Abstract
Neutrophils play an important role in periodontitis by producing nitric oxide (NO) and antimicrobial peptides, molecules with microbicidal activity via oxygen-dependent and -independent mechanisms, respectively. It is unknown whether variation in the production of antimicrobial peptides such as LL-37, human neutrophil peptides (HNP) 1-3, and NO by neutrophils influences the pathogenesis of periodontal diseases. We compared the production of these peptides and NO by lipopolysaccharide (LPS)-stimulated neutrophils isolated from healthy subjects and from patients with periodontitis. Peripheral blood neutrophils were cultured with or without Aggregatibacter actinomycetemcomitans-LPS (Aa-LPS), Porphyromonas gingivalis-LPS (Pg-LPS) and Escherichia coli-LPS (Ec-LPS). qRT-PCR was used to determine quantities of HNP 1-3 and LL-37 mRNA in neutrophils. Amounts of HNP 1-3 and LL-37 proteins in the cell culture supernatants were also determined by ELISA. In addition, NO levels in neutrophil culture supernatants were quantitated by the Griess reaction. Neutrophils from periodontitis patients cultured with Aa-LPS, Pg-LPS and Ec-LPS expressed higher HNP 1-3 mRNA than neutrophils from healthy subjects. LL-37 mRNA expression was higher in neutrophils from patients stimulated with Aa-LPS. Neutrophils from periodontitis patients produced significantly higher LL-37 protein levels than neutrophils from healthy subjects when stimulated with Pg-LPS and Ec-LPS, but no difference was observed in HNP 1-3 production. Neutrophils from periodontitis patients cultured or not with Pg-LPS and Ec-LPS produced significantly lower NO levels than neutrophils from healthy subjects. The significant differences in the production of LL-37 and NO between neutrophils from healthy and periodontitis subjects indicate that production of these molecules might influence individual susceptibility to important periodontal pathogens.
Keywords: Antimicrobial peptides, Nitric oxide, Neutrophils, Periodontitis, Innate immunity
Introduction
Periodontitis is a chronic inflammatory disease characterized by connective tissue and alveolar bone destruction, eventually leading to tooth loss. The recruitment of neutrophils and other leukocytes in the periodontal pocket is an important feature of the inflammatory process in periodontal disease (1). Important periodontopathogens, e.g., Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis, seem to induce destruction of periodontal tissues through lipopolysaccharide (LPS)-dependent mechanisms or by eliciting the production of a variety of biologically active substances by host immune cells (2). In general, LPS activates different cells, including epithelial cells, fibroblasts, neutrophils and macrophages, by activating Toll-like receptor-4 (TLR4) signaling pathways (3,4), promoting phagocytosis, production of reactive oxygen species, cytokines, and release of antimicrobial peptides from azurophil granules (5).
Neutrophils respond to bacterial products or inflammatory mediators by chemotaxis, phagocytosis, and microbial killing through oxygen radical- and non-oxygen-dependent mechanisms (6). The non-oxidative antibacterial mechanisms involve a diverse group of antimicrobial peptides including alpha-defensins (7) and human cathelicidin, LL-37 (8), which are stored in azurophil granules. The defensins are divided into alpha, beta and theta defensins and are found in vertebrates and invertebrates. Alpha-defensins include a group of six types of small peptides (7), four of which are produced by human neutrophils, thus being designated human neutrophil peptides (HNP) -1, -2, -3, and -4 (7). HNP 1-3 are the most abundant, and individual analysis of these peptides is difficult because of the high similarity of their amino acid sequences (1,9). HNP 1-3 are detected in whole saliva (10) and gingival crevicular fluid of both healthy and periodontal disease subjects (1). LL-37 is known to play an important role in the lysis of periodontal pathogens, which is consistent with the frequent development of severe periodontal diseases in subjects with Morbus Kostmann syndrome. In this congenital disease, neutrophils are deficient in LL-37, and this antimicrobial peptide is also present in abnormally low levels in saliva (11). Additionally, neutrophils from these subjects produce reduced amounts of HNP 1-3 (8). LL-37 impairs the in vitro growth of several bacterial species of the oral cavity, including the periodontal pathogens A. actinomycetemcomitans (12), Fusobacterium nucleatum and Prevotella intermedia (13). Additionally, LL-37 shows high affinity for LPS from different bacteria and thus can neutralize these endotoxins (14).
Defensins and LL-37 have the ability to kill and/or inactivate several bacterial species (including A. actinomycetemcomitans and P. gingivalis) (12), fungi, and some enveloped viruses (15). These microbicidal properties lie in the ability of these peptides to form pores in the membranes, promoting bacterial lysis or affecting viral envelopes (16). In addition, HNP 1-3 and LL-37 induce and/or amplify subsequent innate and adaptive immune responses against pathogens, such as mast cell degranulation, production of interleukins (IL) such as IL-10 and tumor necrosis factor, and dendritic cell activation (17,18). The production of nitric oxide (NO) represents another mechanism of pathogen destruction in activated neutrophils (19). Production of NO or expression of inducible NO synthase (iNOS) by peripheral neutrophils or in gingival tissues was associated with periodontal disease in human and animal models, respectively (20,21). Other studies have shown that production of NO and reactive oxygen species is enhanced by peripheral neutrophils stimulated in vitro with A. actinomycetemcomitans and P. gingivalis (22,23). Despite the massive presence of neutrophils and their enhanced activity at sites of periodontal disease (24), the roles of these leukocytes and their antimicrobial products in the susceptibility and/or pathogenesis of periodontal disease remain to be examined. Although neutrophils have been considered to be responsible for the destruction of periodontal tissues (24), some studies have suggested that neutrophils play protective roles in controlling pathogenic bacteria involved in periodontal disease (25,26).
