Abstract
Human resources for health have been recognized as essential to the development of responsive and effective health systems. Low- and middle-income countries seeking to achieve universal health coverage face human resource constraints – whether in the form of health worker shortages, maldistribution of workers or poor worker performance – that seriously undermine their ability to achieve well-functioning health systems. Although much has been written about the human resource crisis in the health sector, labour economic frameworks have seldom been applied to analyse the situation and little is known or understood about the operation of labour markets in low- and middle-income countries. Traditional approaches to addressing human resource constraints have focused on workforce planning: estimating health workforce requirements based on a country’s epidemiological and demographic profile and scaling up education and training capacities to narrow the gap between the “needed” number of health workers and the existing number. However, this approach neglects other important factors that influence human resource capacity, including labour market dynamics and the behavioural responses and preferences of the health workers themselves. This paper describes how labour market analysis can contribute to a better understanding of the factors behind human resource constraints in the health sector and to a more effective design of policies and interventions to address them. The premise is that a better understanding of the impact of health policies on health labour markets, and subsequently on the employment conditions of health workers, would be helpful in identifying an effective strategy towards the progressive attainment of universal health coverage.
Résumé
Les ressources humaines du secteur de la santé sont essentielles au développement de systèmes médicaux efficaces et réactifs. Les pays à revenu faible et moyen qui cherchent à obtenir une couverture maladie universelle souffrent de restrictions en matière de ressources humaines - que ce soit sous forme de pénurie d'agents de santé, de mauvaise répartition ou de faibles performances des travailleurs - qui compromettent sérieusement leur capacité à créer un système de santé optimal. Même si on a beaucoup écrit au sujet de la crise des ressources humaines dans le secteur de la santé, des cadres économiques de travail ont rarement été appliqués pour analyser la situation, et on connaît ou on comprend peu de choses sur le fonctionnement des marchés du travail dans les pays à revenu faible et moyen. Les approches traditionnelles dans le but de répondre aux restrictions en matière de ressources humaines accordent de l'importance à la planification des effectifs : estimer les besoins en matière de travailleurs de la santé par rapport au profil démographique et épidémiologique d'un pays, et intensifier les capacités de formation et d'enseignement pour réduire l'écart entre le nombre de travailleurs "nécessaire" et le nombre réel. Toutefois, cette approche néglige d'autres facteurs importants qui influent sur la capacité des ressources humaines, notamment les dynamiques du marché du travail et les réponses et préférences comportementales des travailleurs de la santé. Ce document explique comment l'analyse du marché du travail peut aider à mieux comprendre les facteurs qui sont à l'origine des restrictions en matière de ressources humaines dans le secteur de la santé, mais aussi à mettre en oeuvre des politiques et des interventions plus efficaces pour y remédier. L'hypothèse initiale est qu'une meilleure compréhension de l'impact des politiques de santé sur les marchés du travail de la santé et, par ailleurs, sur les conditions d'emploi des travailleurs de la santé, serait utile pour pouvoir identifier une stratégie efficace et progressivement mettre en place une couverture maladie universelle.
Resumen
El papel de los recursos humanos en el sector sanitario se considera esencial para el desarrollo de sistemas sanitarios eficaces y con capacidad de respuesta. Los países de ingresos bajos y medianos que aspiran a alcanzar la cobertura sanitaria universal se enfrentan a las limitaciones en materia de recursos humanos, sea por escasez de personal sanitario, la distribución ineficaz del personal o el desempeño ineficiente del mismo, factores que socavan gravemente la capacidad para lograr sistemas sanitarios con un funcionamiento adecuado. Aunque se ha vertido mucha tinta acerca de la crisis de recursos humanos en el sector sanitario, rara vez se han aplicado los marcos económicos laborales para analizar la situación y poco se sabe o entiende sobre el funcionamiento de los mercados laborales en los países de ingresos bajos y medianos. Los enfoques tradicionales para hacer frente a las limitaciones en materia de recursos humanos se han centrado en la planificación del personal, mediante el cálculo de las necesidades de personal sanitario basada en el perfil epidemiológico y demográfico del país y la ampliación de los recursos educativos y formativos para reducir la brecha entre el número «necesario» de personal sanitario y el número real. Sin embargo, este enfoque deja de lado otros factores importantes que influyen en la capacidad de los recursos humanos, como la dinámica del mercado de trabajo, las respuestas de comportamiento y las preferencias del personal sanitario. Este informe describe cómo el análisis del mercado laboral pretende mejorar la comprensión de los factores que explican la escasez en materia de recursos humanos en el sector sanitario y ofrecer un diseño más eficaz de las políticas e intervenciones para abordarlos. La premisa para ello es que una mejor comprensión del impacto de las políticas sanitarias en el mercado laboral sanitario, y por consiguiente, en las condiciones laborales del personal sanitario, sería de gran ayuda en la identificación de una estrategia eficaz para alcanzar la cobertura sanitaria universal de forma progresiva.
