Abstract
Infection with Bartonella spp may cause cardiac arrhythmias, myocarditis and endocarditis in humans. The aim of the present study was to evaluate a possible association between Bartonella spp bacteremia and endocarditis, arrhythmia and Chagas cardiomyopathy in patients from Brazil and Argentina. We screened for the presence of bacterial 16S rRNA in human blood by PCR using oligonucleotides to amplify a 185-bp bacterial DNA fragment. Blood samples were taken from four groups of subjects in Brazil and Argentina: i) control patients without clinical disease, ii) patients with negative blood-culture endocarditis, iii) patients with arrhythmias, and iv) patients with chronic Chagas cardiomyopathy. PCR products were analyzed on 1.5% agarose gel to visualize the 185-bp fragment and then sequenced to confirm the identity of DNA. Sixty of 148 patients (40.5%) with cardiac disease and 1 of 56 subjects (1.8%) from the control group presented positive PCR amplification for Bartonella spp, suggesting a positive association of the bacteria with these diseases. Separate analysis of the four groups showed that the risk of a Brazilian patient with endocarditis being infected with Bartonella was 22 times higher than in the controls. In arrhythmic patients, the prevalence of infection was 45 times higher when compared to the same controls and 40 times higher for patients with Chagas cardiomyopathy. To the best of our knowledge this is the first report of the association between Bartonella spp bacteremia and Chagas disease. The present data may be useful for epidemiological and prevention studies in Brazil and Argentina.
Keywords: Human, PCR, Bartonella spp, Chagas disease, Endocarditis, Arrhythmia
Introduction
The Gram-negative organisms of the Bartonella genus are fastidious micro-aerobic bacteria classified into the second subgroup of the Proteobacteria class (1). This genus contains about 30 species, some of which have been isolated from humans (B. bacilliformis, B. henselae, B. elizabethae, and B. quintana) and from cats and dogs (B. koehlerae and B. vinsonii berkhoffii). Most known species of Bartonella have been isolated from rodent blood (2,3).
The life cycle of Bartonella spp consists of a reservoir host and vectors (e.g., ticks, fleas and lice) that transmit bacteria from the reservoir to novel hosts (3). Transmission may also occur through shared needles and syringes used by drug users. Hosts accidentally infected with Bartonella spp can show systemic signs, such as bacteremia and cardiac diseases mostly related to abnormalities in the heart valves, which may result in endocarditis (4,5). Surgery may be required in 20-40% of patients with infective endocarditis, mostly for valve replacement (5,6).
Ticks are considered to be zoonotic vectors that cause several diseases, and the tick Ixodes pacificus in particular may play an important role in the transmission of Bartonella to both humans and animals (2). Bartonella has been found in the blood of residential animals (domestic cats and dogs) and rodents, which are regarded as vectors and transmitters of several diseases (7,8). B. v. berkhoffii was isolated from a domestic dog with endocarditis (9), and an epidemiological study demonstrated that B. v. berkhoffii infection frequently occurs through ticks (10). B. v. berkhoffii and B. henselae were isolated from cerebrospinal fluid and periodontal swab samples from a patient who had contact with infected animals (11).
B. bacilliformis has also been found in erythrocytes, resulting in a severe hemolytic anemia known as Oroya fever (12). The cat-scratch disease, which is mainly caused by B. henselae, has been described as the most common Bartonella infection in humans worldwide (13). B. quintana infection was described during World War I, leading to trench or quintana fever (13), and there have been recent reports of urban trench fever (14,15). The symptoms of Bartonella infection include fever, fatigue, insomnia, joint pain, headache, weight loss, cardiac arrhythmias, and muscle pain (16). The major risk factors for B. quintana include infections, precarious conditions and chronic alcoholism. These risk factors are the same as those found for human immunodeficiency virus (HIV) and endocarditis (17). Therefore, although endocarditis caused by Bartonella spp has been underestimated, the presence of Bartonella infection should be further investigated in patients with negative blood culture and epidemiological antecedents related to chronic alcoholism, precarious conditions, contact with cats, fleas and lice, and in patients with endocarditis and positive serology for Chlamydia sp (18). B. quintana, B. henselae and B. elizabethae were first described as the causal agents of endocarditis in humans. Two other subspecies of B. vinsonii, berkhoffii and arupensis, were later found to be associated with endocarditis in patients with existing valvulopathies (14,18). B. henselae, which leads to endocarditis in children, exhibits negative results in serological tests (19). A number of studies in European countries have recently demonstrated that Coxiella burnetii, B. henselae and B. quintana are significantly associated with endocarditis in patients with negative blood culture (20). Siciliano et al. (21) showed that, of 61 assessed patients with endocarditis, 17 (27%) still had negative blood cultures. We reason that there are many negative blood cultures because the bacteria grow slowly and only in enriched medium (usually colonies are seen only after 20 days), which are conditions not routinely used in diagnostic laboratories. Serological tests are still helpful for diagnosis, but serum cross-reactivity between Bartonella, Chlamydia, and Coxiella species may interfere with the diagnosis and choice of treatment (6,20). Thus, molecular techniques such as PCR may be critical in providing a faster and more specific diagnosis of the disease (15,22). More recently, a multiplex PCR assay was developed to detect more than 20 different known and some unknown Bartonella species in both clinical and environmental samples (23). The gene targets for PCR amplification for the identification of specific species of Bartonella are either the conserved 16S rRNA, a generic marker for detecting any Bartonella species, or the intergenic transcribed spacer 16S-23S rRNA (23).
