Abstract
Sarcoidosis is a multisystem, granulomatous disease of unknown etiology that can affect the pulmonary, reticulo-endothelial, skin, gastrointestinal, cardiac, musculo – skeletal, endocrine or central nervous system. Exclusive cutaneous involvement is very rare in sarcoidosis. Lupus pernio is a variant of cutaneous sarcoidosis presenting with erythematous to violaceous nodules and plaques located symmetrically over the nose, cheeks, ears and digits. We present a case of lupus pernio which showed rapid improvement with topical steroids and has yet not developed any systemic involvement even after 6 years of regular follow up.
Keywords: Cutaneous sarcoidosis, granuloma, lupus pernio
INTRODUCTION
Sarcoidosis is a multisystem, granulomatous disease of unknown etiology that can affect the pulmonary, reticuloendothelial, skin, gastrointestinal, cardiac, musculoskeletal, endocrine, or central nervous system. Though seen in all age groups, it occurs more commonly in the 2nd-4th decades and is more prevalent in females.[1] Cutaneous involvement is seen in 20-35% of patients with sarcoidosis.[1] Exclusive cutaneous involvement is rare and is reported in about 4-5% of total patients of sarcoidosis.[2] Skin lesions assume a vast array of morphologies, hence cutaneous sarcoidosis is known as one of the “great imitators” in dermatology.[3]
Sarcoidosis is uncommonly reported from our country and the cases presenting with skin lesions have been very few.[4,5,6,7,8,9,10,11,12] Lupus pernio variant tends to be associated particularly with other forms of chronic fibrotic sarcoidosis, including upper respiratory tract sarcoidosis, bone cysts, lacrimal gland, and renal sarcoidosis, and with hyperglobulinemia and hypercalcemia. Lupus pernio tends to persist; lesions of more than 2 years standing seldom resolve.[1] The facial disfigurement may cause emotional scarring, which may justify aggressive lines of therapy including plastic surgery.[13]
We report a lupus pernio variant of cutaneous sarcoidosis without systemic involvement even after 6 years of close follow-up.
CASE REPORT
A 50-year-old male presented with multiple asymptomatic erythematous skin lesions over the nose and both ears since 1 year. Patient had not taken any form of treatment for the same. The lesions were progressive and there were no aggravating or relieving factors. There was no history of fever, cough, nasal discharge, loss of sensation, or joint pains. Cutaneous examination revealed erythematous, firm plaques and nodules over tip, base and left ala of nose, right nasolabial fold, both pinna, and preauricular region [Figures 1–3]. General examination and sensory examination were normal. There was no lymphadenopathy. Ophthalmic and systemic examinations were normal. Chest X-ray, routine hemogram, serum, and 24 h urinary calcium were normal. Erythrocyte sedimentation rate was 60 mm in the 1st h. Mantoux test was negative. Slit skin smears for acid fast bacilli and Leishmania donovani bodies were negative. Pulmonary function tests were normal. Angiotensin-converting enzyme levels were not done due to lack of resources. Skin biopsy revealed multiple, circumscribed, non-caseating tuberculoid granuloma with epithelioid cells and occasional giant cell [Figures 4 and 5]. Wade Fite and Periodic acid-Schiff (PAS) stain were negative. He was treated with betamethasone dipropionate 0.05% cream twice daily application. Within 6 months, skin lesions improved drastically. Patient is on follow-up for 6 years now and has not developed any new skin lesions or systemic involvement yet [Figures 6–8].
Figure 1.