ملخص
تم الاعتراف بضرورة الموارد البشرية الصحية لتطوير أنظمة صحية فعالة وسريعة الاستجابة. وتواجه البلدان المنخفضة والمتوسطة الدخل التي تسعى لتحقيق التغطية الصحية الشاملة قيوداً تتعلق بالموارد البشرية – سواء أكانت في شكل نقص في العاملين الصحيين أو سوء توزيع للعاملين أو الأداء الضعيف لهم – والتي تضعف بشكل خطير من القدرة على إنشاء أنظمة صحية تعمل بشكل جيد. ورغم وجود أبحاث كثيرة حول أزمة الموارد البشرية في القطاع الصحي، إلا انه كان من النادر تطبيق أطر العمل الاقتصادية للعمالة لتحليل الموقف، ولا يوجد سوى القليل من المعرفة والفهم حول تشغيل أسواق العمالة في البلدان المنخفضة والمتوسطة الدخل. وركزت النهج التقليدية للتعامل مع قيود الموارد البشرية على تخطيط قوة العمل: تقدير متطلبات قوة العمل الصحية استناداً إلى الحالة الوبائية والسكانية للبلد والتوسع في نطاق القدرات التعليمية والتدريبية لتضييق الفجوة بين العدد "المطلوب" من العاملين الصحيين والعدد الموجود. ومع ذلك، يهمل هذا الأسلوب عوامل أخرى هامة تؤثر على قدرة الموارد البشرية، بما في ذلك القوى المحركة لسوق العمالة والاستجابات السلوكية وتفضيلات العاملين الصحيين أنفسهم. ويصف هذا البحث كيفية إسهام تحليل سوق العمالة في التوصل إلى فهم أفضل للعوامل التي تقف وراء قيود الموارد البشرية في القطاع الصحي وإلى تصميم أكثر فعالية للسياسات والتدخلات للتعامل معها. وتقوم الفرضية على أن الفهم الأفضل لتأثير السياسات الصحية على أسواق العمالة الصحية، ومن ثم على ظروف توظيف العاملين الصحيين، سيساعد في تحديد إستراتيجية فعالة باتجاه الإدراك المتدرج للتغطية الصحية الشاملة.