The medical significance of Bartonella species as human pathogens has been demonstrated by epidemiological, natural history, pathological, and host-microbial interaction studies (11,24). Patient co-infection by B. henselae and Borrelia burgdorferi has also been described (25) and therefore the association of Bartonella spp with other zoonoses must be investigated. Chagas disease is an important zooparasitosis in South America that frequently evolves to cardiomyopathy (26). To gain a better understanding of the consequences of Bartonella infection, we have analyzed samples from Brazilian and Argentinean patients with a single-step PCR assay. The subjects of this study, classified as heart disease patients, presented negative blood-culture endocarditis, relevant arrhythmias or Chagas cardiomyopathy. Our results suggest a strong association between the presence of Bartonella spp and these diseases. To the best of our knowledge this is the first report of such data from South America.
Material and Methods
Ethical aspects
The current project was approved by the Ethics Committee of Universidade Federal de São Carlos (UFSCar; CAAE #0024.1.135.000-06) and all subjects gave written informed consent to participate.
Patients and controls
This study investigated 56 normal voluntary subjects (control group) without cardiac disease and 148 voluntary subjects with heart diseases (46 cases with negative blood-culture endocarditis, 29 with relevant cardiac arrhythmias and 73 with chronic Chagas cardiomyopathy) between 2004-2008. These subjects were assessed and selected by cardiologists from Brazil and Argentina. Each subject was asked to complete a standard questionnaire, which included age, gender, previous contact with animals and arthropods, clinical symptoms, and eventual antibiotic treatment. The control group included 32 volunteers from a medical course in the city of Paracatu, Minas Gerais State, and 24 from the city of São Carlos, in São Paulo State, Brazil. Among this last group, 10 were from a rest home for the elderly and did not present any detectable heart problems. The patients with arrythmia and endocarditis were from the cities of São Carlos (SP, 10 cases) and from the city of São Paulo (SP, 65 cases). Fifty-two cases of Chagas cardiomyopathy were selected from the University Hospital, Ribeirão Preto (SP), Brazil. Twenty-one patients with chronic Chagas cardiomyopathy from Argentina were selected from the locality of Añatuya, Santiago del Estero, a highly endemic region in Argentina. Thirty-two asymptomatic subjects but seropositive for Chagas disease were selected from blood donors admitted to Hemocentro Buenos Aires and to the service of Obstetrics of Rivadavia Hospital. All of them were residents of the metropolitan area of Buenos Aires but 6 were originally from Bolivia, 3 from Paraguay, and 6 from the Chaco region (26).
Blood sample collection from the subjects
A 10-mL sample of venous blood was collected into vacuum tubes containing 72 USP units of EDTA/tube that was used for extraction of genomic DNA. DNA was extracted from 500 µL total blood according to modifications of the methodology described by Lahiri and Nurnberg Jr. (27). Alternatively, 10 mL peripheral blood was collected from Chagas disease patients and immediately mixed with one volume of 2X lysis buffer containing 6 M guanidinium hydrochloride and 0.2 M EDTA, pH 8.0 (GE) (28). The GE-blood lysate (GEB) was boiled (29) and stored at 4°C. DNA was purified from 100 µL aliquots of GEB by phenol extraction and isopropanol precipitation, as previously reported (30).
DNA amplification
Genomic DNA from blood was used as template for PCR to confirm the presence of Bartonella spp. The primers used in the PCR were designed as previously described (7). The primer sequences were Bh16SF (5′-AGAGTTTGATCCTGGCTCAG-3′) and Bh16SR (5′-CCGATAAATCTTTCTCCCTAA-3′), which amplify a 185-bp fragment of the 16S rRNA gene of B. henselae strain Houston-1 (GenBank accession No. NC_005956). The primers P1-5EZ (5′-ATAATCACATGGAGAGCCACAAGCT-3′) and P2-3EZ (5′-GCACTTCTTTGGTATCTGAGAAAGT-3′), which amplify a 447-bp product of the ZFY and ZFX human genes, were used to assess the DNA integrity of the extracted blood samples (31). Each reaction contained 1 µg DNA, 0.2 µg of each primer, 250 µM of each dNTP, 10 mM Tris-HCl, pH 8.5, 25 mM KCl, 5 mM (NH4)2SO4, 2 mM MgCl2, and 1.5 U Taq DNA polymerase in a final volume of 100 µL.
