Abstract
Follicular mucinosis is an uncommon inflammatory disorder that characteristically presents as follicular papules and/or indurated plaques. The face, neck, and scalp are the most frequently affected sites, although lesions may occur on any site of the body. Histologically, the disorder is characterized by mucin deposition in the follicular epithelium. The condition is frequently divided into primary and secondary forms, with the latter form frequently associated with mycosis fungoides. In this case report, we describe a child with follicular mucinosis of the back and trunk and discuss the clinical variants, histopathological pattern, and treatment options.
Keywords: Alopecia mucinosa, follicular mucinosis
INTRODUCTION
Follicular mucinosis is a rare disorder. The primary form occurs in children and young adults. In the absence of other disorders, it commonly shows localized lesions of the face, head and neck that have a tendency to resolve within two months to two years. There are no clinical criteria to distinguish primary cases from cases associated with mycosis fungoides (MF); however, most patients with limited involvement tend to have a benign course. Despite this assumption, follow-up is essential.
CASE REPORT
A 5-year-old girl child presented with a two-year history of a non-pruritic, occasionally scaly spots initially present on the back, which spread to involve the trunk. The child was otherwise healthy with a past medical history of atopic dermatitis and no previous surgeries. Her medications included: multi-vitamin, fish oil, and vitamin D.
In her family history, her mother had seasonal allergies and father had hypertension and basal cell carcinoma.
Upon examination, there were orange-tan, patches with follicular papules involving the trunk [Figures 1 and 2]. At that time, no laboratory tests were ordered. Previous biopsies completed in 2010 and early 2012 showed “Conspicuous patchy infiltrates of lymphocytes associated with hair follicles at the level of the infundibulum and isthmus, associated with mild focal follicular spongiosis and vacuolar alteration of the interface between the outer root sheath and the dermis. Additional findings include lymphocytes that are sparse superficial perivascular and intraepidermal, a rare necrotic keratinocyte, and focal smudging of the dermoepidermal junction.” Another biopsy of the upper and lower back was performed on 02/16/2012 and showed the following: “The findings in these two specimens are identical to those in the previous biopsies, with lymphocytic infiltrates that surround, and involve, follicular infundibular and isthmic epithelium [Figures 3–7]. Associated follicular epithelial spongiosis is, for the most part, mild, though there is focal spongiosis that may be graded as moderate. Colloidal iron stains at multiple levels from both specimens demonstrate mucin, both within the infundibular epithelium and the perifollicular sheath. Immunohistochemical stains performed on Specimen “2” (Upper back) reveal a mild loss of CD7 positivity (approximately 40% of cells staining overall), when compared with CD3, CD2, and CD5, CD4 and CD8 stains reveal an overall helper: Suppressor ratio of approximately 5:1, while CD45RO and CD45RB appear to stain cells in both compartments in a roughly equal fashion.” Upper back: “molecular gene rearrangements negative.” The diagnosis: Follicular mucinosis.
Figure 1.

Follicular mucinosis back
Figure 2.

Follicular mucinosis back close up photograph
Figure 3.
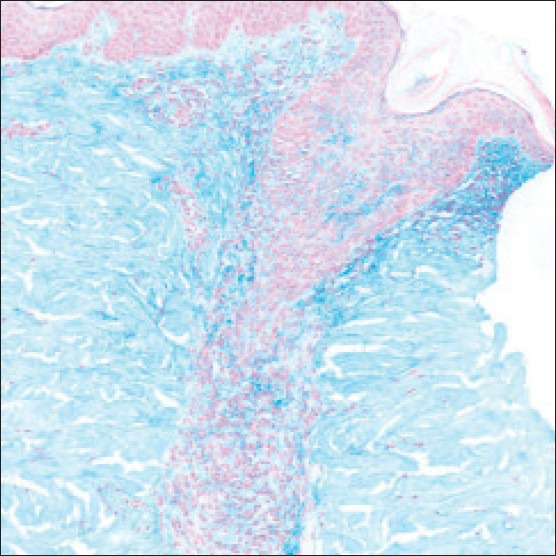
Colloidal Iron stain, ×20, biopsy performed in 2012
Figure 7.
