Abstract
Angiotensin II (Ang II) plays an important role in cardiomyocyte hypertrophy. The combined effect of hepatocyte growth factor (HGF) and Ang II on cardiomyocytes is unknown. The present study was designed to determine the effect of HGF on cardiomyocyte hypertrophy and to explore the combined effect of HGF and Ang II on cardiomyocyte hypertrophy. Primary cardiomyocytes were isolated from neonatal rat hearts and cultured in vitro. Cells were treated with Ang II (1 µM) alone, HGF (10 ng/mL) alone, and Ang II (1 µM) plus HGF (10 ng/mL) for 24, 48, and 72 h. The amount of [3H]-leucine incorporation was then measured to evaluate protein synthesis. The mRNA levels of β-myosin heavy chain and atrial natriuretic factor were determined by real-time PCR to evaluate the presence of fetal phenotypes of gene expression. The cell size of cardiomyocytes was also studied. Ang II (1 µM) increased cardiomyocyte hypertrophy. Similar to Ang II, treatment with 1 µM HGF promoted cardiomyocyte hypertrophy. Moreover, the combination of 1 µM Ang II and 10 ng/mL HGF clearly induced a combined pro-hypertrophy effect on cardiomyocytes. The present study demonstrates for the first time a novel, combined effect of HGF and Ang II in promoting cardiomyocyte hypertrophy.
Keywords: Angiotensin II, Hepatocyte growth factor, Cardiomyocyte, Hypertrophy
Introduction
Myocardial hypertrophy is defined as a thickening of the myocardium, which results in a decrease in the size of the chamber of the heart, including the left and right ventricles, and is an important risk factor for subsequent cardiac morbidity and mortality. The pathophysiology and role of cardiomyocyte hypertrophy in heart disease have been intensively investigated; however, to date they are only partially understood. Cardiac hypertrophic growth is the primary responsive mechanism by which the heart reduces stress on the ventricular wall. Conventional views suggest that cardiomyocyte hypertrophy is a compensatory response to increased hemodynamic overload, which leads to cardiac disease. However, recent findings in genetic animal models of myocardial hypertrophy as well as human studies have revealed support for a molecular basis whereby either compensatory or maladaptive forms of hypertrophy exist, and only the latter lead to cardiac failure (1). In the case of myocardial infarction, hypertrophic responses occur in cardiomyocytes in the surviving portion of the ventricle, and ventricular dilatation follows as a result of re-organization of the myocardium, including cardiomyocytes and mesenchymal cells in combination (2,3). To execute this response, the cardiomyocytes are stimulated by neurohumoral factors and subsequent intracellular reactive cascade systems. All of these processes entail an increase in protein synthesis as well as the size and architectural rearrangement within individual cardiomyocytes.
Angiotensin II (Ang II), the central product of the renin-angiotensin system, is believed to be one of the most important regulators of the initiation of a positive feedback regulation of the cardiac hypertrophic response (4). In cultured cardiomyocytes, Ang II was shown to directly induce the gene expression of β-myosin heavy chain (β-MHC) and atrial natriuretic factor (ANF) (4) and also increase protein synthesis and protein content (5) through the activation of angiotensin receptor I. More detailed mechanisms have been described in recent years, including involvement with mitochondrial oxidative stress (6), autophagy (7,8), p70-S6 protein kinase (9), nitric oxide (10), focal adhesion kinase (11), and AMP-activated protein kinase (12,13). In fact, in addition to Ang II, large numbers of intracellular or extracellular factors affect cardiomyocyte hypertrophy in vivo (14). Moreover, the influence of these factors on Ang II-induced cardiomyocyte hypertrophy is largely unknown.
In the present study, we hypothesized that there may be crosstalk between Ang II and hepatocyte growth factor (HGF) in cardiomyocyte hypertrophy. HGF is a paracrine cellular growth, motility, and morphogenic factor. It was initially isolated from fibroblasts and was shown to stimulate the motility of epithelial cells and to have a wide range of effects on many biological processes (15). Specifically, HGF acts primarily on epithelial cells, endothelial cells, and hematopoietic progenitor cells (16). It has been shown to have a major role in embryonic organ development, adult organ regeneration, and wound healing (16). In recent years, the impact of HGF on the heart or cardiomyocytes has been gradually uncovered. HGF protects the heart from ischemic/reperfusion injury, attenuates cardiac remodeling, improves angiogenesis, and induces endothelial progenitor cell mobilization (16). In our study, we first determined the effects of a single treatment of Ang II or HGF on cardiomyocytes and then examined whether the combined treatment of Ang II and HGF differed from each factor administered individually.
Material and Methods
Animals and reagents
Newborn Sprague-Dawley rats (18-20 g) were supplied by the Animal Center of Guangzhou Medical University. Rats were housed and used in accordance with our institutional guidelines for animal care and the Guide for Animal Care of the National Institutes of Health. Dulbecco's modified Eagle's medium (DMEM), fetal bovine serum (FBS), and TRIzol were purchased from Gibco BRL (USA). Trypsin was obtained from Amersco (USA). Alpha-sarcomeric actin was purchased from Santa Cruz Biotechnology (USA). The SYBR®GreenPCR Master Mix was obtained from Applied Biosystems (USA). The Thermo ScriptRT-PCR kit was purchased from Invitrogen (USA). [3H]-leucine (Leu) was obtained from the China Institute of Atomic Energy (China) and recombinant Ang II and HGF were purchased from Sigma (Germany).
