Abstract
OBJECTIVE:
To evaluate the accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the diagnosis of adenomyosis, leiomyoma, or combined adenomyosis and leiomyoma by the use of transvaginal ultrasonography (TVS) compared to the histopathological findings.
SUBJECTS AND METHODS:
This is a retrospective study of patients with a preoperative TVS diagnosis of adenomyosis, leiomyoma, or combined. Patients diagnosed with adenomyosis or combined adenomyosis and leiomyoma via TVS underwent hysterectomy. Symptomatic patients diagnosed with adenomyosis and leiomyoma via TVS underwent myomectomy with excision of the surrounding myometrium which contained possible adenomyosis. Following surgery, a histopathological examination was performed by the hospital pathologists. The microscopic diagnosis of the specimen was recorded.
RESULTS:
TVS diagnosis of adenomyosis was sensitive but not specific. TVS was sensitive, specific, and accurate in the diagnosis of leiomyoma and combined adenomyosis and leiomyoma.
CONCLUSION:
This study demonstrated that TVS is a valuable noninvasive method that should be utilized in the diagnosis of leiomyoma and combined adenomyosis and leiomyoma. TVS is sensitive, but is not specific in the diagnosis of adenomyosis only.
KEY WORDS: Adenomyosis, histopathology, leiomyoma, transvaginal ultrasound
INTRODUCTION
Adenomyosis is a common gynecological condition that is characterized by ingrowths of the endometrial cells into the myometrium. Leiomyoma are commonly associated with adenomyosis. Adenomyosis and leiomyoma are benign conditions that are often responsible for uterine enlargement, menorrhagia, anemia, and infertility.[1] Adenomyosis or internal endometriosis may occur as a result of increased overgrowth of the endometrium with invasion of the underlying myometrium or the displacement of the endometrium during pregnancy, delivery, endometrial curettage, cesarean section, myomectomy, or metroplasty.[1]
Because of its similarities to leiomyoma, it can be difficult in some cases to accurately diagnose adenomyosis by ultrasound. The treatment options and the prognosis of each diagnosis are different. Most gynecologists will consider conservative medical treatment more often for adenomyosis only, while surgical options will be chosen frequently for leiomyoma or combined adenomyosis and leiomyoma, especially in large uteri. The three most common methods of clinical diagnosis of adenomyosis are magnetic resonance imaging (MRI), transabdominal ultrasonography (TAS), and transvaginal ultrasonography (TVS).[2] There is limited diagnostic capacity with TAS, while TVS is a more feasible option.[3,4,5,6] Moreover, TVS is also much more cost effective than MRI and is generally more readily available in the office to most practicing gynecologists.
The aim of this retrospective study was to determine the accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TVS in the diagnosis of adenomyosis and leiomyoma confirmed by postsurgical histopathological findings. The importance of an accurate noninvasive diagnostic method like ultrasound for adenomyosis, leiomyoma, or combined is an ongoing need in the gynecological community.[7]
SUBJECTS AND METHODS
This was an Institutional Review Board (IRB) approved retrospective consecutive case series study.
From November 2006 to May 2012, patients underwent surgery for the treatment of adenomyosis, leiomyoma, or combined adenomyosis and leiomyoma. A preoperative TVS was administered to each patient. Diagnostic criteria of uterine adenomyosis include two of the five sonographic features on TVS:[5,8,9,10,11] (1) No distinction of the endometrial-myometrial junction; (2) asymmetry of the anterior and posterior myometrium; (3) subendometrial myometrial striations; (4) myometrial cysts and fibrosis; and (5) heterogeneous myometrial echotexture.
Diagnostic criteria of uterine leiomyoma include two of the five sonographic features on TVS: (1) Clear demarcation of the tumor margin; (2) whorly appearance of the tumor content; (3) the presence of blood vessels (by color Doppler) surrounding the tumor; (4) irregularities of the uterine surface (subserous and intramural tumors); and (5) irregularities of the endometrial surface (submucous tumors type 1 and 2).
Patients diagnosed with adenomyosis or combined adenomyosis and leiomyoma via TVS underwent hysterectomy. Symptomatic patients diagnosed with adenomyosis and leiomyoma via TVS underwent myomectomy with excision of the surrounding myometrium which presumably contained adenomyosis. Following surgery, a histopathological examination was performed by the hospital pathologists. The microscopic diagnosis of the specimen was recorded.