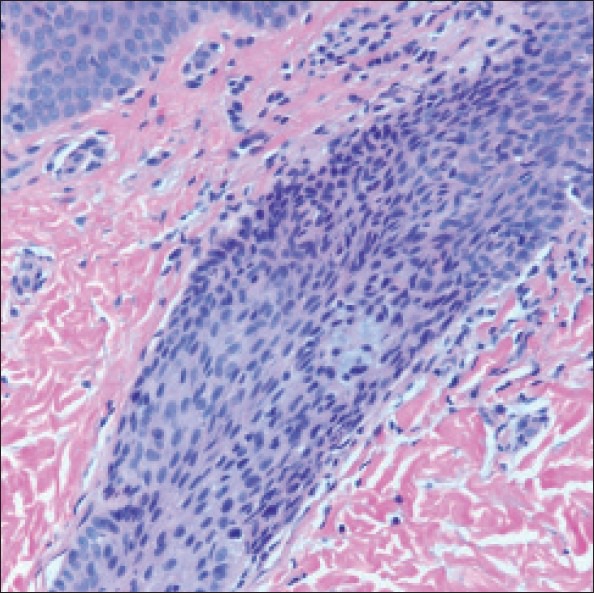
H and E, ×40, biopsy performed in 2010
Figure 4.
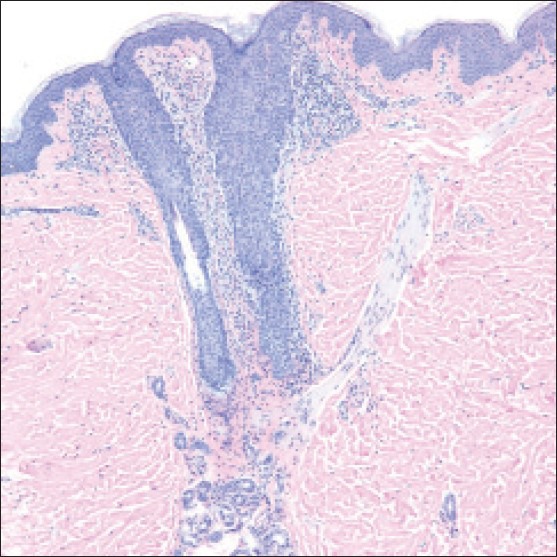
H and E, ×10, biopsy performed in 2012
Figure 5.
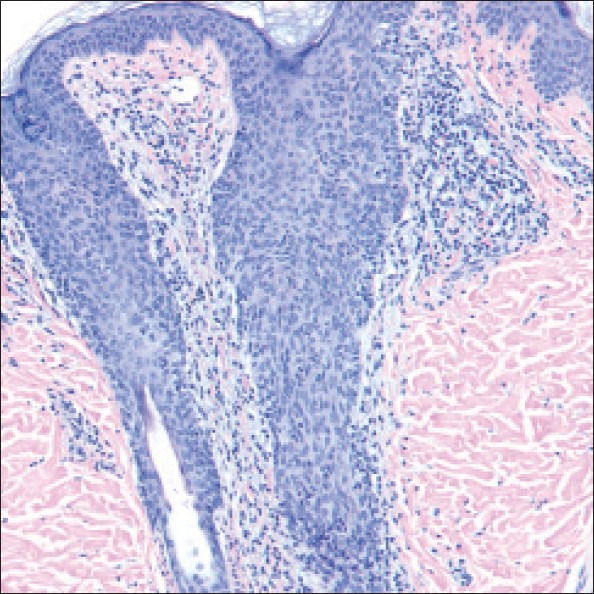
H and E, ×20, biopsy performed in 2012
Figure 6.