Primary cardiomyocyte culture
Rat neonatal ventricular cardiomyocytes were prepared as previously described, with some modifications (17). The cells were suspended in DMEM containing 10% FBS and 0.1 mM bromodeoxyuridine and plated on either glass coverslips or polystyrene-treated Petri dishes. The cells were cultured at 37°C in a 5% CO2 incubator for 72 h. Pulsations of the cardiomyocytes were observed with an inverted biological microscope (18). In addition, the cardiomyocytes were fixed and stained by immunohistochemical methods using an anti-α-sarcomeric actin antibody (19). The purity of the cardiomyocytes was approximately 95%.
Groups and treatments
The cardiomyocyte medium was changed to serum-free DMEM for 24 h. The cardiomyocytes were then treated with different concentrations of Ang II (0.01-10 µM) and HGF (1, 10, 100 ng/mL) for 48 h in order to explore the most appropriate concentrations of each factor.
Based on these experiments, we identified an optimal treatment regimen. Cardiomyocytes were divided into four groups: Control group (0.1 M PBS), HGF-treated group (10 ng/mL), Ang II-treated group (1 µM), and HGF (10 ng/mL) plus Ang II (1 µM)-treated group. The cells were treated with these agents for 24, 48, and 72 h.
[3H]-Leu incorporation assay
Tritiated leucine ([3H]-Leu) incorporation studies were performed as previously described (20) to investigate the effects of the treatments on total protein synthesis. Cells were seeded on 24-well plates (1 × 105 cells/well) and treated with HGF (10 ng/mL) or Ang II (1 µM) or HGF (10 ng/mL) plus Ang II (1 µM), as described in the preceding section. Cells were then pulsed with [3H]-Leu (104 Bq/mL) for 12 h before the end of the treatment. At the end of the incubation, the cells were washed three times with ice-cold PBS and then disrupted by the addition of 200 µL 0.1% sodium dodecyl sulfate and 0.1 N NaOH. The solubilized cell lysates (100 µL) were added to 5 mL scintillation fluid. The incorporation of [3H]-Leu into the protein was determined by scintillation counting. Incorporation is reported as the ratio: [3H]-Leu incorporation/number of cells.
RNA extraction and real-time PCR analysis
After the cells were treated with HGF (10 ng/mL), Ang II (1 µM), or HGF (10 ng/mL) plus Ang II (1 µM) for 12 h, they were washed with ice-cold PBS buffer. Total RNA was extracted from the cells using Trizol (21), and 1 µg RNA was reverse transcribed to cDNA using Thermo ScriptRT-PCR (22). Real-time PCR was performed using an Applied Biosystems 7500 fast real-time PCR system and SYBR Premix Ex Taq mixture with specific primers (Sangon, China) (23). The PCR assays were initiated with a denaturation step at 95°C for 10 s, followed by amplification with 40 cycles at 95°C for 10 s and annealing at 60°C for 20 s (two-step method) (24). Finally, a melting curve analysis was performed from 60° to 85°C. Data were evaluated with the Applied Biosystems software. The following primers designed with the Primer Express Software (Applied Biosystems) were used: ANF: 5′-AAA GCAAAC TGA GGGCT-3′ (sense) and 5′-GGG ATC TTT TGC GAT CT-3′ (antisense); β-MHC: 5′-TGC AGT TAA AGG TGA AGG C-3′ (sense) and 5′-CAG GGC TTC ACA GGC AT-3′ (antisense); glyceraldehyde 3-phosphate dehydrogenase (GAPDH): 5′-CGG AGT CAA CGG ATT TGG TGG TAT-3′ (sense) and 5′-AGC CTT CTC CAT GGT GGT GAA GAC-3′ (antisense). GAPDH was used as an internal control and the amount of target was defined by the 2ΔΔCt method (25).
Measurement of cell size
Cardiomyocytes were seeded on 24-well plates and cultured for 48 h. After treatment with HGF (10 ng/mL), Ang II (1 µM), or HGF (10 ng/mL) plus Ang II (1 µM) for 12 h, the cells were digested with EDTA-trypsin (0.25%) for 5 min, 10% FBS was used to terminate the reaction and the average cell size was determined using the Image J software (http://rsb.info.nih.gov/ij/download.html) as previously described (26). The average cell size was determined by observation of 150 cells (50 cells/well × 3 wells).
Statistical analysis
Data are reported as means ± SD. The differences were evaluated by a two-tailed Student t-test (2 groups) or one-way analysis of variance (ANOVA) followed by the Tukey post hoc test (3 or more groups) using the SPSS software (version 9.0, USA) (27). Statistical significance was set at P < 0.05.
