Abstract
Objective:
To study the incidence and type of musculoskeletal and aesthetic abnormalities after thoracotomy in children.
Materials and Methods:
Children below 12 years of age who had undergone thoracotomy for any condition and have at least 2 years follow up were included in the study. Detailed assessment of the patients included: history and general examination, clinical examination of chest and musculoskeletal system, X-ray chest including bilateral shoulders [antero-posterior (AP), lateral, oblique], X-ray whole spine (AP, lateral, right and left side bending AP view).
Results:
Fifty-two pateints were recruited. The incidences of various clinically and radiologically assessed musculoskeletal and aesthetic abnormalities observed were: winging of scapula (5.7%), ipsilateral elevation of shoulder (5.7%), fixation of skin cicatrix to bony thorax (7.7%), maldevelopment of pectoral muscles (11.5%), asymmetry of the level of nipples (1.9%), rib fusion (5.7%), crowding of ribs (9.6%), mediastinal shift (3.8%), decreased space available for lungs (3.8%), Scoliosis with Cobb's angle >100 (1.9%).
Conclusions:
The incidences of musculoskeletal and aesthetic abnormalities after posterolateral thoracotomies in children were low. Longer follow up of patients after thoracotomy is needed to pick up these abnormalities as the children grow.
KEY WORDS: Aesthetic abnormalities, long term follow-up, musculoskeletal abnormalities, thoracotomy in children
INTRODUCTION
Postero-lateral thoracotomy incision is a relatively common surgical approach for thoracic procedures in infants and children. This approach results in division of the latissimus-dorsi and serratus-anterior muscles. Division of these muscles can result in significant post-operative pain, diminished pulmonary function, and marked impairment of motion. The thoracotomy incision may result in long-term physical impairment and deformity. Chest-wall deformities are less common in patients who have undergone only one thoracotomy and have had no rib resection. Typical findings may include scapular winging, anterior chest wall deformity, and scoliosis. Scoliosis may also be because of associated congenital vertebral anomalies. Damage to the innervations of serratus anterior muscle may contribute to the chest wall deformity. The incidence of scapular winging could be diminished by careful preservation of long thoracic nerve during thoracotomy. In addition to chest wall asymmetry, female patients may develop significant breast asymmetry that may require later plastic surgical repair. Scoliosis may occur after thoracotomy for esophageal atresia but is more common and more severe in patients with associated vertebral anomalies. Scoliosis that is associated with thoracotomy is usually mild and does not cause symptoms. In patients with vertebral anomalies, scoliosis may need surgical intervention.
Objectives
To study the incidence, type of musculoskeletal and aesthetic abnormalities after thoracotomy in children.
MATERIALS AND METHODS
This cross-sectional study was performed at a tertiary care center. Children below 12 years of age who had undergone thoracotomy for any condition and had at least 2-year follow-up were included in the study. Children having pre-existing spinal and chest-wall deformities, congenital myopathy disorders, excision of chest wall tumors and whose parents refused to give consent were excluded from the study.
Clearance from institute's ethics committee was obtained. Records of all children who had undergone thoracotomy before 2009 were retrieved. Patients were called on phone or with post cards for completion of missing data and further investigations as required. Patients coming for follow-up between July 2010 and June 2011 were included in the analysis. All the investigations done in this study were routine investigations performed during follow-up after thoracotomy requiring no specific safety measures.
Statistical analysis
Data was analyzed using the Stata software version 11.0 (Stata Corp. College Station, TX). Results were calculated as mean and inter-quartile range accordingly.
Clinical assessment
Detailed assessment of the patients included: history and general examination, clinical examination of chest and musculoskeletal system, investigations like X-ray chest including bilateral shoulders (AP, lateral, oblique) and X-ray whole spine (AP, lateral, right, and left side bending AP view).
Examination of musculoskeletal system was done and parameters assessed were limitation of arm abduction (in degrees), shoulder elevation, deformity of chest (including asymmetry of chest wall), thumb excursion test,[1] deformity of spine, winging of scapula, tenderness over scar, fixation of skin cicatrix to bony thorax limiting shoulder mobility, pectoral muscle maldevelopment.
Examination of breast was done by Index method i.e., index 0 (symmetrical breast development), index I (asymmetry at the level of nipples), and index II (asymmetry at the level of the lower part of breast).