摘要
卫生人力资源被公认为发展灵敏有效的卫生系统不可或缺的一环。努力实现全民医疗保障制度的中低收入国家面临着人力资源限制的问题——或是缺乏卫生工作者,或是卫生工作者配置不合理,或是卫生工作者绩效差——这些问题严重削弱了实现完善卫生系统的能力。尽管有关卫生部门人力资源危机的论述为数众多,却很少有研究应用劳动经济框架分析这种状况,人们对中低收入国家劳动力市场的运作了解或认识得非常少。解决人力资源限制问题的传统方法将重点放在劳动力规划上:基于国家的流行病学和人口统计学特征估计卫生工作人员需求,升级教育培训实力来缩短“需要”卫生工作者数量和现有数量之间的差距。但是,这种方法忽略了影响人力资源容量的其他重要因素,包括劳动力市场动力和卫生工作者自身的行为反应和偏好。本文描述了劳动力市场分析对更好理解卫生部门人力资源限制因素的作用,以及对制定更有效应对政策和干预措施的作用。其论述的前提是:更好地理解卫生政策对卫生劳动力市场的影响,继而对卫生工作者就业状况的影响,将有助于识别出逐步实现全民医保的有效战略。
Резюме
Человеческие ресурсы в сфере здравоохранения были признаны необходимым фактором для развития оперативной и эффективной системы здравоохранения. Страны с низким и средним уровнем доходов, стремящиеся обеспечить всеобщий охват населения медико-санитарными услугами, сталкиваются с нехваткой человеческих ресурсов в виде либо нехватки работников здравоохранения, либо неравномерного распределения работников, либо низкой эффективности труда работников, что серьезно подрывает способность данных стран обеспечить хорошее функционирование систем здравоохранения. Хотя уже много написано на тему кризиса человеческих ресурсов в секторе здравоохранения, для анализа ситуации редко применялись экономические концепции, касающиеся труда, и о функционировании рынков труда в странах с низким и средним уровнем дохода мало что известно или мало кто понимает, как они функционируют. Традиционные подходы к решению проблем нехватки человеческих ресурсов были направлены на планирование трудовых ресурсов, то есть на оценку потребности в трудовых ресурсах в сфере здравоохранения на основе эпидемиологического и демографического профиля страны и пропорциональном наращивании возможностей образования и подготовки с целью сократить разрыв между «необходимым» и имеющимся количеством работников здравоохранения. Однако такой подход не учитывает других важных факторов, которые влияют на человеческие ресурсы, в том числе динамику рынка труда и поведенческие реакции и предпочтения самих работников здравоохранения. В этой статье описывается то, как анализ рынка труда может способствовать лучшему пониманию факторов, обуславливающих нехватку человеческих ресурсов в секторе здравоохранения, и разработке более эффективной политики и мероприятий по устранению данных факторов. Исходной посылкой является то, что лучшее понимание влияния политики в области здравоохранения на рынки труда в данной сфере и, соответственно, на условия труда работников здравоохранения может оказаться полезным при выборе эффективной стратегии по постепенному достижению всеобщего охвата населения медико-санитарными услугами.
Health workforce challenges
Human resources for health are central to any health system insofar as health workers perform or mediate most health system functions. They make treatment decisions at the point of service and their actions determine how efficiently other resources are used.1 Health-care delivery is highly labour intensive. To be effective, a health-care system must have the right number and mix of health-care workers and it must ensure that they possess the means and motivation to skilfully perform the functions they are assigned. Many countries are facing a “crisis in human resources for health” that involves three dimensions: availability, which relates to the supply of qualified health workers; distribution, which relates to the recruitment and retention of health workers where their presence is most needed; and performance, which relates to health worker productivity and to the quality of the care that health workers provide.
Traditional approaches to resolving human resource constraints in the health sector have relied primarily on workforce planning, i.e. the practice of estimating health workforce requirements based on a country’s epidemiological and demographic profile and of scaling up education and training capacities to narrow the gap between the existing number of health workers and the number required. However, focusing narrowly on the production of health workers results in the neglect of other important factors that influence human resource capacity, such as labour market dynamics and the behaviour and preferences of the health workers themselves. Thus, despite the extensive published literature on the human resource crisis in the health sector, few analyses have been conducted using labour economic frameworks and the dynamics of labour markets remain little known or understood, especially in low- and middle-income countries.
