Abstract
Intestine perforation is one of the most dreaded and common complication of typhoid fever remarkably so in developing world; it usually leads to diffuse peritonitis, requiring early surgical intervention. Despite various measures such as safe drinking water supply and safe disposal of waste, intestinal perforation from salmonellosis remains the most common emergency surgery performed. The incidence continues to rise, so also the mortality, despite new antibiotics and improvement in surgical technique. More disturbing is that we now see increasing number of ileal perforations and colonic involvement. We hereby present a case report of 35-year-old male with multiple (24) intestinal perforation in the Ileum and Cecum.
Keywords: Asia, Multiple ileal perforations, Salmonellosis
Introduction
Intestinal perforation is a common cause of peritonitis necessitating emergency surgical intervention. Perforation of the bowel from typhoid perforation is a serious abdominal complication. The prevalence of typhoid fever is gradually decreasing worldwide; however, it still remains endemic in the Indian subcontinent.[1] Although, intestinal hemorrhage is the most common complication of typhoid fever yet intestinal perforation continues to be the most frequent cause of its high morbidity and mortality.[2] In general, hemorrhage and perforation occur in the terminal ileum secondary to necrosis of Peyer's patches at 2-3 weeks after the onset of the disease. Mortality rates of typhoid intestinal perforation (TIP) cases are reported to be between 5% to 62%.[3,4] Perforation of terminal ileum is a cause for acute obscure peritonitis, heralded by exacerbation of abdominal pain associated with tenderness, rigidity and guarding, most pronounced over right iliac fossa. However, for many patients in a severe toxic state, there may be obscured clinical features with resultant delays in diagnosis and adequate surgical intervention.[5] While early surgical procedures are regarded as definitive treatments along with pre-operative resuscitation and post-operative intensive care, the methods that should be used in surgery are still contentious. In the present case report, we present a rare case of 24 perforations in the terminal ileum and cecum of a patient. To the best of our knowledge, this is the 3rd highest number of intestinal perforations from typhoid in an adult patients reported in the literature.[6,7]
Case Report
A 35-year-old male patient was admitted in surgery out-patient department with complains of fever for 2 weeks, abdominal pain and vomiting for 4 days, abdominal distension for 2 days, and constipation for 2 days. He did not receive any treatment during 2 weeks. There was no history of chronic abdominal pain or analgesic abuse, but patient was a smoker and alcoholic. There was no any history suggestive of previous typhoid infection. On physical examination, abdomen was tense, tender, and distended with absent bowel sound. Both guarding and rigidity were present all over the abdomen. On digital rectal examination, there was empty rectum. An upright abdominal radiograph showed free gas under both domes of diaphragm. Laboratory examinations gave the following results: Hematocrit 30%, white blood cell count 14500/cm3, platelets 268 000/cm3, sodium 138 mEq/L, potassium 3.2 mEq/L, blood urea 32 mg/dl, S. Creatinine 1.6 mg/dl, blood glucose 110 mg/dl, and total bilirubin of 2.5 mg/dl. Diagnostic test for hepatitis B, hepatitis C and HIV were negative. The patient was Widal positive (Titer of > 1:160). An abdominal ultrasound showed features consistent with intestinal perforation showing both free fluid and free air with fine floating echoes in peritoneal cavity. However, blood culture was negative for Salmonella typhi in the patient. No bile culture was performed pre-operatively. Hence, the diagnosis of acute peritonitis due to intestinal perforation was made pre-operatively.
The patient was resuscitated with intravenous fluid and commenced on antibiotics ceftriaxone and metronidazole pre-operatively. Nasogastric tube insertion for decompression and urethral catheterization was carried out for monitoring urine output. Exploratory laparotomy was performed through midline incision and fecal peritonitis with exudative flakes all over the intestine was found. Thorough peritoneal lavage was carried out with normal saline. There were 24 perforations (21 in terminal ileum and 3 in cecum) present in distal 35-40 cm of terminal ileum reaching up to ileocecal junction and the Cecum on anti-mesenteric border as shown in Figures 1 and 2. Resection of the perforated intestinal segment with ileo-transverse anastomosis (side-to-side) with proximal loop ileostomy was performed. Abdominal tube drain Fr. 30 was put in pelvis after thorough peritoneal lavage using the normal saline and abdomen was closed in layers. Patient was kept on i.v. fluids and nil orally for 3 days. Broad spectrum antibiotic in the form of 3rd generation cephalosporin with metronidazole and fluoroquinolone were given for 7 days. Nasogastric tube and abdominal drain tube were removed on 3rd post -operative day (POD). Ileostomy started functioning on 4th POD. Patient was discharged on 7th POD with oral fluoroquinolone for 7 days. Histopathological examination revealed evidence of severe acute inflammation, with fibrinopurulent exudates extending along the serosal surface of intestine and acute and chronic inflammation was observed immediately adjacent to the site of perforation. Evidence of villous blunting and elongation of the crypts was observed, which suggests chronic mucosal injury. We were unable to isolate S. typhi from resected bowel specimen; however, stool culture was positive for S. typhi. We were unable to perform Polymerase chain reaction for isolation of S. typhi and other serotypes responsible for TIP due to scarcity of resources at our center. These findings are consistent with TIP. On the basis of these findings, the diagnosis of typhoid enteric perforation was confirmed. Patient came regularly for follow-up, gained weight, and managed ileostomy properly. We closed ileostomy after 12 weeks.