The PCR conditions were as follows: 35 cycles of 95°C for 30 s, 54°C for 1 min, and 72°C for 45 s, followed by a final extension of 10 min at 72°C. The amplification products were analyzed on 1.5% agarose gels in the presence of ethidium bromide. A negative control was included in each PCR run to avoid false results. Bands from representative samples corresponding to the 185-bp fragment were removed from the agarose gels, purified using the Perfectprep Gel Cleanup Kit (Eppendorf, Germany) and sequenced. The samples were prepared using the DYEnamic™ ET Dye Terminator Kit (GE Healthcare®, Sweden) with the same primers. The reactions were cycled (95°C for 20 s, 50°C for 15 s, and 60°C for 1 min), precipitated using ammonium acetate and ethanol, washed with 70% ethanol, eluted in 10 µL loading solution, and run on a MegaBACE™ DNA Analysis System (GE Healthcare®).
DNA data analysis
The sequences obtained were analyzed using the BLAST program (http://www.ncbi.nlm.nih.gov/BLAST/) (32) and compared to each other with the MULTALIN program (http://prodes.toulouse.inra.fr/multalin/multalin.html) (33).
Statistical analysis
The correlation between DNA amplification for Bartonella spp and human heart diseases was analyzed by the chi-square test. This test was used to determine if the observed frequency of heart disease associated with Bartonella bacteremia was significantly different from the distribution of expected heart disease frequency. In addition, the odds ratio was also calculated to measure the strength of association or non-independence between the two calculated frequencies (34).
Results
Study patients and controls
A total of 204 subjects were selected clinically and DNA samples were obtained from their blood (Table 1). The most important criteria for inclusion in the heart disease group were the presence of blood-negative endocarditis, relevant arrhythmias or Chagas cardiomyopathy. Patients with endocarditis or arrhythmias were serum negative for Chagas disease. Most subjects reported to have had previous contact with animals (dogs, cats, and horses) but this was not an exclusive criterion since it was highly variable along their lifetime. The most frequent diagnoses in the endocarditis group were mitral insufficiency, aortic stenosis, mitral stenosis, and mitral dysfunction, among others. Four cases of endocarditis were treated with nonspecific antibiotics before blood collection. Data from a group of 32 asymptomatic Argentinean subjects but with positive serology for Chagas disease were also obtained and used only for comparison with Chagas disease patients. However, this group was not considered to be either a control or case group and therefore it was not included in the total.
Table 1. Distribution of the 204 subjects who participated in this study from April 2004 to June 2008.
| Groups | N/group | City/Statea | Age | Gender | Contact with animals |
|---|---|---|---|---|---|
| Brazil | |||||
| Control group | 32 | Paracatu, MG | 22.3 ± 4.0 | 15 M, 17 F | ∼50% |
| 24 | São Carlos, SP | 47.2 ± 21.4 | 8 M, 16 F | 100% | |
| Case groups | |||||
| Endocarditis | 46 | São Paulo, SP | 53.5 ± 15.1 | 26 M, 20 F | ∼60% |
| Arrhythmias | 19 | São Paulo, SP | NI | 12 M, 7 F | 100% |
| Arrhythmias | 10 | São Carlos, SP | 61.8 ± 23.7 | 3 M, 7 F | 100% |
| Chagas cardiomyopathy | 52 | Ribeirão Preto, SP | 71.3 ± 12.9 | 36 M, 16 F | NI |
| Argentina | |||||
| Chagas cardiomyopathy | 21 | Buenos Aires | 37.9 ± 6.9 | 9 M, 12 F | NI |
| Chagas asymptomaticb | 32 | Buenos Aires | 41.8 ± 8.7 | 16 M, 16 F | NI |
Data are reported as means ± SD.
Place of blood donation. Four members of the endocarditis group were treated with nonspecific antibiotics before blood collection.
Asymptomatic Argentinean subjects (N = 32) were used only for comparison with Chagas disease patients and not included in the total. NI = not informed.