The health status of a population, its health-care needs and its requirements in the area of human resources for health are linked in complex ways.2 For example, the employment opportunities available to health workers and the type of employment conditions that health workers prefer are not always aligned with priority health-care needs. Health workers may be attracted to positions that do not respond to such needs or may choose to migrate in search of alternative employment opportunities. Sometimes a paradoxical situation arises: vacancies in high-priority positions in the public sector coexist with high unemployment rates among health workers. This paradox is explained by the labour market failure to match the supply and demand for health workers. For instance, several African countries (e.g. Kenya, Mali and Senegal) are experiencing acute under-employment among doctors and nurses, yet they are simultaneously investing substantial public funds in producing more health workers. This worsens underemployment and reduces the efficiency of government expenditures. The system of posting health workers to rural areas further illustrates the limitations of traditional workforce planning. When health workers are officially assigned to a remote rural area, they often find unofficial ways to evade the assignment and find employment in an urban area. These examples highlight the inadequacy of a human resource strategy focused exclusively on the needs-based production of health workers.3
Labour market conditions such as low salaries and a lack of other economic benefits are known to influence employment processes, but their influence on the planned allocation of resources is less widely recognized. Thus, an analysis of the labour market is essential to achieve a better understanding of the forces that drive health worker shortage, maldistribution and suboptimal performance and to develop policies and interventions tailored to different labour market conditions.
What is a labour market?
A market is any structure that allows buyers and sellers to exchange goods, services or information of any type. A labour market is the structure that allows labour services to be bought and sold.4 In a labour market, those who seek to employ staff are the “buyers” and those who seek employment are the “sellers”. A labour market can be delineated according to different criteria: geographical (national or international); occupational (specialized or unspecialized); and sectoral (formal or informal). A special feature of labour markets is that labour cannot be sold but only rented. Furthermore, conditions of employment (e.g. adequate infrastructure, supportive management, opportunities for professional development and career progression) are as important as prices (wages) in determining labour market outcomes. Thus, these outcomes are driven by the behaviour of employers and workers in response to changes in the terms of employment (wages, compensation levels and working conditions).
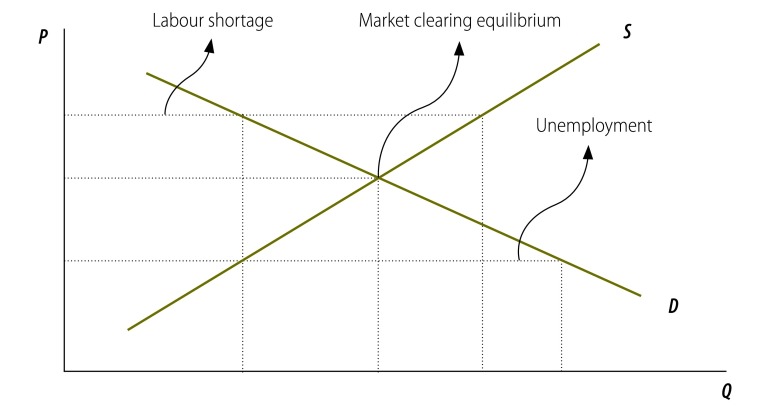
In a well-functioning labour market, wages or “compensation” – which can be understood as the overall return received for employment in a particular post and not only the financial component of that return – act as the mechanism whereby the intentions of buyers and sellers are reconciled. The demand and the supply of labour tend towards equilibrium. A point is reached in which the amount of labour supplied equals the amount demanded at the going level of compensation. Labour markets are said to “clear” when the supply of labour matches the demand for workers. However, labour markets do not always “clear” in this way. When they fail to do so, they exhibit either labour surplus or unemployment (i.e. people seek jobs at the going rate of pay but cannot find them), or labour shortage (i.e. employers seek to fill posts at the going rate of pay but cannot find people to fill them). These possible scenarios are illustrated in Fig. 1.
Fig. 1.
Possible labour market scenarios
Note: The supply curve (S) slopes upward because higher levels of P (price or, in this case, the wage rate) result in a higher quantity (Q) of supply: more health workers ready to offer their services or health workers willing to work more hours. The demand (D) curve slopes downward because, at higher levels of price, those that demand health workers’ services reduce the quantity they demand as the wage rate rises.