Results
Effects of Ang II on [3H]-Leu incorporation and on ANF and β-MHC mRNA levels in primary cardiomyocytes
As shown in Table 1, Ang II (0.01 µM) caused a slight but significant increase in [3H]-Leu incorporation compared to control (1494.58 ± 65.00 vs 1188.83 ± 72.20 cpm/well, respectively; P < 0.05). However, at this concentration of Ang II, the mRNA levels of ANF and β-MHC in primary cardiomyocytes were not changed.
Table 1. Effects of different concentrations of Ang II on [3H]-Leu incorporation, and mRNA levels of ANF and β-MHC in primary cardiomyocytes.
| Ang II (µM) | [3H]-Leu incorporation (cpm/well) | Relative ANF mRNA | Relative β-MHC mRNA |
|---|---|---|---|
| Control | 1188.83 ± 72.20 | 1 ± 0 | 1 ± 0 |
| 0.01 | 1494.58 ± 65.00* | 1.07 ± 0.09 | 1.17 ± 0.06 |
| 0.1 | 1821.33 ± 54.65* | 1.20 ± 0.02* | 1.75 ± 0.03* |
| 1 | 2374.08 ± 49.34* | 1.44 ± 0.08* | 1.85 ± 0.13* |
| 10 | 2414.67 ± 56.70* | 1.65 ± 0.04* | 2.08 ± 0.14* |
Data reported as means ± SD for N = 6/concentration performed in triplicate. Ang II = angiotensin II; ANF = atrial natriuretic factor; β-MHC = β-myosin heavy chain.
P < 0.05 vs control (one-way ANOVA).
When Ang II was administered at a higher concentration (0.1 µM), the [3H]-Leu incorporation increased to 1820 cpm/well, which was approximately 1.5-fold higher than the control group (P < 0.01). In addition, this concentration of Ang II also significantly enhanced the mRNA levels of ANF (1.2-fold, P < 0.01) and β-MHC (1.75-fold, P < 0.01).
When the Ang II concentration was increased to 1 µM, the amount of [3H]-Leu incorporation increased approximately 2-fold compared to the control group (2374.08 ± 49.34 vs 1188.83 ± 72.20 cpm/well, respectively; P < 0.01), while the mRNA levels of ANF and β-MHC increased by 44% (P < 0.01) and 85% (P < 0.01), respectively.
The highest concentration of Ang II tested (10 µM) increased the [3H]-Leu incorporation only slightly (2414.67 ± 56.70 vs 1188.83 ± 72.20 cpm/well, respectively; P < 0.01). Moreover, at this concentration of Ang II, the mRNA levels of ANF and β-MHC only increased by 1.65-fold and 2.08-fold, respectively. Therefore, we chose 1 µM as the optimal concentration of Ang II for subsequent experiments.
Effects of HGF on [3H]-Leu incorporation and on ANF and β-MHC mRNA levels in primary cardiomyocytes
We sought to determine the effects of different concentrations of HGF on [3H]-Leu incorporation as well as on mRNA levels of ANF and β-MHC in primary cardiomyocytes. As shown in Table 2, administration of 1 ng/mL HGF significantly increased the [3H]-Leu incorporation in cardiomyocytes to 2430.47 ± 72.65 cpm/well, which was approximately 2.2-fold higher than the control group (P < 0.01). Moreover, HGF at this concentration also significantly (P < 0.01) enhanced the mRNA levels of ANF (2.33-fold) and β-MHC (2.14-fold).
Table 2. Effects of different concentrations of HGF on [3H]-Leu incorporation, and mRNA levels of ANF and β-MHC in primary cardiomyocytes.
| HGF (ng/mL) | [3H]-Leu incorporation (cpm/well) | Relative ANF mRNA | Relative β-MHC mRNA |
|---|---|---|---|
| Control | 1113.45 ± 62.58 | 1 ± 0 | 1 ± 0 |
| 1 | 2430.47 ± 72.65* | 2.33 ± 0.04* | 2.14 ± 0.03* |
| 10 | 3848 ± 71.57* | 3.32 ± 0.08* | 2.81 ± 0.07* |
| 100 | 3256 ± 68.34* | 3.01 ± 0.01* | 2.42 ± 0.06* |
Data are reported as means ± SD for N = 6/concentration performed in triplicate. HGF = hepatology growth factor; ANF = atrial natriuretic factor; β-MHC = β-myosin heavy chain.
P < 0.05 vs control (one-way ANOVA).
When the HGF concentration was increased to 10 ng/mL, the [3H]-Leu incorporation was higher compared to control (3848 ± 71.57 vs 1113.45 ± 62.58 cpm/well, respectively; P < 0.01). Moreover, the ANF and β-MHC mRNA levels were also increased (3.32- and 2.81-fold, respectively; P < 0.01). Interestingly, the highest concentration of HGF (100 ng/mL) did not further increase [3H]-Leu incorporation or ANF and β-MHC mRNA levels compared to the lower concentration of HGF (10 ng/mL). Therefore, we chose 10 ng/mL as the optimal concentration of HGF in subsequent experiments.