Figure 1.
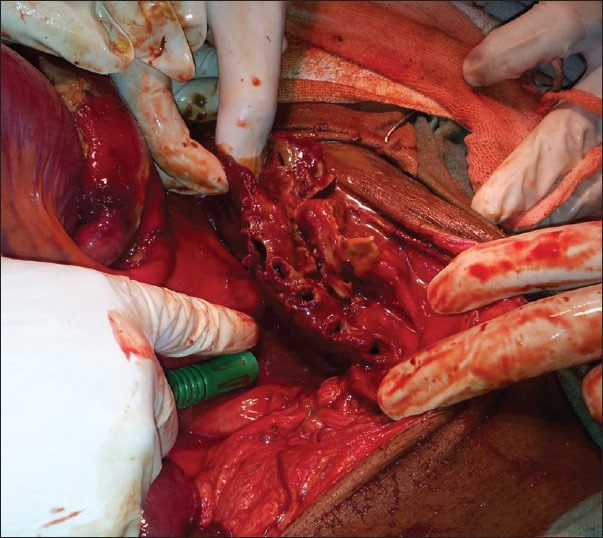
Intra-operative on table view of multiple perforations
Figure 2.
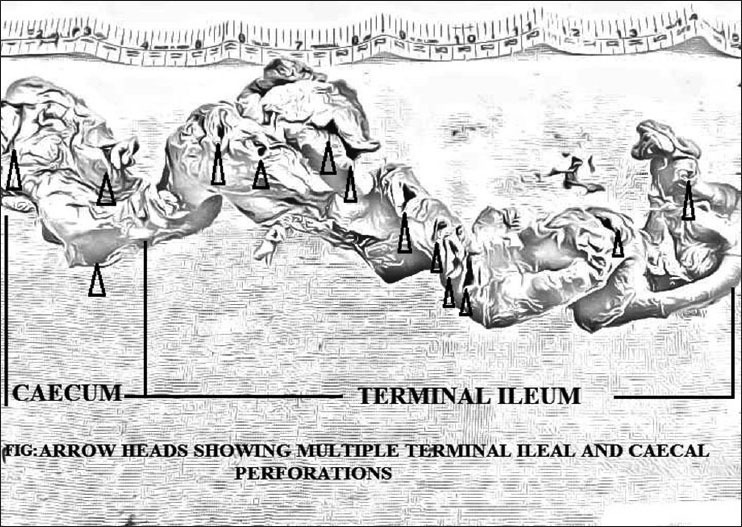
Multiple perforations in ileum
Discussion
Typhoid ileal perforation still remains a very severe condition in tropical countries.[1] Its incidence ranges from 0.9% to 39%, with a mortality rate, which remains very high.[2,3] Primarily, the mortality and the morbidity rate do not depend on the surgical technique, but rather on the general status of the patient, the virulence of the salmonella and the duration of disease evolution before surgical treatment. That is why, it is so important to provide adequate pre-operative management associating aggressive resuscitation with antibiotic therapy. In the literature, it is usually advocated that the last 60 cm of the ileum presents a high concentration of Peyer's patches whose infection is a source of intestinal perforation.[5]
Typhoid fever with perforation is best managed by early surgical intervention. Various surgical options available are simple primary closure, primary closure with omental patch, resection and anastomosis, and closure with ileo-transverse colostomy. Fecal fistula, which is the most common complication of enteric perforation, may occur either because of anastomotic dehiscence, reperforation or different site of perforation. Simple primary closure is still the procedure of choice as it is quick and cost-effective.[8] However, some of the studies showed that the development of fecal fistula and mortality is unrelated to the operative procedure.[9]
In our case report, patient was a middle aged Indian male; enteric perforation is more common in middle aged male because they are more exposed to infection as they consume food outside, which may be unhygienic.[10] Traditionally, diagnosis is made mainly on the basis of clinical history and examination, X-ray abdomen, and ultrasound abdomen supported our diagnosis. Although serologic and bacteriologic data may be supportive, these are frequently negative. Blood cultures are positive for S. typhi in only 3-34% of cases of typhoid perforation, and cultures of the stool and peritoneal fluid are usually negative for this organism.[11] Salmonella paratyphi B involves colon more frequently than terminal ileum.[12] Unfortunately, we cannot phase type strain at our center. On exploration, we found gross peritoneal contamination with relatively healthy proximal intestine. There were 24 perforations present in the distal 35-40 cm of ileum including cecum. So, we decided to perform resection of perforated gut along with cecum and ascending colon and ileotransverse side-to-side anastomosis with proximal defunctioning ileostomy. Histopathological examination revealed acute and chronic inflammation at and near to perforated intestine with cryptic changes with peyer's patches inflammation. These findings are consistent with TIP. Pathophysiology of TIP is complex depending upon both host immunity and bacterial virulence. Musharraf et al. recommended performing resection and anastomosis in multiple perforations with relatively healthy gut as was carried out in this patient.[13] Early and appropriate surgical intervention with effective pre -and post-operative care may improve survival in TIP.[3]
