Abstract
Scabies is an infestation caused by Sarcoptes scabiei, characterized by polymorphous lesions that may include burrows, papules, nodules, excoriation, and crusts. Vesicular and bullous lesions are rather rare. Bullous scabies is regarded as a distinct subtype of scabies, closely resembling bullous pemphigoid. Here, we report a case of bullous scabies in an adult male and review the literature.
Keywords: Adult, bullous, scabies
INTRODUCTION
Scabies, a contagious infestation caused by the human mite, Sarcoptes scabiei, affects all races and social classes worldwide.
The most common presentations of scabies include classic burrows, pruritic papules, and inflammatory nodules, although in the crusted variant, thick hyperkeratoses with numerous mites predominate. Sometimes, secondary lesions like impetigo or folliculitis, eczematous changes or pseudolymphoma, and some atypical presentations such as urticaria, Darier's disease, dermatitis herpetiformis, and bullous pemphigoid may be seen.[1,2]
In communities where scabies is not endemic, the index of suspicion is low, bullous scabies can be confused with vesiculobullous diseases like bullous pemphigoid.[3] Moreover, missing the diagnosis of diseases like scabies can lead to an outbreak among health-care workers.
Bullous lesions over scabies-prone sites, nocturnal itching, genital involvement, detection of mite on histopathology, and response to antiscabies treatment finally confirmed the diagnosis of bullous scabies in our case.
CASE REPORT
A 26-year-old unmarried male presented with a four-day history of multiple blisters over both hands preceded by a two-week history of generalized pruritus. The patient was living alone. He also complained of itchy red raised lesions over the genitals. The itching was more during night. The patient denied any history of unprotected sexual exposure.
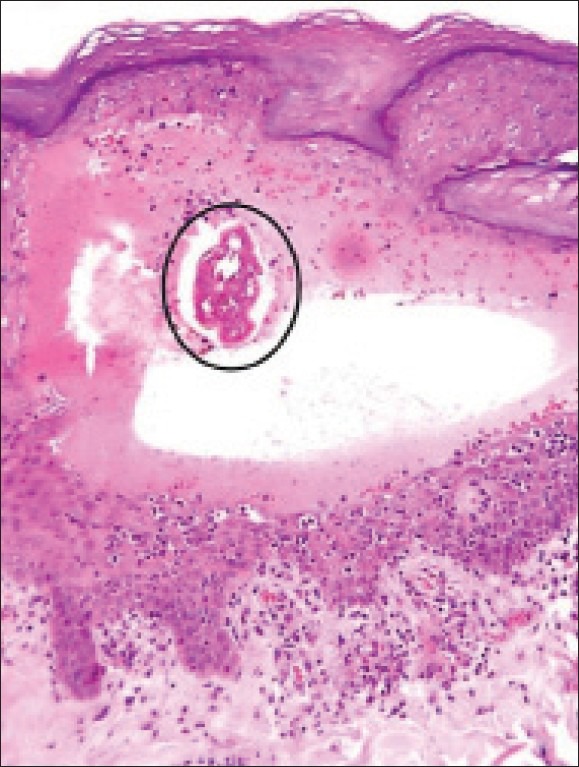
Examination revealed multiple, erythematous excoriated papules on the wrist, trunk, lower limbs, and web spaces of fingers. Multiple erythematous papulonodular lesions were seen over the scrotum and penis. Multiple tense vesicles and bullae, 0.5-1.5 cm sized, containing clear fluid were also present on the dorsum of both hands and web spaces of fingers [Figure 1]. There were no mucosal lesions. Other cutaneous and systemic examination was unremarkable. A diagnosis of bullous scabies was considered.
Figure 1.

(a) Multiple tense blisters over hands with erythematous papules over wrist, (b) papulovesicular lesions over dorsum of right hand, (c) papulovesicle, on the first web space of the left hand, and (d) papulonodular lesions over the the scrotum and glans penis
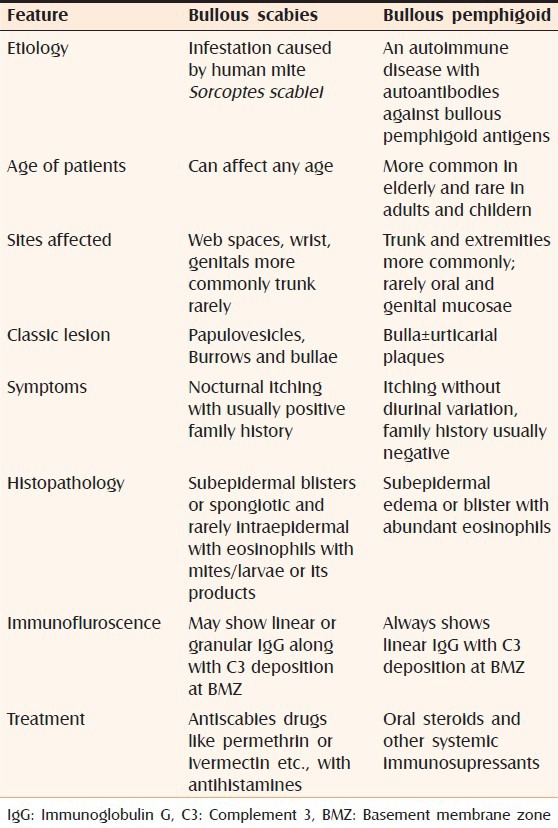
Biopsy and histopathology of one of the vesicles revealed epidermal spongiosis, multilocular intraepidermal blisters, subepidermal edema with dense lymphohistiocytic infiltrate, and a few eosinophils. The blister cavity also contained inflammatory cells with eosinophils being predominant. The presence of mites within the blister cavity was also noted [Figure 2]. Based on clinicopathological correlation, a diagnosis of bullous scabies was made.