Effects of HGF in combination with Ang II on [3H]-Leu incorporation and on ANF and β-MHC mRNA levels in primary cardiomyocytes
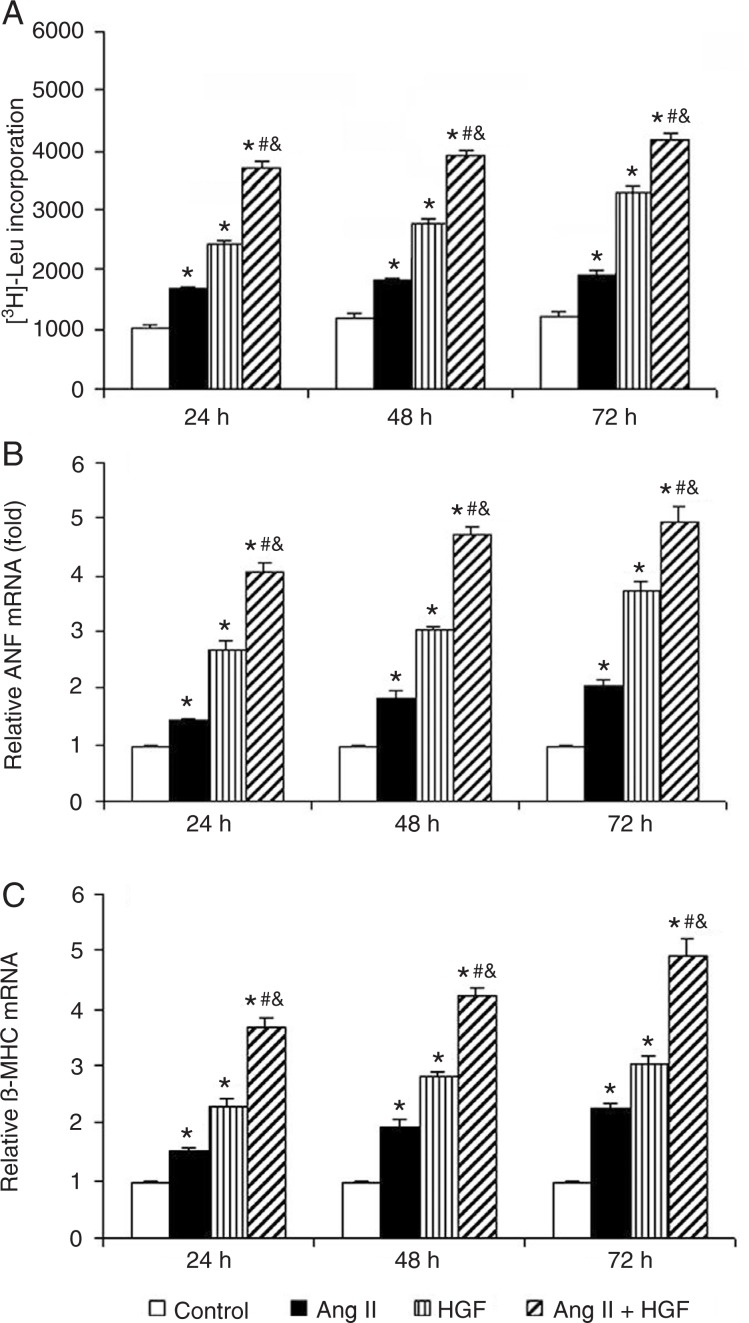
We next investigated whether HGF and Ang II had combined effects on cardiomyocytes. Ang II and HGF in combination induced a significant increase in [3H]-Leu incorporation and in ANF mRNA and β-MHC mRNA levels (Figure 1A-C). Interestingly, the HGF-induced cardiomyocyte hypertrophy was even greater than Ang II-induced hypertrophy (Figure 1A-C).
Figure 1. Effects of Ang II (1 µM), HGF (10 ng/mL), and HGF (10 ng/mL) plus Ang II (1 µM) on [3H]-Leu incorporation (A), the mRNA levels of ANF (B) and the mRNA levels of β-MHC (C) in primary cardiomyocytes. N = 8 per group. The experiments were repeated three times. HGF = hepatology growth factor; Ang II = angiotensin II; ANF = atrial natriuretic factor; β-MHC = β-myosin heavy chain. *P < 0.05 vs control; #P < 0.05 vs HGF; &P < 0.05 vs Ang II (one-way ANOVA).
Compared to the HGF (10 ng/mL) or Ang II (1 µM) groups, the combined treatment of HGF (10 ng/mL) and Ang II (1 µM) increased [3H]-Leu incorporation even further at 24, 48, and 72 h (Figure 1A; P < 0.01). Similarly, combined treatment of cardiomyocytes with HGF (10 ng/mL) and Ang II (1 µM) significantly upregulated the mRNA levels of ANF (Figure 1B) and β-MHC (Figure 1C) compared to separate treatment with HGF (10 ng/mL) or Ang II (1 µM) alone at these time points.