Investigations
X-ray chest including bilateral shoulders (AP, lateral, and oblique view) were done and deformities assessed were elevation of shoulder, chest-wall deformities like asymmetry of chest and pectus deformity, rib changes like rib fusion, rib crowding and irregularity, mediastinal shift, space available for lung (SAL),[1] condition of lungs, its vasculature and pleura.
X-ray whole spine (AP, lateral, right, and left side bending AP view) was done and spinal deformities like scoliosis (Cobb's angle), kyphosis, lordosis, and other abnormal curvatures of spine were measured. The Scoliosis Research Society (SRS) definitions of different spinal curve deformities were used during measurement.[2]
RESULTS
Patient characteristics
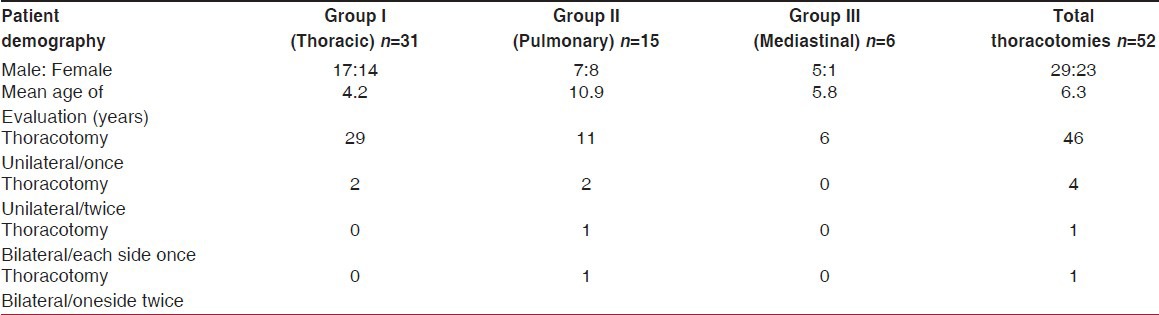
The study included total of 52 patients and they were stratified into three groups according to the diseases for which thoracotomies were done [Figure 1]. Out of 52 patients, 29 (55.8%) were male and 23 (44.2%) were female. The age at the time of evaluation ranged from 2 to 18 years (mean 6.3 years) [Table 1]. Thirty-nine patients had undergone right-sided thoracotomy and 11 patients had undergone left-sided thoracotomy while two patients had undergone bilateral thoracotomy. Out of 50 unilateral thoracotomies, 46 were done once and in two patients unilateral thoracotomy was done twice. Out of two bilateral thoracotomies, one patient had once on each side and the other patient had twice on right side [Table 1]. All thoracotomies were done through postero-lateral route without rib resection.
Figure 1.
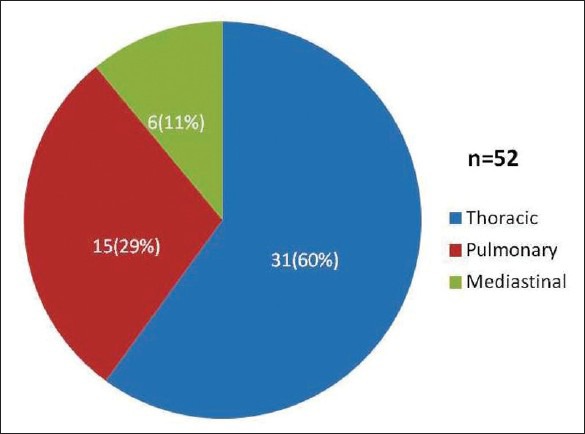
Distribution of cases within each group
Table 1.
Patient demography
In Group I, out of 31 thoracic cases, 27 (87.1%) were cases of esophageal atresia with trachea-esophageal fistula (EA-TEF), 2 (6.5%) were eventration of diaphragm, 1 (3.3%) each of H-type TEF and congenital esophageal stenosis [Figure 2]. In Group II, out of 15 pulmonary cases, 9 (60%) were lung metastasis from abdominal solid tumors, 3 (20%) were hydatid cyst, 2 (13.3%) were bronchiectasis, and 1 (6.6%) was eventration of diaphragm. This patient of eventration had undergone second thoracotomy for decortication and lingulectomy. In Group III, out of 6 mediastinal cases, 4 (66.7%) were mediastinal tumors like neuroblastoma and germ cell tumor and 2 (33.3%) were cases of lymphangioma [Figure 2].
