Abstract
Progressive symmetric erythrokeratoderma (PSEK) is a rare genodermatosis with variable inheritance. It is characterized by symmetrical, erythematous, and hyperkeratotic plaques on the extremities. We report a case of a 15-year-old boy with PSEK of autosomal recessive inheritance associated with nephrotic syndrome.
Keywords: Erythrokeratoderma, nephrotic syndrome, symmetric
INTRODUCTION
Progressive symmetric erythrokeratoderma (PSEK) or Gottron's syndrome is a rare genodermatosis with variable inheritance, but mostly follows an autosomal dominant pattern.[1] It is characterized by stable, well-demarcated, symmetric hyperkeratotic plaques. Approximately 40 cases have been described in literature. There are few case reports of association of PSEK with other disorders. We report a rare case of PSEK associated with nephrotic syndrome.
CASE REPORT
A15-year-old boy born of second-degree consanguineous marriage presented with asymptomatic scaly skin lesions on the extremities since 5 years. Lesions initially started on dorsum of feet, and gradually progressed to involve knees and hands. These lesions were persistent and nonmigratory. There was no history of similar skin eruptions in the family or siblings. He had steroid-dependent nephrotic syndrome from infancy.
Cutaneous examination showed well-demarcated, hyperpigmented, hyperkeratotic scaly plaques distributed symmetrically on the dorsum of hands and feet, elbows, knees, and tendoachillies [Figures 1–3]. Palms and soles were normal. There was no abnormality of hair, nails, or mucous membrane. There was no musculoskeletal or ocular abnormality. He had puffiness of face with cushingoid features and pedal edema. Skin biopsy revealed hyperkeratosis, focal parakeratoses, acanthosis, normal granular layer, and a moderate mononuclear infiltration in upper dermis [Figure 4]. Based on clinical and histopathological findings, diagnosis of PSEK was made. He was treated with emollients, topical steroids, and keratolytics with marked improvement.
Figure 1.

Well-demarcated hyperkeratotic plaques on dorsum of hands
Figure 3.

Well-demarcated symmetrical hyperpigmented, hyperkeratotic plaques on knee joint and dorsum of feet
Figure 4.
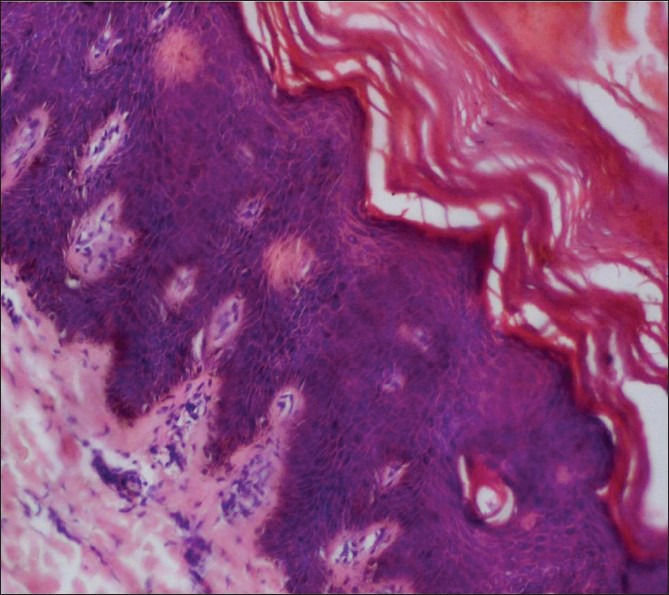
Moderate acanthosis, hyperkeratosis, focal parakeratosis, and mild superficial perivascular dermal lymphocytic infiltrate (H and E, ×400)
Figure 2.