Statistical analysis was performed using SAS 9.3 for Windows. Student's t-tests were used for parametric continuous variables; and the Chi-square or Fisher's exact test, where suitable, was used for categorical variables. Sensitivity, specificity, NPV, PPV, positive and negative likelihood ratios, and accuracy were determined for ultrasound findings as they corresponded to the final histopathological diagnosis. Statistical significance was set at P < 0.05.
RESULTS
From November 2006 to May 2012, 163 patients underwent surgery for the treatment of adenomyosis, leiomyoma, or combined adenomyosis and leiomyoma. One hundred and twenty-three patients were diagnosed with adenomyosis, and 134 patients were diagnosed with leiomyoma. Twenty-nine patients were diagnosed with adenomyosis only, 40 patients were diagnosed with leiomyoma only, and 94 patients were diagnosed with combined adenomyosis and leiomyoma, as illustrated in Figure 1.
Figure 1.
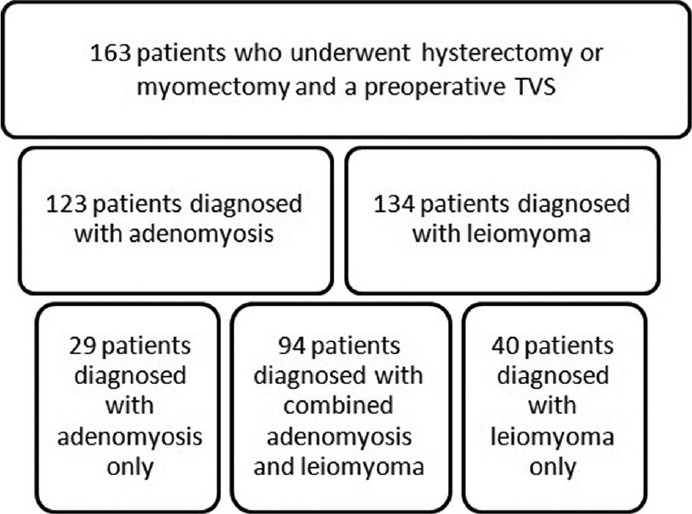
Patient diagnosis groups
One hundred and thirty patients diagnosed with adenomyosis or combined adenomyosis and leiomyoma via TVS underwent hysterectomy. Thirty-three symptomatic patients diagnosed with adenomyosis and leiomyoma via TVS underwent myomectomy.
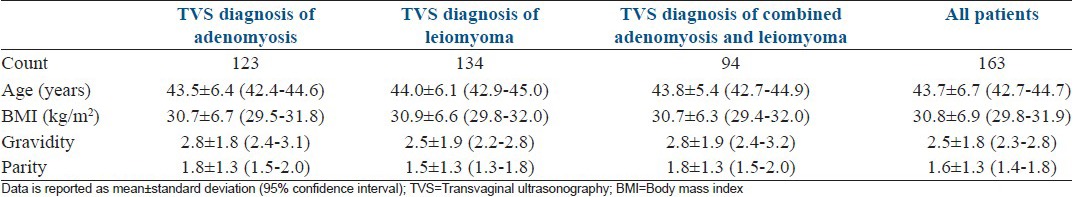
The patients ranged in age from 27 to 68 years. The mean age was 43.7 years with a standard deviation (SD) of 6.7 years and median of 43 years. There was no significant difference in the mean age, weight, height, gravidity, and parity of the patient diagnosis groups. The characteristics of the patients included in this study are represented in Table 1.
Table 1.
Patient characteristics for 163 females who underwent hysterectomy or myomectomy between 2006 and 2012
Of the 123 patients (75.46%) who were positively diagnosed with adenomyosis, 93 of the patients’ (75.61% PPV) diagnoses were confirmed by the histopathological findings. The other 30 patients (24.39%) had a negative histopathological diagnosis. Forty patients were negatively diagnosed upon the initial TVS. Histopathological reports found 23 (57.50% NPV) confirmed negative diagnoses and 17 (42.50%) positive findings. The sensitivity of TVS in the diagnosis of adenomyosis was 84.55% (95% CI 76.4-90.7, P < 0.0001) and the specificity was 43.40% (95% CI 29.8-57.7, P = 0.41). Table 2 shows the sensitivities, specificities, PPVs, NPVs, and accuracy for each of the initial TVS diagnoses. This suggests that TVS is sensitive in the diagnosis of adenomyosis but not specific. This could be explained by the difficulty to diagnose adenomyosis in patients with other intrauterine abnormalities or conditions. Patients positively diagnosed with adenomyosis via TVS are 1.49 (95% CI 1.16-1.92, P < 0.002) times more likely to have the condition. Conversely, patients negatively diagnosed with adenomyosis via TVS are 2.81 (95% CI 1.65-4.79, P = 0.0002) times less likely to have the condition.