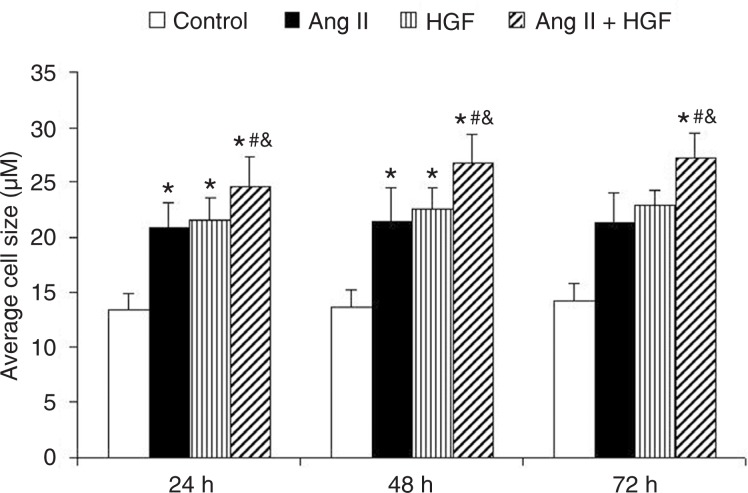
Effect of HGF and Ang II on the cell size of primary cardiomyocytes
We also determined the effect of HGF and Ang II on cardiomyocyte cell size. Compared to the control group, both the HGF (10 ng/mL)-treated group and Ang II (1 µM)-treated group showed an increase in cell size (Figure 2). The combination treatment of HGF and Ang II increased the cell size of cardiomyocytes further (Figure 2).
Figure 2. Effects of Ang II (1 µM), HGF (10 ng/mL), and HGF (10 ng/mL) plus Ang II (1 µM) on average cell size. N = 8 per group. The experiments were repeated three times. HGF = hepatology growth factor; Ang II = angiotensin II. *P < 0.05 vs control; #P < 0.05 vs HGF; &P < 0.05 vs Ang II (one-way ANOVA).
Discussion
This study was the first to directly assess whether there was a combined effect of HGF and Ang II on cardiomyocyte hypertrophy. Based on the increase in [3H]-Leu incorporation, the increased ANF and β-MHC mRNA expression and the increase in cell size in primary cardiomyocytes, we concluded that HGF and Ang II have a combined effect on neonatal cardiomyocyte hypertrophy. In addition, we also demonstrated for the first time that HGF alone can potently induce cultured neonatal cardiomyocyte hypertrophy.
In this study, we first found that HGF could induce cardiomyocyte hypertrophy. To our surprise, the HGF-induced cardiomyocyte hypertrophy was even greater than Ang II-induced hypertrophy (Figure 1A-C). The presence of the HGF receptor on cardiomyocytes was first confirmed by Akiyama et al. (28). Subsequently, several independent reports have demonstrated a protective effect of HGF on myocardial infarction in vivo (29,30). However, as yet the underlying mechanisms for the pro-hypertrophy of cardiomyocytes are not clear. Moreover, the results of in vivo experiments cannot exclude the possibility that HGF treatment stimulates cardiac fibroblasts (31) and thereby releases factors that induce hypertrophy of the surrounding cardiomyocytes. Pathological cardiomyocyte hypertrophy is characterized not only by an increase in cardiomyocyte size, but also by cardiomyocyte gene reprogramming, as shown by the enhanced expression of fetal phenotypes of genes, such as skeletal α-actin, β-MHC, and ANF (32). In our study, we evaluated cell hypertrophy by determining [3H]-Leu incorporation and the average cell size as well as ANF and β-MHC mRNA levels. Based on these various parameters, we have clearly shown that HGF can directly induce cardiomyocyte hypertrophy. It should be noted that Nakamura et al. (33) demonstrated an interference of administered HGF on cardiomyopathy remodeling in hamster hearts. The authors found a direct negative effect of HGF on the transcript levels of ANF. In the present study, we showed an inductive effect of HGF on ANF levels, in agreement with a previous report (34). We considered that this disparity might be due to the species difference.
Based on these findings, we sought to determine how this pro-hypertrophy effect of HGF may occur. Since the most common cause of cardiomyocyte hypertrophy is hypertension, and since an increased Ang II level in hypertension is a critical pro-hypertrophy trigger, we next explored whether there might be an association between HGF and Ang II in cardiomyocytes. Importantly, we found a combined effect of HGF and Ang II on cardiomyocyte hypertrophy. The roles of Ang II in the regulation of the cardiovascular system under normal and pathological conditions have been well documented, and it has been well accepted that Ang II is a direct pro-hypertrophy factor in cardiomyocytes. Moreover, there is evidence that Ang II and related proteins such as interleukin-1β and tumor necrosis factor-α, play key roles in cardiac fibroblast growth and collagen deposition following myocardial infarction (35). In addition, heparin, a highly sulfated glycosaminoglycan and widely used injectable anticoagulant, was found to potently inhibit Ang II-mediated cardiomyocyte hypertrophy (36). The interleukin-6 family of cytokines was also reported to contribute to Ang II-induced cardiomyocyte hypertrophy (37). However, to the best of our knowledge, there has been no report to date on the combined effect of Ang II and any other protein on cardiomyocyte hypertrophy. More importantly, since cardiomyocyte hypertrophy is related to the pathophysiological mechanisms of many cardiovascular diseases, our findings in this study may bring new focus on HGF in treating cardiovascular diseases.