Well-demarcated symmetrical hyperkeratotic plaques on dorsum of feet and lower legs
DISCUSSION
Erythrokeratodermas are rare genodermatosis inherited as autosomal dominant disorders, although autosomal recessive transmission has been observed with high penetrance but marked intra- and interfamilial variability of expression. Erythrokeratodermas have been divided into two major non-syndromic types and some syndromes such as KID (keratitis, ichthyosis, deafness) syndrome and HID (hystrix like, ichthyosis, deafness) syndrome.[2] The two major non-syndromic types have been described as PSEK and erythrokeratoderma variabilis (EKV).[3] It was first described by Darier in 1911 as “progressive and symmetrical verrucous erythrokeratoderma.” Gottron shortened the name of this condition to “symmetrical progressive erythrokeratoderma.”[4] PSEK is heterogeneous with considerable phenotypic variability. Although some cases have been identified to have loricrin and few to have connexin mutations in PSEK, EKV, or both, recent reports show that the same gene mutations were not found in some pedigree of PSEK.[5]
PSEK usually appears in infancy or childhood, and shows an equal sex incidence. Skin lesions are characterized by fixed, large, well-defined hyperkeratotic plaques, or reddish orange to brownish color with marked erythema at their periphery. They are symmetrically distributed. Lesions commonly occur on limbs, buttocks, shoulders, and fingers, and may involve the face.[6] There is marked tendency for improvement after puberty, but may persist into adulthood. An erythematous palmoplantar keratoderma is seen in about 50% of patients.[6]
PSEK has to be differentiated from pityriasis rubra pilaris, psoriasis, and other types of erythrokeratoderma, especially EKV. It differs from EKV in the absence of migratory erythematous lesions and in greater incidence of palmoplantar keratoderma. The symmetry of the lesions in PSEK is more striking than in EKV.[6] Two sisters have been described, among whom the younger one suffered from EKV whereas the older one suffered from PSEK, and this report brought forward the hypothesis that PSEK and EKV were different manifestations of a single condition.[7]
The histopathology is nonspecific and shows hyperkeratosis with patchy parakeratoses overlying an acanthotic epidermis with intact granular layer.[6] Various reports are published in literature regarding association of PSEK with high-arched palate, fissured tongue, pectus excavatum, symmetric syndactylism, and keratosis pilaris.[8,9] Recently PSEK associated with delayed intellectual milestones and convulsions has been reported.[10] In our case, PSEK was associated with nephrotic syndrome. Topical emollients, keratolytics, and topical steroids have limited benefit, but oral retinoid therapy may result in improvement.[11] There was marked improvement with topical steroids and keratolytics in our case.
It is not known whether there is underlying genetic cause for association of PSEK with nephrotic syndrome or it is just a coincidence. This case is interesting not only for its rarity but also for its rare association with nephrotic syndrome, which is not described in literature earlier and hence reported.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Walia NS, Raj R, Tak CS. Gottron's syndrome. Indian J Dermatol Venereol Leprol. 2001;67:211. [PubMed] [Google Scholar]
- 2.van Steensel MA, van Geel M, Nahuys M, Smitt JH, Steijlen PM. A novel connexin 26 mutation in a patient diagnosed with keratitis-ichthyosis-deafness syndrome. J Invest Dermatol. 2002;118:724–7. doi: 10.1046/j.1523-1747.2002.01735.x. [DOI] [PubMed] [Google Scholar]
- 3.Bongiorno MR, Aricò M. Progressive symmetric erythrokeratodermia associated with oligodontia, severe caries, disturbed hair growth and ectopic nail: A new syndrome? Dermatology. 2008;217:347–50. doi: 10.1159/000155648. [DOI] [PubMed] [Google Scholar]
- 4.Gottron HA. Congenital symmetrical progressive erythrokeratoderma. Arch Dermatol Syph. 1923;7:416. [Google Scholar]
- 5.Yan H, Zhang J, Liang W, Zhang H, Liu J. Progressive symmetric erythrokeratoderma: Report of a Chinese family. Indian J Dermatol Venereol Leprol. 2011;77:597–600. doi: 10.4103/0378-6323.84070. [DOI] [PubMed] [Google Scholar]
- 6.Ruiz-Maldonado R, Tamayo L, del Castillo V, Lozoya I. Erythrokeratoderma progressive symmetrica: report of 10 cases. Dermatologica. 1982;164:133–41. [PubMed] [Google Scholar]
- 7.Macfarlane AW, Chapman SJ, Verbov JL. Is erythrokeratoderma one disorder? A clinical and ultrastructural study of two siblings. Br J Dermatol. 1991;124:487–91. doi: 10.1111/j.1365-2133.1991.tb00632.x. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S, Kataria U. Symmetrical progressive erythro-keratoderma. Indian J Dermatol Venereol Leprol. 1999;65:191–2. [PubMed] [Google Scholar]
- 9.Jaiswal AK. Progressive symmetric erythrokeratoderma associated with symmetric syndactylism. Indian J Dermatol Venereol Leprol. 1994;60:343–4. [Google Scholar]
- 10.Verma SB, Uwe W. Progressive symmetric erythrokeratodermia with delayed intellectual milestones and convulsions. Indian Dermatol Online J. 2012;3:54–6. doi: 10.4103/2229-5178.93502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van de Kerkhof PC, Steijlen PM, van Dooren-Greebe RJ, Happel R. Acitretin in the treatment of erythrokeratodermia variabilis. Dermatologica. 1990;181:330–33. doi: 10.1159/000247841. [DOI] [PubMed] [Google Scholar]