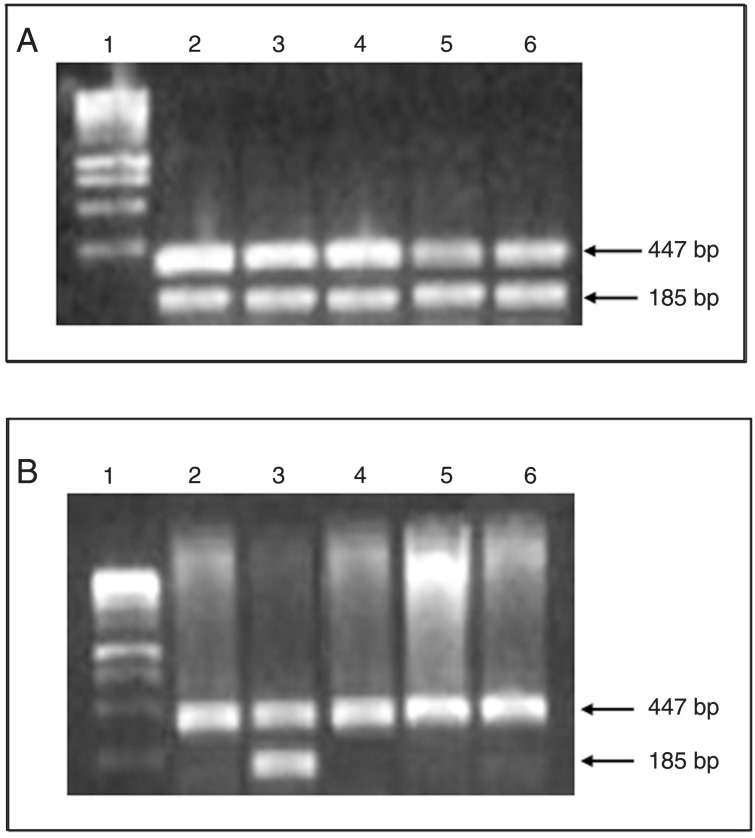
Amplification of human DNA samples
Patient DNA was subjected to PCR with the described oligonucleotides and the products were analyzed on a 1.5% agarose gel for the detection of 185- and 447-bp fragments. All reactions showed the positive control fragment of 447 bp. The 185-bp fragment, corresponding to the 16S rRNA gene of Bartonella, was present in 1 (1.8%) subject from the control group and in 60 (40.5%) subjects from the group of patients (Table 2; Figure 1A and B). The odds ratio and calculated chi-square are shown in Table 3. The odds ratio test showed a strong association between all groups of patients and the presence of bacteria. The risk of the Brazilian and Argentinean patients being infected with Bartonella spp was 37 times higher compared to control.
Table 2. Amplification of 16S rRNA for the detection of Bartonella spp in healthy volunteers (controls) and patients with heart diseases from Brazil and Argentina.
| Group | Number of samples* | Positive PCR (16S rRNA) | Negative PCR (16S rRNA) |
|---|---|---|---|
| Controls | 56 | 1 (1.8%) | 55 (98.2%) |
| Cases# | 148 | 60 (40.5%) | 88 (59.5%) |
| Total | 204 | 61 (29.9%) | 143 (70.1%) |
Samples from the two countries.
Asymptomatic subjects from Argentina were not included.
Figure 1. Analysis of the products obtained by PCR amplification of a fragment of the Bartonella spp 16S rRNA gene from DNA extracted from whole blood of humans with endocarditis (A) and subjects from the control group (B). Lane 1 = Ladder 1-kb marker; lanes 2 to 6 = PCR products in representative samples from 5 individuals. The 185- and 447-bp fragments (lower and upper bands) refer to the amplification of bacterial 16S rRNA and control gene, respectively.
Table 3. Association of heart disease and the presence of bacteria in the blood of patients.
| Groups | No. of subjects | Positive PCR | Negative PCR | OR | 95%CI | P |
|---|---|---|---|---|---|---|
| Without heart disease, total | 56 | 1 | 55 | |||
| Heart disease, total | 148 | 60 | 88 | 37.50 | 5.4-748.7 | <0.001* |
| Chagas disease, total | 73 | 34 | 39 | 47.95 | 6.5-981.0 | <0.001* |
| Brazilian subjects | ||||||
| Controls | 56 | 1 | 55 | |||
| Endocarditis | 46 | 13 | 33 | 21.67 | 2.7-463.8 | <0.001* |
| Arrhythmias | 29 | 13 | 16 | 44.69 | 5.3-986.2 | <0.001* |
| Chagas cardiomyopathy | 52 | 22 | 30 | 40.33 | 5.3-842.8 | <0.001* |
| Argentinean subjects | ||||||
| Chagas cardiomyopathy | 21 | 12 | 9 | |||
| Chagas asymptomatic | 32 | 11 | 21 | 2.55 | 0.71-9.28 | 0.17# |
| Chagas cardiomyopathy | ||||||
| Brazilian patients | 52 | 22 | 30 | |||
| Argentinean patients | 21 | 12 | 9 | 0.55 | 0.17-1.72 | 0.37## |
OR = odds ratio; CI = confidence interval.
Compared to control.
