Abstract
We sought to determine the optimal placement and screw length for C2 pedicle screw fixation to compare with recommendations in literature. Nine patients were included in this study and underwent C2 pedicle instrumentation either for a hangman's fracture as part of C2 pedicle–C3 lateral mass fixation or for C2–C3 subluxation. All nine patients had good postoperative improvement with satisfactory fracture consolidation. Mediolateral and rostrocaudal angulations of the inserted screws were not consistent with the traditional angulations of 20 degrees in each plane due to the fracture lines and the anatomical variations. Because the frequent observation of the bony anatomical variations and the lines of fractures brought about by trauma, a shift from the classic 20 degrees of angulation in both trajectories has been concluded. But still fixed angles of angulations cannot be generalized. As a consequence, accurate preoperative planning can be obtained by computed tomography with three-dimensional images so that it gives the surgeon a good prediction of the best length of utilized screws in the procedure and the best angulations for safety of the neighboring neurovascular structures.
Keywords: hangman's fracture, C2 pedicle screw
Axis traumatic spondylolisthesis (ATS) and hangman's fracture are terms that describe a specific fracture group, which involves the posterior C2 elements.1 Wood-Jones first described a C2 vertebra fracture in 1913. He described fractures produced by hanging a person, and he observed that the lesion was produced by a violent cervical traction with abrupt stretching of the head backward, leading to C2 pedicle fractures.1 Later in 1964, Garber described C2 pedicle fractures with a forward dislocation of the C2 body in victims of motor vehicle accidents, called axis' traumatic spondylolisthesis.2
In 1965, Schneider et al described another series of patients with the same fractures, naming them “hangman's fracture.”3 The ATS was referred to as an uncommon and predominantly stable lesion, rarely accompanied by neurologic deficit, for which the recommended treatment was cervical traction and rigid immobilization.2 3
The surgical management of occipitocervical instability has evolved in the past two decades due to advances in instrumentation materials and a better understanding of spinal biomechanics, and imaging. Before the use of rigid internal fixation, all attempts to stabilize this segment of the spine required supplemental external fixation.4 5 Although Leconte was the first to describe the use of C2 pedicle screws in the management of traumatic spondylolisthesis in 1964,6 it was not until 20 years later that Borne et al published the first series of patients treated with this technique.7 Borne et al's work demonstrated excellent results using the C2 pedicle as an anchor for internal stabilization of occipitocervical instability. The technique did not gain widespread attention until Roy-Camille et al reported its use in the treatment of C2-related instability in 1989 and again in 1991.8 9 Moreover, the increasing popularity of lateral mass plating led to incorporation of the C2 pedicle in these constructs for both traumatic and non-traumatic occipitocervical instability. Since then, several anatomical studies of the C2 were addressed to establish guidelines for the placement of pedicle screws.10 11 However, adherence to such algorithmic approaches failed to account for individual variations and too often resulted in cortical breach of the pedicle. As no two patients are identical, a surgeon must have a full comprehension of each patient's anatomy. Such knowledge allows the surgeon to use the C2 pedicle as an anchor in occipitocervical stabilization with minimal risk of damage to neurovascular structures.
The following case series reports our experience at a single center in treating patients with ATS, with or without C2–C3 subluxation, and reporting of our surgical technique in determining optimal C2 pedicle screw placement.
Patients and Methods
From June 2008 to April 2010, nine patients with ATS with or without C2–3 subluxation were operated. All patients were admitted and operated at Dr. Soliman Fakeeh Hospital, Jeddah, Saudi Arabia. There were eight males and one female, with a mean age of 35.7 years. Eight patients had a motor vehicle accident and one fell from second floor into the street. Two patients had previous conservative treatment and showed signs of pseudarthrosis at the fracture site, with intense pain at the cervical spine region. Three patients had head injury, two of them with multiple cranial fractures and the third was submitted for surgical treatment for a ruptured cervical disc. Three patients had dislocation of C2–C3, which was not satisfactorily reduced with conservative treatment. None of the patients showed neurologic deficit.