One limitation of this study is that the molecular mechanisms underlying the combined effect of Ang II and HGF on cardiomyocyte hypertrophy remain to be elucidated. It has been reported that post-infarction HGF gene therapy resulted in substantial cardiomyocte hypertrophy at the edges of the infarcted tissue, accompanied by the overexpression of the HGF receptor (c-Met), which is a transmembrane tyrosine kinase through which HGF activates the Ras-Raf-MEK-ERK signaling pathway, thereby contributing to myocardial hypertrophy (38). The c-Met is also a receptor for the scatter factor (SF) (39). The activation of c-Met by HGF/SF can elicit a variety of cellular responses including proliferation, migration, invasion, and branching morphogenesis. These processes are associated with several signaling pathways such as PI3K/Akt, Src, and STAT3 (39). Moreover, these signaling pathways also contribute to Ang II-induced hypertrophy. Aoki et al. (40) have shown that the ERK pathway has an important role in Ang II-induced cardiac hypertrophy. Moreover, the PI3K/Akt, Src, and STAT3 pathways have also been reported to be vital controllers in Ang II-induced cardiac hypertrophy. Therefore, it may be difficult to determine the exact underlying molecular mechanisms of the combined effect of HGF and Ang II on cardiomyocyte hypertrophy. The convergence point between HGF and Ang II needs to be further elucidated in future experiments.
Our study has provided the first evidence that HGF and Ang II administered in combination induce cardiomyocyte hypertrophy. This finding was supported by the changes observed in protein synthesis, the presence of fetal phenotypes of gene expression (ANF and β-MHC), an increase in cell size, and ultrastructural changes of neonatal cardiomyocytes. These results may help to improve the management and treatment of patients with cardiac hypertrophy.
Acknowledgments
Research supported by the National Natural Science Foundation of China (Grant #30570759), the Natural Science Foundation of Guangdong Province, China (#S201101004269) and the Foundation of Guangzhou Municipal Health Bureau Scientific Research and Education Managment System (#201102A213125).
References
- 1.Lips DJ, deWindt LJ, van Kraaij DJ, Doevendans PA. Molecular determinants of myocardial hypertrophy and failure: alternative pathways for beneficial and maladaptive hypertrophy. Eur Heart J. 2003;24:883–896. doi: 10.1016/s0195-668x(02)00829-1. [DOI] [PubMed] [Google Scholar]
- 2.Li Q, Li B, Wang X, Leri A, Jana KP, Liu Y, et al. Overexpression of insulin-like growth factor-1 in mice protects from myocyte death after infarction, attenuating ventricular dilation, wall stress, and cardiac hypertrophy. J Clin Invest. 1997;100:1991–1999. doi: 10.1172/JCI119730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, et al. Bone marrow cells regenerate infarcted myocardium. Nature. 2001;410:701–705. doi: 10.1038/35070587. [DOI] [PubMed] [Google Scholar]
- 4.Sadoshima J, Izumo S. Molecular characterization of angiotensin II-induced hypertrophy of cardiac myocytes and hyperplasia of cardiac fibroblasts. Critical role of the AT1 receptor subtype. Circ Res. 1993;73:413–423. doi: 10.1161/01.res.73.3.413. [DOI] [PubMed] [Google Scholar]
- 5.Wada H, Zile MR, Ivester CT, Cooper G, McDermott PJ. Comparative effects of contraction and angiotensin II on growth of adult feline cardiocytes in primary culture. Am J Physiol. 1996;271:H29–H37. doi: 10.1152/ajpheart.1996.271.1.H29. [DOI] [PubMed] [Google Scholar]
- 6.Dai DF, Rabinovitch P. Mitochondrial oxidative stress mediates induction of autophagy and hypertrophy in angiotensin-II treated mouse hearts. Autophagy. 2011;7:917–918. doi: 10.4161/auto.7.8.15813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gottlieb RA, Mentzer RM, Jr, Linton PJ. Impaired mitophagy at the heart of injury. Autophagy. 2011;7:1573–1574. doi: 10.4161/auto.7.12.18175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zois CE, Giatromanolaki A, Sivridis E, Papaiakovou M, Kainulainen H, Koukourakis MI. “Autophagic flux” in normal mouse tissues: focus on endogenous LC3A processing. Autophagy. 2011;7:1371–1378. doi: 10.4161/auto.7.11.16664. [DOI] [PubMed] [Google Scholar]