In the present study, we investigated the expression of genes encoding HNP 1-3, LL-37, NO, and HNP 1-3/LL-37 production in neutrophils isolated from generally healthy subjects with and without periodontitis, in response to bacterial LPS from species considered or not to be periodontal pathogens.
Subjects and Methods
Subjects
All subjects enrolled in this study were clinically and radiographically examined at the Graduate Clinic of the Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas (UNICAMP), Brazil. Periodontal examination included full-mouth probing depth, plaque index, gingival index, and gingival recession. Inclusion criteria were: subjects diagnosed with generalized moderate chronic periodontitis (at least 4 teeth with probing depth ≥5 mm) who had not received periodontal treatment and/or antibiotics in the last 6 months preceding the study, with at least 14 natural teeth. Exclusion criteria were: systemic modifying factors affecting the immune response, such as diabetes mellitus, immune and hormone disorders, smokers and former smokers, alcoholics and former alcoholics, pregnant and lactating women, and those taking oral contraceptive drugs.
The subjects were separated into two experimental groups. The chronic periodontitis group included 6 patients, 3 males and 3 females (mean age: 47.5 ± 11.8 years) with moderate chronic periodontitis according to the criteria proposed by the 1999 International Workshop for a Classification of Periodontal Diseases and conditions (27). The healthy control group included 6 subjects, three males and three females (mean age: 31.4 ± 3.4 years). All subjects were clinically healthy (probing depth <3 mm, without bleeding on probing, with no detectable radiographic alveolar bone loss on radiography). All procedures performed were approved by the Ethics Committee of Faculdade de Odontologia de Piracicaba, UNICAMP, and all volunteers involved in this study signed a consent form.
Bacterial strains, growth conditions and antigens
Periodontopathogens A. actinomycetemcomitans strain Y4 and P. gingivalis strain ATCC 33277 were obtained from the Bacterial Collection of the Research Group in Oral Biology (GREB), School of Dentistry, Laval University, Quebec, Canada. These microorganisms were cultured at 37°C in brain heart agar (Difco Co., USA) supplemented with 7% defibrinated sheep blood, 5 mg/mL hemin and 1 mg/mL menadione (Sigma, USA) under anaerobic conditions (10% CO2, 10% H2 and 80% N2) in a Mini MACS Anaerobic Workstation (Don Whitley Scientific, UK) (28).
Purification of LPS from A. actinomycetemcomitans and P. gingivalis was performed as described (29). LPS samples were freeze-dried and stored at -20°C. Protein contamination of these samples was lower than 0.001% in all preparations, as evaluated using a Quick Start™ Bradford protein assay with bovine serum albumin standard (Bio-Rad Laboratories, Canada). Escherichia coli-LPS (Ec-LPS) obtained from Sigma was used as positive control.
Isolation and in vitro stimulation of human neutrophils
Whole blood (20 mL) from control and periodontitis subjects was collected into lithium heparin tubes (BD Vacutainer™, USA). Neutrophils purified from 5 mL Histopaque 1119 (Sigma-Aldrich Brazil Ltda., Brazil) were poured into a 15-mL round bottom tube and overlaid with 3 mL Histopaque 1083 (Sigma-Aldrich Brazil Ltda.), and 6 mL whole blood was layered over the gradients. Tubes containing gradients and blood were centrifuged at 460 g for 28 min at 25°C. The layer containing the neutrophils was aspirated and washed twice with cold RPMI 1640 (Invitrogen™, Brazil), supplemented with 10% fetal bovine serum and antibiotics. The erythrocytes were eliminated by hypotonic lysis for 30 s. The viability of blood neutrophils was determined by Trypan blue exclusion using a Neubauer chamber. One x 107 cells/well were incubated at 37°C in the presence of 5% CO2 for 1 h. Neutrophils were then stimulated with 100 ng/mL of A. actinomycetemcomitans-LPS (Aa-LPS), P. gingivalis-LPS (Pg-LPS) or Ec-LPS. In order to examine the effects of LPS on gene expression and production of HNP 1-3 or LL-37 by neutrophils, the cells isolated from blood were stimulated with LPS for 6 and 12 h. Neutrophils from similar cultures not exposed to LPS were used as negative controls. After incubation, cells were centrifuged (290 g, at 4°C for 10 min), and the culture supernatants were stored at -70°C until use for the determination of HNP 1-3 and LL-37 production. The neutrophils were used for the total mRNA extraction for the analysis of HNP 1-3 and LL-37 gene expression.