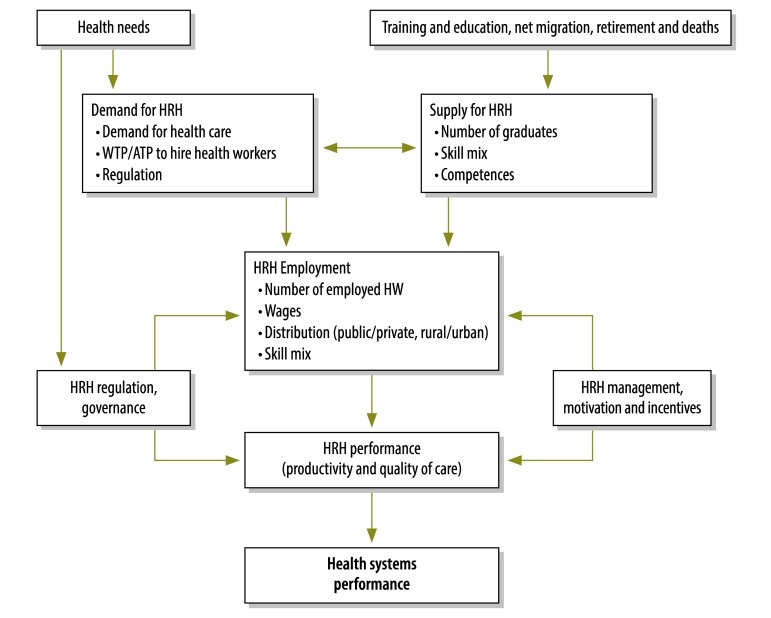
A health labour market is a dynamic system comprising two distinct but closely related economic forces: the supply of health workers and the demand for such workers, whose actions are shaped by a country’s institutions and regulations. Traditionally, analyses of human resources for health have been framed as a supply crisis, with demand-side factors receiving scant attention. The demand for health workers in a country is determined by what government, private sector and international actors, such as donors and multinational corporations, are willing to pay to hire them. “Willingness to pay” is dependent on the level of health-care financing and the willingness to hire health workers depends on the money available for doing so. “Willingness to pay” marks a distinction between demand and “need”. A mismatch commonly exists between the financial resources available – and hence, willingness to pay – for employing health workers and the number of workers needed to cover the health-care needs of the population.2 The supply of health workers is influenced by the level of remuneration and by many other factors that are economic, social, technological, legal, demographic and political. Fig. 2 illustrates the dynamics of the health labour market.
Fig. 2.
Framework for analysis of health workers labour market dynamics
ATP, ability to pay; HRH, human resources for health; HW, health workers; WTP, willingness to pay.
Source: adapted from Soucat et al.5
Markets fail to “clear” for two reasons. Either prices are not flexible (e.g. wages may be fixed by legislative or bureaucratic process or tied to civil service schedules that are insensitive to health market conditions), or demand or supply does not adjust to price signals. This may be because “demand” is predominantly defined by government and driven by legislative or bureaucratic process rather than by market forces, or because supply is regulated. An example of such regulation is offered by graduates who are “bonded” and constrained from exiting the labour market on their own volition. In health labour markets both types of rigidities are common. The market clearing position may be politically unacceptable. It may, for example, result in unaffordable health services and, in this respect, failure to “clear” may be a foreseeable result of price control. In such cases, health labour market analysis will allow a forecast of the resulting difficulty in filling available posts.
To overcome these constraints, health labour markets may require regulatory or institutional intervention to achieve socially desirable and economically efficient outcomes. Health labour markets can be regulated through a wide range of interventions: licensing professional occupations, accrediting universities and institutions that offer professional degrees, subsidizing medical education, restricting entry to the market and creating coercive measures (e.g. bonding and compulsory service) to direct health workers to rural and underserved areas.6 The selection of the appropriate balance of regulations and policies requires a solid understanding of the dynamics of the health labour market.
When conducting health labour market analysis, it is also crucial to take into account market structures – i.e. the degree of concentration on the demand and supply sides. The organization of health professionals through institutions such as labour unions or professional associations creates a degree of monopoly in the supply of health labour through collective bargaining. Medical professional associations may play a role beyond that of a union and often take on internal regulation of health workers by setting the requirements for obtaining a licence, defining minimum quality standards and determining the number of workers entering the profession.6 Restricting supply in this way results in higher wages and introduces inflexibilities in the labour market. On the demand side, where potential employers are well organized, for example, in the form of a single or dominant public sector employer, a health worker may have to accept the terms on offer or leave the sector altogether. These conditions can explain why markets fail to “clear”, as the dominant roles of unions, professional associations and public sector employers or single payer employers set conditions that are often driven by political goals rather than market conditions.
