate with alcohol. Lastly, type IV (the ‘Adaptation’ group, n = 47) patients generally have existing cerebral damages and serious social problems. Acamprosate was shown to be more effective, compared with placebo, in lengthening the duration of abstinence in types I and II patients, but not types III and IV patients [59].
Similarly, a group of German investigators later examined the relative efficacy of acamprosate vs. naltrexone, across two different alcoholism topologies, Lesch's and Cloninger's [60]. In brief, Cloninger's dual typology distinguishes alcohol patients primarily based on onset of problem drinking (early in type II and late in type I) [57]. Also, while Cloninger's type II alcoholism is dominated by hereditary or familial factors and usually affects sons of male alcoholics, type I alcoholism is influenced by both genetic and environmental factors, and affects both genders [57]. In the mentioned study, 160 patients were randomized into one of four treatment groups: (i) acamprosate, (ii) naltrexone, (iii) acamprosate plus naltrexone and (iv) placebo, with n = 40 in each group [60]. Using Cloninger's typology, it was found that only type II patients responded to pharmacological treatments, with a five-fold increase in abstinence duration in the first three conditions, as compared with the placebo condition. With respect to Lesch's topology, in line with the Austrian Acamprosate study, type I patients responded better to acamprosate, whereas type III and IV patients most benefited from naltrexone treatment [60].
With the publication of DSM-V anticipated in 2013 and ICD-11 anticipated in 2015, the debate around diagnostic classifications and their utility has been given renewed relevance and has been the subject of considerable discussion [61, 62]. The proposed merging of dependence and abuse into an umbrella substance use disorder classification is likely to result in even more heterogeneity within this diagnostic classification, and is at odds with research identifying subgroups of patients who require different treatment approaches.
Pharmacogenetics of naltrexone treatment
Pharmacogenetics is the study of how variations in the DNA sequence of specific genes affect drug response phenotypes. Genetic polymorphisms in genes coding for metabolizing enzymes, transporter proteins (p-glycoprotein, P-gp), dopamine receptors and μ-opioid receptors may explain part of the observed interindividual variation in the response to alcohol dependence treatment with naltrexone. Genetic studies using candidate genes are being conducted to understand the underpinnings of the differential responses to treatment agents among alcohol dependence subtypes.
i. Opioid receptor related genes
There are three types of opioid receptors classified according to their specific ligands, the μ-opioid receptor (OPRM1), the κ-opioid receptor (OPRK1) and the δ-opioid receptor (OPRD1). Naltrexone is a specific opioid antagonist targeting primarily, but not exclusively, the μ-opioid receptor. There is a high concentration of μ-opioid receptors in areas of the brain that have been implicated in the reward pathway associated with alcohol and the μ-opioid receptor is increasingly becoming a main focus in genetic studies of alcohol addiction. Previous studies have reported a complete (or saturating) blockade of μ-opioid receptors [63, 64], but only partial (21–35% occupancy) blockade of δ-opioid receptors [64], following a 50 mg oral naltrexone dose.
It has been suggested that a polymorphism (G118A) located in exon 1 of the OPRM1 gene resulting in either an asparagine (asp40; G allele) or an aspartate amino acid substitute for asparagine (asn40; A allele) associated with position 40 in the μ-opioid type 1 (OPRM1) receptor, upon which both the endogenous opioid β-endorphin and naltrexone exert their opiate agonist or antagonist/blockade effect, respectively, may significantly affect alcohol treatment outcomes associated with naltrexone treatment [65, 66]. In some early studies, these Asp40 allele carriers showed greater alcohol sensitivity [67] and alcohol cue-induced craving [68] than non-Asp40 allele carriers. Receptors with Asp40 (encoded by the 118G allele) have been shown to bind β-endorphin with greater affinity [69, 70]. Treatment data on oral naltrexone also suggest that alcohol dependent individuals with at least one copy of the Asp40 allele have a significantly lower risk of relapse and a longer time to return to heavy alcohol use compared with those with a homozygous Asn40 allele [71]. More recently this finding has been supported by a large multi-site US study which showed that when alcohol dependent patients treated with oral naltrexone were divided into polymorphism by an amino acid Asp40 or Asn40, those with Asp40 showed significantly better clinical outcomes associated with oral naltrexone (increased days of abstinence, decreased heavy drinking days, with a greater percentage having good clinical outcomes) compared with their Asn40 polymorphism counterparts [66, 72].
