Abstract
Objective: To determine the prevalence, correlates and changes in secondhand smoke (SHS) exposure over the period after comprehensive smoke-free policy implementation in two Latin American countries.
Methods: Data were analysed from population-based representative samples of adult smokers and recent quitters from the 2008 and 2010 waves of the International Tobacco Control Policy Evaluation Survey in Mexico (n = 1766 and 1840, respectively) and Uruguay (n = 1379 and 1411, respectively). Prevalence of SHS exposure was estimated for regulated venues, and generalized estimating equations were used to determine correlates of SHS exposure.
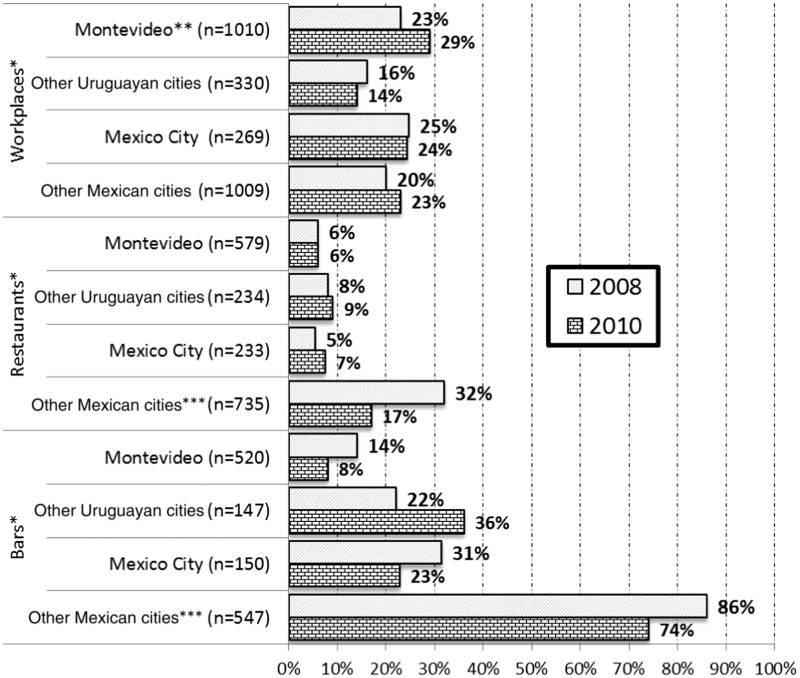
Results: Workplace SHS exposure in the last month was similar within and across countries (range: Mexico 20–25%; Uruguay 14–29%). At the most recent restaurant visit, SHS exposure was lower where comprehensive smoke-free policies were implemented (range: Uruguay 6–9%; Mexico City 5–7%) compared with Mexican cities with weaker policies, where exposure remained higher but decreased over time (32–17%). At the most recent bar visit, SHS exposure was common (range: Uruguay 8–36%; Mexico City 23–31%), although highest in jurisdictions with weaker policies (range in other Mexican cities: 74–86%). In Uruguay, males were more likely than females to be exposed to SHS across venues, as were younger compared with older smokers in Mexico.
Conclusions: Comprehensive smoke-free policies are more effective than weaker policies, although compliance in Mexico and Uruguay is not as high as desired.
Keywords: Tobacco smoke pollution, secondhand smoke, public policy, policy compliance, developing countries
KEY MESSAGES.
High-income countries appear to have higher compliance with smoke-free policies than low- and middle-income countries (LMICs); however, evidence regarding policy compliance in LMICs over the post-implementation period is mostly anecdotal, suffers from selection bias and does not assess whether some populations suffer relatively higher SHS exposure.
This study provides population-based representative data on smoke-free policy compliance in two countries that have been leaders in tobacco control, confirming that comprehensive smoke-free policies are more effective than smoke-free policies that allow for exceptions.
It also indicates compliance issues in Mexico and Uruguay, suggesting the need for new efforts and strategies to enhance compliance and further reduce SHS exposure.
Introduction
Smoke-free policies are a cornerstone of the World Health Organization’s Framework Convention on Tobacco Control (WHO FCTC), which promotes a co-ordinated international policy and programmatic response to the tobacco epidemic (WHO 2003). Comprehensive smoke-free laws that prohibit smoking in all enclosed workplaces, including hospitality venues, have reduced secondhand smoke (SHS) exposure and associated disease in high- and middle-income countries (Skeer et al. 2004; Borland et al. 2006; Fong et al. 2006; Haw and Gruer 2007; Thrasher et al. 2010a,b; Lee et al. 2011; Nagelhout et al. 2011; Sebrié et al. 2012a). High levels of compliance with smoke-free policies have been found in some middle-income countries (WHO 2007; Reis et al. 2010), but not in others (WHO 2009; Ma et al. 2010; Thrasher et al. 2010a,b; Yong et al. 2010). Strategies to enhance compliance with smoke-free policies should be informed by a better understanding both of the venues where SHS exposure is most prevalent and of the sub-populations that are most likely to be exposed. This study aims to address these issues using representative data from cohorts of adult smokers and recent ex-smokers over a 2-year period of time after implementation of smoke-free laws in Mexico and Uruguay.
Background
In March 2006, Uruguay implemented the first countrywide comprehensive smoke-free policy in Latin America, prohibiting smoking in all enclosed workplaces and public venues (WHO 2011). Immediately after policy implementation, support for smoke-free policies among smokers was higher in Uruguay than in Mexico, where, at that time, no comprehensive smoke-free policies had been implemented (Thrasher et al. 2009). Anecdotal evidence (WHO 2009) and air monitoring suggests that initial compliance was good (Blanco-Marquizo et al. 2010), although this research was not conducted outside the capital of Montevideo, did not include private worksites, and suggested that SHS exposure declined less in restaurants and bars than in schools and public buildings. Nevertheless, the dramatic reduction in cardiovascular events in Montevideo after implementation suggests that the policy significantly reduced SHS exposure there (Sebrié et al. 2012a).