Health labour market analysis and better policies
Despite the limited number of studies on the health labour market dynamics in low- and middle-income countries, recent analyses of underlying market scenarios are beginning to reveal the importance of understanding such dynamics and of tailoring policy responses to the unique conditions of each country. To illustrate this point, we now turn to some examples of analyses that provide useful insights into the dynamics of the health labour market.
In a comparative study, Vujicic et al. (2009)7 analysed the implications of government wage bill policies in the Dominican Republic, Kenya, Rwanda and Zambia for the health workforce. All four countries were implementing general government wage bill restriction policies and the study’s purpose was to explore the effects of those policies on the strategy for maintaining or expanding the health workforce. Their research suggests that in Rwanda the health sector wage bill was maintained despite the general wage bill restriction and that the health workforce was successfully expanded in line with the country’s health strategy. In Kenya, on the other hand, the wage bill for the health sector was reduced in line with the general restrictions and this limited expansion of the workforce. In Zambia, the main obstacle to the expansion of the workforce was not deemed to be the wage bill restrictions, but the difficulties in filling budgeted posts. In the Dominican Republic, wage bill restrictions constrained growth in salaries but not in the number of health workers, which resulted in a contraction of the hours worked in the public sector and an increase in the prevalence of dual practice. Health workers responded to their reduced pay by allocating more time to other occupations. These differential responses illustrate how four countries that introduced similar wage bill policies faced different health worker responses because of their very different market situations. Supply responded flexibly to labour market conditions in the Dominican Republic and Rwanda. In the Dominican Republic, the supply of health workers fell in response to declining pay, whereas in Rwanda the supply increased in response to non-wage measures that supported expansion. Despite having a shortage of health workers relative to need, Kenya has a pool of long-term surplus in human resources for health (i.e. unemployed health professionals). The “shortage” is thus generated by inadequate demand – employment opportunities with adequate working conditions. By contrast, in Zambia the health labour market faces a long-term shortage, such that an increase in the demand for health workers did not increase employment, since there was an insufficient pool of unemployed or under-employed workers wanting to take advantage of better conditions.
Another example is that of Malawi, which faced a dire shortage, maldistribution and outmigration of health workers in the early 2000s. Malawi has subsequently succeeded in reversing a negative trend through a combination of demand- and supply-side interventions. A 50% increase in training output for priority cadres was accompanied by a 52% salary top-up to enhance deployment and retention. This led to a significant improvement in health workforce availability, as health worker density rose from 0.87 to 1.44 per 1000 population between 2004 and 2009.8
A widely promoted solution for increasing the availability of human resources for health is to expand training and increase funding for public sector employment. But this requires funds, largely from the public purse. Countries such as Ethiopia and Niger, whose macroeconomic conditions prevented them from implementing this approach, chose to invest in community-based health workers, who undergo shorter training and require less pay. In early experiences, these cadres have played a significant role in improving service coverage and health outcomes in underserved communities.9,10 Similarly, experiences in Mozambique11 and elsewhere show that mid-level cadres respond differently to health labour market conditions and are more easily retained in rural areas than physicians.
These examples highlight why it is important to understand underlying market conditions when introducing human resource policies in the health sector, as summarized below:
where constraints to supply are most important, policies such as expanding training opportunities may be appropriate;
where constraints on demand are most important, policies such as increasing the funding available for the health workforce are likely to be appropriate;
an effective strategy will more often address both supply and demand constraints simultaneously; and
in some cases, solutions may require structural changes to the labour market, such as the reorganization of the service delivery system and changes in the skills required of health workers (e.g. greater use of mid-level health workers), which in turn will change the labour market dynamics.