It has been estimated that, among the substance dependent populations, as low as 1.3% of African Americans [73] or as high as 15.5% of European Americans and 42% of Asians [74] carry the Asp40 allele. This suggests that management of alcohol dependence with naltrexone might have a greater efficacy in populations with high Asp40 allele prevalence, such as Asians, and lower efficacy in those with low Asp40 allele prevalence, such as African Americans. This is supported by finding that Asians with the Asp40 allele had lower alcohol craving on naltrexone, compared with placebo and to Asn40-homozygotes [75]. Similarly, oral naltrexone was found to have greater efficacy in Caucasians than subjects of African descent (with lower Asp40 allele prevalence) [8]. Nevertheless, an extension of Ray et al.'s study [75], using behavioural economic measures, found naltrexone effective in decreasing intensity of alcohol demand among Asn40-homozygotes, rather than among Asp allele carriers [76]. Recent work by Anton and associates [77] suggests that the Asp allele mediated naltrexone response may not be straightforward and may also be mediated by dopamine transporter (SLC6A3) genes.
ii. Naltrexone metabolism
Although naltrexone, methadone or buprenorphine all exert their primary action through binding to the μ-opioid receptor, the metabolism of naltrexone is quite distinct. Specifically, the cytochrome P450 enzymes, which are significantly involved in metabolism of methadone or buprenorphine, do not play a role in naltrexone metabolism. Naltrexone is largely metabolized by the aldo-keto reductase family of enzymes (AKR1C1, 1C2 and 1C4) [78] with AKR1C4 the most efficient [79]. The effect of polymorphisms of AKR1C enzymes in response to naltrexone treatment for alcohol abuse/dependence has yet to be investigated. However it has been postulated that a polymorphism of the AKR1C4 enzyme is responsible for inter-individual variability in 6β-naltrexol concentrations and could play a role in the efficacy of and compliance with naltrexone treatment [78].
It is possible that enhanced, compared with normal or low, metabolism of naltrexone will result in reduced naltrexone bioavailability following equivalent dosing with either oral or a sustained release naltrexone preparation. Consequently, rapid metabolism of naltrexone can lead to poorer treatment outcomes, including reduced time of alcohol absence, increased alcohol craving and higher risk of return to alcohol or dependent alcohol use. The contribution of the 6β-naltrexol metabolite to naltrexone's therapeutic effect is unclear. However, in a study mentioned earlier, higher serum 6β-naltrexol concentration was strongly associated with lower ratings of alcohol liking and effect among 23 heavy drinkers [40]. This suggests the need for, and perhaps the possibility of, identifying prospective patients as slow, ‘normal’ or rapid naltrexone metabolizers by use of candidate gene screening. Such genetic profiling will likely assist clinicians in determining the acceptability of a treatment type, dosage, and duration of treatment necessary to optimize more fully clinical outcomes for any individual patient.
iii. Genome wide techniques
The recent development of genome wide techniques has made it possible to move beyond the traditional approach of investigating known genes in known pathways to identify unanticipated candidate genes that may contribute to treatment response. The hypothesis free approach of the Genome Wide Association Study (GWAS) can potentially discover novel associations with drug response phenotypes, even though the biological mechanism of their effect may be unclear [80]. While drug response phenotypes, such as poor drug metabolism or severe adverse drug reactions, may be monogenetic traits, drug efficacy as defined by continued abstinence in the case of substance abuse treatments is very likely a function of a multitude of genetic and non-genetic factors and their interaction effects. The candidate gene approach is appropriate for investigating hypothesis driven associations. Although the effect sizes of some of these associations may be small, they will provide a starting point for further research. The key to the success of both targeted gene and GWAS is precise measurement of drug exposure and consistent, accurate and extensive characterization of drug response phenotype [80].
Conclusions
Pharmacotherapeutic interventions are widely recognized as central to the treatment of problem alcohol use but continue to have highly variable results, prompting the question of why some individuals respond to treatment and others do not. While the clinical efficacy of oral naltrexone in the management of alcohol dependence has been limited with many patients failing to use their daily medication, some patients have achieved good clinical outcomes.