Figure 2.
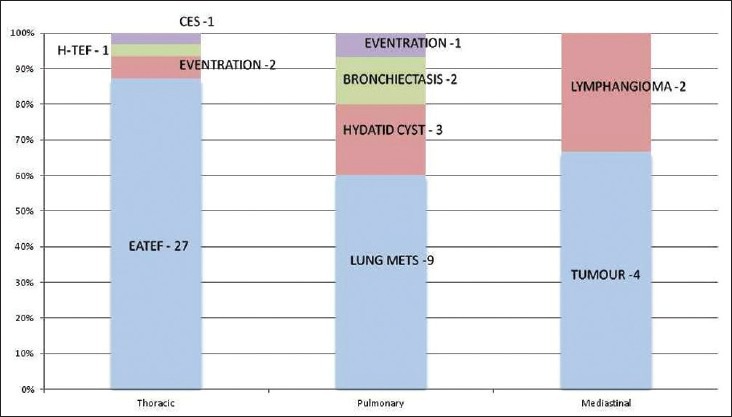
Disease distribution in each group of patients. (EATEF- esophageal atresia with tracheo-esophageal fistula; CES – congenital esophageal stenosis; H-TEF- H type tracheo-esophageal fistula; Lung Mets - Lung metastasis)
In thoracic group, all patients had undergone unilateral thoracotomy. In two patients thoracotomy was done twice. One neonate of congenital short esophagus had developed a major leak after resection and end-to-end anastomosis for which decortications and diversion was done in newborn period and later reverse gastric tube for esophageal replacement was done. Second case was persistent anastomotic stricture following primary repair of EA-TEF for which resection of stricture and end-to-end anastomosis of esophagus was done. In pulmonary group (n=15), 13 had unilateral and 2 bilateral thoracotomy. Out of 13 unilateral thoracotomies, two patients underwent thoracotomy twice. One case was left eventration of diaphragm who had undergone plication of diaphragm and developed persistent lower respiratory tract infection and thickening of pleura with collapse of lingula for which decortication and lingulectomy was done. The other was a follow-up case of Wilms’ tumor with bilateral lung metastasis for which left thoracotomy was done twice for removal of recurrent metastatic nodule within one year interval and right lung metastatic nodule disappeared after chemotherapy. Out of two bilateral thoracotomies in the group II one patient had left thoracotomy done twice. This was a case of hepatoblastoma with bilateral lung metastasis. The other bilateral thoracotomy was a case of osteosarcoma of right tibia with bilateral lung metastasis. All the patients in mediastinal group had undergone unilateral thoracotomy once.
Out of 52 patients, four patients had undergone lobectomy and one patient lingulectomy. Out of four lobectomies, three patients (two right lower lobes and one left lower lobe) had lung metastasis from abdominal solid tumors. One patient of complicated hydatid cyst had undergone left upper lobectomy for complete removal of cyst. One lingulectomy was done in a patient of left eventration of diaphragm as has been mentioned earlier. Two pneumonectomies (one left and one right) were done for bronchiectasis of lung. Out of six wedge excision of lung parenchyma five were done for removal of metastatic lesions (2 from left lung lower lobe, 2 from right lung lower lobe, and 1 from right lung upper and middle lobe) and one from right lung middle lobe with complete excision of germ cell tumor of mediastinum.
Musculoskeletal morbidity after thoracotomy
All 52 patients underwent musculoskeletal system examination [Table 2]. Only 1 (1.9%) patient had scoliosis, 3 (5.7%) patients had winging of scapula, 3 (5.7%) patients had shoulder elevation on thoracotomy side, 4 (7.7%) had skin cicatrix fixed to bony thorax, and 6 (11.5%) patients had pectoral muscle maldevelopment. In thoracic group out of 31 patients, 1 (3.2%) patient had winging of scapula, 3 (9.7%) patients had shoulder elevation, 3 (9.7%) patients had skin cicatrix fixed to bony thorax and 2 (6.4%) patients had pectoral muscle maldevelopment. In pulmonary group 1 (6.6%) patient had scoliosis at upper thoracic region (T3 level) and 1 (6.6%) each had winging of scapula, skin cicatrix fixed to bone and 4 (26.6%) patients had pectoral muscle maldevelopment. In mediastinal group only 1 (16.6%) patient had winging of scapula [Table 2].
Table 2.