In April 2008, Mexico City became the first Mexican jurisdiction to implement a comprehensive smoke-free policy in all enclosed public venues and workplaces (Guillermo-Tenorio 2008; Thrasher et al. 2010b). At that time, Mexican jurisdictions were subject to weak federal regulations that only banned smoking in federal buildings. In May 2008, the General Tobacco Control Law was signed, which prohibited smoking in all enclosed workplaces and hospitality venues, while allowing for designated smoking areas (DSAs), as long as they had a separate ventilation system and were physically separated by walls from the rest of the venue (Ley General para el Control del Tabaco, 2008). Other countries with less restrictive DSAs than Mexico, such as Spain and Chile, have experienced difficulties with compliance and have not produced declines in SHS exposure that are found with comprehensive legislation (Erazo et al. 2010; López et al. 2012). The Mexican Federal Law came into force in August 2008, but regulations were not issued until May 2009 (Reglamento de la Ley General para el Control de Tabaco, 2009) and no studies have been published on its impact on SHS exposure.
SHS exposure declined and support for smoke-free policies increased more in Mexico City compared with three other Mexican cities, from before to after implementation of the Mexico City law (i.e. 2007–08) (Thrasher et al. 2010a). Policy implementation was also associated with declines in hospitalizations and mortality due to SHS-related diseases (Guerrero-López et al. 2012; Muños-Hernández et al. 2012). Nevertheless, SHS exposure in Mexico City was higher than in jurisdictions in high-income countries with comprehensive smoke-free policies (ITC Project 2012), and non-compliance was highest in bars, as has been found in high-income countries (Borland et al. 2006). SHS exposures in Mexico City have not been studied since initial policy implementation.
To our knowledge, no research has been conducted in middle-income countries to determine the correlates of SHS exposure after implementation of comprehensive smoke-free policies. In countries with partial smoking bans, SHS exposure has been associated with higher educational attainment (China) (Ma et al. 2010) and higher smoke-free policy support (Malaysia) (Yong et al. 2010), as well as with more positive attitudes towards smoking and lower knowledge of SHS health risks (Netherlands) (Nagelhout et al. 2011). In contrast, studies in high-income countries with comprehensive smoke-free policies have found that sociodemographic and smoking-related characteristics are unassociated with SHS exposure (Borland et al. 2006; Edwards et al. 2008), with some evidence suggesting that these policies can reduce pre-policy sociodemographic disparities in SHS exposure (Edwards et al. 2008). Further research in middle-income countries is needed to determine whether the benefits of comprehensive smoke-free policies are distributed equitably across population sub-groups and to determine whether additional strategies are necessary to target specific groups.
This study aimed to determine the prevalence, smoking-related and sociodemographic correlates, and changes over time in SHS exposure across regulated venues in Mexico and Uruguay. We expected that SHS exposure would remain stable over time in jurisdictions with comprehensive smoke-free policy; that SHS exposure would be lower in these jurisdictions than in those subject to the weaker federal law in Mexico; and that SHS exposure would be higher in bars than other venues. We also explored whether compliance was higher in the Uruguayan capital than in smaller Uruguayan cities that could experience less intensive monitoring by authorities.
Methods
Sample
Institutional Review Board approvals for this study were received from the Instituto Nacional de Salud Pública in Mexico and the Universidad de la República in Uruguay, and voluntary and informed consent of participants was obtained. Data were analysed from the 2008 and 2010 administrations of the International Tobacco Control Policy Evaluation Survey (ITC Survey) in Mexico and Uruguay. Data collection in Mexico occurred between November and December 2008, 7 months after smoke-free policy implementation in Mexico City, and between January and February 2010, when Mexican states should have implemented weaker federal legislation. Data collection in Uruguay began in September 2008, 30 months after initial implementation, and lasted until February 2009, followed by data collection between September and December 2010. A stratified, multi-stage sampling scheme was used in six Mexican cities (Mexico City, Guadalajara, Monterrey, Puebla, Tijuana and Mérida) and five Uruguayan cities (Montevideo, Salto, Maldonado, Durazno and Rivera), wherein census tracts and then block groups were selected with probability proportional to the number of households. Participant households were selected at random and visited up to four times to enumerate household members and recruit smokers who were 18 or older, smoked more than 100 lifetime cigarettes and smoked at least once in the previous week (see Thrasher et al. 2009 for further information). The same participants were followed from one wave to the next, and due to loss at follow-up, samples were replenished with adult smokers from already selected census tracts to maintain sample size across waves. The analytic samples for Uruguay (n = 1379 in 2008; n = 1411 in 2010) and Mexico (n = 1760 in 2008; n = 1840 in 2010) included both smokers and those who had quit smoking over the period of observation.
Measures
Dependent variables: SHS exposure
Participants were queried about smoking activity in three regulated venues: workplaces; restaurants and cafes (hereafter called ‘restaurants’); and bars, cantinas and discos (hereafter called ‘bars’). Participants who reported paid employment in enclosed environments were asked if someone had smoked in their workplace during the previous month (Mexico) or during the previous 6 months (Uruguay); participants were classified as exposed if they responded affirmatively. SHS exposure in restaurants and bars was assessed with questions on the frequency of going to these venues and whether someone had smoked inside during the last visit. Participants were classified as exposed if they visited the venue in the previous month and they indicated SHS exposure at their last visit.
Independent variables: smoking behaviour, sociodemographics and survey wave
For each wave, we created dummy variables for consumption intensity, with non-daily smokers as the reference group. Country-specific median cut-points were used for low- and high-daily consumption intensity (i.e. <5 per day and 5 or more per day in Mexico; <15 per day and 15 or more in Uruguay). As smokers could have quit after initial enrolment, another dummy variable indicated if the participant was no longer smoking at the assessment. Sex, age (i.e. 18–24, 25–39, 40–54, 55 or older), education (elementary or less, middle school, high school or technical, more than high school) and monthly household income (Mexican pesos: low 0–$3000, middle–low $3001–$5000, middle–high $5001–$8000, high >$8000; Uruguayan pesos: low 0–$4500, middle–low $4501–$8000, middle–high $8001–$15 000, high >$15 000) were all coded with dummy variables. We also created a dummy variable to indicate missing income data, so that this population would remain in analyses that included adjustment by income. City-level indicators were constructed, with the capital cities of each country as the reference group. Finally, a survey wave indicator was derived with 2008 as the reference group.
Analysis
Stata version 11.0 (StataCorp LP, College Station, TX, USA) was used for all analyses. Unweighted descriptive statistics were analysed, including chi-square tests to determine differences between the 2008 and 2010 samples within each country. All other estimates and analyses involved adjustment for sampling design and survey weights. Weights accounted for likelihood of participant selection and were rescaled to the number of observations within each city to produce more efficient estimates that kept data from the larger capital cities from overwhelming data from the other cities (Korn and Graubard 1999).