The development of sustained release naltrexone products that remove the need for daily oral naltrexone use have improved, and will continue to improve significantly clinical outcomes for persons who suffer alcohol abuse/dependence. There is a clear need for large scale clinical trials to address a range of issues that remain outstanding. The identification of clinically relevant blood concentrations to ensure maintenance of therapeutic blood concentrations, and to inform the development of new sustained release naltrexone products specifically for the management of alcohol abuse/dependence is essential to clinical improvement. Further, the identification of treatment entry clinical markers, which identify those patients most likely to benefit from naltrexone treatment and determine which patients are better suited to oral vs. a particular sustained release naltrexone delivery profile, will be extremely useful to clinicians.
Given the complexity of factors that contribute to the development of alcohol addiction it is likely that multiple factors contribute to any single alcohol dependent patient's responsiveness to treatment with naltrexone, susceptibility to relapse and associated morbidity (alcohol, mental health and general) and mortality. It is now increasingly clear that genetic variables, environmental factors and their interaction are major factors mediating response to treatment. The identification of genes that influence the pharmacokinetic and pharmacodynamic actions of naltrexone as a management for alcohol dependence, genes that predispose the patient to a higher risk of relapse, and how they interact with the patient's baseline characteristics and available environment will ultimately enable the development of more personalized treatment. Recognition of the heterogeneity of this patient group, provision of the widest possible range of safe, evidence based treatment options and a comprehensive understanding of the inter-individual variability in response to those treatments will improve the efficacy of both currently available and future treatments. These advances in our understanding of alcohol addiction and the development of targeted treatment interventions will most certainly ease the burden and cost of addiction for individuals, families and society.
Competing Interests
The author has completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request) and declares no support from any organization for the submitted work, the author (GH) had entered into a contractual arrangement with Go Medical Industries (who manufactures the Australian naltrexone implant) to conduct a number of research studies in the previous 3 years and the author (GH) has co-authored with Dr George O'Neil (Director, Go Medical Industries) on a number of previous publications.
References
- 1.Chesterton GK. Wine When It Is Red. Cambridge: Harvard University: J. Lane Company; 1910. All Things Considered. [Google Scholar]
- 2.WHO. Alcohol [database on the Internet] 2011. Available at http://www.who.int/mediacentre/factsheets/fs349/en/index.html (last accessed 4 April 2012)
- 3.Collins DJ, Lapsley HM. The Costs of Tobacco, Alcohol and Illicit Drug Abuse to Australian Society in 2004/05. Canberra, ACT: Commonwealth of Australia; 2008. [Google Scholar]
- 4.Balakrishnan R, Allender S, Scarborough P, Webster P, Rayner M. The burden of alcohol-related ill health in the United Kingdom. J Public Health. 2009;31:366–373. doi: 10.1093/pubmed/fdp051. [DOI] [PubMed] [Google Scholar]
- 5.Latt NC, Jurd S, Houseman J, Wutzke SE. Naltrexone in alcohol dependence: a randomised controlled trial of effectiveness in a standard clinical setting. Med J Aust. 2002;176:530–534. doi: 10.5694/j.1326-5377.2002.tb04550.x. [DOI] [PubMed] [Google Scholar]