Compared to Argentinean subjects with Chagas cardiomyopathy;
compared to Brazilian subjects with Chagas cardiomyopathy.
Data were also analyzed by Brazilian subgroups of the diseases. In this case, the risk of Bartonella spp bacteremia was 21.7 times higher for patients with endocarditis, 47.1 times higher for patients with arrhythmias, and 40.3 times higher for Chagas cardiomyopathy patients (Table 3). The risk of an Argentinean patient with Chagas cardiomyopathy to be infected with Bartonella was not significantly different from that of a Brazilian patient with the same disease. No statistical difference was found between Argentinean asymptomatic subjects with positive serology and the group of Argentinean patients with Chagas cardiomyopathy.
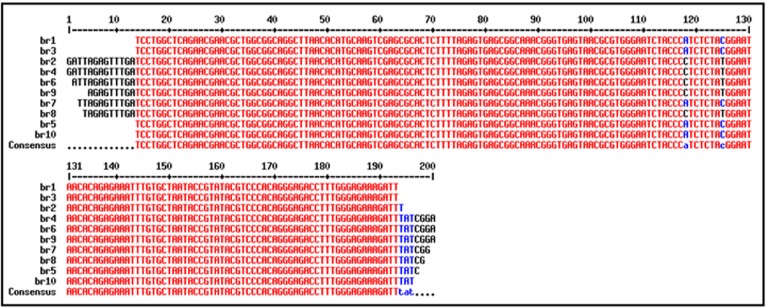
DNA sequencing of PCR products
Representative sequences (N = 35) from each group obtained from the PCR products were compared to the sequences deposited in public databases and confirmed the presence of Bartonella spp in the subjects. Figure 2 shows an alignment of representative sequences from 10 different positive subjects. Only two substitutions were found for this group in the sequence spanning position +13 to +193 bp. The consensus sequence of this alignment was compared to bacterial sequences at GenBank with the highest hits (e-value of 9e-06) with the 16S ribosomal RNA from several Bartonella species (Table 4). The majority of sequenced samples showed greater similarity to B. henselae, but bacteremic subjects could be found with B. vinsonii, B. v. berkhoffii and B. quintana sequence similarity.
Figure 2. Alignment of 10 representative sequences of amplified fragments from patients infected with Bartonella. The alignment shows the high identity between the sequences. The consensus sequence was blasted against the GenBank collection with significant hits (e-value of 9e-06) with 16S ribosomal RNA from different Bartonella species (accession Nos. of the best hits: DQ645425.1, DQ228135.1, U26258.1, M11927, AF143446.1, DQ641913.1).
Table 4. Best BLAST results for the PCR product sequences of representative samples of each group.
| Groups | Retrieved BLAST number | Number of individuals with identical sequences within the same group | Species with the highest hit | Similarity (%) |
|---|---|---|---|---|
| Control (N = 10) | DQ228135.1 | 4 | B. vinsonii berkhofii | 99 |
| DQ645425.1 | 3 | B. henselae | 99 | |
| U26258.1 | 2 | B. vinsonii | 99 | |
| M11927 | 1 | B. quintana | 97 | |
| Endocarditis (N = 9) | DQ641913.1 | 4 | B. henselae | 99 |
| AF143446.1 | 3 | B. vinsonii berkhofii | 99 | |
| U26258.1 | 2 | B. vinsonii | 98 | |
| Arrhythmia (N = 8) | DQ645425.1 | 3 | B. henselae | 99 |
| DQ641913.1 | 3 | B. vinsonii berkhofii | 99 | |
| U26258.1 | 2 | B. vinsonii | 98 | |
| Chagas disease (N = 8) | DQ645425.1 | 4 | B. henselae | 99 |
| DQ228135.1 | 2 | B. vinsonii berkhofii | 99 | |
| U26258.1 | 2 | B. vinsonii | 99 |
N = number of representative PCR products that were sequenced for each group. B. = Bartonella.
N = number of representative PCR products that were sequenced for each group. B. = Bartonella.
Discussion
The incidence of negative blood-culture endocarditis cases ranges from 3 to 31% of all cases of endocarditis (20,35). Zoonoses and bacterial infections transmitted by arthropods are now recognized as emerging infectious agents that could cause endocarditis. In the present study, we analyzed 46 culture-negative endocarditis patients and found that 13 (28%) were positive for Bartonella spp. These results are consistent with previous data, which suggest that Bartonella infection is observed in 28 to 50% of all culture-negative endocarditis cases (20,35). Bartonella infection is probably underdiagnosed due to nonspecific symptoms such as fever, weight loss and muscle pain. However, symptoms may become progressively more severe with eventual neurological symptoms if patients are not treated (11). Embolic phenomena and glomerulonephritis have also been described as complications of Bartonella infection (18,20). Serology has been shown to be useful in confirming the presence of C. burnetii and Bartonella species, but the PCR technique proved to be more sensitive and specific for the diagnosis of specimens such as Tropheryma whipplei, Bartonella and fungi in blood and valvular biopsies (36).