Primary analyses were restricted to participants that could have been exposed to SHS in the venues of interest: (1) participants with paid work in enclosed places (Mexico: n = 987 persons with 1278 observations; Uruguay: n = 986 persons with 1340 observations); (2) participants who visited a restaurant in the previous month (Mexico: n = 814 persons with 968 observations; Uruguay: n = 671 persons with 813 observations); (3) participants who visited a bar in the prior month (Mexico: n = 598 persons with 697 observations; Uruguay: n = 559 persons with 667 observations). For each country, we estimated the prevalence of self-reported SHS exposure at each venue by city (capital city and other cities) and wave (2008 and 2010). Over time differences within city strata (i.e. capital city, other cities) involved pooling data from both survey years and regressing SHS exposure on a dummy variable for survey year, using generalized estimating equations (GEEs) to account for repeated observations of participants surveyed at both waves (Hardin and Hilbe 2003). Subsequently, all data for each country were pooled and logistic GEE models estimated to determine the country-specific correlates of SHS exposure in each venue. For each venue, both crude and adjusted odds ratios (OR and AOR, respectively) were estimated for sociodemographics, smoking behaviour, survey wave and residence (i.e. capital city vs other cities).
Results
Sample characteristics
From 2008 to 2010, 74% (1309/1760) of the Mexican cohort and 70% (971/1379) of the Uruguay cohort were followed. Replacement participants in 2010 (n = 531 in Mexico; n = 440 in Uruguay) were recruited from the same geographical units as were sampled in 2008. No statistically significant differences in sample characteristics were found across years for Mexico, except that the percentage of smokers who had quit was higher in 2010. This difference was also found for Uruguay, as was a significantly higher income in 2010 than in 2008 (Table 1).
Table 1.
Smoker cohort sample characteristics in Mexico and Uruguay, 2008 and 2010
| Charcteristics | Mexico |
Uruguay |
||
|---|---|---|---|---|
| 2008 | 2010 | 2008 | 2010 | |
| (n = 1760) | (n = 1840) | (n = 1379) | (n = 1411) | |
| Sex | ||||
| Female | 38% | 38% | 51% | 51% |
| Male | 62% | 62% | 49% | 49% |
| Age | ||||
| 18–24 | 18% | 17% | 19% | 17% |
| 25–39 | 37% | 36% | 33% | 33% |
| 40–54 | 28% | 29% | 30% | 31% |
| 55 or older | 16% | 18% | 19% | 19% |
| Education | ||||
| <Middle school | 28% | 31% | 25% | 23% |
| Middle school | 29% | 30% | 36% | 32% |
| High School | 27% | 24% | 22% | 26% |
| >High School | 17% | 15% | 17% | 19% |
| Incomea | ||||
| Low | 25% | 28% | 17% | 8% |
| Middle–low | 24% | 24% | 21% | 13% |
| Midde–high | 20% | 21% | 27% | 25% |
| High | 19% | 20% | 27% | 43%c |
| Missing | 12% | 7% | 8% | 11% |
| Smoking behaviourb | ||||
| Non-daily | 32% | 28% | 8% | 8% |
| Low daily consumption | 38% | 37% | 41% | 39% |
| High daily consumption | 24% | 20% | 44% | 40% |
| Quitter | 7% | 15% | 6% | 13% |
| Cities | ||||
| Capital cityc | 23% | 23% | 71% | 71% |
| Other cities | 77% | 77% | 29% | 29% |
| SHS exposure | ||||
| Workplace | ||||
| Did not work in enclosed workplace | 42% | 45% | 28% | 25% |
| No SHS exposure in last month | 45% | 43% | 57% | 58% |
| SHS exposure in last month | 13% | 12% | 15% | 17% |
| Restaurant | ||||
| Did not go to restaurant in last month | 73% | 73% | 70% | 71% |
| No SHS exposure in last visit | 14% | 19% | 27% | 26% |
| SHS exposure in last visit | 13% | 8% | 3% | 3% |
| Bar | ||||
| Did not go to bar in last month | 79% | 82% | 74% | 78% |
| No SHS exposure in last visit | 7% | 7% | 20% | 17% |
| SHS exposure in last visit | 14% | 11% | 6% | 5% |
From 2008 to 2010, 74% (1309/1760) of the Mexican cohort and 70.4% (971/1379) of the Uruguay cohort were followed, with replacements in 2010 (n = 531 in Mexico; n = 440 in Uruguay) recruited from same geographical units.
aIncome higher in 2010 than in 2008 for Uruguay, P < 0.001.
bHigher percentage of quitters in 2010 than in 2008, in both Uruguay and Mexico, P < 0.001.
cCapital city = Mexico City for Mexico and Montevideo for Uruguay.
Workplace SHS exposure
Approximately three-quarters of Uruguayan participants worked indoors. In logistic GEE models for Uruguay (Table 2), males were more likely to report SHS workplace exposure than females (AOR = 1.77), as were smokers older than 55 years compared with the youngest group (AOR = 2.40). Crude and adjusted odds of reporting workplace exposure were lower in other Uruguayan cities compared with Montevideo (AOR = 0.58). Interactions between city and time were not statistically significant. Nevertheless, when changes over time were assessed within city strata (Figure 1), a statistically significant increase was found for Montevideo (23% in 2008 and 29% in 2010; P = 0.04).
Table 2.