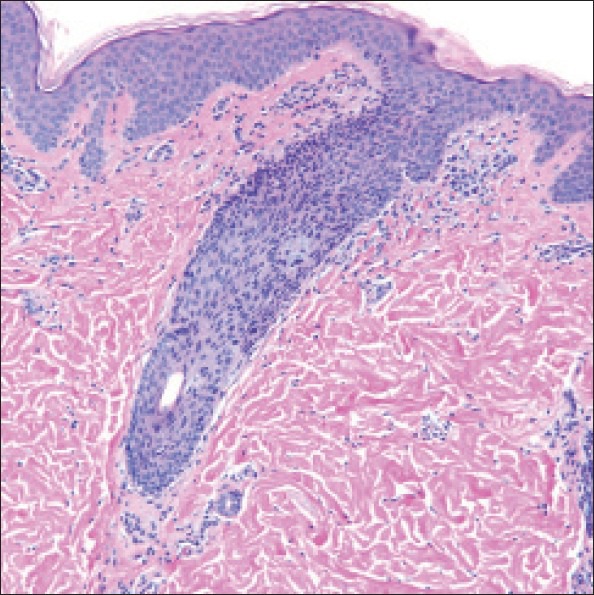
H and E, ×20, biopsy performed in 2010
DIAGNOSIS: FOLLICULAR MUCINOSIS
DISCUSSION
Pinkus first reported alopecia mucinosa in 1957 and the term follicular mucinosis (FM) was introduced in 1959. Patients most commonly present with follicular papules and indurated plaques and hair loss.[1] It is a disease process characterized by mucin deposition within the follicular epithelium with a superficial and deep perivascular and interstitial mixed-cell infiltrate. Previous reports have shown variation in the amount of follicular mucin. The follicular keratinocytes have been considered to be the source of mucin. The exact pathogenesis is unknown, although the role of circulating immune complexes and cell-mediated immunity has been considered including a reaction to persistent antigens such as Staphylococcus aureus.[2] Clinicohistopathologic correlation favored a diagnosis of follicular mucinosis in our patient.
The dermatosis can have several clinical variants. Primary (idiopathic) follicular mucinosis (PFM) can occur in children and young adults as well as older adults. PFM is also considered to be an idiopathic, benign and transient form of the disease. PFM in young people tends to involve the head and neck, with resolution after 2 to 24 months. Most of the cases have a benign course and demonstrate spontaneous resolution in the pediatric population. However, rare case reports of the development of Hodgkin's disease, other lymphomas, and leukemia have been seen. PFM in older adults usually has widespread lesions and can last indefinitely.[1] Secondary follicular mucinosis (SFM) usually occurs in older patients and is associated with an underlying inflammatory or neoplastic condition, with mycosis fungoides (MF) being the most common malignancy.[2]
Unfortunately, no clinical or histopathological pattern is predictive of its course or can reliably differentiate the two entities. Many have proposed criteria to differentiate PFM from SFM with considerable difficulty. It has been suggested that patients with clonal TCR gene rearrangements may be at a higher risk for the development of lymphoma, although long-term follow-up of seven patients younger than forty years of age failed to show progression to MF despite the presence of a clonal TCR gene rearrangement.[3]
There are no specific treatments for idiopathic FM. A wait and see approach is usually recommended and most cases resolve within 2 to 24 months. Current treatment options include: topical, intralesional and systemic corticosteroids, dapsone, antimalarials, isotretinoin, indomethacin, dapsone, and interferon, minocycline. And photodynamic therapy. Sufficient long-term follow-up may be the ultimate criteria to assess the biologic nature of this entity.[4] Our patient began using topical corticosteroids with no real improvement. She was also offered photodynamic therapy, but her parents declined and decided to continue close monitoring and follow-up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lockshin BN, Khachemoune A, Cohen C. Follicular mucinosis in a 4-year-old boy. Int J Dermatol. 2004;43:950–2. doi: 10.1111/j.1365-4632.2004.01954.x. [DOI] [PubMed] [Google Scholar]
- 2.Rongioletti F, De Lucchi S, Meyes D, Mora M, Rebora A, Zupo S, et al. Follicular mucinosis: A clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides-associated follicular mucinosis. J Cutan Pathol. 2010;37:15–9. doi: 10.1111/j.1600-0560.2009.01338.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown HA, Gibson LE, Pujol RM, Lust JA, Pittelkow MR. Primary follicular mucinosis: Long-term follow-up of patients younger than 40 years with and without clonal T-cell receptor gene rearrangement. J Am Acad Dermatol. 2002;47:856–62. doi: 10.1067/mjd.2002.124604. [DOI] [PubMed] [Google Scholar]
- 4.Parker SR, Murad E. Follicular mucinosis: Clinical, histologic, and molecular remission with minocycline. J Am Acad Dermatol. 2010;62:139–41. doi: 10.1016/j.jaad.2009.01.031. [DOI] [PubMed] [Google Scholar]