RNA extraction and reverse transcription
Neutrophils from cultures exposed or not to LPS were washed twice with PBS and the total RNA was immediately extracted using Trizol reagent (Invitrogen, USA), according to manufacturer instructions. After treatment of RNA samples with DNase (Turbo DNA-free, Ambion Inc., USA), a total of 0.5 µg RNA was used for cDNA synthesis. Reverse transcription was carried out using the Transcriptor First-Strand cDNA Synthesis kit (Roche Diagnostic Co., USA) according to manufacturer instructions.
Quantitative real-time polymerase chain reaction (qRT-PCR)
The levels of HPN 1 and HPN 3 transcripts were assessed using a primer set specific for a conserved sequence of these peptides (30). Table 1 shows the primer sequences applied in qRT-PCR for HPN 1-3 and LL-37.
Table 1. Primer sequences for the genes, amplification profile, and amplicon length studied here.
| Gene | Sequence (5′-3′) | Amplification profile (temperature (°C)/time (s) | Amplification (bp) |
|---|---|---|---|
| GAPDH | GAAGGTGAAGGTCGGAGTC | 95/0; 51/2; 72/9 | 226 |
| GAAGATGGTGATGGGATTTC | |||
| HNP 1-3 | TGCATGGGACGAAAGCTTG | 95/10; 55/3; 72/6 | 52 |
| CATGTTTTTCCTTGAGCCTGG | |||
| LL-37 | GCTAACCTCTACCGACTCCT | 95/10; 59/4; 72/5 | 131 |
| TCCTCTGGTGACTGCTGGT |
The sequences of the primers for qRT-PCR analysis were obtained using the Light-Cycler software (Roche Diagnostics GmbH, Germany). The qRT-PCR assays were performed using the Light Cycler system (Roche Diagnostics GmbH). The reaction mixture (15 µL) included template cDNA (0.5 µg), 0.75 µM of each primer, and 1X SYBR-Green mix (Fast Start DNA Master plus, Roche Diagnostic Co.). The thermal cycling conditions were: 95°C for 10 min for the initial denaturation, followed by 40 cycles of three steps consisting of denaturation at 95°C for 10 s, primer annealing at 59°C for 4 s, and primer extension at 72°C for 5 s. Controls included reaction mixtures without template cDNA. The housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH), was amplified in parallel to the gene of interest. Relative copy numbers compared with GAPDH were calculated using 2ΔCt. Assays with RNA samples were performed in triplicate.
Enzyme-linked immunosorbent assay (ELISA)
The amounts of HNP 1-3 and LL-37 produced by neutrophils exposed or not to LPS samples were quantified by ELISA using kits from Hycult Biotechnology (The Netherlands), according to manufacturer instructions. Individual quantification of each HNP subtype (1, 2, and 3) is not possible because of the high structural similarity of these defensins. The concentrations of HNP 1-3 and LL-37 in culture fluids are reported as pg/mL and ng/mL, respectively. Assays were performed in triplicate with the supernatants of neutrophil culture.
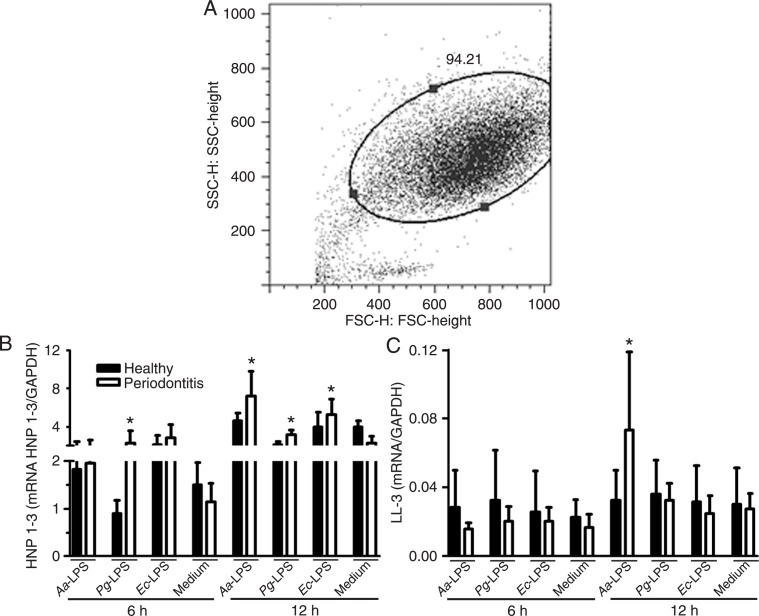
Flow cytometry analysis
Cell acquisition was performed with a FACSort flow cytometer using the CellQuest software (BD Biosciences, USA). The absolute leukocyte values/20 mL peripheral blood were calculated according to characteristics of granularity and size (side scatter vs forward scatter) based on the percentage obtained by FACS (50,000 events), and the amount of cells was determined in a Neubauer chamber.