Musculoskeletal system examination findings
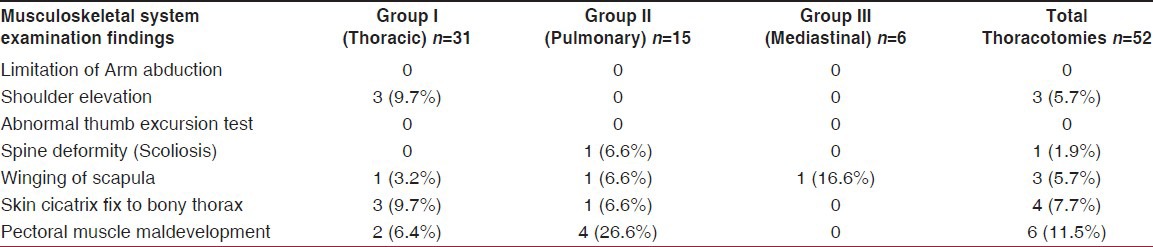
Figure 3a depicts a follow-up case of TEF operated 18 years back showing skin cicatrix fixed to bony thorax but not limiting arm movement. Same patient also had right pectoral muscle maldevelopment [Figure 3b].
Figure 3.

(a) Cicatrix fixed to bony thorax (b) same patient showing right pectoral muscle maldevelopment
Out of 52 patients, only 1 patient had breast asymmetry at level of nipple who was 11-year-old male and had undergone left upper lobectomy for hydatid cyst excision at age of 5 years.
Radiological evaluations
Out of 52 patients, 3 (5.7%) patients had rib fusion, 5 (9.6%) patients had crowding of ribs, 2 (3.8%) patients had mediastinal shift, 2 (3.8%) patients had decreased space available for lung and 1 (1.9%) patient had scoliosis (Cobbs angle >10 degree) [Table 3]. In thoracic group out of 31 patients, 3 (9.6%) patients had rib fusion and 4 (12.9%) had rib crowding (all were cases of EA/TEF). A follow-up case of TEF operated 4 years back showing rib fusion in X-ray chest in right hemithorax is depicted in Figure 4a. In pulmonary group, 1 (6.6%) patient had rib crowding who had undergone lobectomy for hydatid cyst excision, 2 (13.3%) patients had mediastinal shift (both following pneumonectomy), 2 (13.3%) patients had decreased space available for lung (SAL)-92% and 98%, who had undergone right and left pneumonectomy at the age of 10 years and 7 years, respectively, for bronchiectasis and assessed two and half years after surgery. Only one patient had scoliosis [Table 3] of left side at upper thoracic level (T3 vertebra) with Cobb's angle of 15 degree [Figure 4b]. This patient had undergone right pneumonectomy by postero-lateral thoracotomy through the bed of 4th rib, for bronchiectasis at the age of 10 years and scoliosis was noticed 52 months after surgery. Rest all patients had Cobb's angle <10 degrees which is not significant. None of the patients from mediastinal group had abnormal findings [Table 3]. Shoulder elevation, kyphosis, lordosis, and other spinal curvatures were not seen in any of our patients.
Table 3.
Findings on X-ray chest, shoulder and whole spine
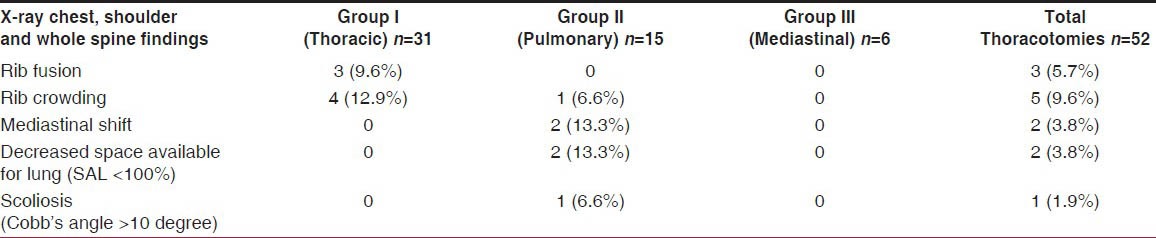
Figure 4.