There are few reports on the association of Bartonella and cardiac malignant arrhythmias in dogs (7) or humans (8). It was suggested that Bartonella spp induced silent subacute myocarditis and electric instability, which could be the major pathogenic factor in the development of arrhythmogenic right ventricular cardiomyopathy-like disease. However, the association between Bartonella spp infection and the onset of arrhythmias is not yet well understood. In this study, we show that 13 of 29 patients (45%) with arrhythmias were also positive for Bartonella, suggesting a strong association between bacterial infection and the disease.
Chagas disease (American trypanosomiasis) is still a major health concern in South America. According to the World Health Organization, 10 million people are infected with Trypanosoma cruzi worldwide, mostly in Latin America (37). Up to 30% of chronically infected people develop cardiac disorders and up to 10% develop digestive, neurological, or mixed alterations, for which specific treatment may become necessary. Here we demonstrate a strong association between Chagas cardiomyopathy and Bartonella infection in Brazilian and Argentinean patients. Also, there was no statistically significant difference between asymptomatic Argentinean subjects with positive serology and the group of Argentinean patients with Chagas cardiomyopathy. These results suggest a role for the vector of American trypanosomiasis, mostly Triatoma infestans, in transmitting Bartonella or other bacteria. This possibility should be investigated in order to achieve a better understanding of the association of Chagas disease and Bartonella bacteremia. The high prevalence of positive subjects in the Chagas disease group strongly suggests that a method for controlling this zoonosis is necessary. The contribution of Bartonella spp infection to the evolution of Chagas disease or to the intensity of symptoms remains to be determined.
One in 56 asymptomatic subjects that donated blood for this study had Bartonella spp bacteremia. Asymptomatic bacteremia had been already reported in blood donors (38). Immunodeficient patients, as HIV seropositive patients or patients receiving corticotherapy, can have angioproliferative reactions as seen in bacillary angiomatosis or bacillary peliosis hepatic as well fatal Bartonella spp infection (39). Further studies will be necessary to establish the relevance of Bartonella spp transmission by transfusion, especially in immunodeficient patients.
Our data show that Bartonella spp may be important etiologic agents of culture-negative endocarditis and should be investigated in all culture-negative endocarditis cases as well as in other suspected conditions. Our results also suggest a strong association between Bartonella spp bacteremia and arrythmia or Chagas cardiomyopathy. As far as we know, this is the first report of such data from South America.
Acknowledgments
The authors are grateful to Dr. João Santana da Silva, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, SP, Brazil, for providing the samples from patients with Chagas disease. Research supported by FAPESP and CNPq.
References
- 1.La Scola B, Raoult D. Culture of Bartonella quintana and Bartonella henselae from human samples: a 5-year experience (1993 to 1998) J Clin Microbiol. 1999;37:1899–1905. doi: 10.1128/jcm.37.6.1899-1905.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang CC, Chomel BB, Kasten RW, Romano V, Tietze N. Molecular evidence of Bartonella spp. in questing adult Ixodes pacificus ticks in California. J Clin Microbiol. 2001;39:1221–1226. doi: 10.1128/JCM.39.4.1221-1226.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Welch DF, Carroll KC, Hofmeister EK, Persing DH, Robison DA, Steigerwalt AG, et al. Isolation of a new subspecies, Bartonella vinsonii subsp. arupensis, from a cattle rancher: identity with isolates found in conjunction with Borrelia burgdorferi and Babesia microti among naturally infected mice. J Clin Microbiol. 1999;37:2598–2601. doi: 10.1128/jcm.37.8.2598-2601.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol Rev. 2001;14:177–207. doi: 10.1128/CMR.14.1.177-207.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jenkins NP, Habib G, Prendergast BD. Aorto-cavitary fistulae in infective endocarditis: understanding a rare complication through collaboration. Eur Heart J. 2005;26:213–214. doi: 10.1093/eurheartj/ehi076. [DOI] [PubMed] [Google Scholar]