Nitric oxide production
Nitrate was reduced to nitrite with nitrate reductase and the concentration of nitrite was determined by mixing culture supernatants of neutrophils exposed or not to LPS with Griess reagent, as described below. Briefly, neutrophils (1 × 107 cells/mL) from subjects with periodontal disease or healthy ones were cultured in the presence or absence of Aa-LPS, Pg-LPS or Ec-LPS (100 ng/mL) for 6 and 12 h, at 37°C and in the presence of 5% CO2. A total of 50 µL culture supernatant was then incubated at room temperature with an equal volume of the Griess reagent on 96-well plates (Corning, USA) for 30 min. The absorbance (A540 nm) of the samples was measured using a plate scanner (VersaMax Tunable Microplate Reader; Molecular Devices, USA). The amounts of NO2 in the samples were then calculated using a standard curve of NaNO2 (1-200 µM) within a linear range. Assays were performed in triplicate with supernatants of neutrophil cultures from each subject.
Statistical analysis and software
The Student t-test was used to determine the statistical significance of the differences observed between the volunteers with and without periodontitis and periodontally healthy volunteers. The statistical analyses were performed with the help of the GRAPHPAD PRISM software version 5.00 for Windows (http://www.graphpad.com). Differences were considered to be statistically significant at P values of <0.05.
Results
Expression of HNP 1-3 and LL-37 in peripheral blood neutrophils
The purity of cells isolated from peripheral blood of patients with periodontitis and healthy subjects was assessed by flow cytometry (Figure 1A). Approximately 94% total gated cells were polymorphonuclear neutrophils, thus ensuring a minimum influence of cell contaminants in the experiments performed. Subsequently, it was verified that Aa-LPS, Pg-LPS and Ec-LPS could induce different levels of HNP 1-3 and LL-37 mRNA in neutrophils from patients and healthy subjects. According to our data, neutrophils from patients with periodontitis express higher amounts of mRNA corresponding to HNP 1-3 than control cells after Pg-LPS stimuli for 6 and 12 h (Figure 1B). Similarly, Aa-LPS and Ec-LPS induced high levels of HNP 1-3 transcripts in neutrophils from periodontitis patients compared to neutrophils from control subjects after 12 h of incubation (Figure 1B). However, no significant difference was observed in the levels of HNP 1-3 transcripts between neutrophils from the two groups that were cultured with Aa-LPS for a shorter period of time (6 h). No significant differences in HNP 1-3 transcripts were detected between neutrophils from the periodontitis and healthy groups when cells were cultured without the LPS stimulus for 12 h (Figure 1B).
Figure 1. HNP 1-3 and LL-37 mRNA expression in peripheral neutrophils from periodontitis and healthy subjects. Neutrophils were isolated from peripheral blood and analyzed by flow cytometry, showing more than 94% purity according to side scatter (SSC) vs forward scatter (FSC) parameters (A). Neutrophils were incubated for 6 and 12 h with culture medium only or with medium containing Aa-LPS (100 ng/mL), Pg-LPS (100 ng/mL) or Ec-LPS (100 ng/mL). The relative mRNA expression of HNP 1-3 (B) and LL-37 (C) in neutrophils was assessed by qRT-PCR. Data are reported as means ± SD for N = 6 in each group. Aa-LPS = Aggregatibacter actinomycetemcomitans-lipopolysaccharide; Pg-LPS = Porphyromonas gingivalis-LPS; Ec-LPS = Escherichia coli-LPS. *P ≤ 0.05, periodontitis compared to healthy subjects (Student t-test).
The LL-37 transcript levels were closely similar for neutrophils from periodontitis patients and healthy subjects after stimulation or not with LPS for 6 and 12 h (Figure 1C). An exception were the neutrophils of periodontitis patients exposed to Aa-LPS for 12 h, which showed significantly higher levels of LL-37 transcripts compared to neutrophils from healthy controls exposed to Aa-LPS under the same conditions (Figure 1C).
Production of HNP 1-3 and LL-37 proteins by peripheral blood neutrophils
The neutrophils from healthy subjects tended to produce higher concentrations of alpha-defensin proteins than cells from periodontitis subjects, but the differences were not statistically significant (Figure 2A). Additionally, similar levels of LL-37 protein were produced by neutrophils from periodontitis and healthy subjects regardless of LPS stimulation for 6 h (Figure 2B). Neutrophils from periodontitis subjects stimulated with Pg-LPS and Ec-LPS for 12 h produced significantly higher amounts of LL-37 protein compared to neutrophils from healthy subjects similarly stimulated (Figure 2B). However, neutrophils from both groups produced similar amounts of total protein after a 12-h stimulation with Aa-LPS or without LPS exposure (Figure 2B).
Figure 2. HNP 1-3 and LL-37 production by peripheral neutrophils. Neutrophils were incubated for 6 and 12 h with culture medium only or with medium containing Aa-LPS (100 ng/mL), Pg-LPS (100 ng/mL) or Ec-LPS (100 ng/mL), and production of HNP 1-3 (A) and LL-37 (B) was determined by ELISA. Data are reported as means ± SD for N = 6 in each group. *P ≤ 0.05, periodontitis compared to healthy subjects (Student t-test). For abbreviations, see legend to Figure 1.