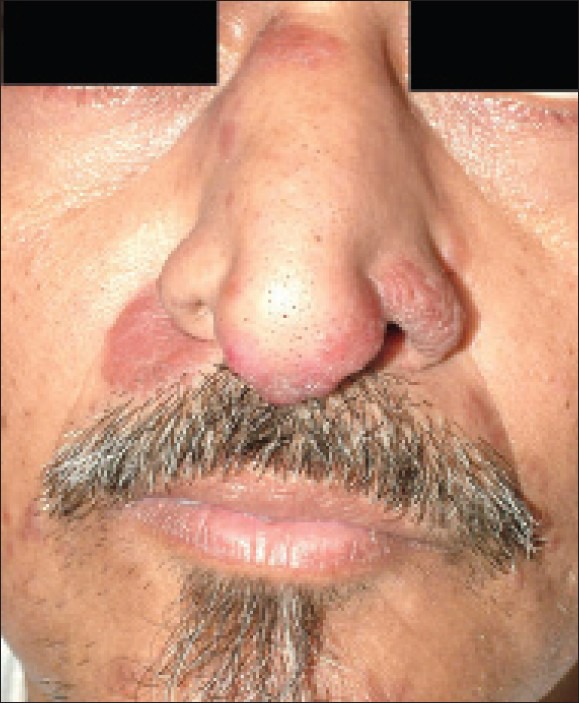
Plaques and nodules involving nose
Figure 3.

Left ear with nodules and plaques
Figure 4.
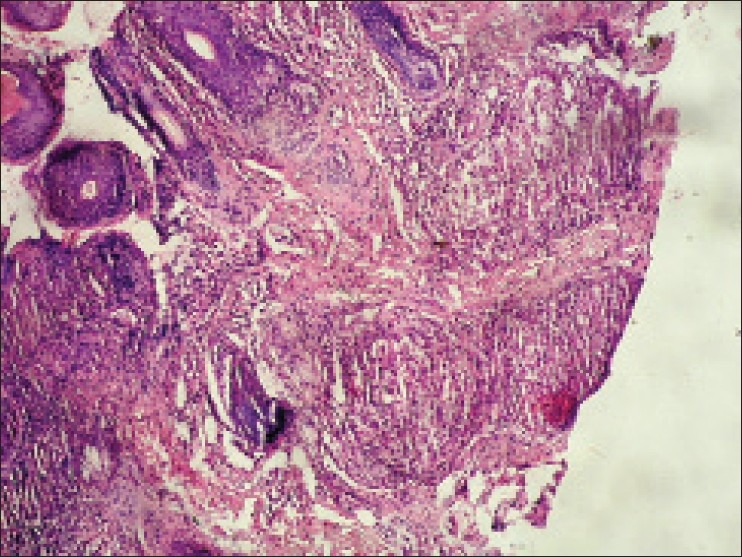
Histopathology (H & E ×100) shows naked granulomas consisting of epithelioid cells
Figure 5.
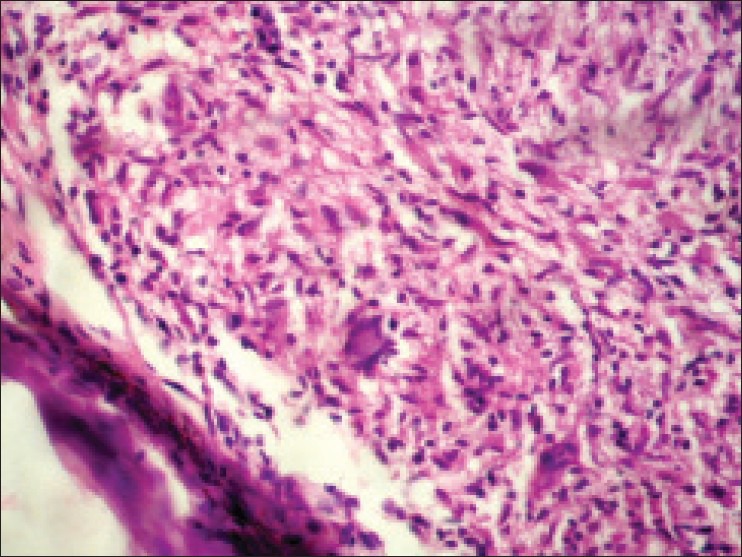
Histopathology (H & E ×400) shows a Langhans giant cell and numerous epithelioid cells
Figure 6.