- 6.Tang YW. Duplex PCR assay simultaneously detecting and differentiating Bartonella quintana, B. henselae, and Coxiella burnetii in surgical heart valve specimens. J Clin Microbiol. 2009;47:2647–2650. doi: 10.1128/JCM.00721-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breitschwerdt EB, Atkins CE, Brown TT, Kordick DL, Snyder PS. Bartonella vinsonii subsp. berkhoffii and related members of the alpha subdivision of the Proteobacteria in dogs with cardiac arrhythmias, endocarditis, or myocarditis. J Clin Microbiol. 1999;37:3618–3626. doi: 10.1128/jcm.37.11.3618-3626.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breitschwerdt EB, Kordick DL. Bartonella infection in animals: carriership, reservoir potential, pathogenicity, and zoonotic potential for human infection. Clin Microbiol Rev. 2000;13:428–438. doi: 10.1128/cmr.13.3.428-438.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breitschwerdt EB, Kordick DL, Malarkey DE, Keene B, Hadfield TL, Wilson K. Endocarditis in a dog due to infection with a novel Bartonella subspecies. J Clin Microbiol. 1995;33:154–160. doi: 10.1128/jcm.33.1.154-160.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pappalardo BL, Correa MT, York CC, Peat CY, Breitschwerdt EB. Epidemiologic evaluation of the risk factors associated with exposure and seroreactivity to Bartonella vinsonii in dogs. Am J Vet Res. 1997;58:467–471. [PubMed] [Google Scholar]
- 11.Breitschwerdt EB, Maggi RG, Farmer P, Mascarelli PE. Molecular evidence of perinatal transmission of Bartonella vinsonii subsp. berkhoffii and Bartonella henselae to a child. J Clin Microbiol. 2010;48:2289–2293. doi: 10.1128/JCM.00326-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pitassi LH, Magalhaes RF, Barjas-Castro ML, de Paula EV, Ferreira MR, Velho PE. Bartonella henselae infects human erythrocytes. Ultrastruct Pathol. 2007;31:369–372. doi: 10.1080/01913120701696510. [DOI] [PubMed] [Google Scholar]
- 13.Kordick DL, Hilyard EJ, Hadfield TL, Wilson KH, Steigerwalt AG, Brenner DJ, et al. Bartonella clarridgeiae, a newly recognized zoonotic pathogen causing inoculation papules, fever, and lymphadenopathy (cat scratch disease) J Clin Microbiol. 1997;35:1813–1818. doi: 10.1128/jcm.35.7.1813-1818.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lejko-Zupanc T, Slemenik-Pusnik C, Kozelj M, Klokocovnik T, Avsic-Zupanc T, Dolenc-Strazar Z, et al. Native valve endocarditis due to Bartonella henselae in an immunocompetent man. Wien Klin Wochenschr. 2008;120:246–249. doi: 10.1007/s00508-008-0951-3. [DOI] [PubMed] [Google Scholar]
- 15.Jenkins NE, Ferguson DJ, Alp NJ, Harrison TG, Bowler IC. Urban trench fever presenting as culture-negative endocarditis. QJM. 2009;102:63–65. doi: 10.1093/qjmed/hcn118. [DOI] [PubMed] [Google Scholar]
- 16.Breitschwerdt EB, Maggi RG, Robert MB, Hegarty BC, Bradley JM, Mascarelli PE. PCR amplification of Bartonella koehlerae from human blood and enrichment blood cultures. Parasit Vectors. 2010;3:76. doi: 10.1186/1756-3305-3-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Velho PE, Pimentel V, Del Negro GM, Okay TS, Diniz PP, Breitschwerdt EB. Severe anemia, panserositis, and cryptogenic hepatitis in an HIV patient infected with Bartonella henselae. Ultrastruct Pathol. 2007;31:373–377. doi: 10.1080/01913120701696601. [DOI] [PubMed] [Google Scholar]
- 18.Fournier PE, Lelievre H, Eykyn SJ, Mainardi JL, Marrie TJ, Bruneel F, et al. Epidemiologic and clinical characteristics of Bartonella quintana and Bartonella henselae endocarditis: a study of 48 patients. Medicine. 2001;80:245–251. doi: 10.1097/00005792-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Pitchford CW, Creech CB, Peters TR, Vnencak-Jones CL. Bartonella henselae endocarditis in a child. Pediatr Cardiol. 2006;27:769–771. doi: 10.1007/s00246-006-1383-3. [DOI] [PubMed] [Google Scholar]
- 20.Martin L, Vidal L, Campins A, Salva F, Riera M, Carrillo A, et al. Bartonella as a cause of blood culture-negative endocarditis. Description of five cases. Rev Esp Cardiol. 2009;62:694–697. doi: 10.1016/s1885-5857(09)72235-2. [DOI] [PubMed] [Google Scholar]
- 21.Siciliano RF, Strabelli TM, Zeigler R, Rodrigues C, Castelli JB, Grinberg M, et al. Infective endocarditis due to Bartonella spp. and Coxiella burnetii: experience at a cardiology hospital in São Paulo, Brazil. Ann N Y Acad Sci. 2006;1078:215–222. doi: 10.1196/annals.1374.123. [DOI] [PubMed] [Google Scholar]