Differentiated production of NO by neutrophils
Neutrophils from periodontitis patients cultured with Pg-LPS or Ec-LPS for 6 h or cultured without LPS stimulation produced significantly lower levels of NO levels when compared to neutrophils from healthy subjects (Figure 3). After 12 h of incubation, NO production was still significantly lower in cultures of neutrophils from periodontitis patients stimulated with Pg-LPS and Ec-LPS compared to cells of control subjects. However, equivalent NO levels were produced by neutrophils isolated from periodontitis and healthy subjects stimulated with Aa-LPS for 6 and 12 h. No significant differences in the amounts of NO were observed between neutrophils from the two groups not stimulated with LPS (Figure 3).
Figure 3. NO production by neutrophils stimulated with LPS. Neutrophils isolated from peripheral blood of periodontitis and healthy subjects were cultured for 6 and 12 h in the presence and absence of Aa-LPS (100 ng/mL), Pg-LPS (100 ng/mL) and Ec-LPS (100 ng/mL). Nitric oxide (NO) concentrations were measured by the Griess reaction in the cell culture supernatant. Data are reported as means ± SD for N = 6 in each group. *P ≤ 0.05, periodontitis compared to healthy subjects (Student t-test). For abbreviations, see legend to Figure 1.
Discussion
In periodontal disease, neutrophil deficiency may be associated with the worsening of clinical symptoms of periodontitis (26). Neutrophils are also recognized as the major source of alpha-defensins (or HNP) and LL-37. In humans, these antimicrobial peptides seem to play a key role in protecting the periodontal tissues against oral bacteria (12,13). In patients with Morbus Kostmann syndrome, the treatment with granulocyte colony-stimulating factor restores neutrophils to normal blood counts and reduces recurrent infections, but does not prevent severe periodontitis (31). Peripheral neutrophils from these patients are deficient in LL-37 production and produce reduced amounts of HNP 1-3 defensins. However, whether neutrophils from periodontitis patients have atypical responses to components of periodontal pathogens (e.g., LPS) compared to periodontally healthy subjects remains to be investigated. In the present study, we show that neutrophils from subjects with periodontitis respond differently to stimuli with LPS from different bacterial sources (periodontal pathogens and E. coli) compared to neutrophils from healthy subjects, expressing significantly higher levels of HNP 1-3 and LL-37 genes and showing reduced amounts of NO.
Although the number of subjects with periodontitis studied was relatively small, given the complex nature of chronic periodontitis, the data presented here open a new line of investigation about the influence of neutrophil phenotypes on the course of periodontal diseases. Previous studies using a similar number of patients with aggressive and chronic periodontitis (6 and 12 subjects, respectively) were able to detect significant differences in neutrophil phagocytosis and killing of A. actinomycetemcomitans and P. gingivalis when compared to neutrophils from healthy subjects (20). In addition, the profiles of transcription and protein production of LL-37 were previously determined in gingival tissues of the same number of volunteers with chronic periodontitis (32). Further studies will be necessary to compare the phenotypes of peripheral and periodontal neutrophils between subjects with and without periodontal diseases.
It is known that the amounts of mRNA from peripheral blood neutrophils can be consistently quantified by molecular biology methods (33). We measured the amounts of HNP 1-3 and LL-37 transcripts in neutrophils from blood samples exposed to different types of LPS. We observed that neutrophils harvested from peripheral blood of periodontitis patients expressed higher HNP 1-3 mRNA levels when stimulated with Aa-LPS, Pg-LPS and Ec-LPS, specifically during 12 h of exposure. However, the protein levels of HNP 1-3 produced did not vary significantly between neutrophils from healthy versus periodontitis subjects. In a previous study, the amounts of HNP 1-3 were determined in the gingival crevice fluid of sites affected or not by periodontitis from periodontally healthy subjects or subjects with periodontitis using mass-spectrometry analysis (1). The authors demonstrated no significant differences in the amounts of these peptides detected between healthy and diseased sites, although these defensins seem to be more abundant in healthy gingival crevicular fluid (1). In another study, no association was observed between HNP 1-3 levels in gingival fluid and periodontal status (34). On the other hand, low levels of HNP 1-3 in neutrophils from Morbus Kostmann syndrome patients were associated with the development of chronic periodontal disease in these patients (11). The discrepancies between these studies might be due to different models used to obtain clinical samples and protein quantification. It has been recognized that periodontal infections elicit systemic inflammatory responses likely due to transient bacteremias from periodontitis-affected sites (35). These events may ultimately influence peripheral neutrophil concentration and activation (35). The present study shows that circulating neutrophils from periodontitis-affected subjects are more responsive to LPS, expressing higher levels of antimicrobial peptides compared to neutrophils from periodontally healthy subjects. Although no significant differences were observed in the amounts of HNP 1-3 in the supernatants of neutrophil cultures between these two groups, it is possible that alpha-defensin produced after LPS stimulation remained stored in neutrophil azurophil granules, which contain up to 50% HNP 1-3 (1,36).