Knowledge and research gaps
One reason that labour market analysis has received little attention in the debate surrounding human resources for health is that data in this domain are scarce in low- and middle-income countries. Some critical areas in terms of data and research are highlighted below:
Central to any labour market analysis is an understanding of the absolute and relative levels of health worker remuneration from all sources. This is a very difficult variable to measure in the health sector and doing so requires considerable effort. Pay of health professionals, especially in low- and middle-income countries, consists of multiple components including salaries, informal payments and bonuses and allowances that can vary considerably among individual health workers. Furthermore, health professionals often hold multiple jobs or generate income outside their primary employment. Availability of more comprehensive data on their pay levels will be essential for understanding the dynamics of the health labour market.
Technological changes require transformation in the health system and are important determinants of labour market evolution, although little research is available to guide government policies and investments. One important implication for labour markets of the growth of medical technologies over the last decade is the growing demand for highly skilled workers that cost more to produce and employ.12,13
Few studies have been conducted in low- and middle-income countries to measure the “elasticity” (responsiveness) of the supply of health workers to changes in the wage rate. One study conducted in China suggests that the elasticity of supply may be considerably higher in that country than in high-income countries, and the authors conclude that increasing health worker pay may be a more cost-effective strategy to expand the health workforce than expanding training programmes.14 More empirical studies will be needed to establish whether this is equally applicable to low- and middle-income countries other than China.
Little research has been conducted on the responsiveness of health worker quality to economic variables. Among the well-known human resource problems in the health sector are low productivity, effort and morale. There is a need to evaluate the impact of changes in salaries, training availability and other working conditions on health worker performance. Some work in this area has already begun.15-18 Such studies will help to generate hypotheses about the impact of pay and institutional variables on health worker effort and will inform the effectiveness and sustainability of pay for performance and other financial and non-financial incentives to elicit more effort and greater productivity from health workers.
Health worker preferences and responses to market conditions are also beginning to attract some research in the context of health worker recruitment and retention in rural and remote areas. Discrete choice experiments have been conducted in several low- and middle-income countries to elucidate workers’ preferences in terms of job characteristics and assess their willingness to be deployed to remote and rural areas.19,20
Conclusion
We have described how labour market analysis can enhance our understanding of the factors that constrain human resources for health and result in more effective policies and interventions to address these. We have also described the health labour force analytical framework and explained that labour markets are eminently shaped by supply and demand and only indirectly by need. Although any policy conclusions derived from labour market analysis are tentative at this stage because of gaps in data and research, several country experiences point to important challenges in the health labour market and, depending on the country context, such challenges should be tackled by considering market forces from both a supply- and demand-side perspective. The identification of appropriate policy options will require further research and evaluation of effective strategies, as well as a deeper understanding of the underlying labour market conditions affecting the health worker situation in a specific country.
A better understanding of the impact of health policies on health labour markets and, subsequently, on the employment conditions of health workers would be helpful in identifying an effective strategy for the progressive attainment of universal health coverage. The human resource challenges faced by the health sector should therefore be addressed within a country’s broader development framework, where the factors affecting the dynamics of the health labour workforce – from education to regulation, incentives and the fiscal space for the wage bill – can be addressed in a holistic, integrated manner.
Acknowledgements
The authors are grateful to Christiane Wiskow (International Labour Organization) and the participants of the African Regional Workshop on Health Labour Market Analysis held in Hammamat, Tunisia, in March 2013.
Competing interests:
None declared.