- 22.Walls T, Moshal K, Trounce J, Hartley J, Harris K, Davies G. Broad-range polymerase chain reaction for the diagnosis of Bartonella henselae endocarditis. J Paediatr Child Health. 2006;42:469–471. doi: 10.1111/j.1440-1754.2006.00900.x. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Esteban C, Gil H, Rodriguez-Vargas M, Gerrikagoitia X, Barandika J, Escudero R, et al. Molecular method for Bartonella species identification in clinical and environmental samples. J Clin Microbiol. 2008;46:776–779. doi: 10.1128/JCM.01720-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karem KL, Paddock CD, Regnery RL. Bartonella henselae, B. quintana, and B. bacilliformis: historical pathogens of emerging significance. Microbes Infect. 2000;2:1193–1205. doi: 10.1016/s1286-4579(00)01273-9. [DOI] [PubMed] [Google Scholar]
- 25.Podsiadly E, Chmielewski T, Tylewska-Wierzbanowska S. Bartonella henselae and Borrelia burgdorferi infections of the central nervous system. Ann N Y Acad Sci. 2003;990:404–406. doi: 10.1111/j.1749-6632.2003.tb07400.x. [DOI] [PubMed] [Google Scholar]
- 26.Bisio M, Seidenstein ME, Burgos JM, Ballering G, Risso M, Pontoriero R, et al. Urbanization of congenital transmission of Trypanosoma cruzi: prospective polymerase chain reaction study in pregnancy. Trans R Soc Trop Med Hyg. 2011;105:543–549. doi: 10.1016/j.trstmh.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 27.Lahiri DK, Nurnberger JI., Jr A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res. 1991;19:5444. doi: 10.1093/nar/19.19.5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avila HA, Sigman DS, Cohen LM, Millikan RC, Simpson L. Polymerase chain reaction amplification of Trypanosoma cruzi kinetoplast minicircle DNA isolated from whole blood lysates: diagnosis of chronic Chagas' disease. Mol Biochem Parasitol. 1991;48:211–221. doi: 10.1016/0166-6851(91)90116-n. [DOI] [PubMed] [Google Scholar]
- 29.Britto C, Cardoso MA, Wincker P, Morel CM. A simple protocol for the physical cleavage of Trypanosoma cruzi kinetoplast DNA present in blood samples and its use in polymerase chain reaction (PCR)-based diagnosis of chronic Chagas disease. Mem Inst Oswaldo Cruz. 1993;88:171–172. doi: 10.1590/s0074-02761993000100030. [DOI] [PubMed] [Google Scholar]
- 30.Schijman AG, Vigliano C, Burgos J, Favaloro R, Perrone S, Laguens R, et al. Early diagnosis of recurrence of Trypanosoma cruzi infection by polymerase chain reaction after heart transplantation of a chronic Chagas' heart disease patient. J Heart Lung Transplant. 2000;19:1114–1117. doi: 10.1016/s1053-2498(00)00168-6. [DOI] [PubMed] [Google Scholar]
- 31.Aasen E, Medrano JF. Amplification of the ZFY and ZFX genes for sex identification in humans, cattle, sheep and goats. Biotechnology. 1990;8:1279–1281. doi: 10.1038/nbt1290-1279. [DOI] [PubMed] [Google Scholar]
- 32.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J Mol Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 33.Corpet F. Multiple sequence alignment with hierarchical clustering. Nucleic Acids Res. 1988;16:10881–10890. doi: 10.1093/nar/16.22.10881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morris JA, Gardner MJ. Calculating confidence intervals for relative risks (odds ratios) and standardised ratios and rates. Br Med J (Clin Res Ed) 1988;296:1313–1316. doi: 10.1136/bmj.296.6632.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Houpikian P, Raoult D. Blood culture-negative endocarditis in a reference center: etiologic diagnosis of 348 cases. Medicine. 2005;84:162–173. doi: 10.1097/01.md.0000165658.82869.17. [DOI] [PubMed] [Google Scholar]
- 36.Fournier PE, Thuny F, Richet H, Lepidi H, Casalta JP, Arzouni JP, et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin Infect Dis. 2010;51:131–140. doi: 10.1086/653675. [DOI] [PubMed] [Google Scholar]
- 37.WHO . South America. Accordingly to the World Health Organization. Available at [ http://www.who.in/en]. [Google Scholar]
- 38.Magalhaes RF, Cintra ML, Barjas-Castro ML, Del Negro GM, Okay TS, Velho PE. Blood donor infected with Bartonella henselae. Transfus Med. 2010;20:280–282. doi: 10.1111/j.1365-3148.2010.01001.x. [DOI] [PubMed] [Google Scholar]
- 39.Velho PE, Cintra ML, Uthida-Tanaka AM, de Moraes AM, Mariotto A. What do we (not) know about the human bartonelloses? Braz J Infect Dis. 2003;7:1–6. doi: 10.1590/s1413-86702003000100001. [DOI] [PubMed] [Google Scholar]