Sir,
Piezogenic pedal papules are uncommon skin-colored asymptomatic papules that are observed more frequently among healthy adults and children.[1] Four patients who initially presented with thick, skin-colored papules on the feet that became pronounced after physical activity and standing were diagnosed with piezogenic pedal papules. We report these cases due to its rarity.
CASE 1
A 19-year-old female admitted for numerous soft and round lesions on the heels that became prominent with standing. The lesions initially appeared on the lateral and posterior parts of both feet, and their size and number continued to increase over time. Standing and walking resulted in a continuous pain in the heels that gradually intensified. The pain subsided with the cessation of standing and walking, and also by applying pressure in areas of the feet other than the heels. The patient had no previous history of feet injuries and of excessive or continuous pressure exerted on the feet (due to factors such as excessive weight, jumping, etc.).
When no pressure was applied to the lesions, they presented as soft, round, skin-colored and about 0.1-0.4 cm diameter papules on the outer edges of the heels. Under pressure, the lesions became harder, tense and painful [Figure 1a]. One papular lesion was completely excised from the lateral of the patient's left foot. A histopathological evaluation revealed hyperkeratosis, irregular acanthosis, thickening of the dermis and small fat cell populations in the dermis (H-E staining, ×5) [Figure 2]. As the patient had complaints of pain and did not wish to undergo surgery, intralesional corticosteroid injection was performed twice. No improvement or recovery was detected on follow-up visits. The patient is currently under follow-up.
Figure 1.

(a and b) Pedal papules of case 1 and case 2
Figure 2.
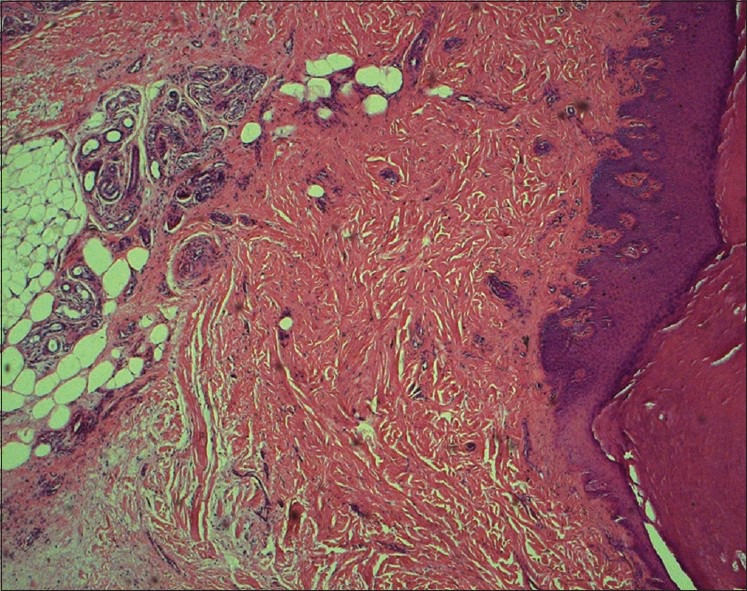
Hyperkeratosis, irregular acanthosis, thickening of the dermis and small fat cell populations in the dermis (H and E staining, ×5)
CASES 2 AND 3
A 43- and a 45-year-old female patients presented to our clinic due to prominent papules on the heels over the past years. The clinical features were similar, but less prominent compared to Case 1 [Figure 1b]. Echocardiography examination of Case 2 showed mitral and tricuspid insufficiency. Histopathological findings of Case 2 were similar to Case 1. Intralesional steroid injections were performed in both cases; however, no recovery or regression of lesions was achieved.
CASE 4
A 33-year-old male, amateur marathon runner, presented with similar papules for over a year that gradually increased in number over the past 3 months. Clinically, the number of lesions was less compared to the other cases. He did not accept to have a biopsy, so histopathological analysis was not able to be performed. Intralesional steroid injection was not helpful.