Correlates of workplace SHS exposure in last month (Mexico and Uruguay, 2008 and 2010)
| Characteristics | Mexico |
Uruguay |
||||
|---|---|---|---|---|---|---|
| % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | |
| Sex | ||||||
| Female | 22 | 1 | 1 | 17 | 1 | 1 |
| Male | 23 | 0.98 (0.67–1.43) | 0.98 (0.67–1.43) | 31 | 2.01 (1.16–3.48)* | 1.77 (1.15–2.72)** |
| Age | ||||||
| 18–24 | 26 | 1 | 1 | 21 | 1 | 1 |
| 25–39 | 23 | 0.87 (0.57–1.34) | 0.82 (0.52–1.27) | 23 | 1.09 (0.58–2.05) | 1.17 (0.60–2.27) |
| 40–54 | 20 | 0.75 (0.46–1.20) | 0.57 (0.35–0.95)* | 18 | 0.78 (0.41–1.47) | 0.81 (0.42–1.59) |
| 55 or more | 24 | 0.94 (0.42–2.13) | 0.80 (0.31–2.03) | 43 | 2.51 (0.75–8.40) | 2.40 (1.01–5.69)* |
| Education | ||||||
| <Middle school | 23 | 1 | 1 | 30 | 1 | 1 |
| Middle school | 26 | 1.34 (0.82–2.20) | 1.23 (0.73–2.06) | 25 | 0.93 (0.34–2.57) | 1.21 (0.62–2.34) |
| High School | 22 | 1.03 (0.64–1.66) | 0.93 (0.54–1.60) | 22 | 0.82 (0.29–2.32) | 0.94 (0.45–1.97) |
| >High School | 19 | 0.89 (0.50–1.58) | 0.76 (0.37–1.57) | 17 | 0.53 (0.18–1.53) | 0.61 (0.28–1.30) |
| Income | ||||||
| Low | 22 | 1 | 1 | 20 | 1 | 1 |
| Middle–low | 26 | 1.27 (0.75–2.16) | 1.31 (0.78–2.20) | 16 | 0.80 (0.48–1.33) | 0.71 (0.42–1.21) |
| Midde–high | 23 | 1.07 (0.65–1.79) | 1.11 (0.66–1.87) | 23 | 1.30 (0.68–2.49) | 1.28 (0.59–2.78) |
| High | 22 | 1.08 (0.67–1.77) | 1.26 (0.73–2.16) | 24 | 1.36 (0.72–2.57) | 1.21 (0.55–2.70) |
| Missing | 14 | 0.55 (0.28–1.11) | 0.59 (0.28–1.24) | 36 | 1.71 (0.46–6.42) | 1.18 (0.44–3.16) |
| Smoking behaviour | ||||||
| Non-daily smoker | 20 | 1 | 1 | 19 | 1 | 1 |
| Low daily consumption | 22 | 1.12 (0.73–1.73) | 1.13 (0.73–1.76) | 17 | 0.90 (0.46–1.78) | 0.90 (0.46–1.78) |
| High daily consumption | 33 | 1.96 (1.21–3.2)** | 2.16 (1.31–3.54)** | 26 | 1.43 (0.75–2.71) | 1.43 (0.75–2.71) |
| Quitter | 18 | 0.78 (0.41–1.52) | 0.81 (0.42–1.57) | 39 | 1.96 (0.84–4.54) | 1.96 (0.84–4.54) |
| Year | ||||||
| 2008 | 22 | 1 | 1 | 21 | 1 | 1 |
| 2010 | 23 | 1.07 (0.77–1.5) | 1.05 (0.75–1.45) | 26 | 1.17 (0.92–1.49) | 1.17 (0.88–1.57) |
| Residence | ||||||
| Capital city | 24 | 1 | 1 | 26 | 1 | 1 |
| Other cities | 22 | 0.87 (0.58–1.3) | 0.78 (0.51–1.21) | 15 | 0.55 (0.33–0.92)* | 0.58 (0.36–0.93)* |
aAdjusted ORs control for all variables shown in the table.
*P < 0.05; **P < 0.01.
Figure 1.
Prevalence of secondhand smoke (SHS) exposure inside regulated venues in Uruguay and Mexico, 2008 and 2010 *Analytic samples included only the participants who could have been exposed (i.e. worked in enclosed workplaces; visited restaurant or bar in last month). Workplace exposure included any SHS in last month. Restaurant and bar exposure was queried for the most recent visit. **Significant changes over time within city strata at P < 0.05. ***Significant changes over time within city strata at P < 0.01.
A little more than half of Mexican participants worked in enclosed places (58% in 2008 and 55% in 2010). In GEE models (Table 2), Mexican participants who were 40–54 years old were significantly less likely to report workplace SHS exposure than the youngest participants (AOR = 0.57). Higher workplace SHS exposure was reported by participants who smoked five or more cigarettes per day compared with non-daily smokers (AOR = 2.16). No statistically significant associations were observed for time, city or their interaction with workplace SHS exposure, which was consistent with the stable levels of SHS exposure over time and across cities observed in Figure 1.
Restaurant SHS exposure
Logistic GEE models restricted to the 30% of Uruguayans who visited a restaurant in the previous month (n = 962) show males and participants with relatively higher education and lower income were less likely to report restaurant SHS exposure (Table 3). Consistent with the stable prevalence of restaurant SHS exposure observed in Figure 1, no statistically significant effects were found for time, city or their interaction.
Table 3.