Table 2.
Number of patients, positive and negative predictive values, sensitivity, specificity, and accuracy of transvaginal ultrasound for initial diagnosis with histopathological correlation (n=107)
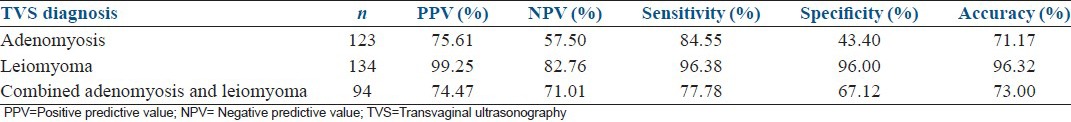
One hundred and thirty-four patients (82.21%) were diagnosed with leiomyoma and 29 patients (17.79%) were negative for leiomyoma upon the initial TVS. Of the 134 patients diagnosed with leiomyoma, 133 (99.25% PPV) had a confirmed diagnosis represented in their postsurgical pathology report and one patient's (0.75%) pathology report did not confirm the diagnosis. Of the 29 patients whose TVS diagnosis was negative for leiomyoma, 24 (82.76%) patients’ histopathological findings were also negative, and five patients (17.24%) had a positive histopathological diagnosis. The corresponding sensitivity and specificity of TVS as a diagnostic test for leiomyoma was 96.38% (95% CI 91.75-98.81) and 96.00% (95% CI 79.65-99.90), respectively. Patients with a positive diagnosis of leiomyoma via TVS are 24.09 times (95% CI 35.30-164.45, P = 0.001) more likely to have leiomyoma. Patients with a negative diagnosis of leiomyoma via TVS are 26.53 times (95% CI 11.16-62.89, P < 0.0001) less likely to have leiomyoma. The accuracy of TVS in the diagnosis of leiomyoma was 96.32%.
For the statistical calculations of adenomyosis and leiomyoma as coexisting conditions, analyses were performed excluding the patients who were diagnosed with a singular condition. These patients were classified as “negative” solely for the purpose of calculations regarding the combined condition. Of the 94 patients (57.67%) that were positively diagnosed with combined adenomyosis and leiomyoma, 70 (74.47% PPV) had histopathological confirmation of both conditions and 24 patients (25.53%) did not have evidence of both conditions in their post-surgical pathology report. Sixty-nine (42.33%) patients had a negative TVS diagnosis for combined adenomyosis and leiomyoma, and 49 (71.01% NPV) had histopathological confirmation of the negative diagnosis. However, 20 patients (28.99%) had a positive histopathological diagnosis for both adenomyosis and leiomyoma. The sensitivity and specificity of TVS in the diagnosis of combined adenomyosis and leiomyoma was 77.78 (95% CI 67.79-85.87) and 67.12% (95% CI 55.13-77.67), respectively. Patients who obtained a positive TVS diagnosis are 2.37 times (95% CI 1.67-3.34, P < 0.0001) more likely to be diagnosed with combined adenomyosis and leiomyoma. Alternatively, patients who are negatively diagnosed with adenomyosis and leiomyoma via TVS are 3.02 times (95% CI 1.99-4.59, P < 0.0001) less likely to be diagnosed with combined adenomyosis and leiomyoma. The accuracy of TVS in the diagnosis of combined adenomyosis and leiomyoma was 73.00%.