Procedure
All of the patients had plain radiographs, computed tomography (CT) of the cervical spine, and magnetic resonance imaging, confirming the C2 pedicle fracture diagnosis with possible C2–C3 subluxation, without compromising the vertebral canal. In cases of pseudarthrosis after conservative treatment, dynamic plain radiographs of the cervical spine (bending and stretching) were also performed aiming to confirm a flaw in the fracture's union. All patients were operated by the same surgeon. C2 pedicle screw trajectories were measured on CT (Siemens, Munich, Germany).
Surgical Technique
All patients underwent C2 pedicle arthrodesis, with a pedicle screw fixation crossing the fracture lines (a technique described by Leconte).6 Each patient was placed in the prone position with the head fixed by a Mayfield-type support, keeping the best possible cranioatlantoaxial alignment. Fluoroscopic imaging was available throughout the case and images were obtained whenever necessary to assess the bony anatomy, specially the C2 pedicles and body. An approximate 8-cm posterior midline cervical incision from the craniocervical junction downward was made providing adequate exposure for the surgeon to angulate his instruments during the rostrocaudal inclination and exposing the entry site of the C2 pedicles. The C2 articular masses were exposed and the paravertebral muscles were detached. Two centralized holes were made with a drill connected to a light drilling machine or to a high-speed motor, one in each articular mass. The drilling then proceeded toward the C2 vertebral body, maintaining an inclination consistent with what has been obtained from the three-dimensional (3D) CT images. Traditionally screw angulation of the screw insertion is ~20 degrees in the axial plane and 20 degrees in the sagittal plane (Fig. 1). However, in our cases, the preoperative CT scans noted greater distortions by the fracture line(s) and variations in the local anatomy (e.g., enlarged foramen transversarium; Fig. 2). As such, this indicated that screw insertion would necessitate a greater degree of angulation. Hence, we corrected our angulations from the traditional method of 20 degrees to the expected degrees indicated in the preoperative scan. These inclinations were controlled by continuous plain radiographic imaging to keep the drill strictly within the C2 pedicles. In each of these trajectories, guide wires were inserted. These wires guided the two 3.5-mm-diameter cannulated screws, with the thread only at the end (partial thread screws). At times, overdrilling the proximal bony segment obviates the possibility of using such screws and hence a fully threaded screw is then used. Correction and fracture fixation are better obtained when two screws are fixed simultaneously, pulling the C2 vertebral body toward the fractured pedicles. In cases where C2–C3 reduction appears more difficult, a lateral mass plate can be added connecting the C2 pedicle screws to the two lateral masses on each side of the C3 as described by Roy-Camille et al.9 In our series, lateral mass screws were inserted at C3 for a better fracture reduction, if possible.
Fig. 1.
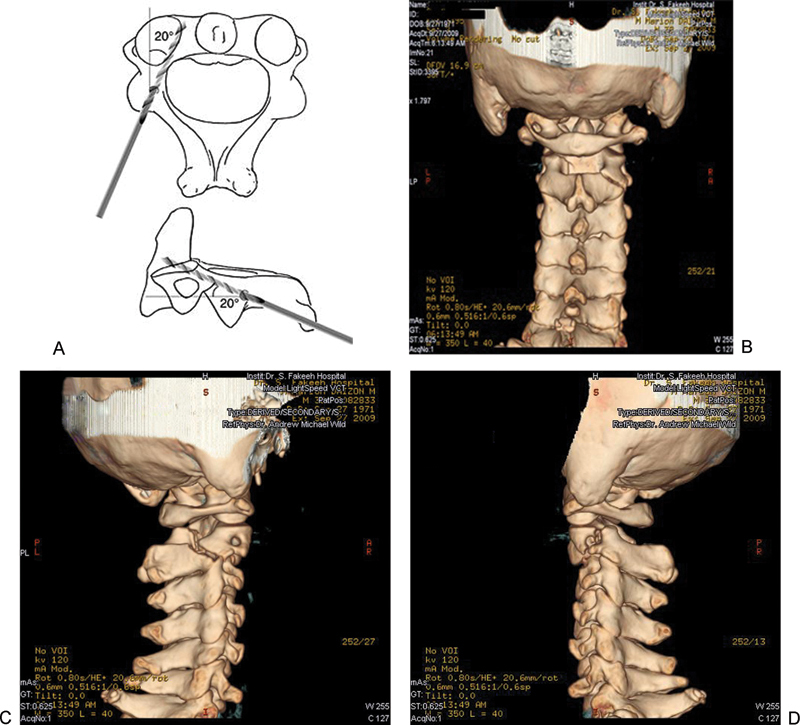
(A) The classic angles of angulation, both mediolateral and craniocaudal. (B, C, D) Preoperative three-dimensional computed tomography scans showing the fracture line in both pedicles; note the left one is traversing the foramen transversarium and the right is in the lamina.