- 6.Morris PL, Hopwood M, Whelan G, Gardiner J, Drummond E. Naltrexone for alcohol dependence: a randomized controlled trial. Addiction. 2001;96:1565–1573. doi: 10.1046/j.1360-0443.2001.961115654.x. [DOI] [PubMed] [Google Scholar]
- 7.Garbutt JC. Efficacy and tolerability of naltrexone in the management of alcohol dependence. Curr Pharm Des. 2010;16:2091–2097. doi: 10.2174/138161210791516459. [DOI] [PubMed] [Google Scholar]
- 8.Kranzler HR, Van Kirk J. Efficacy of Naltrexone and Acamprosate for alcoholism treatment: a meta-analysis. Alcohol Clin Exp Res. 2001;25:1335–1341. [PubMed] [Google Scholar]
- 9.Mitchell JM, Bergren LJ, Chen KS, Rowbotham MC, Fields HL. Naltrexone aversion and treatment efficacy are greatest in humans and rats that actively consume high levels of alcohol. Neurobiol Dis. 2009;33:72–80. doi: 10.1016/j.nbd.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Carmen B, Angeles M, Ana M, Maria AJ. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction. 2004;99:811–828. doi: 10.1111/j.1360-0443.2004.00763.x. [DOI] [PubMed] [Google Scholar]
- 11.Walters D, Connor J, Feeney GF, Yooung RM. The cost effectiveness of naltrexone added to cognitive-behavioral therapy in the treatment of alcohol dependence. J Addict Dis. 2009;28:137–144. doi: 10.1080/10550880902772456. [DOI] [PubMed] [Google Scholar]
- 12.Srisurapanont M, Jarusuraisin N. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2005;(1) doi: 10.1002/14651858.CD001867.pub2. CD001867. [DOI] [PubMed] [Google Scholar]
- 13.Kranzler HR, Armeli S, Feinn R, Tennen H. Targeted naltrexone treatment moderates the relations between mood and drinking behavior among problem drinkers. J Consult Clin Psychol. 2004;72:317–327. doi: 10.1037/0022-006X.72.2.317. [DOI] [PubMed] [Google Scholar]
- 14.Volpicelli JR, Rhines KC, Rhines JS, Volpicelli LA, Alterman AI, O'Brien CP. Naltrexone and alcohol dependence. Role of subject compliance. Arch Gen Psychiatry. 1997;54:737–742. doi: 10.1001/archpsyc.1997.01830200071010. [DOI] [PubMed] [Google Scholar]
- 15.Kranzler HR, Stephenson JJ, Montejano L, Shaohung W, Gastfriend DR. Persistence with oral naltrexone for alcohol treatment: implications for health-care utilization. Addiction. 2008;103:1801–1808. doi: 10.1111/j.1360-0443.2008.02345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mark TL, Kranzler HR, Poole VH, Hagen CA, McLeod C, Crosse S. Barriers to the use of medications to treat alcoholism. Am J Addict. 2003;12:281–294. [PubMed] [Google Scholar]
- 17.Baros AM, Latham PK, Moak DH, Voronin K, Anton RF. What role does measuring medication compliance play in evaluating the efficacy of naltrexone? Alcohol Clin Exp Res. 2007;31:596–603. doi: 10.1111/j.1530-0277.2007.00343.x. [DOI] [PubMed] [Google Scholar]
- 18.Comer SD, Sullivan MA, Hulse GK. Sustained-release naltrexone: novel treatment for opioid dependence. Expert Opin Investig Drugs. 2007;16:1285–1294. doi: 10.1517/13543784.16.8.1285. [DOI] [PubMed] [Google Scholar]
- 19.Olsen JL, Kincl FA. A review of parental sustained-release naltrexone systems. In: Willette RE, Barnett G, editors. Naltrexone Research Monograph. Rockville, MD: National Institute on Drug Abuse; 1980. pp. 187–264. [Google Scholar]
- 20.Chiang CN, Hollister LE, Gillespie HK, Foltz RL. Clinical evaluation of a naltrexone sustained-release preparation. Drug Alcohol Depend. 1985;16:1–8. doi: 10.1016/0376-8716(85)90076-6. [DOI] [PubMed] [Google Scholar]
- 21.Chiang CN, Hollister LE, Kishimoto A, Barnett G. Kinetics of a naltrexone sustained-release preparation. Clin Pharmacol Ther. 1984;36:704–708. doi: 10.1038/clpt.1984.243. [DOI] [PubMed] [Google Scholar]