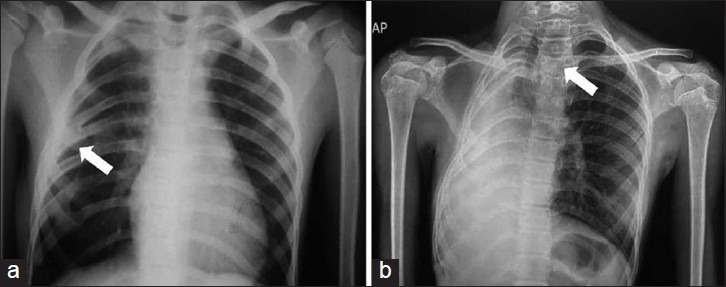
(a) Rib fusion on X-ray chest (white arrow) (b) X-ray chest showing mediastinal shift, rib crowding, ends of excised rib, and space available for lung (SAL) – 92%. X-ray thoracic spine showing scoliosis with Cobb's angle of 150, with convexity toward left at T3 level (White arrow)
DISCUSSION
Musculoskeletal morbidity after thoracotomy (clinical and radiological)
Two larger series of chest-wall deformities after surgery for EA-TEF have been reported. In first series of 232 patients with esophageal atresia but no congenital vertebral anomaly; 77 (33%) patients developed chest-wall deformities.[3] Anterior chest wall deformities were found in 47, scoliosis in 18 and a combination of both in 12 patients. Chest-wall deformity appeared to be more common in patients after 25 years of age and scoliosis in patients who had undergone numerous thoracotomies. One patient required surgery for severe scoliosis. Another series of similar experience in 89 patients operated on for esophageal atresia, via a right dorso-lateral thoracotomy and followed up for 3-16 years.[4] Twenty-nine of the patients had significant musculoskeletal deformities: 21 (24%) had a “winged” scapula from partial paralysis of the latissimus-dorsi muscle; 18 (20%) had marked asymmetry of the thoracic wall from atrophy of the serratus anterior muscle; 9 (10%) had rib fusion (with major respiratory dysfunction in one patient); and 7 (8%) had severe thoracic scoliosis. No patient required surgical correction but all needed physiotherapy.
Orthopedic surgeons subsequently described severe scoliosis in 18 patients followed up for more than 10 years after repair of tracheo-esophagealfistula.[5] A spinal curvature of more than 10 degrees had developed in nine patients and in eight of these cases the curves were convex away from the side of the incision. The scoliosis had appeared at any time from early childhood to skeletal maturity but was more likely to be progressive in those in whom it had developed before the adolescent growth spurt.
Similar sequelae have been described after thoracotomy for congenital cardiac disease. In a prospective study of 36 premature infants after left thoracotomy for patent ductus arteriosus,[6] one developed thoracic scoliosis and 20 of 27 (74%) had minor radiologic skeletal abnormalities in the form of rib deformation or fusion; the latter carries a risk of long-term scoliosis. No left shoulder elevation or left arm dysfunction was noticed. Bal et al., confirmed this high prevalence of musculoskeletal problems in a series of 49 children who had required postero-lateral thoracotomy for cardiac surgery. After a mean follow-up period of 6 years, 94% had various deformities: 31% had scoliosis, with a severe curve exceeding 25 degrees in two; 61% had shoulder elevation; 77% had a winged scapula; and 14% had asymmetry of the thoracic wall due to the atrophy of the serratus anterior muscle.[7] Primary esophageal atresia repair through the postero-lateral thoracotomy frequently (30%) resulted in rib fusions, and these were major contributors to the later scoliosis. Thoracotomy in infancy for various reasons has been reported to cause scoliosis in 4-50% of cases.[7]
In 1969, Freeman and Walkden first reported right shoulder deformities after repair of esophageal atresia by right thoracotomy.[8] Severe scoliosis was more likely in patients who had experienced postoperative infectious complications such as mediastinitis and empyema secondary to esophageal dehiscence; in these cases it was often accompanied by marked scarring and rib fusion.[9]
In the current study out of 52 patients, 1 (1.9%) patient had scoliosis, 3 (5.7%) patients had winging of scapula, 3 (5.7%) patients had shoulder elevation on thoracotomy side, 4 (7.7%) had skin cicatrix fixed to bony thorax, 6 (11.5%) patients had pectoral muscle maldevelopment, 3 (5.7%) patients had rib fusion, 5 (9.6%)patients had crowding of ribs, 2 (3.8%) patients had mediastinal shift and 2 (3.8%) patient had decreased space available for lung [Tables 2 and 3]. In comparison to other studies incidence of musculoskeletal abnormalities were low, this observation might be due to more number of patients with shorter duration (2 years) of follow-up. In this study, rib fusion, rib crowding were more frequently seen after neonatal thoracotomies due to decreased rib space and increased chance of injury to rib periosteum. Similarly, skin cicatrix fixed to bony thorax and shoulder elevation abnormalities were also more commonly seen after neonatal thoracotomies due to increased likelihood of damaging nerve to Serratus and Latissimus-dorsi muscles and poor physiotherapy of these muscles in post-operative period.