Correlates of SHS exposure in last visit to restaurant, amongst participants who went to a restaurant in the previous month (Mexico and Uruguay, 2008 and 2010)
| Characteristics | Mexico |
Uruguay |
||||
|---|---|---|---|---|---|---|
| % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | |
| Sex | ||||||
| Female | 19 | 1 | 1 | 4 | 1 | 1 |
| Male | 21 | 1.18 (0.80–1.75) | 1.07 (0.72–1.58) | 9 | 2.66 (1.24–5.68)** | 2.41 (1.01–5.75)* |
| Age | ||||||
| 18–24 | 29 | 1 | 1 | 5 | 1 | 1 |
| 25–39 | 17 | 0.54 (0.32–0.88)* | 0.62 (0.38–1.01) | 8 | 1.92 (0.81–4.59) | 2.16 (0.82–5.71) |
| 40–54 | 20 | 0.65 (0.39–1.10) | 0.68 (0.39–1.17) | 7 | 1.51 (0.59–3.84) | 1.66 (0.57–4.82) |
| 55 or more | 12 | 0.34 (0.16–0.73)** | 0.36 (0.16–0.85)* | 6 | 1.38 (0.42–4.56) | 1.25 (0.34–4.63) |
| Education | ||||||
| <Middle school | 16 | 1 | 1 | 14 | 1 | 1 |
| Middle school | 20 | 1.32 (0.70–2.48) | 1.17 (0.59–2.3) | 4 | 0.33 (0.10–1.08) | 0.27 (0.09–0.76)* |
| High School | 21 | 1.42 (0.77–2.63) | 1.02 (0.53–1.99) | 10 | 0.91 (0.30–2.82) | 0.71 (0.26–1.94) |
| >High School | 23 | 1.55 (0.83–2.88) | 1.03 (0.51–2.06) | 4 | 0.32 (0.10–0.99)* | 0.30 (0.10–0.96)* |
| Income | ||||||
| Low | 17 | 1 | 1 | 1 | 1 | 1 |
| Middle–low | 16 | 0.89 (0.46–1.73) | 0.89 (0.46–1.72) | 9 | 18.79 (1.25–281.4)* | 12.54 (1.42–110.6)* |
| Midde–high | 20 | 1.20 (0.65–2.21) | 1.21 (0.64–2.30) | 6 | 12.95 (0.99–168.9)* | 11.39 (1.36–95.41)* |
| High | 24 | 1.57 (0.85–2.89) | 1.67 (0.88–3.18) | 6 | 13.19 (1.05–165.2)* | 13.44 (1.66–108.71)* |
| Missing | 25 | 1.55 (0.74–3.22) | 1.25 (0.55–2.85) | 9 | 21.08 (1.39–319.6)* | 19.08 (2.07–176.1)*** |
| Smoking behaviour | ||||||
| Non-daily smoker | 21 | 1 | 1 | 5 | 1 | 1 |
| Low daily consumption | 21 | 1.00 (0.64–1.57) | 1.12 (0.71–1.76) | 7 | 1.34 (0.40–4.44) | 1.29 (0.37–4.56) |
| High daily consumption | 20 | 0.95 (0.54–1.68) | 1.08 (0.63–1.87) | 6 | 1.09 (0.41–2.92) | 0.89 (0.30–2.67) |
| Quitter | 16 | 0.61 (0.30–1.22) | 0.99 (0.48–2.02) | 9 | 2.12 (0.66–6.85) | 2.71 (0.72–10.18) |
| Year | ||||||
| 2008 | 28 | 1 | 1 | 7 | 1 | 1 |
| 2010 | 14 | 0.45 (0.30–0.66)*** | 0.45 (0.29–0.68)*** | 7 | 1.02 (0.54–1.93) | 0.86 (0.42–1.76) |
| Residence | ||||||
| Capital city | 7 | 1 | 1 | 6 | 1 | 1 |
| Other cities | 25 | 4.45 (2.58–7.66)*** | 3.89 (2.25–6.71)*** | 8 | 1.36 (0.67–2.76) | 1.25 (0.58–2.7) |
aAdjusted ORs control for all variables shown in the table.
*P < 0.05; **P < 0.01; ***P < 0.001.
In the Mexico sample, 27% went to a restaurant in the previous month. SHS exposure in restaurants was reported less frequently by the oldest compared with the youngest participants (AOR = 0.36), and more frequently in other Mexican cities than in Mexico City (AOR = 3.89). Although model results indicated an overall decrease in SHS exposure from 2008 to 2010 (AOR = 0.45), a statistically significant interaction between time and city was found (AOR = 0.21; P < 0.001; model results not shown). SHS prevalence in restaurants was stable over time in Mexico City (range 5–7%), whereas in other Mexican cities, SHS prevalence was significantly higher and decreased significantly from 2008 to 2010 (32–17%; P < 0.01; see Figure 1).
Bar SHS exposure
In 2008 and 2010, 26% and 22% of the Uruguayan study sample, respectively, went to a bar in the previous month. GEE models for Uruguay (see Table 4) indicated that bar SHS exposure was more likely among males compared with females (AOR = 2.95), and less likely among participants with high compared to low educational attainment (AOR = 0.25) and with high compared to low income (AOR = 0.26). Likelihood of bar SHS exposure was also higher in other cities compared with Montevideo (AOR = 2.84; see Figure 1). The interaction between city and time was not statistically significant.
Table 4.
Correlates of SHS exposure in last visit to a bar, amongst participants who went to a restaurant in the previous month (Mexico and Uruguay, 2008 and 2010)
| Characteristics | Mexico |
Uruguay |
||||
|---|---|---|---|---|---|---|
| % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | % exposed to ETS | Bivariate OR [95% CI] | Adjusteda OR [95% CI] | |
| Sex | ||||||
| Female | 61 | 1 | 1 | 7 | 1 | 1 |
| Male | 70 | 1.67 (1.11–2.51)* | 1.68 (1.07–2.63)* | 22 | 3.30 (1.02–10.75)* | 2.95 (1.31–6.65)*** |
| Age | ||||||
| 18–24 | 76 | 1 | 1 | 13 | 1 | 1 |
| 25–39 | 61 | 0.50 (0.32–0.80)** | 0.59 (0.37–0.94)* | 20 | 2.28 (1.00–5.17)* | 2.30 (0.98–5.42) |
| 40–54 | 60 | 0.48 (0.28–0.84)* | 0.45 (0.24–0.85)* | 12 | 1.03 (0.44–2.40) | 1.07 (0.40–2.83) |
| 55 or more | 68 | 0.64 (0.26–1.58) | 0.46 (0.20–1.04) | 17 | 1.99 (0.76–5.20) | 1.31 (0.42–4.11) |
| Education | ||||||
| <Middle school | 72 | 1 | 1 | 28 | 1 | 1 |
| Middle school | 65 | 0.72 (0.33–1.56) | 0.70 (0.32–1.56) | 15 | 0.46 (0.17–1.21) | 0.39 (0.13–1.15) |
| High School | 65 | 0.82 (0.38–1.73) | 0.68 (0.30–1.52) | 21 | 0.68 (0.24–1.89) | 0.57 (0.19–1.68) |
| >High School | 71 | 0.96 (0.45–2.07) | 0.74 (0.33–1.67) | 5 | 0.16 (0.05–0.47)*** | 0.25 (0.07–0.90)* |
| Income | ||||||
| Low | 63 | 1 | 1 | 40 | 1 | 1 |
| Middle–low | 58 | 1.03 (0.58–1.82) | 1.44 (0.77–2.69) | 17 | 0.29 (0.07–1.20) | 0.24 (0.05–1.11) |
| Midde–high | 73 | 1.56 (0.83–2.93) | 1.83 (0.90–3.75) | 3 | 0.45 (0.12–1.60) | 0.46 (0.12–1.77) |
| High | 70 | 1.62 (0.92–2.85) | 1.80 (0.97–3.36) | 10 | 0.19 (0.05–0.72)* | 0.26 (0.07–1.01) |
| Missing | 70 | 1.62 (0.70–3.75) | 1.54 (0.66–3.62) | 9 | 0.23 (0.05–0.95)* | 0.21 (0.04–0.98)* |
| Smoking behaviour | ||||||
| Non-daily smoker | 66 | 1 | 1 | 23 | 1 | 1 |
| Low daily consumption | 69 | 1.07 (0.66–1.72) | 1.16 (0.71–1.91) | 9 | 0.47 (0.18–1.25) | 0.20 (0.06–0.67) |
| High daily consumption | 70 | 1.10 (0.70–2.04) | 1.21 (0.68–2.15) | 17 | 0.78 (0.30–2.03) | 0.50 (0.20–1.22) |
| Quitter | 55 | 0.62 (0.28–1.35) | 0.63 (0.26–1.55) | 12 | 0.65 (0.22–1.92) | 0.50 (0.14–1.78) |
| Year | ||||||
| 2008 | 73 | 1 | 1 | 17 | 1 | 1 |
| 2010 | 60 | 0.57 (0.38–0.83)** | 0.50 (0.32–0.77)** | 15 | 0.88 (0.53–1.46) | 0.93 (0.52–1.68) |
| Residence | ||||||
| Capital city | 28 | 1 | 1 | 11 | 1 | 1 |
| Other cities | 78 | 8.12 (5.24–12.58)*** | 8.28 (5.20–13.18)*** | 30 | 3.21 (1.60–6.41)*** | 2.84 (1.49–5.4)*** |
aAdjusted ORs control for all variables shown in the table.