- 22.Galloway GP, Koch M, Cello R, Smith DE. Pharmacokinetics, safety, and tolerability of a depot formulation of naltrexone in alcoholics: an open-label trial. BMC Psychiatry. 2005;5:18. doi: 10.1186/1471-244X-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garbutt JC, Kranzler HR, O'Malley SS, Gastfriend DR, Pettinati HM, Silverman BL, Loewy JW, Ehrich EW Vivitrex Study Group. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: a randomized controlled trial. JAMA. 2005;293:1617–1625. doi: 10.1001/jama.293.13.1617. [DOI] [PubMed] [Google Scholar]
- 24.Kranzler HR, Wesson DR, Billot L. Naltrexone depot for treatment of alcohol dependence: a multicenter, randomized, placebo-controlled clinical trial. Alcohol Clin Exp Res. 2004;28:1051–1059. doi: 10.1097/01.alc.0000130804.08397.29. [DOI] [PubMed] [Google Scholar]
- 25.Kranzler HR, Modesto-Lowe V, Nuwayser ES. Sustained-release naltrexone for alcoholism treatment: a preliminary study. Alcohol Clin Exp Res. 1998;22:1074–1079. [PubMed] [Google Scholar]
- 26.Johnson BA, Ait-Daoud N, Aubin H-J, van den Brink W, Guzzetta R, Loewy J. A pilot evaluation of the safety and tolerability of repeat dose administration of long-acting injectable naltrexone (Vivitrex (R)) in patients with alcohol dependence. Alcohol Clin Exp Res. 2004;28:1356–1361. doi: 10.1097/01.alc.0000139823.30096.52. [DOI] [PubMed] [Google Scholar]
- 27.O'Malley SS, Garbutt JC, Gastfriend DR, Dong Q, Kranzler HR. Efficacy of extended-release aaltrexone in alcohol-dependent patients who are abstinent before treatment. J Clin Psychopharmacol. 2007;27:507–512. doi: 10.1097/jcp.0b013e31814ce50d. [DOI] [PubMed] [Google Scholar]
- 28.Ciraulo DA, Dong Q, Silverman BL, Gastfriend DR, Pettinati HM. Early treatment response in alcohol dependence with extended-release naltrexone. J Clin Psychiatry. 2008;69:190–195. doi: 10.4088/jcp.v69n0204. [DOI] [PubMed] [Google Scholar]
- 29.Gastfriend DR. Intramuscular extended-release naltrexone: current evidence. Ann N Y Acad Sci. 2011;1216:144–166. doi: 10.1111/j.1749-6632.2010.05900.x. [DOI] [PubMed] [Google Scholar]
- 30.King AC, Volpicelli JR, Gunduz M, O'Brien CP, Kreek MJ. Naltrexone biotransformation and incidence of subjective side effects: a preliminary study. Alcohol Clin Exp Res. 1997;21:906–909. [PubMed] [Google Scholar]
- 31.Ngo HTT, Arnold-Reed DE, Hansson RC, Tait RJ, Hulse GK. Blood naltrexone levels over time following naltrexone implant. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:23–28. doi: 10.1016/j.pnpbp.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Dunbar JL, Turncliff RZ, Dong Q, Silverman BL, Ehrich EW, Lasseter KC. Single- and multiple-dose pharmacokinetics of long-acting injectable naltrexone. Alcohol Clin Exp Res. 2006;30:480–490. doi: 10.1111/j.1530-0277.2006.00052.x. [DOI] [PubMed] [Google Scholar]
- 33.Hulse GK, Stalenberg V, McCallum D, Smit W, O'Neil G, Morris N, Tait RJ. Histological changes over time around the site of sustained release naltrexone-poly(DL-Lactide) implants in humans. J Control Release. 2005;108:43–55. doi: 10.1016/j.jconrel.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 34.Hulse GK, Low VHS, Stalenberg V, Morris N, Thompson RI, Tait RJ, Phan CT, Ngo HTT, Arnold-Reed DE. Biodegradability of naltrexone-poly(DL) lactide implants in vivo assessed under ultrasound in humans. Addict Biol. 2007;11:364–372. doi: 10.1111/j.1369-1600.2007.00081.x. [DOI] [PubMed] [Google Scholar]
- 35.Kunoe N, Lobmaier P, Vederhus JK, Hjerkinn B, Hegstad S, Gossop M, Kristensen O, Waal H. Naltrexone implants after in-patient treatment for opioid dependence: randomised controlled trial. Br J Psychiatry. 2009;194:541–546. doi: 10.1192/bjp.bp.108.055319. [DOI] [PubMed] [Google Scholar]