Out of 52 patients, only one patient had scoliosis [Table 3] who was a 14-year-old female, follow-up case of right lung bronchiectasis undergone right pneumonectomy four and half years back. X-ray chest showing mediastinal shift, rib crowding, ends of excised rib, and space available for lung (SAL) – 92%. X-ray thoracic spine showing scoliosis with Cobb's angle of 15 degree, with convexity toward left at T3 level [Figure 4b]. Rest all patients had Cobb's angle <10 degree which is not significant. Very low incidence of scoliosis in this study might be due to exclusion of congenital vertebral anomalies from the study and also shorter duration of follow-up (2 years) after thoracotomy. Patients with rib fusion may be expected to develop some degree of scoliosis at a later date and so need to be followed up for longer period of time.
Aesthetic morbidity after thoracotomy
Skin incisions for pediatric thoracotomy are usually short and devoid of major aesthetic sequelae. Postoperative wound infection is uncommon after lung resection, thereby increasing the chance of a satisfactory scar. Postero-lateral thoracotomy through an axillary skin incision has been described, allowing for access through the third or fourth intercostal space.[10]
Deformities caused by atrophy of chest wall muscles from nerve injuries during thoracotomy have been reported. A series of 58 adult computed tomography (CT) scans in patients who had had a previous thoracotomy were compared with muscle thickness on the side of surgery with that on the contralateral chest wall.[11] Muscle atrophy was found in 42 patients but in two cases this was confined to the serratus anterior muscle only. Signs of atrophy of the latissimus-dorsi muscle and the inferior portion of the serratus anterior muscle were seen in all patients after postero-lateral thoracotomy, whereas this pattern of atrophy was present in only two of 18 patients after antero-lateral thoracotomy. No equivalent pediatric series has been published.
In order to preserve muscle, a muscle-sparing thoracotomy is an alternative and may be particularly important if rotational muscle flaps might be necessary.[12] Muscle-sparing thoracotomy has been reported in children.[13] The only specific morbidity described using this technique rather than the classical approach was the occurrence of seroma.[14]
A more serious aesthetic complication of thoracotomy concerns breast development. One study reported scar disfiguration of the right breast in 3.3% of patients after right postero-lateral thoracotomy for esophageal atresia; one patient had mammary maldevelopment.[5] Nipple asymmetry has been described in 63% of patients after thoracotomy for congenital cardiac disease.[7] After cardiac surgery via an antero-lateral thoracotomy, reported disturbance in breast development were in 55% of women (left breast volume at least 20% greater than right breast), with an asymmetry of the lower part of the right breast in 61%.[15] These authors concluded that antero-lateral thoracotomy can significantly interfere with ipsilateral breast development.
In the current study out of 52 patients, only 1 patient had breast asymmetry at level of nipple who was a 11-year-old male and had undergone left upper lobectomy for hydatid cyst excision at age of 5 years. No female patient in this study had breast disfigurement. Four (7.7%) patients had skin cicatrix fixed to bony thorax [Figure 3a] and 6 (11.5%) patients had pectoral muscle mal-development [Figure 3b]. Low incidence of aesthetic complications including breast asymmetry were due to inclusion of only postero-lateral thoracotomies and incision far away from nipple and also decreased incidence of thoracic wound infection. More abnormalities were likely to be detected if these patients are studied later in adolescence/early adulthood. Most of the female patients in this study had not reached adolescence, so long-term follow-up of these patients need to be done to look for their aesthetic morbidities and treatment if required.