Figure 2.
Skin biopsy from lesion showing intraepidermal cleft containing a scabies mite (encircled) and mixed inflammatory infiltrate (H and E, ×100)
Immunofluroscence study could not be done due to economic constraints. The patient was treated with whole-body applications of 5% permethrin lotion and a single 12 mg dose of oral ivermectin along with oral antihistamines to control pruritus. New lesions stopped appearing and after one week, significant improvement was noted. Skin lesions cleared after one month.
DISCUSSION
Bullous lesions are rare in scabies and various mechanisms have been suggested. Superinfection of mite lesions with Staphylococcus aureus could cause blisters, as occurs in bullous impetigo.[1] Autoantibody-mediated bulla formation could occur secondary to (a) exposure of basement membrane zone (BMZ) antigens following physical injury by the mite or lytic enzymatic digestion, or (b) cross reactivity of mite antigens with the BMZ antigens (antigenic mimicry).[2] Bullae may occur as an id reaction to scabietic mites, a process that has been termed scabid.[4] The presence of mites within the intraepidermal blister cavity gives credence to the theory of lytic enzymes of the mite as a cause of blisters.[5]
Regardless of the pathogenesis, lesions consist of pruritic, tense or flaccid large bullae, sometimes hemorrhagic or crusted, in a disseminated distribution in scabies-prone sites with or without classic lesions of scabies.[1,6]
In our review of the literature, there were totally 30 cases of bullous scabies presenting with blister formation with or without classic burrows and itchy papules and nodules of scabies [Table 1].[3,4,5,6,7,8,9] Of the 30 cases, 21 were males and only were 9 females. Our patient was also male. Bullous scabies is typically reported with subepidermal blisters.[1,3,5,6] However, in our case, the blisters were intra epidermal.
Table 1.
Cases of bullous scabies reported in world literature

Because of the clinical and histopathologic similarity of the two conditions, bullous pemphigoid may be difficult to differentiate from bullous scabies.[1,3] The diagnosis of bullous scabies should be considered for any bullous eruption accompanied by papules and itching that are resistant to steroid treatment.[8,9]
Some of the differentiating features between bullous scabies and bullous pemphigoid are summarized in Table 2.
Table 2.
Bullous scabies versus bullous pemphigoid
Treatment of bullous scabies is essentially similar to that of classical scabies. Recurrences have been reported, requiring multiple applications. A short course of oral steroids may be needed for some cases.[4]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ansarin H, Jalali MH, Mazloomi S, Arabshahi RS, Setarehshenas R. Scabies presenting with bullous pemphigoid like lesions. Dermatology online J. 2006;12:19. [PubMed] [Google Scholar]
- 2.Ackerman AB, Stewart R, Stillman M. Scabies masquerading as dermatitis herpetiformis. JAMA. 1975;233:53–4. [PubMed] [Google Scholar]
- 3.Jena DK, Dash ML, Chhetia R. Bullous scabies in patient on anticancer therapy. Indian J Dermatol Venereol Leprol. 2005;71:53–4. doi: 10.4103/0378-6323.13794. [DOI] [PubMed] [Google Scholar]
- 4.Kaur S, Thami GP. Bullous scabies in an adult. Clin Exp Dermatol. 2003;28:93–4. doi: 10.1046/j.1365-2230.2003.01156_2.x. [DOI] [PubMed] [Google Scholar]
- 5.Veraldi S, Scarabelli G, Zerboni R, Pelosi A, Gianotti R. Bullous scabies. Acta Derm Venereol. 1996;76:167–8. doi: 10.2340/0001555576167168. [DOI] [PubMed] [Google Scholar]
- 6.Galvany RL, Salleras RM, Umbert MP. Bullous scabies responding to ivermectin therapy. Actas Dermosifiliogr. 2010;101:81–4. [PubMed] [Google Scholar]
- 7.Wozniacka A, Hawro T, Schwartz RA. Bullous scabies: A diagnostic challenge. Cutis. 2008;82:350–2. [PubMed] [Google Scholar]
- 8.Serra D, Pedro RJ, Mariano A, Machado A, Figueiredo A. Recurrent bullous scabies. J Cutan Med Surg. 2010;14:175–7. doi: 10.2310/7750.2010.09028. [DOI] [PubMed] [Google Scholar]
- 9.Roxana Stan T, Piaserico S, Bordignon M, Salmaso R, Zattra E, Alaibac M. Bullous scabies simulating pemphigoid. J Cutan Med Surg. 2011;15:55–7. doi: 10.2310/7750.2011.10040. [DOI] [PubMed] [Google Scholar]