- 9.Jonassen AK, Sack MN, Mjos OD, Yellon DM. Myocardial protection by insulin at reperfusion requires early administration and is mediated via Akt and p70s6 kinase cell-survival signaling. Circ Res. 2001;89:1191–1198. doi: 10.1161/hh2401.101385. [DOI] [PubMed] [Google Scholar]
- 10.Landmesser U, Engberding N, Bahlmann FH, Schaefer A, Wiencke A, Heineke A, et al. Statin-induced improvement of endothelial progenitor cell mobilization, myocardial neovascularization, left ventricular function, and survival after experimental myocardial infarction requires endothelial nitric oxide synthase. Circulation. 2004;110:1933–1939. doi: 10.1161/01.CIR.0000143232.67642.7A. [DOI] [PubMed] [Google Scholar]
- 11.Taylor JM, Rovin JD, Parsons JT. A role for focal adhesion kinase in phenylephrine-induced hypertrophy of rat ventricular cardiomyocytes. J Biol Chem. 2000;275:19250–19257. doi: 10.1074/jbc.M909099199. [DOI] [PubMed] [Google Scholar]
- 12.Timmers L, Sluijter JP, Verlaan CW, Steendijk P, Cramer MJ, Emons M, et al. Cyclooxygenase-2 inhibition increases mortality, enhances left ventricular remodeling, and impairs systolic function after myocardial infarction in the pig. Circulation. 2007;115:326–332. doi: 10.1161/CIRCULATIONAHA.106.647230. [DOI] [PubMed] [Google Scholar]
- 13.Xie Z, He C, Zou MH. AMP-activated protein kinase modulates cardiac autophagy in diabetic cardiomyopathy. Autophagy. 2011;7:1254–1255. doi: 10.4161/auto.7.10.16740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rohini A, Agrawal N, Koyani CN, Singh R. Molecular targets and regulators of cardiac hypertrophy. Pharmacol Res. 2010;61:269–280. doi: 10.1016/j.phrs.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Funakoshi H, Nakamura T. Hepatocyte growth factor: from diagnosis to clinical applications. Clin Chim Acta. 2003;327:1–23. doi: 10.1016/s0009-8981(02)00302-9. [DOI] [PubMed] [Google Scholar]
- 16.Morishita R, Aoki M, Yo Y, Ogihara T. Hepatocyte growth factor as cardiovascular hormone: role of HGF in the pathogenesis of cardiovascular disease. Endocr J. 2002;49:273–284. doi: 10.1507/endocrj.49.273. [DOI] [PubMed] [Google Scholar]
- 17.Simpson P, McGrath A, Savion S. Myocyte hypertrophy in neonatal rat heart cultures and its regulation by serum and by catecholamines. Circ Res. 1982;51:787–801. doi: 10.1161/01.res.51.6.787. [DOI] [PubMed] [Google Scholar]
- 18.Mellor KM, Reichelt ME, Delbridge LM. Autophagy anomalies in the diabetic myocardium. Autophagy. 2011;7:1263–1267. doi: 10.4161/auto.7.10.17148. [DOI] [PubMed] [Google Scholar]
- 19.Przyklenk K, Undyala VV, Wider J, Sala-Mercado JA, Gottlieb RA, Mentzer RM., Jr Acute induction of autophagy as a novel strategy for cardioprotection: getting to the heart of the matter. Autophagy. 2011;7:432–433. doi: 10.4161/auto.7.4.14395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Z, Li J, Jiang Z, Qi Y, Tang C, Du J. Effects of ad-renomedullin, C-type natriuretic peptide, and parathyroid hormone-related peptide on calcification in cultured rat vascular smooth muscle cells. J Cardiovasc Pharmacol. 2003;42:89–97. doi: 10.1097/00005344-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Dong LW, Hou YJ, Tan YX, Tang L, Pan YF, Wang M, et al. Prognostic significance of Beclin 1 in intrahepatic cholangio-cellular carcinoma. Autophagy. 2011;7:1222–1229. doi: 10.4161/auto.7.10.16610. [DOI] [PubMed] [Google Scholar]
- 22.Cottam EM, Maier HJ, Manifava M, Vaux LC, Chandra-Schoenfelder P, Gerner W, et al. Coronavirus nsp6 proteins generate autophagosomes from the endoplasmic reticulum via an omegasome intermediate. Autophagy. 2011;7:1335–1347. doi: 10.4161/auto.7.11.16642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang P, Xu TY, Guan YF, Su DF, Fan GR, Miao CY. Perivascular adipose tissue-derived visfatin is a vascular smooth muscle cell growth factor: role of nicotinamide mononucleotide. Cardiovasc Res. 2009;81:370–380. doi: 10.1093/cvr/cvn288. [DOI] [PubMed] [Google Scholar]
- 24.Wang P, Zhang RY, Song J, Guan YF, Xu TY, Du H, et al. Loss of AMP-activated protein kinase-alpha2 impairs the insulin-sensitizing effect of calorie restriction in skeletal muscle. Diabetes. 2012;61:1051–1061. doi: 10.2337/db11-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang J, Zhao Y, Ma K, Jiang FJ, Liao W, Zhang P, et al. Deficiency of hepatocystin induces autophagy through an mTOR-dependent pathway. Autophagy. 2011;7:748–759. doi: 10.4161/auto.7.7.15822. [DOI] [PubMed] [Google Scholar]