CONCLUSIONS
The incidences of musculoskeletal and aesthetic abnormalities after posterolateral thoracotomies in children were low. So close follow-up of patients after thoracotomy is needed for longer periods of time to pick up these abnormalities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Campbell RM, Jr, Smith MD, Mayes TC, Mangos JA, Willey-Courand DB, Kose N, et al. The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. 2003;85A:399–408. doi: 10.2106/00004623-200303000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Scoliosis research society terminology committee and working group on spinal classification revised glossary of terms by the working group on 3-D Classification (Chair Larry Lenke, MD), and the terminology committee. 2000 Mar [Google Scholar]
- 3.Seghaye MC, Grabitz R, Alzen G, Trommer F, Hörnchen H, Messmer BJ, et al. Thoracic sequelae after surgical closure of the patent ductus arteriosus in premature infants. Acta Paediatr. 1997;86:213–6. doi: 10.1111/j.1651-2227.1997.tb08871.x. [DOI] [PubMed] [Google Scholar]
- 4.Chetcuti P, Myers NA, Phelan PD, Beasley SW, Dickens DR. Chest wall deformity in patients with repaired esophageal atresia. J Pediatr Surg. 1989;24:244–7. doi: 10.1016/s0022-3468(89)80003-x. [DOI] [PubMed] [Google Scholar]
- 5.Jaureguizar E, Vazquez J, Murcia J, DiezPardo JA. Morbid musculoskeletal sequelae of thoracotomy for tracheo-esophageal fistula. J Pediatr Surg. 1985;20:511–4. doi: 10.1016/s0022-3468(85)80477-2. [DOI] [PubMed] [Google Scholar]
- 6.Durning RP, Scoles PV, Fox OD. Scoliosis after thoracotomy in tracheo-esophageal fistula patients: A follow-up study. J Bone Joint Surg Am. 1980;62:1156–9. [PubMed] [Google Scholar]
- 7.Bal S, Elshershari H, Celiker R, Celiker A. Thoracic sequels after thoracotomies in children with congenital cardiac disease. Cardiol Young. 2003;13:264–7. [PubMed] [Google Scholar]
- 8.Freeman NV, Walkden J. Previously unreported shoulder deformity following right lateral thoracotomy for esophageal atresia. J Pediatr Surg. 1969;4:627–36. doi: 10.1016/0022-3468(69)90490-4. [DOI] [PubMed] [Google Scholar]
- 9.Gilsanz V, Boechat IM, Birnberg FA, King JD. Scoliosis after thoracotomy for esophageal atresia. Am J Roentgenol. 1983;141:457–60. doi: 10.2214/ajr.141.3.457. [DOI] [PubMed] [Google Scholar]
- 10.Kalma A, Verebely T. The use of axillary skin crease incision for thoracotomies of neonates and children. Eur J Pediatr Surg. 2002;12:226–9. doi: 10.1055/s-2002-34487. [DOI] [PubMed] [Google Scholar]
- 11.Frola C, Serrano J, Cantoni S, Casiglia M, Turtulici I, Loria F. CT findings of atrophy of chest wall muscle after thoracotomy: Relationship between muscles involved and type of surgery. Am J Roentgenol. 1995;164:599–601. doi: 10.2214/ajr.164.3.7863878. [DOI] [PubMed] [Google Scholar]
- 12.Landreneau RJ, Pigula F, Luketich JD, Keenan RJ, Bartley S, Fetterman LS, et al. Acute and chronic morbidity differences between muscle-sparing and standard lateral thoracotomies. J Thorac Cardiovasc Surg. 1996;112:1326–50. doi: 10.1016/S0022-5223(96)70150-2. [DOI] [PubMed] [Google Scholar]
- 13.Rothenberg SS, Pokorny WJ. Experience with a total muscle-sparing approach for thoracotomies in neonates, infants and children. J Pediatr Surg. 1992;27:1157–9. doi: 10.1016/0022-3468(92)90579-v. [DOI] [PubMed] [Google Scholar]
- 14.Akcalli Y, Demir H, Tezcan B. The effect of standard postero-lateral versus muscle-sparing thoracotomy on multiple parameters. Ann Thorac Surg. 2003;76:1050–4. doi: 10.1016/s0003-4975(03)00565-4. [DOI] [PubMed] [Google Scholar]
- 15.Bleiziffer S, Schreiber C, Burgkart R, Regenfelder F, Kostolny M, Libera P, et al. The influence of right antero-lateral thoracotomy in prepubescent female patients on late breast development and on the incidence of scoliosis. J Thorac Cardiovasc Surg. 2004;127:1474–80. doi: 10.1016/j.jtcvs.2003.11.033. [DOI] [PubMed] [Google Scholar]