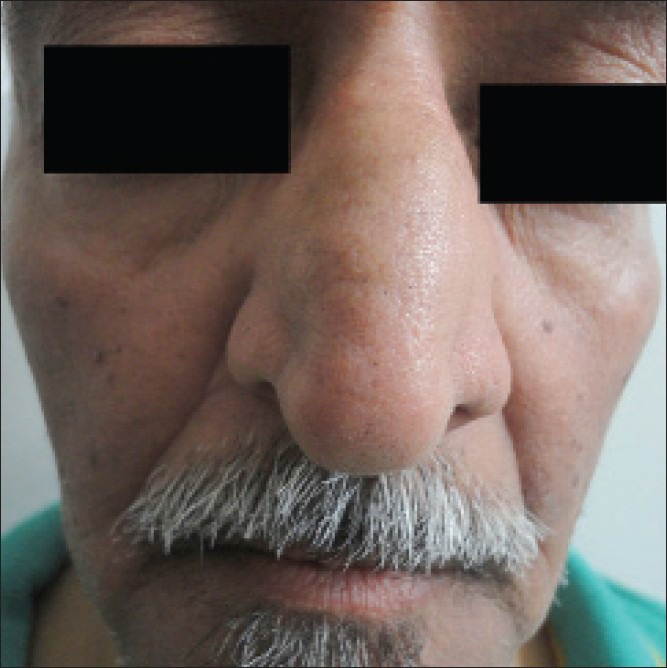
Complete resolution of lesions after treatment
Figure 8.

Complete resolution of lesions after treatment
Figure 2.

Right ear with nodules and plaques
Figure 7.

Complete resolution of lesions after treatment
DISCUSSION
The earliest description of a case which would now be categorized as sarcoidosis was probably Besnier's report in 1889 of an association between reddish-blue lesions of the face and nose with swellings of the fingers; the name “Lupus pernio” reflected his view that this might be a variant of lupus vulgaris. In 1898, Hutchinson described two more cases of a skin eruption, probably sarcoidosis, to which he gave the name of “Mortimer's malady” after one of his patients. Around the same time, Boeck in 1899 recorded his “multiple benign sarkoid of the skin,” and the current term “sarcoidosis” stems from his misinterpretation of the histological changes. However, it was Boeck who first developed the concept of a disease involving both the skin and internal organs.[1]
In India, first case was reported in 1957 by Rajam et al.[6] In about 20% of cases of sarcoidosis, the skin lesions appear before the systemic disease, in 50% there is a simultaneous appearance of the skin and the systemic disease, and in 30% the skin lesions appear upto 10 years after the systemic disease has occurred.[14] Cutaneous involvement may be classified as specific, which reveals granulomas on biopsy or non-specific, which is mainly reactive such as erythema nodosum.[14]
The cause of sarcoidosis remains unknown; it is not even clear whether the condition has only one or many causes. Infectious bacterial agents such as mycobacterium, propionibacterium, and fungal agents such as histoplasma, cryptococcosis, and others have all been implicated. Evidence from genetic and environmental sources has been inconclusive, and immunological studies have, perhaps, raised more questions than they have solved. Speculations now lie in two main areas: Infectious causes and genetic factors both of which may be interlinked.[1]
Sarcoidosis presenting with cutaneous lesions is quite uncommon and cutaneous sarcoidosis lupus pernio variant without systemic involvement is even rare. Although there are numerous therapeutic options for sarcoid, little data exist regarding which therapy is best suited for the various cutaneous manifestations. Systemic glucocorticoids are generally beneficial for all patients with sarcoid, although long-term use of high doses is not recommended. Intralesional injections of triamcinolone acetonide is suited for limited skin disease.[12]
Various other treatment modalities mentioned in literature are chloroquine, hydroxychloroquine, methotrexate, azathioprine, cyclophosphamide, thalidomide, and also Tumor necrosis factor (TNF) inhibitors like infliximab.