*P < 0.05; **P < 0.01; ***P < 0.001.
In Mexico, 21% of participants in 2008 and 18% of participants in 2010 went to a bar in the month prior to the survey. Males were more likely than females to report SHS exposure (AOR = 1.68) and older participants were less likely than youngest participants to report exposure (AOR25–39 vs 18–24 years old = 0.57; AOR40–54 vs 18–24 years old = 0.57). SHS exposure decreased over time (AOR = 0.50) and was higher in other cities compared with Mexico City (AOR = 8.28). The interaction between city and time was not statistically significant. Nevertheless, Figure 1 shows that the decrease in SHS exposure in other cities was statistically significant (86–74%; P < 0.001), whereas it was not for Mexico City (31–23%).
Discussion
The results from this study are consistent with other research showing that comprehensive smoke-free policies are more effective in reducing SHS exposure than weaker policies that allow for exceptions, whether exposure is based on self-report (Borland et al. 2006; Haw and Gruer 2007; Thrasher et al. 2010a), air monitoring methods (Navas-Acien et al. 2004; Connolly et al. 2009; Blanco-Marquizo et al. 2010; Callinan et al. 2010; Erazo et al. 2010; Schoj et al. 2010; Semple et al. 2010; Barnoya et al. 2011; Gotz et al. 2011; Nafees et al. 2011; López et al. 2012) or interviews with key informants (WHO 2009). In our study, this pattern was most evident for restaurants, where reported SHS exposure was generally stable and low across Uruguay (6–9%) and in Mexico City (5–7%), where comprehensive policies were implemented. These estimates were significantly lower than SHS exposure in other Mexican cities, where DSAs were allowed (32% in 2008, 17% in 2010).
Our assessment of SHS exposure in bars showed a similar pattern within and across countries, although SHS exposure was higher than for restaurants across all jurisdictions. Bar SHS exposure declined in other Mexico Cities over this time, although it did not reach levels observed in the comprehensive smoke-free jurisdictions. Overall, it appears that the complexity and difficulty of implementing DSA regulations under the Mexican Law may account for reduced SHS exposure in public venues, but as in Chile (Erazo et al. 2010) and in Spain under its 2006 Law (López et al. 2012), DSAs have not been as effective as comprehensive policies that do not allow smoking inside.
Compared to SHS exposure in the hospitality industry, we found less within-and between-country variation in workplace SHS exposure, where monitoring may be more difficult than for restaurants and bars. About one quarter of participants reported SHS exposure at work, which is consistent with results from the Global Adult Tobacco Survey in both countries (MSP 2009; INSP 2010). This level is notably higher than what has been reported in high-income countries with comprehensive smoke-free laws (2–8% during post-law periods) (Edwards et al. 2008; Lee et al. 2011). Future research should determine which workplace types most often violate smoke-free laws to inform the development of interventions to reduce non-compliance.
Overall, results reflect a significant degree of non-compliance in bars and workplaces, and, less so, in restaurants. Non-compliance appeared higher in Uruguay and Mexico than in high-income countries when considering restaurants (2.5–5.5%) (Borland et al. 2006; Cooper et al. 2010) or bars (7.2–9.0%) (Cooper et al. 2010). According to the WHO, of 17 countries implementing comprehensive smoke-free policies by 2009, only six reported high compliance (WHO 2009). Reports of high compliance were more prevalent in high-income than middle-income countries, and one of these high compliance countries was Uruguay. However, the WHO report relied on stakeholder interviews, and our population-based representative data that includes small cities suggest that compliance may not be as high as originally reported. Indeed, private workplace SHS exposure is particularly difficult for stakeholders to monitor. Additional efforts will likely be necessary to augment compliance in workplaces and bars in both Uruguay and Mexico, which may require greater sanctions for violators, more frequent inspections and educational campaigns to raise awareness of the issue (WHO 2007, 2009; Villalobos et al. 2010; Thrasher et al. 2011).
Sociodemographic characteristics rather than smoking behaviours were most consistently related to SHS exposure in regulated venues. In Uruguay, SHS exposure was higher among males than females across all venues, and, for restaurants and bars, it was associated with having relatively low educational attainment. Therefore, comprehensive smoke-free policy implementation in Uruguay has been relatively less successful in venues frequently visited by males and lower SES groups, and the health benefits of smoke-free policy may be less likely to accrue to these sub-populations unless something is done to enhance compliance.
In Mexico, younger participants were more likely to report SHS exposure across all venues. Other statistically significant correlates of exposure varied across venues examined, with males slightly more likely to be exposed to SHS in bars and those who smoked most frequently reporting higher SHS exposure at their workplaces than non-daily smokers. The fact that SHS exposure did not differ by income or education is noteworthy and consistent with what was found in New Zealand (Edwards et al. 2008). Nevertheless, the consistency of higher SHS exposure amongst younger participants suggests the importance of addressing this issue in this population not only to enhance compliance but also to ensure that norms regarding non-compliance do not spread to the next generation and propagate over time.