Piezogenic papules are constituted of herniations of fat tissue into weight-carrying connective tissue of the heels.[1,2] They occur as a result of continuous pressure on the heels, as a result of factors such as excessive weight, jumping, running, or carrying heavy loads. The pain appears to be caused from the continuous contact between the papules and footwear, although some have proposed that neurovascular anoxia in the lesions may also contribute to the pain.[1,2,3]
Piezogenic papules are generally observed in healthy individuals, sportsmen and especially among marathon runners.[4] It is for this reason it is considered as among the frictional and mechanical dermatoses related to sports and observed among athletes. Of our cases, the third was a marathon runner. Patients with Ehler–Danlos syndrome, Prader Willi syndrome, rheumatic heart disease and rheumatoid arthritis have been reported in the literature.[5,6,7] There are few cases with heart valve disease concomitant to pedal papules that were identified in the literature. Only two cases related with rheumatic valve disease has currently been reported.[8,9]
In the histopathologic findings of piezogenic pedal papules, dermal fibrosis and the herniation of subcutaneous fat tissue from the papillary dermis are observed.[1]
Treatment outcomes are not always satisfactory. Patients successfully treated with compression treatment, intralesional steroid and anesthetic injection[10] have been reported in literature. Changes in footwear and orthopedic support are also known to alleviate the pain and symptoms associated with the papules. Surgery options including the excision of the papules as well as a sealing of the existing hernia can also be performed in patients received unsuccessful conservative treatments. The surgery option is more effective than the conservative methods.[2] Since our cases did not want to have surgery, a combination of triamcinolone and lidocaine was injected intralesionally into the larger lesions. However, this treatment was not successful in all of the cases.
In conclusion, piezogenic pedal papule is a benign pathology that has been identified in the past four decades. It is presumed to be observed more frequently than it has been reported. As observed in our four cases, different associations can be observed in its etiology. It is overlooked by certain physicians, while other physicians that are unfamiliar with the pathology may not be able to diagnose it. There are no accompanying systemic diseases in most cases. It is important to relieve the patients’ concern regarding its process, and to attempt various treatment options in symptomatic individuals.
REFERENCES
- 1.Graham BS, Barrett TL. Solitary painful piezogenic pedal papule. J Am Acad Dermatol. 1997;36:780–1. doi: 10.1016/s0190-9622(97)80346-5. [DOI] [PubMed] [Google Scholar]
- 2.Montgomery F, Fioriti A. Piezogenic pedal papules: Treated by resection and hernial closure. The Foot. 1998;8:171–2. [Google Scholar]
- 3.Shelley WB, Rawnsley HM. Painful feet due to herniation of fat. JAMA. 1968;205:308–9. [PubMed] [Google Scholar]
- 4.Redbord KP, Adams BB. Piezogenic pedal papules in a marathon runner. Clin J Sport Med. 2006;16:81–3. doi: 10.1097/01.jsm.0000180871.22426.60. [DOI] [PubMed] [Google Scholar]
- 5.Ronnen M, Suster S, Huszar M, Schewach-Millet M. Solitary painful piezogenic pedal papule in a patient with rheumatoid arthritis. Int J Dermatol. 1987;26:240–1. doi: 10.1111/j.1365-4362.1987.tb00909.x. [DOI] [PubMed] [Google Scholar]
- 6.Kahana M, Feinstein A, Tabachnic E, Schewach-Millet M, Engelberg S. Painful piezogenic pedal papules in patients with Ehlers-Danlos syndrome. J Am Acad Dermatol. 1987;17:205–9. doi: 10.1016/s0190-9622(87)70192-3. [DOI] [PubMed] [Google Scholar]
- 7.Schepis C, Greco D, Siragusa M, Romano C. Piezogenic pedal papules during Prader-Willi syndrome. J Eur Acad Dermatol Venereol. 2005;19:136–7. doi: 10.1111/j.1468-3083.2004.01048.x. [DOI] [PubMed] [Google Scholar]
- 8.Singh SK, Tehseen M, Kalam A. Painless piezogenic pedal papules in a patient with rheumatic heart disease. Indian J Dermatol Venereol Leprol. 2002;68:107–8. [PubMed] [Google Scholar]
- 9.Polat M, Kaya H, Guüven M, Guürel K, Parlak AH. A case of piezogenic pedal papules associated with mitral valve insufficiency. Turkderm. 2012;46:167–9. [Google Scholar]
- 10.Doukas DJ, Holmes J, Leonard JA. A nonsurgical approach to painful piezogenic pedal papules. Cutis. 2004;73:339–40. 346. [PubMed] [Google Scholar]