DISCUSSION
Adenomyosis is a gynecological disorder that is characterized by the overgrowth of the endometrium into the underlying myometrium. The difficulty in diagnosing adenomyosis clinically is due to the lack of strong positive pathognomonic signs and/or clinical findings.[12] The frequency of adenomyosis that is reported varies widely from 8 to 85%.[7,4,8,9,10,11,13] The explanation for this wide range of values, as described by Azziz, is the result of differences in the histological criteria for the diagnosis of adenomyosis, the care of which the pathologic specimens are handled, and the number of blocks of sampling specimens taken.[14]
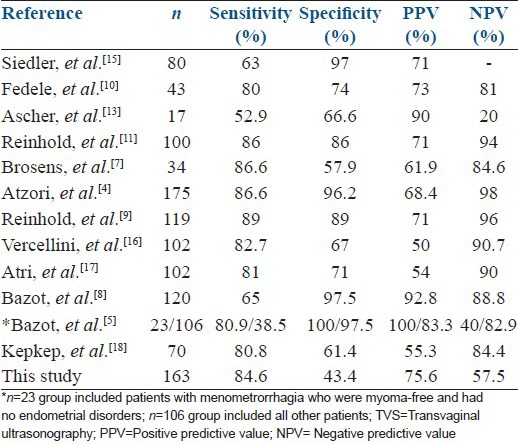
Various measures of accuracy were calculated for the diagnosis of adenomyosis, leiomyoma, and combined adenomyosis and leiomyoma. TVS was 71.17% accurate in the diagnosis of adenomyosis. Table 3 shows a comparison of sensitivity, specificity, PPV, and NPV of this study with several previous studies that investigated the diagnosis of adenomyosis.[4,5,7,8,9,10,11,13,15,16,17,18] It is important to note that the mean number of patients included in the 13 previous studies in Table 3 is 76.8 patients; however, this study utilized 163 patients in the analyses. Along with differences in inclusion criteria, ultrasound equipment, and/or the differences in the criteria to diagnose adenomyosis, the larger sample size could contribute to the difference in results. The sensitivity and specificity of TVS for the diagnosis of adenomyosis in this study was 84.55 and 43.40%, respectively. The associated P value for the specificity was not significant, suggesting TVS as a diagnostic tool is sensitive, but not specific in the diagnosis of adenomyosis. The sensitivity in this study is similar to those previously reported in Table 3, but the specificity is the lowest of those reported. This could be due to the difficulty in diagnosing adenomyosis in the presence of other uterine abnormalities and conditions, especially uterine leiomyomata that may distort the uterus. Patients that were diagnosed with multiple intrauterine conditions were not excluded from this study, since the principle inclusion criteria was patients who underwent hysterectomy or myomectomy and a preoperative TVS.
Table 3.
Sensitivity, specificity, positive and negative predictive values of TVS for the diagnosis of adenomyosis from previous series compared with this series
The sensitivity of TVS for the diagnosis of leiomyoma was 96.38% and the specificity was 96.00%, which is similar to that of a previous study.[19] TVS was 96.32% accurate in the diagnosis of leiomyoma. The accuracy of TVS in diagnosing combined adenomyosis and leiomyoma was 73.00%. The sensitivity for the diagnosis of combined adenomyosis and leiomyoma was 77.78%, and the specificity was 67.12%.
TVS is a useful and dependable diagnostic tool in the diagnosis of adenomyosis. It was accurate, sensitive, and specific in the diagnosis of leiomyoma and combined adenomyosis and leiomyoma. TVS was both accurate and sensitive in the diagnosis of adenomyosis, but not specific. Moreover, TVS is cost effective and readily available in the office to the majority of practicing gynecologists.
CONCLUSION
This study demonstrated that TVS is a valuable noninvasive method that should be utilized in the diagnosis of leiomyoma and combined adenomyosis and leiomyoma. TVS is sensitive, but is not specific in the diagnosis of adenomyosis only.
ACKNOWLEDGEMENTS
The author thanks Rebecca D. Cantrell, BS for data collection and statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ferenezy A. Pathophysiology of adenomyosis. Hum Reprod Update. 1998;4:312–22. doi: 10.1093/humupd/4.4.312. [DOI] [PubMed] [Google Scholar]
- 2.Sun YL, Wang CB, Lee CY, Wun TH, Lin P, Lin YH, et al. Transvaginal sonographic criteria for the diagnosis of adenomyosis based on histopathological correlation. Taiwan J Obstet Gynecol. 2010;49:40–4. doi: 10.1016/S1028-4559(10)60007-1. [DOI] [PubMed] [Google Scholar]