- 36.Kunoe N, Lobmaier P, Vederhus JK, Hjerkinn B, Hegstad S, Gossop M, Kristensen O, Waal H. Retention in naltrexone implant treatment for opioid dependence. Drug Alcohol Depend. 2010;111:166–169. doi: 10.1016/j.drugalcdep.2010.03.021. [Short communication] [DOI] [PubMed] [Google Scholar]
- 37.Lobmaier P, Kunoe N, Gossop M, Katevoll T, Waal H. Naltrexone implants compared to methadone: outcomes six months after prison release. Eur Addict Res. 2010;16:139–145. doi: 10.1159/000313336. [DOI] [PubMed] [Google Scholar]
- 38.Hulse GK, Ngo HTT, Tait RJ. Risk factors for craving and relapse in heroin users treated with oral or implant naltrexone. Biol Psychiatry. 2010;68:296–302. doi: 10.1016/j.biopsych.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Hulse GK, Morris N, Arnold-Reed DE, Tait RJ. Improving clinical outcomes in treating heroin dependence: randomized, controlled trial of oral or implant naltrexone. Arch Gen Psychiatry. 2009;66:1108–1115. doi: 10.1001/archgenpsychiatry.2009.130. [DOI] [PubMed] [Google Scholar]
- 40.McCaul ME, Wand GS, Rohde C, Lee SM. Serum 6-beta-naltrexol levels are related to alcohol responses in heavy drinkers. Alcohol Clin Exp Res. 1985;24:1385–1391. [PubMed] [Google Scholar]
- 41.Meyer MC, Straughn AB, Lo MW, Schary WL, Whitney CC. Bioequivalence, dose-proportionality, and pharmacokinetics of naltrexone after oral administration. J Clin Psychiatry. 1984;45(9 Pt 2):15–19. [PubMed] [Google Scholar]
- 42.Yoon G, Kim SW, Thuras P, Westermeyer J. Safety, tolerability, and feasibility of high-dose naltrexone in alcohol dependence: an open-label study. Hum Psychopharmacol. 2011;26:125–132. doi: 10.1002/hup.1183. [DOI] [PubMed] [Google Scholar]
- 43.Crowley TJ, Wagner JE, Zerbe G, Macdonald MJ. Naltrexone-induced dysphoria in former opioid addicts. Am J Psychiatry. 1985;142:1081–1084. doi: 10.1176/ajp.142.9.1081. [DOI] [PubMed] [Google Scholar]
- 44.Miotto K, McCann M, Basch J, Rawson R, Ling W. Naltrexone and dysphoria: fact or myth? Am J Addict. 2002;11:151–160. doi: 10.1080/10550490290087929. [DOI] [PubMed] [Google Scholar]
- 45.Ritter AJ. Naltrexone in the treatment of heroin dependence: relationship with depression and risk of overdose. Aust N Z J Psychiatry. 2002;36:224–228. doi: 10.1046/j.1440-1614.2002.01012.x. [DOI] [PubMed] [Google Scholar]
- 46.Mendelson JH, Ellingboe J, Keuhnie JC, Mello NK. Effects of naltrexone on mood and neuroendocrine function in normal adult males. Psychoneuroendocrinology. 1979;3:231–236. doi: 10.1016/0306-4530(78)90013-6. [DOI] [PubMed] [Google Scholar]
- 47.Pettinati HM, Oslin DW, Kampman KM, Dundon WD, Xie H, Gallis TL, Dackis CA, O'Brien CP. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occuring depression and alcohol dependence. Am J Psychiatry. 2010;167:668–675. doi: 10.1176/appi.ajp.2009.08060852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salloum IM, Cornelius JR, Thase ME, Daley DC, Kirisci L, Spotts C. Naltrexone utility in depressed alcoholics. Psychopharmacol Bull. 1998;34:111–115. [PubMed] [Google Scholar]
- 49.Monterosso JR, Flannery BA, Pettinati HM, Oslin DW, Rukstalis M, O'Brien CP, Volpicelli JR. Predicting treatment response to naltrexone: the influence of craving and family history. Am J Addict. 2001;10:258–268. doi: 10.1080/105504901750532148. [DOI] [PubMed] [Google Scholar]
- 50.Volpicelli JR, Watson NT, King AC, Sherman CE, O'Brien CP. Effect of naltrexone on alcohol ‘high’ in alcoholics. Am J Psychiatry. 1995;152:613–615. doi: 10.1176/ajp.152.4.613. [DOI] [PubMed] [Google Scholar]