This study has a number of potential limitations. Smokers may under-report SHS exposures if they do not feel comfortable revealing law-breaking behaviour. To address this issue, our questions asked whether ‘anyone’ smoked inside at the last visit, not whether the participant smoked. Nevertheless, this may not have entirely overcome social desirability effects. Furthermore, we asked only about SHS at the last visit, and survey questions and air monitoring that involve longer time frames are likely to produce higher estimates of SHS exposure. On the other hand, smokers who break the law may selectively go to restaurants and bars where they know people will smoke, and which are not representative of these venues. Although we did not survey non-smokers to assess the extent of this bias, our results suggest a tendency for quitters to report somewhat lower levels of SHS exposure than heavy smokers, at least in Mexico; hence, we may have overestimated non-compliance. The extent of bias and lack of generalizability from smokers’ reports of SHS requires further research, including cross-validation studies using self-reports of non-smokers and more objective air monitoring measures. Whatever the self-report biases or issues with external validity, asking the same question at both waves allows for greater confidence regarding assessment of changes in SHS exposure over time.
Conclusions
This study provides the first population-based, prospective data on SHS exposure over the period after implementation of smoke-free policies in middle-income countries in Latin America. Beyond confirming that comprehensive smoke-free legislation is most effective for reducing SHS exposure, this study provides critical evidence regarding SHS in private workplaces that often elude surveillance efforts, suggesting difficulties in compliance there and in bars, even when legislation is comprehensive. New enforcement efforts are needed to enhance compliance and ensure the equitable impact of smoke-free policy, especially in the Latin American region, whereas of May 2012, 12 countries have adopted comprehensive smoke-free policies at the national level (Sebrié et al. 2012b).
Funding
Funding for data collection and analyses on this study came from the Mexican Consejo Nacional de Ciencia y Tecnología (Salud-2007-C01-70032), with additional funding for analysis provided by the National Cancer Institute at the National Institutes of Health (P01 CA138389) and the Flight Attendant Medical Research Institute (FAMRI to Sebrie).
Conflict of interest
None declared.
References
- Ley General para el Control del Tabaco. 2008. Cámara de Senadores de los Estados Unidos Mexicanos 198. Distrito Federal, México: Gaceta Oficial del Senado de la República, 115–23.
- Reglamento de la Ley General para el Control del Tabaco. 2009. Secretaría de Salud. Distrito Federal, México: Diario Oficial de la Federación.
- Barnoya J, Arvizu M, Jones M, et al. Secondhand smoke exposure in bars and restaurants in Guatemala City: before and after smoking ban evaluation. Cancer Causes & Control. 2011;22:151–6. doi: 10.1007/s10552-010-9673-8. [DOI] [PubMed] [Google Scholar]
- Blanco-Marquizo A, Goja B, Peruga A, et al. Reduction of secondhand tobacco smoke in public places following national smoke-free legislation in Uruguay. Tobacco Control. 2010;19:231–4. doi: 10.1136/tc.2009.034769. [DOI] [PubMed] [Google Scholar]
- Borland R, Yong H-H, Siapush M, et al. Support for and reported compliance with smoke-free restaurants and bars in four countries: findings from the International Tobacco Control Four Country Survey. Tobacco Control. 2006;15:iii34–41. doi: 10.1136/tc.2004.008748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan J, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database of Systematic Review. 2010 doi: 10.1002/14651858.CD005992.pub2. 14:CD005992. [DOI] [PubMed] [Google Scholar]
- Connolly G, Carpenter C, Travers M, et al. How smoke-free laws improve air quality: a global study of Irish pubs. Nicotine & Tobacco Research. 2009;11:600–5. doi: 10.1093/ntr/ntp038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J, Borland R, Yong H, Hyland A. Compliance and support for bans on smoking in licensed venues in Australia: findings from the International Tobacco Control Four-Country Survey. Australian and New Zealand Journal of Public Health. 2010;34:379–85. doi: 10.1111/j.1753-6405.2010.00570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards R, Thomson G, Wilson N, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tobacco Control. 2008;17:1–10. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- Erazo M, Iglesias V, Droppelmann A, et al. Secondhand tobacco smoke in bars and restaurants in Santiago, Chile: evaluation of partial smoking ban legislation in public places. Tobacco Control. 2010;19:469–74. doi: 10.1136/tc.2009.035402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong GT, Hyland A, Borland R, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK survey. Tobacco Control. 2006;15:iii51–8. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotz N, van Tongeren M, Wareing H, et al. Changes in air quality and second-hand smoke exposure in hospitality sector businesses after introduction of the English Smoke-free legislation. Journal of Public Health. 2011;30:421–8. doi: 10.1093/pubmed/fdn062. [DOI] [PubMed] [Google Scholar]
- Guerrero-López C, Muños-Hernández J, Reynales-Shigematsu L. Reduction in Hospitalizations due to Acute Myocardial Infarction and Cerebrovascular Disease after a Smoke-free Law in Mexico City. World Conference on Tobacco or Health. Singapore: 2012. [Google Scholar]
- Guillermo-Tenorio X. Expacios 100% libres de humo: una realidad del Distrito Federal. Salud Pública de México. 2008;50:S384–90. doi: 10.1590/s0036-36342008000900016. [DOI] [PubMed] [Google Scholar]
- Hardin J, Hilbe J. Generalized Estimating Equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross-sectional survey. BMJ. 2007;335:549–52. doi: 10.1136/bmj.39315.670208.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INSP. Encuesta Mundial de Tabaquismo en Adultos, México 2009 [Global Adult Tobacco Survey, México 2009] Cuernavaca, México: Instituto Nacional de Salud Pública & PanAmerican Health Organization; 2010. [Google Scholar]
- ITC Project. Smoke-free Policies: ITC Cross-country Comparison Report. Waterloo, Ontario, Canada: University of Waterloo; 2012. [Google Scholar]