To our knowledge, there are no published studies that correlate the cellular expression and release of antimicrobial peptides in neutrophil culture supernatants. Furthermore, no correlation between levels of transcripts and antimicrobial peptides released by neutrophils may be expected, since these cells even at rest have significant amounts of preformed antimicrobial peptides in cytosolic granules. Thus, newly activated neutrophils can secrete LL-37 and HNP 1-3 without de novo synthesis of these peptides. Further studies will be necessary to characterize the contents of azurophilic and specific granules of peripheral neutrophils from subjects with periodontitis. High LL-37 expression and production was previously reported for local neutrophils from gingival tissues of periodontitis patients, as evaluated by qRT-PCR and immunohistochemistry (34,37), as also observed in our study. Concentrations of LL-37 in gingival tissue homogenates were also positively correlated with the depth of the gingival pockets (37). LL-37 has variable bactericidal activity against diverse bacterial species such as A. actinomycetemcomitans, P. gingivalis, F. nucleatum, Streptococcus sobrinus, and Streptococcus mutans (13).
There is evidence that LPS from different bacterial species differs regarding the ability to activate TLR. P. gingivalis expresses a heterogeneous mixture of lipid A species that can induce cell activation through TLR2 or TLR4, while Aa-LPS and Ec-LPS interact with TLR4 only (5,38). The heterogeneity that characterizes P. gingivalis lipid A moieties is environmentally regulated and the resulting changes in Pg-LPS structure may determine the type of host response (8). Differences in biological activity of lipid A from various organisms have been recognized (39). However, the key structural differences between E. coli lipid A and P. gingivalis lipid A that account for the differences in activity have not been defined (39). In the present study, we observed some differences in neutrophil stimulation between different bacterial sources of LPS, i.e., Aa-LPS vs Pg/Ec-LPS. However, the biological basis of these differences remains to be elucidated, since there is no information regarding specific structural traits of Aa-LPS compared to Pg-LPS and Ec-LPS. The similar effects of Pg-LPS and Ec-LPS further suggest that the phenotypic changes induced in neutrophils by these two types of LPS might involve a common signal pathway of neutrophil activation. Besides differences in LPS structures, neutrophil responses to these components might be a result of a complex variation in the array of TLR/ligand complexes.
In addition to the antimicrobial peptides, neutrophils also apply oxygen-dependent microbicidal mechanisms, with the NO production during pathogen phagocytosis being one of the most studied (19). Periodontopathogenic bacteria such as A. actinomycetemcomitans, P. gingivalis and F. nucleatum are able to induce iNOS enzyme activation, resulting in high NO production in gingival tissues and blood of healthy subjects (22,23). Corroborating these data, we showed that neutrophils from healthy subjects were able to produce elevated quantities of this toxic radical after Pg-LPS and Ec-LPS stimulation. In contrast, low NO levels were produced by neutrophils from chronic periodontitis patients cultured in the presence of Pg-LPS and Ec-LPS or in the absence of LPS stimuli. These results contrast with previous studies in that NO production was enhanced in peripheral neutrophils from chronic periodontitis subjects after exposure of these cells with opsonized bacteria by the components from the patient's own serum (20). Also, animals with experimental periodontitis expressed more iNOS in periodontal tissue than controls (21). Although the criteria for selection of subjects with or without periodontitis were similar to those adopted in other studies (20), difference in methods for NO quantification and in conditions/time used for neutrophil exposure to antigens could influence the results.
The precise role of NO during the development of inflammatory processes such as periodontitis remains unknown. We worked with the hypothesis that variation in NO production by neutrophils might influence individual susceptibility to periodontal infections, i.e., subjects with neutrophils with low NO synthesis might have increased susceptibility to periodontal disease. This hypothesis is strengthened by studies showing that iNOS inhibition or deficiency allows uncontrolled growth of diverse periodontopathogenic bacteria and periodontal disease development (21-23). However, to determine the clinical/biological relevance of the data presented here, further studies are being conducted by our research group.
This study indicates that peripheral neutrophils from subjects with chronic periodontitis differ from neutrophils from periodontally healthy subjects regarding their responses to different LPS types, which affects the expression and production of antimicrobial peptides and NO production. Low NO production by neutrophils of periodontitis patients might ultimately represent an increased susceptibility to periodontal pathogen infections.
Acknowledgments
We thank Dr. Fatiha Chandad from the Research Group in Oral Biology (GREB), School of Dentistry, Laval University, Quebec, Canada, for providing LPS purified from A. actinomycetemcomitans and P. gingivalis. We also thank Dr. Thaís Helena Gasparoto from the Faculdade de Odontologia de Bauru, USP, Bauru, SP, Brazil, and Dr. Thaisângela Lopes Rodrigues from the Faculdade de Odontologia de Piracicaba, UNICAMP, Piracicaba, SP, Brazil, for their help in setting up the assays applied in this study. Research supported by FAPESP (#2007/00219-1).