- 51.Tidey JW, Monti PM, Rohsenow DJ, Gwaltney CJ, Miranda R, Jr, McGeary JE, MacKillop J, Swift RM, Abrams DB, Shiffman S, Paty JA. Moderators of naltrexone's effects on drinking, urge, and alcohol effects in non-treatment-seeking heavy drinkers in the natural environment. Alcohol Clin Exp Res. 2008;32:58–66. doi: 10.1111/j.1530-0277.2007.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rohsenow DJ, Colby SM, Monti PM, Swift RM, Martin RA, Mueller TI, Gordon A, Eaton CA. Predictors of compliance with naltrexone among alcoholics. Alcohol Clin Exp Res. 2000;24:1542–1549. [PubMed] [Google Scholar]
- 53.Rubio G, Ponce G, Rodriguez-Jimenez R, Jimenez-Arriero MA, Hoenicka J, Palomo T. Clinical predictors of response to naltrexone in alcoholic patients: who benefits most from treatment with naltrexone? Alcohol Alcohol. 2005;40:227–233. doi: 10.1093/alcalc/agh151. [DOI] [PubMed] [Google Scholar]
- 54.Rubio G, Jimenez-Arriero MA, Ponce G, Palomo T. Naltrexone versus acamprosate: one year follow-up of alcohol dependence treatment. Alcohol Alcohol. 2001;36:419–425. doi: 10.1093/alcalc/36.5.419. [DOI] [PubMed] [Google Scholar]
- 55.Oncken C, Van Kirk J, Kranzler HR. Adverse effects of oral naltrexone: analysis of data from two clinical trials. Psychopharmacology. 2001;154:397–402. doi: 10.1007/s002130000666. [DOI] [PubMed] [Google Scholar]
- 56.Babor TF, Grant M. Project on Identification and Management of Alcohol-Related Problems. Report on Phase II: A Randomized Clinical Trial of Brief Interventions in Primary Health Care. Geneva: World Health Organization; 1992. [Google Scholar]
- 57.Cloninger C, Sigvardsson S, Bohman M. Type 1 and Type 2 alcoholism: an update. Alcohol Health Res World. 1996;20:18–23. [PMC free article] [PubMed] [Google Scholar]
- 58.Lesch OM, Walter H. Subtypes of alcoholism and their role in therapy. Alcohol Alcohol Suppl. 1996;1:63–67. [PubMed] [Google Scholar]
- 59.Lesch OM, Riegler A, Gutierrez K, Hertling I, Ramskogler K, Semler B, Zoghlami A, Benda N, Walter H. The European acamprosate trials: conclusions for research and therapy. J Biomed Sci. 2001;8:89–95. doi: 10.1007/BF02255976. [DOI] [PubMed] [Google Scholar]
- 60.Kiefer F, Helwig H, Tarnaske T, Otte C, Jahn H, Wiedemann K. Pharmacological relapse prevention of alcoholism: clinical predictors of outcome. Eur Addict Res. 2005;11:83–91. doi: 10.1159/000083037. [DOI] [PubMed] [Google Scholar]
- 61.Grove R, McBride O, Slade T. Towards DSM-V: exploring diagnostic thresholds for alcohol dependence and abuse. Alcohol Alcohol. 2010;45:45–52. doi: 10.1093/alcalc/agp069. [DOI] [PubMed] [Google Scholar]
- 62.Lesch OM. [Addiction in DSM V and ICD-11 state of the art] J Public Health. 2009;77:507–512. doi: 10.1055/s-0028-1109590. [DOI] [PubMed] [Google Scholar]
- 63.Lee MC, Wagner HNJ, Tanada S, Frost JJ, Bice AN, Dannals RF. Duration of occupancy of opiate receptors by naltrexone. J Nucl Med. 1988;29:1207–1211. [PubMed] [Google Scholar]
- 64.McCaul ME, Wand GS, Kim YK, Bencherif B, Dannals RF, Frost JJ. Naltrexone effects on mu- and delta-opioid receptor availability in alcohol dependence. Alcohol Clin Exp Res. 2003;27(S6):21A. [Google Scholar]
- 65.Anton RF. Genetic basis for predicting response to naltrexone in the treatment of alcohol dependence. Pharmacogenomics. 2008;9:655–658. doi: 10.2217/14622416.9.6.655. [DOI] [PubMed] [Google Scholar]
- 66.Anton RF, Oroszi G, O'Malley S, Couper D, Swift R, Pettinati H, Goldman D. An evaluation of mu-opioid receptor (OPRM1) as a predictor of naltrexone response in the treatment of alcohol dependence: results from the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) study. Arch Gen Psychiatry. 2008;65:135–144. doi: 10.1001/archpsyc.65.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ray LA, Hutchison KE. A polymorphism of the μ-opioid receptor gene (OPRM1) and sensitivity to the effects of alcohol in humans. Alcohol Clin Exp Res. 2004;28:1789–1795. doi: 10.1097/01.alc.0000148114.34000.b9. [DOI] [PubMed] [Google Scholar]