- Korn EL, Graubard BI. Analysis of Health Surveys. New York: Wiley-Interscience; 1999. [Google Scholar]
- Lee J, Glantz S, Millett C. Effect of smoke-free legislation on adult smoking behaviour in England in the 18 months following implementation. PLoS One. 2011;6:e2093. doi: 10.1371/journal.pone.0020933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López M, Nebot M, Schiaffino A, et al. Two-year impact of the Spanish smoking law on exposure to secondhand smoke: evidence of the failure of the ‘Spanish model’. Tobacco Control. 2012;21:407–11. doi: 10.1136/tc.2010.042275. [DOI] [PubMed] [Google Scholar]
- Ma J, Apelberg B, Avila-Tang E, et al. Workplace smoking restrictions in China: results from a six county survey. Tobacco Control. 2010;19:403–9. doi: 10.1136/tc.2009.034207. [DOI] [PubMed] [Google Scholar]
- MSP. Global Adults Tobacco Survey Uruguay (GATS)—Fact Sheet Uruguay 2009. Montevideo, Uruguay: Ministerio de Salud Pública; 2009. [Google Scholar]
- Muños-Hernández J, Guerrero-López C, Reynales-Shigematsu LM. A Decline in Mortality from Acute Myocardial Infarction, Cerebrovascular Disease and Asthma, due to the Implementation of the Non-Smokers Health Protection Law in Mexico City, World Conference on Tobacco or Health. Singapore: 2012. [Google Scholar]
- Nafees A, Taj T, Kadir M, et al. Indoor air pollution (PM2.5) due to secondhand smoke in selected hospitality and entertainment venues of Karachi, Pakistan. Tobacco Control. 2012 doi: 10.1136/tc.2011.043190. 21(5): 460–4. [DOI] [PubMed] [Google Scholar]
- Nagelhout G, Mons U, Allwright S, et al. Prevalence and predictors of smoking in “smoke-free” bars: Findings from the International Tobacco Control (ITC) Europe Surveys. Social Science and Medicine. 2011;72:1643–51. doi: 10.1016/j.socscimed.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navas-Acien A, Peruga A, Breysse P, et al. Secondhand tobacco smoke in public places in Latin America, 2002-2003. JAMA. 2004;291:2741–5. doi: 10.1001/jama.291.22.2741. [DOI] [PubMed] [Google Scholar]
- Reis M, Precioso J, Rebelo L, Carrota R, Aguilar P. First exploratory descriptive study on adherence to and compliance with the Portuguese smoke-free law in the leisure-hospitality sector. Tobacco Control. 2010;19:171–2. doi: 10.1136/tc.2008.028720. [DOI] [PubMed] [Google Scholar]
- Schoj V, Sebrié E, Pizarro M, Hyland A, Travers M. Informing effective smokefree policies in Argentina: air quality monitoring study in 15 cities (2007–2009) Salud Pública de México. 2010;52:157–67. doi: 10.1590/s0036-36342010000800011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebrié E, Sandoya E, Hyland E, et al. Hospital admissions for acute myocardial infarction before and after implementation of a comprehensive smoke-free policy in Uruguay. Tobacco Control. 2012a doi: 10.1136/tobaccocontrol-2011-050134. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebrié E, Schoj V, Travers MJ, McGraw B, Glantz S. Smokefree policies in Latin America and the Caribbean: making progress. International Journal of Environmental Research & Public Health. 2012b;9(5):1954–70. doi: 10.3390/ijerph9051954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple S, van Tongeren M, Galea K, et al. UK smoke-free legislation: changes in PM2.5 concentrations in bars in Scotland, England, and Wales. Annals of Occupational Hygiene. 2010;54:272–80. doi: 10.1093/annhyg/mep094. [DOI] [PubMed] [Google Scholar]
- Skeer M, Land ML, Cheng DM, Siegel MB. Smoking in Boston bars before and after a 100% smoke-free regulation: An assessment of early compliance. Journal of Public Health Management and Practice. 2004;10:501–7. doi: 10.1097/00124784-200411000-00005. [DOI] [PubMed] [Google Scholar]
- Thrasher J, Swayampakala K, Arillo-Santillán E, et al. Differential impact of local and federal smoke-free legislation in Mexico: a longitudinal study of campaign exposure, support for smoke-free policies and secondhand smoke exposure among adult smokers. Salud Pública de México. 2010a;52:S244–253. doi: 10.1590/s0036-36342010000800020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Boado M, Sebrié EM, Bianco E. Smoke-free policies and the social acceptability of smoking in Uruguay and Mexico: findings from the International Tobacco Control Policy Evaluation (ITC) Project. Nicotine & Tobacco Research. 2009;11:591–9. doi: 10.1093/ntr/ntp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Huang L, Pérez-Hernández R, et al. Evaluation of a social marketing campaign to support Mexico City’s comprehensive smoke-free law. American Journal of Public Health. 2011;101:328–35. doi: 10.2105/AJPH.2009.189704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Pérez-Hernández R, Swayampakala K, Arillo-Santillan E, Bottai M. Policy support, norms, and secondhand smoke exposure before and after implementation of a comprehensive smoke-free policy in Mexico City. American Journal of Public Health. 2010b;100:1079–96. doi: 10.2105/AJPH.2009.180950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villalobos V, Ortiz-Ramirez O, Thrasher JF, et al. Mercadotecnia social y políticas públicas de salud: Campaña para promover espacios libres de humo de tabaco en México [Social marketing and public health policy: development of a campaign to promote smoke-free policy in Mexico] Salud Pública de México. 2010;52:S129–37. [PubMed] [Google Scholar]
- WHO. Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization, Tobacco Free Initiative; 2003. [Google Scholar]
- WHO. Guidelines for implementation of the Framework Convention on Tobacco Control—Article 8: Protection from exposure to tobacco smoke. Conference of the Parties, World Health Organization, Framework Convention on Tobacco Control. 2007. [Google Scholar]
- WHO. WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-free Environments. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- WHO. WHO Report on the Global Tobacco Epidemic, 2011. Tobacco Free Initiative. Geneva: World Health Organization; 2011. [Google Scholar]
- Yong H-H, Foong K, Borland R, et al. Support for and reported compliance among smokers with smoke-free policies in air-conditioned hospitality venues in Malaysia and Thailand: findings from the International Tobacco Control Southeast Asia Survey. Asia-Pacific Journal of Public Health. 2010;22:98–109. doi: 10.1177/1010539509351303. [DOI] [PMC free article] [PubMed] [Google Scholar]