References
- 1.Lundy FT, Orr DF, Shaw C, Lamey PJ, Linden GJ. Detection of individual human neutrophil alpha-defensins (human neutrophil peptides 1, 2 and 3) in unfractionated gingival crevicular fluid - a MALDI-MS approach. Mol Immunol. 2005;42:575–579. doi: 10.1016/j.molimm.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Trevani AS, Chorny A, Salamone G, Vermeulen M, Gamberale R, Schettini J, et al. Bacterial DNA activates human neutrophils by a CpG-independent pathway. Eur J Immunol. 2003;33:3164–3174. doi: 10.1002/eji.200324334. [DOI] [PubMed] [Google Scholar]
- 3.Sosroseno W, Herminajeng E. The role of macrophages in the induction of murine immune response to Actinobacillus actinomycetemcomitans. J Med Microbiol. 2002;51:581–588. doi: 10.1099/0022-1317-51-7-581. [DOI] [PubMed] [Google Scholar]
- 4.Remer KA, Brcic M, Jungi TW. Toll-like receptor-4 is involved in eliciting an LPS-induced oxidative burst in neutrophils. Immunol Lett. 2003;85:75–80. doi: 10.1016/s0165-2478(02)00210-9. [DOI] [PubMed] [Google Scholar]
- 5.Kinane DF, Demuth DR, Gorr SU, Hajishengallis GN, Martin MH. Human variability in innate immunity. Periodontol 2000. 2007;45:14–34. doi: 10.1111/j.1600-0757.2007.00220.x. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi SD, Voyich JM, DeLeo FR. Regulation of the neutrophil-mediated inflammatory response to infection. Microbes Infect. 2003;5:1337–1344. doi: 10.1016/j.micinf.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Miles K, Clarke DJ, Lu W, Sibinska Z, Beaumont PE, Davidson DJ, et al. Dying and necrotic neutrophils are anti-inflammatory secondary to the release of alpha-defensins. J Immunol. 2009;183:2122–2132. doi: 10.4049/jimmunol.0804187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puklo M, Guentsch A, Hiemstra PS, Eick S, Potempa J. Analysis of neutrophil-derived antimicrobial peptides in gingival crevicular fluid suggests importance of cathelicidin LL-37 in the innate immune response against periodontogenic bacteria. Oral Microbiol Immunol. 2008;23:328–335. doi: 10.1111/j.1399-302X.2008.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehrer RI. Primate defensins. Nat Rev Microbiol. 2004;2:727–738. doi: 10.1038/nrmicro976. [DOI] [PubMed] [Google Scholar]
- 10.Goebel C, Mackay LG, Vickers ER, Mather LE. Determination of defensin HNP-1, HNP-2, and HNP-3 in human saliva by using LC/MS. Peptides. 2000;21:757–765. doi: 10.1016/s0196-9781(00)00205-9. [DOI] [PubMed] [Google Scholar]
- 11.Putsep K, Carlsson G, Boman HG, Andersson M. Deficiency of antibacterial peptides in patients with Morbus Kostmann: an observation study. Lancet. 2002;360:1144–1149. doi: 10.1016/S0140-6736(02)11201-3. [DOI] [PubMed] [Google Scholar]
- 12.Ji S, Hyun J, Park E, Lee BL, Kim KK, Choi Y. Susceptibility of various oral bacteria to antimicrobial peptides and to phagocytosis by neutrophils. J Periodontal Res. 2007;42:410–419. doi: 10.1111/j.1600-0765.2006.00962.x. [DOI] [PubMed] [Google Scholar]
- 13.Ouhara K, Komatsuzawa H, Yamada S, Shiba H, Fujiwara T, Ohara M, et al. Susceptibilities of periodontopathogenic and cariogenic bacteria to antibacterial peptides, {beta}-defensins and LL37, produced by human epithelial cells. J Antimicrob Chemother. 2005;55:888–896. doi: 10.1093/jac/dki103. [DOI] [PubMed] [Google Scholar]
- 14.Ciornei CD, Sigurdardottir T, Schmidtchen A, Bodelsson M. Antimicrobial and chemoattractant activity, lipopolysaccharide neutralization, cytotoxicity, and inhibition by serum of analogs of human cathelicidin LL-37. Antimicrob Agents Chemother. 2005;49:2845–2850. doi: 10.1128/AAC.49.7.2845-2850.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucchese A, Guida A, Petruzzi M, Capone G, Laino L, Serpico R. Peptides in oral diseases. Curr Pharm Des. 2012;18:782–788. doi: 10.2174/138161212799277842. [DOI] [PubMed] [Google Scholar]
- 16.Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol. 2005;3:238–250. doi: 10.1038/nrmicro1098. [DOI] [PubMed] [Google Scholar]
- 17.Fábián TK, Hermann P, Beck A, Fejérdy P, Fábián G. Salivary defense proteins: their network and role in innate and acquired oral immunity. Int J Mol Sci. 2012;13:4295–4320. doi: 10.3390/ijms13044295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi KY, Chow LN, Mookherjee N. Cationic host defence peptides: multifaceted role in immune modulation and inflammation. J Innate Immun. 2012;4:361–370. doi: 10.1159/000336630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogdan C. Nitric oxide and the immune response. Nat Immunol. 2001;2:907–916. doi: 10.1038/ni1001-907. [DOI] [PubMed] [Google Scholar]