- 26.Wang P, Xu TY, Guan YF, Tian WW, Viollet B, Rui YC, et al. Nicotinamide phosphoribosyltransferase protects against ischemic stroke through SIRT1-dependent adenosine monophosphate-activated kinase pathway. Ann Neurol. 2011;69:360–374. doi: 10.1002/ana.22236. [DOI] [PubMed] [Google Scholar]
- 27.Trocoli A, Mathieu J, Priault M, Reiffers J, Souquere S, Pierron G, et al. ATRA-induced upregulation of Beclin 1 prolongs the life span of differentiated acute promyelocytic leukemia cells. Autophagy. 2011;7:1108–1114. doi: 10.4161/auto.7.10.16623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akiyama Y, Ashizawa N, Seto S, Ohtsuru A, Kuroda H, Ito M, et al. Involvement of receptor-type tyrosine kinase gene families in cardiac hypertrophy. J Hypertens. 1999;17:1329–1337. doi: 10.1097/00004872-199917090-00014. [DOI] [PubMed] [Google Scholar]
- 29.Ueda H, Nakamura T, Matsumoto K, Sawa Y, Matsuda H, Nakamura T. A potential cardioprotective role of hepatocyte growth factor in myocardial infarction in rats. Cardiovasc Res. 2001;51:41–50. doi: 10.1016/s0008-6363(01)00272-3. [DOI] [PubMed] [Google Scholar]
- 30.Jin H, Yang R, Li W, Ogasawara AK, Schwall R, Eberhard DA, et al. Early treatment with hepatocyte growth factor improves cardiac function in experimental heart failure induced by myocardial infarction. J Pharmacol Exp Ther. 2003;304:654–660. doi: 10.1124/jpet.102.041772. [DOI] [PubMed] [Google Scholar]
- 31.Taniyama Y, Morishita R, Nakagami H, Moriguchi A, Sakonjo H, Shokei K, et al. Potential contribution of a novel antifibrotic factor, hepatocyte growth factor, to prevention of myocardial fibrosis by angiotensin II blockade in cardiomyopathic hamsters. Circulation. 2000;102:246–252. doi: 10.1161/01.cir.102.2.246. [DOI] [PubMed] [Google Scholar]
- 32.Kim S, Iwao H. Molecular and cellular mechanisms of angiotensin II-mediated cardiovascular and renal diseases. Pharmacol Rev. 2000;52:11–34. [PubMed] [Google Scholar]
- 33.Nakamura T, Matsumoto K, Mizuno S, Sawa Y, Matsuda H, Nakamura T. Hepatocyte growth factor prevents tissue fibrosis, remodeling, and dysfunction in cardiomyopathic hamster hearts. Am J Physiol Heart Circ Physiol. 2005;288:H2131–H2139. doi: 10.1152/ajpheart.01239.2003. [DOI] [PubMed] [Google Scholar]
- 34.Roggia C, Ukena C, Bohm M, Kilter H. Hepatocyte growth factor (HGF) enhances cardiac commitment of differentiating embryonic stem cells by activating PI3 kinase. Exp Cell Res. 2007;313:921–930. doi: 10.1016/j.yexcr.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Ho CY. Hypertrophic cardiomyopathy. Heart Fail Clin. 2010;6:141–159. doi: 10.1016/j.hfc.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akimoto H, Ito H, Tanaka M, Adachi S, Hata M, Lin M, et al. Heparin and heparan sulfate block angiotensin II-induced hypertrophy in cultured neonatal rat cardiomyocytes. A possible role of intrinsic heparin-like molecules in regulation of cardiomyocyte hypertrophy. Circulation. 1996;93:810–816. doi: 10.1161/01.cir.93.4.810. [DOI] [PubMed] [Google Scholar]
- 37.Sano M, Fukuda K, Kodama H, Pan J, Saito M, Matsuzaki J, et al. Interleukin-6 family of cytokines mediate angiotensin II-induced cardiac hypertrophy in rodent cardiomyocytes. J Biol Chem. 2000;275:29717–29723. doi: 10.1074/jbc.M003128200. [DOI] [PubMed] [Google Scholar]
- 38.Li Y, Takemura G, Kosai K, Yuge K, Nagano S, Esaki M, et al. Postinfarction treatment with an adenoviral vector expressing hepatocyte growth factor relieves chronic left ventricular remodeling and dysfunction in mice. Circulation. 2003;107:2499–2506. doi: 10.1161/01.CIR.0000065579.19126.B8. [DOI] [PubMed] [Google Scholar]
- 39.Gao CF, Vande Woude GF. HGF/SF-Met signaling in tumor progression. Cell Res. 2005;15:49–51. doi: 10.1038/sj.cr.7290264. [DOI] [PubMed] [Google Scholar]
- 40.Aoki H, Richmond M, Izumo S, Sadoshima J. Specific role of the extracellular signal-regulated kinase pathway in angiotensin II-induced cardiac hypertrophy in vitro. Biochem J. 2000;347 (Part 1):275–284. [PMC free article] [PubMed] [Google Scholar]