References
- 1.Anand S, Bärnighausen T. Health workers at the core of the health system: framework and research issues. Health Policy. 2012;105:185–91. doi: 10.1016/j.healthpol.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Vujicic M, Zurn P. The dynamics of the health labour market. Int J Health Plann Manage. 2006;21:101–15. doi: 10.1002/hpm.834. [DOI] [PubMed] [Google Scholar]
- 3.Hongoro C, McPake B. How to bridge the gap in human resources for health. Lancet. 2004;364:1451–6. doi: 10.1016/S0140-6736(04)17229-2. [DOI] [PubMed] [Google Scholar]
- 4.Fields G, Andalón M. A toolkit for analyzing labor markets in the health care sector in Africa: health, nutrition and population, AFTHD Africa Region Washington: The World Bank; 2008. [Google Scholar]
- 5.Soucat A, Scheffler R, Ghebreyesus TA, editors. The labor market for health workers in Africa: a new look at the crisis Washington: The World Bank; 2013. [Google Scholar]
- 6.Nicholson S, Propper C. Medical workforce. In: Pauly MV, McGuire TG and Barros PP, eds. Handbook of Health Economics 2. Elsevier; 2012. pp. 873-925. [Google Scholar]
- 7.Vujicic M, Ohiri K, Sparkes S. Working in health: financing and managing the public sector health workforce Washington: The World Bank; 2009. [Google Scholar]
- 8.Management Sciences for Health. Evaluation of Malawi’s emergency human resources programme 2010. Available from: http://www.msh.org/news-bureau/msh-publishes-evaluation-of-malawi-human-resource-program.cfm [accessed 7 July 2013].
- 9.Wakabi W. Extension workers drive Ethiopia’s primary health care. Lancet. 2008;372:880. doi: 10.1016/S0140-6736(08)61381-1. [DOI] [PubMed] [Google Scholar]
- 10.Amouzou A, Habi O, Bensaïd K, Niger Countdown Case Study Working Group Reduction in child mortality in Niger: a Countdown to 2015 country case study. Lancet. 2012;380:1169–78. doi: 10.1016/S0140-6736(12)61376-2. [DOI] [PubMed] [Google Scholar]
- 11.Pereira C, Cumbi A, Malalane R, Vaz F, McCord C, Bacci A, et al. Meeting the need for emergency obstetric care in Mozambique: work performance and histories of medical doctors and assistant medical officers trained for surgery. BJOG. 2007;114:1530–3. doi: 10.1111/j.1471-0528.2007.01489.x. [DOI] [PubMed] [Google Scholar]
- 12.Denton FT, Gafni A, Spencer BG. The SHARP way to plan health care services: a description of the system and some illustrative applications in nursing human resource planning. Socioecon Plann Sci. 1995;29:125–37. doi: 10.1016/0038-0121(95)00004-6. [DOI] [Google Scholar]
- 13.Sales CS, Schlaff AL. Reforming medical education: a review and synthesis of five critiques of medical practice. Soc Sci Med. 2010;70:1665–8. doi: 10.1016/j.socscimed.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 14.Qin X, Li L, Hsieh CR. Too few doctors or too low wages? Labor supply of health care professionals in China. China Econ Rev. 2013;24:150–64. doi: 10.1016/j.chieco.2012.12.002. [DOI] [Google Scholar]
- 15.Das J, Hammer J. Money for nothing: the dire straits of medical practice in Delhi, India Washington: The World Bank; 2005 (World Bank Policy Research Working Paper 3669).
- 16.Das J, Sohnesen TP. Variations in doctor effort: evidence from Paraguay. Health Aff. 2007;26:324–37. doi: 10.1377/hlthaff.26.3.w324. [DOI] [PubMed] [Google Scholar]
- 17.Leonard KL, Masatu MC. Using the Hawthorne effect to examine the gap between a doctor's best possible practice and actual performance. J Dev Econ. 2010;93:226–34. doi: 10.1016/j.jdeveco.2009.11.001. [DOI] [Google Scholar]
- 18.Maestad O, Torsvik G, Aakvik A. Overworked? On the relationship between workload and health worker performance. J Health Econ. 2010;29:686–98. doi: 10.1016/j.jhealeco.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Ryan M, Kolstad J, Rockers P. How to conduct a discrete choice experiment for health workforce recruitment and retention in remote and rural areas: a user guide with case studies Geneva: World Health Organization; 2012. Available from: www.who.int/entity/hrh/resources/DCE_UserGuide_WEB.pdf [accessed 2 July 2013].
- 20.Araújo E, Maeda A. How to recruit and retain health workers in rural and remote areas in developing countries Washington: The World Bank (World Bank Health, Nutrition and Population Discussion Paper). Forthcoming.