- 68.van den Wildenberg E, Wiers RW, Dessers J, Janssen RGJH, Lambrichs EH, Smeets HJM, van Breukelen GJ. A functional polymorphism of the mu-opioid receptor gene (OPRM1) influences cue-induced craving for alcohol in male heavy drinkers. Alcohol Clin Exp Res. 2007;31:1–10. doi: 10.1111/j.1530-0277.2006.00258.x. [DOI] [PubMed] [Google Scholar]
- 69.Bond C, LaForge KS, Tian M, Melia D, Khang S, Borg L, Gong J, Schuler J, Stong JA, Leal SM, Tischfield JA, Kreel MJ, Yu L. Single-nucleotide polymorphism in the human mu opioid receptor gene alters f-endorphin binding and activity: possible implications for opiate addiction. Proc Natl Acad Sci U S A. 1998;95:9608–9613. doi: 10.1073/pnas.95.16.9608. [Journal] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hernandez-Avila CA, Wand G, Luo X, Kranzler HR. Association between the cortisol response to opioid blockade and the Asn40Asp polymorphism at the mu-opioid receptor locus (OPRM1) Am J Med Genet. 2003;118B:60–65. doi: 10.1002/ajmg.b.10054. [DOI] [PubMed] [Google Scholar]
- 71.Oslin DW, Berrettini W, Kranzler HR, Pettinati H, Gelernter J, Volpicelli JR, O'Brien CP. A functional polymorphism of the mu-opioid receptor gene is associated with naltrexone response in alcohol-dependent patients. Neuropsychopharmacology. 2003;28:1546–1552. doi: 10.1038/sj.npp.1300219. [DOI] [PubMed] [Google Scholar]
- 72.Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 73.Arias A, Feinn R, Kranzler HR. Association of and Asn40Asp (A118G) polymorphism in the mu opiod receptor gene with substance dependence: a meta-analysis. Drug Alcohol Depend. 2006;83:262–268. doi: 10.1016/j.drugalcdep.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 74.Gelernter J, Kranzler H, Cubells J. Genetics of two mu opioid receptor gene (OPRM1) exon I polymorphisms: population studies, and allele frequencies in alcohol- and drug-dependent subjects. Mol Psychiatry. 1999;4:476–483. doi: 10.1038/sj.mp.4000556. [DOI] [PubMed] [Google Scholar]
- 75.Ray LA, Bujarski S, Chin PF, Miotto K. Pharmacogenetics of naltrexone in Asian Americans: a randomized placebo-controlled laboratory study. Neuropsychopharmacology. 2012;37:445–455. doi: 10.1038/npp.2011.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bujarski S, MacKillop J, Ray LA. Understanding naltrexone mechanism of action and pharmacogenetics in Asian Americans via behavioral economics: a preliminary study. Exp Clin Psychopharmacol. 2012;20:181–190. doi: 10.1037/a0027379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Anton RF, Voronin KK, Randall PK, Myrick H, Tiffany A. Naltrexone modification of drinking effects in a subacute treatment and bar-lab paradigm: influence of OPRM1 and dopamine transporter (SLC6A3) Genes. Alcohol Clin Exp Res. 2012 doi: 10.1111/j.1530-0277.2012.01807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Porter SJ, Somogyi AA, White JM. Kinetics and inhibition of the formation of 6β-naltrexol from naltrexone in human liver cytosol. Br J Clin Pharmacol. 2000;50:465–471. doi: 10.1046/j.1365-2125.2000.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Breyer-Pfaff U, Nill K. Carbonyl reduction of naltrexone and dolasetron by oxidoreductases isolated from human liver cytosol. J Pharm Pharmacol. 2004;56:1601–1606. doi: 10.1211/0022357045020. [DOI] [PubMed] [Google Scholar]
- 80.Guessous I, Gwinn M, Khoury MJ. Genome-wide association studies in pharmacogenomics: untapped potential for translation. Genome Med. 2009;1:46. doi: 10.1186/gm46. [DOI] [PMC free article] [PubMed] [Google Scholar]