- 20.Guentsch A, Puklo M, Preshaw PM, Glockmann E, Pfister W, Potempa J, et al. Neutrophils in chronic and aggressive periodontitis in interaction with Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. J Periodontal Res. 2009;44:368–377. doi: 10.1111/j.1600-0765.2008.01113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garlet GP, Cardoso CR, Campanelli AP, Garlet TP, Avila-Campos MJ, Cunha FQ, et al. The essential role of IFN-gamma in the control of lethal Aggregatibacter actinomycetemcomitans infection in mice. Microbes Infect. 2008;10:489–496. doi: 10.1016/j.micinf.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 22.Miyasaki KT, Wilson ME, Brunetti AJ, Genco RJ. Oxidative and nonoxidative killing of Actinobacillus actinomycetemcomitans by human neutrophils. Infect Immun. 1986;53:154–160. doi: 10.1128/iai.53.1.154-160.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alayan J, Ivanovski S, Gemmell E, Ford P, Hamlet S, Farah CS. Deficiency of iNOS contributes to Porphyromonas gingivalis-induced tissue damage. Oral Microbiol Immunol. 2006;21:360–365. doi: 10.1111/j.1399-302X.2006.00304.x. [DOI] [PubMed] [Google Scholar]
- 24.Kantarci A, Van Dyke TE. Neutrophil-mediated host response to Porphyromonas gingivalis. J Int Acad Periodontol. 2002;4:119–125. [PubMed] [Google Scholar]
- 25.Miller DR, Lamster IB, Chasens AI. Role of the polymorphonuclear leukocyte in periodontal health and disease. J Clin Periodontol. 1984;11:1–15. doi: 10.1111/j.1600-051x.1984.tb01303.x. [DOI] [PubMed] [Google Scholar]
- 26.Scott DA, Krauss J. Neutrophils in periodontal inflammation. Front Oral Biol. 2012;15:56–83. doi: 10.1159/000329672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 28.Cogo K, Calvi BM, Mariano FS, Franco GC, Goncalves RB, Groppo FC. The effects of nicotine and cotinine on Porphyromonas gingivalis colonisation of epithelial cells. Arch Oral Biol. 2009;54:1061–1067. doi: 10.1016/j.archoralbio.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Darveau RP, Hancock RE. Procedure for isolation of bacterial lipopolysaccharides from both smooth and rough Pseudomonas aeruginosa and Salmonella typhimurium strains. J Bacteriol. 1983;155:831–838. doi: 10.1128/jb.155.2.831-838.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sthoeger ZM, Bezalel S, Chapnik N, Asher I, Froy O. High alpha-defensin levels in patients with systemic lupus erythematosus. Immunology. 2009;127:116–122. doi: 10.1111/j.1365-2567.2008.02997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carlsson G, Wahlin YB, Johansson A, Olsson A, Eriksson T, Claesson R, et al. Periodontal disease in patients from the original Kostmann family with severe congenital neutropenia. J Periodontol. 2006;77:744–751. doi: 10.1902/jop.2006.050191. [DOI] [PubMed] [Google Scholar]
- 32.Turkoglu O, Kandiloglu G, Berdeli A, Emingil G, Atilla G. Antimicrobial peptide hCAP-18/LL-37 protein and mRNA expressions in different periodontal diseases. Oral Dis. 2011;17:60–67. doi: 10.1111/j.1601-0825.2010.01704.x. [DOI] [PubMed] [Google Scholar]
- 33.Jonsson S, Lundberg A, Kalvegren H, Bergstrom I, Szymanowski A, Jonasson L. Increased levels of leukocyte-derived MMP-9 in patients with stable angina pectoris. PLoS One. 2011;6:e19340. doi: 10.1371/journal.pone.0019340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turkoglu O, Emingil G, Kutukculer N, Atilla G. Evaluation of gingival crevicular fluid adrenomedullin and human neutrophil peptide 1-3 levels of patients with different periodontal diseases. J Periodontol. 2010;81:284–291. doi: 10.1902/jop.2009.090517. [DOI] [PubMed] [Google Scholar]
- 35.Loos BG. Systemic markers of inflammation in periodontitis. J Periodontol. 2005;76:2106–2115. doi: 10.1902/jop.2005.76.11-S.2106. [DOI] [PubMed] [Google Scholar]
- 36.Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol. 2003;3:710–720. doi: 10.1038/nri1180. [DOI] [PubMed] [Google Scholar]
- 37.Hosokawa I, Hosokawa Y, Komatsuzawa H, Goncalves RB, Karimbux N, Napimoga MH, et al. Innate immune peptide LL-37 displays distinct expression pattern from beta-defensins in inflamed gingival tissue. Clin Exp Immunol. 2006;146:218–225. doi: 10.1111/j.1365-2249.2006.03200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X, Zhou L, Takai H, Sasaki Y, Mezawa M, Li Z, et al. Aggregatibacter actinomycetemcomitans lipopolysaccharide regulates bone sialoprotein gene transcription. J Cell Biochem. 2012;113:2822–2834. doi: 10.1002/jcb.24157. [DOI] [PubMed] [Google Scholar]
- 39.Bainbridge BW, Coats SR, Pham TT, Reife RA, Darveau RP. Expression of a Porphyromonas gingivalis lipid A palmityla-cyltransferase in Escherichia coli yields a chimeric lipid A with altered ability to stimulate interleukin-8 secretion. Cell Microbiol. 2006;8:120–129. doi: 10.1111/j.1462-5822.2005.00605.x. [DOI] [PubMed] [Google Scholar]