Cutaneous sarcoidosis is often difficult to differentiate from leprosy, leishmaniasis, lupus vulgaris, granuloma annulare, acne agminata, etc.
Only keen observation, clinical awareness, and essential investigations will help in avoiding confusion with other similar skin diseases. This case is unique because, firstly lupus pernio variant has been a rarity in India, second is the drastic improvement with topical steroids and lastly the absence of other systemic involvement over the last 6 years.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gawkrodger DJ. Sarcoidosis. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rooks Textbook of Dermatology. Vol. 3. Massachusetts: Blackwell Science Ltd; 2010. pp. 61.1–21. [Google Scholar]
- 2.Hanno R, Needelman A, Eiferman RA, Callen JP. Cutaneous sarcoidal granulomas and the development of systemic sarcoidosis. Arch Dermatol. 1981;117:203–7. [PubMed] [Google Scholar]
- 3.Reddy RR, Shashi Kumar BM, Harish MR. Cutaneous sarcoidosis: A great masquerader: A report of three interesting cases. Indian J Dermatol. 2011;56:568–72. doi: 10.4103/0019-5154.87158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mishra RS, Indira C, Saxena U, Mukherjee A. Cutaneous sarcoidosis. Indian J Dermatol Venereol Leprol. 1993;59:190–3. [Google Scholar]
- 5.Bajaj AK, Lai M, Gupta SC, Dwivedi SC, Shukla SK. Sarcoidosis a case report. Ind J Dermatol Venereol Leprol. 1979;45:459–62. [PubMed] [Google Scholar]
- 6.Rajam RV, Vishwanathan GS, Rangaiah PN, Misra RS, Saxena P, Indira U, et al. Sarcoidosis a short review with a case report. Indian J Dermatol Venereol Leprol. 1957;23:97–135. [Google Scholar]
- 7.Ramanujam K. Tuberculoid leprosy or sarcoidosis? A diagnostic dilemma. Lepr India. 1982;54:318–23. [PubMed] [Google Scholar]
- 8.Mahajan VK, Sharma NL, Sharma RC, Sharma VC. Cutaneous sarcoidosis: Clinical profile of 23 Indian patients. Indian J Dermatol Venereol Leprol. 2007;73:16–21. doi: 10.4103/0378-6323.30645. [DOI] [PubMed] [Google Scholar]
- 9.Ghorpade A, Ramanan C. Cutaneous sarcoidosis. Indian J Dermatol Venereol Leprol. 1996;62:171–2. [PubMed] [Google Scholar]
- 10.Warrier S, Muhammed Fassaludeen AS, Safia B. Cutaneous sarcoidosis with tuberculoid granuloma. Indian J Dermatol Venereol Leprol. 2002;68:300–1. [PubMed] [Google Scholar]
- 11.Singh G, Sangolli P, Dash K, Grove S. Cutaneous sarcoidosis without systemic involvement. Indian J Dermatol Venereol Leprol. 2000;66:43–4. [PubMed] [Google Scholar]
- 12.Mohanty R, Singh SN, Bhattamishra AB. Cutaneous sarcoidosis without systemic manifestations. Indian J Dermatol. 2009;54:80–2. [Google Scholar]
- 13.Yanardag H, Pamuk ON, Pamuk GE. Lupus pernio in sarcoidosis: Clinical features and treatment outcomes of 14 patients. J Clin Rheumatol. 2003;9:72–6. doi: 10.1097/01.RHU.0000062509.01658.d1. [DOI] [PubMed] [Google Scholar]
- 14.James WD, Berger TG, Elston DM. Andrews’ Diseases of the Skin. 11th ed. Philadelphia: Saunders Elsevier; 2011. Macrophage/Monocyte Disorders; p. 700. [Google Scholar]