- 3.Champaneria R, Abedin P, Daniels J, Balogun M, Khan KS. Ultrasound scan and magnetic resonance imaging for the diagnosis of adenomyosis: Systematic review comparing test accuracy. Acta Obstet Gynecol Scand. 2010;89:1374–84. doi: 10.3109/00016349.2010.512061. [DOI] [PubMed] [Google Scholar]
- 4.Atzori E, Tronci C, Sionis L. Transvaginal ultrasound in diagnosis of diffuse adenomyosis. Gynecol Obstet Invest. 1996;42:39–41. doi: 10.1159/000291887. [DOI] [PubMed] [Google Scholar]
- 5.Bazot M, Dara E, Rouger J, Detchev R, Cortez A, Uzans Limitations of transvaginal sonography for the diagnosis of Adenomyosis, with histopathological correlation. Ultrasound Obstet Gynecol. 2002;20:605–11. doi: 10.1046/j.1469-0705.2002.00852.x. [DOI] [PubMed] [Google Scholar]
- 6.Coleman BG, Arger PH, Grumbach K, Menard MK, Mintz MC, Allen KS, et al. Transvaginal and transabdominal sonography: Prospective comparison. Radiology. 1988;168:639–43. doi: 10.1148/radiology.168.3.3043545. [DOI] [PubMed] [Google Scholar]
- 7.Brosens JJ, de Souza NM, Barker FG, Paraschos T, Winston RM. Endovaginal ultrasonography in the diagnosis of adenomyosis uteri: Identifying the predictive characteristics. Br J Obstet Gynoecol. 1995;102:471–4. doi: 10.1111/j.1471-0528.1995.tb11320.x. [DOI] [PubMed] [Google Scholar]
- 8.Bazot M, Cortez A, Darai E, Rouger J, Chopier J, Antoine JM, et al. Ultrasonography compared with magnetic resonance imaging for the diagnosis of adenomyosis: Correlation with histopathology. Hum Reprod. 2001;16:2427–33. doi: 10.1093/humrep/16.11.2427. [DOI] [PubMed] [Google Scholar]
- 9.Reinhold C, McCarthy S, Bret PM, Mehio A, Atri M, Zakarian R, et al. Diffuse adenomyosis: Comparison of endovaginal US and MR imaging with histopathologic correlation. Radiology. 1996;199:151–8. doi: 10.1148/radiology.199.1.8633139. [DOI] [PubMed] [Google Scholar]
- 10.Fedele L, Bianchi S, Dorta M, Arcaini L, Zanotti F, Carinelli S. Transvaginal ultrasonography in the diagnosis of diffuse adenomyosis. Fertil Steril. 1992;58:94–7. [PubMed] [Google Scholar]
- 11.Reinhold C, Atri M, Mehio A, Zakarian R, Aldis AE, Bret PM. Diffuse uterine adenomyosis: Morphologic criteria and diagnostic accuracy of endovaginal sonography. Radiology. 1995;197:609–14. doi: 10.1148/radiology.197.3.7480727. [DOI] [PubMed] [Google Scholar]
- 12.Matalliotakis IM, Katsikis IK, Panidis DK. Adenomyosis: what is the impact on fertility? Curr Opin Obstet Gynecol. 2005;17:261–4. doi: 10.1097/01.gco.0000169103.85128.c0. [DOI] [PubMed] [Google Scholar]
- 13.Ascher SM, Arnold LL, Patt RH, Schruefer JJ, Bagley AS, Semelka RC, et al. Adenomyosis: Prospective comparison of MR imaging and transvaginal sonography. Radiology. 1994;190:803–6. doi: 10.1148/radiology.190.3.8115630. [DOI] [PubMed] [Google Scholar]
- 14.Azziz R. Adenomyosis: Current perspectives. Obstet Gynecol Clin North Am. 1989;16:221–35. [PubMed] [Google Scholar]
- 15.Siedler D, Laing FC, Jeffry RB, Jr, Wing VW. Uterine adenomyosis. A difficult sonographic diagnosis. J Ultrasound Med. 1987;6:345–9. doi: 10.7863/jum.1987.6.7.345. [DOI] [PubMed] [Google Scholar]
- 16.Vercellini P, Cortesi H, De Giorgi O, Merlo D, Carinelli GS, Crosignani PG. Transvaginal ultrasonography versus uterine needle biopsy in the diagnosis of diffuse Adenomyosis. Hum Reprod. 1998;13:2884–7. doi: 10.1093/humrep/13.10.2884. [DOI] [PubMed] [Google Scholar]
- 17.Atri M, Reinhold C, Mehio AR, Chapman WB, Bret PM. Adenomyosis: US feature with histologic correlation in an in vitro study. Radiology. 2000;215:783–90. doi: 10.1148/radiology.215.3.r00jn06783. [DOI] [PubMed] [Google Scholar]
- 18.Kepkep K, Tuncay YA, Goynumer G, Tutal E. Transvaginal sonography in the diagnosis of Adenomyosis: Which findings are most accurate? Ultrasound Obstet Gynecol. 2007;30:341–5. doi: 10.1002/uog.3985. [DOI] [PubMed] [Google Scholar]
- 19.Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol. 2002;186:409–15. doi: 10.1067/mob.2002.121725. [DOI] [PubMed] [Google Scholar]