Fig. 2.
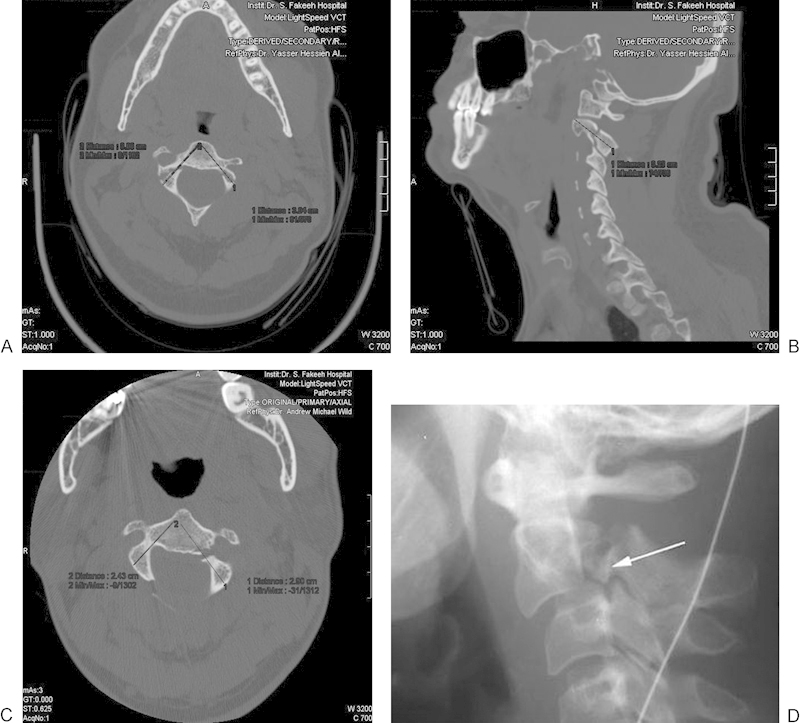
(A) Preoperative sagittal computed tomography scan showing the fracture line and the proposed line of screw insertion with the predicted length. (B, C) Axial cuts showing the proposed screw length with inequality of both screws due to anatomical-pathologic variations in both sides. (D) Preoperative plain radiograph of the cervical spine showing C2–C3 subluxation due to fracture at the C2 pars (thin arrow), and the C2–C3 dislocation (thick arrow).
Following surgery, all patients were placed in a semirigid cervical Philadelphia collar for a period of 2 weeks.
Follow-up
Postoperatively, each patient was clinically evaluated. Physical, neurologic, and radiologic exams were performed on follow-up visits.
Plain radiographs and CT were obtained postoperatively on day 2 and at 3 and 6 months to assess fusion and the integrity of the screw trajectories and length (Fig. 3).
Fig. 3.