Conclusion
Despite global scientific development typhoid fever and its complications continue to be a great health problem especially in developing country. The management of salmonella enteric perforation needs appropriate early surgical intervention, effective resuscitation in the pre-operative period, post-operative care, and use of proper antibiotics. In our study, there is no evidence of decreased immunity of patient, so increased virulence of bacteria might be probable cause of such complication of typhoid enteritis. The key to improved survival in this deadly disease lies not in a better operation or improved perioperative care, but in the prevention of typhoid fever by providing safe drinking water and improved sanitation methods for all of the global community.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Procop GW, Cockerill FL. Enteritis caused by E. coli and Shigella species. In: Wilson WR, Sande MA, editors. Current Diagnosis and Treatment in Infectious Disease. New York: McGraw Hill; 2001. pp. 559–66. [Google Scholar]
- 2.Saxe JM, Cropsey R. Is operative management effective in treatment of perforated typhoid? Am J Surg. 2005;189:342–4. doi: 10.1016/j.amjsurg.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Atamanalp SS, Aydinli B, Ozturk G, Oren D, Basoglu M, Yildirgan MI. Typhoid intestinal perforations: Twenty-six year experience. World J Surg. 2007;31:1883–8. doi: 10.1007/s00268-007-9141-0. [DOI] [PubMed] [Google Scholar]
- 4.Santillana M. Surgical complications of typhoid fever: Enteric perforation. World J Surg. 1991;15:170–5. doi: 10.1007/BF01659050. [DOI] [PubMed] [Google Scholar]
- 5.Talwar S, Sharma RK, Mittal DK, Prasad P. Typhoid enteric perforation. Aust N Z J Surg. 1997;67:351–3. doi: 10.1111/j.1445-2197.1997.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 6.Nasir AA, Adeniran JO, Abdur-Rahman LO, Odi TO, Omotayo JA. Typhoid intestinal disease: 32 perforations in 1 patient. Niger Postgrad Med J. 2008;15:55–7. [PubMed] [Google Scholar]
- 7.Connolly DP, Ugwu BT, Eke BA. Single-layer closure for typhoid perforations of the small intestine: Case report. East Afr Med J. 1998;75:439–40. [PubMed] [Google Scholar]
- 8.Beniwal US, Jindal D, Sharma J, Jain S, Shyam G. Comparative study of operative procedures in typhoid perforation. Indian J Surg. 2003;65:172–7. [Google Scholar]
- 9.Mansoor T, Husain M, Harris SH. Modified ileo-transverse anastomosis in selected cases of typhoid perforation of bowel. Indian J Gastroenterol. 2003;22:110–1. [PubMed] [Google Scholar]
- 10.Patil PV, Kamat MM, Milan M. Hindalekar. Spectrum of perforative peritonitis-A prospective study of 150 cases. Bombay Hosp J. 2012;54:38–50. [Google Scholar]
- 11.Keenan JP, Hadley GP. The surgical management of typhoid perforation in children. Br J Surg. 1984;71:928–9. doi: 10.1002/bjs.1800711203. [DOI] [PubMed] [Google Scholar]
- 12.Elisha SO. Pathology and pathogenesis of typhoid fever. Nig P Med J. 1994;1:38. [Google Scholar]
- 13.Husain M, Khan RN, Rehmani B, Haris H. Omental patch technique for the ileal perforation secondary to typhoid fever. Saudi J Gastroenterol. 2011;17:208–11. doi: 10.4103/1319-3767.80386. [DOI] [PMC free article] [PubMed] [Google Scholar]