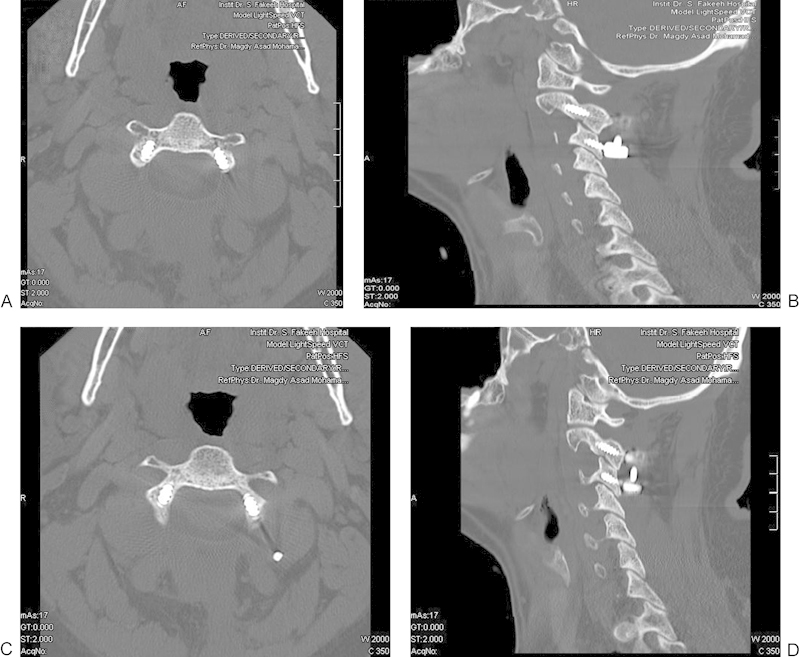
(A–D) Postoperative axial and parasagittal computed tomography scan showing good screw position and healing of the fracture. (Note: Fully threaded screws were used in this case due to overdrilling of the proximal bony segment.)
Results
The mean follow-up period was 6 months (range: 3 to 9 months). All nine patients had good postoperative improvement with satisfactory fracture consolidation and were asymptomatic on follow-up. There were no intra- or postoperative complications, except one patient who developed pneumonia on postoperative day 3, which resolved in 7 days with antibiotic treatment. The hospitalization period varied from 7 to 13 days. Only one patient developed frequent neck pain, especially after performing intense physical effort, which improved after rest, use of nonsteroidal analgesics, and simple physiotherapeutic remedies. On immediate plain radiographic evaluation, all patients showed satisfactory and correct alignment of fractured bony ends with C2–C3 reduction. Six months after surgery, all patients undertook a CT scan where good healing of the fractures with intact pedicle cortices.
There were a total of 18 pedicles inserted in all patients. The mean pedicle screw length was 16.5 mm (range: 16 to17 mm), and the mean medial and rostral inclinations measured were 34.7 degrees (range: 28 to 41degrees) and 38.6 degrees (range: 28 to 41 degrees), respectively (Table 1).
Table 1. Screw lengths and degrees of mediolateral and rostrocaudal angulations in all patients.
| Patient | Length (mm) | Mediolateral angle X (degrees) | Rostrocaudal angle Y (degrees) |
|---|---|---|---|
| 1 | 16/16 | 39/37 | 41/41 |
| 2 | 17/17 | 41/40 | 34/35 |
| 3 | 17/17 | 30/28 | 22/23 |
| 4 | 17/16 | 29/29 | 40/40 |
| 5 | 16/16 | 33/31 | 40/39 |
| 6 | 16/16 | 38/37 | 39/39 |
| 7 | 16/16 | 35/36 | 36/37 |
| 8 | 17/17 | 35/33 | 51/52 |
| 9 | 17/17 | 40/35 | 45/42 |
Discussion
The pedicle of C2 is the segment that joins the body with the posterior elements and not the portion located between the superior and inferior articulating processes.13 This part of the vertebra in the remainder of the spine is termed the pars interarticularis. However, the vast majority of the literature devoted to this topic labels it as the pedicle.
The average dimensions of the pedicles usually do not differ, with the exception of pedicle length. Previous anatomical reports defined the length as the distance from the posterior surface of the C2 inferior articulating process to the anterior surface of the body.10 11 14 15 Others tend to define it as the distance from the posterior surface of the inferior articulating process to the junction of the pedicle with the body.8 Such variation may account for shorter pedicle length in previous studies. As such, insertion of pedicle screws needs to account for potential variation in anatomy.
The use of screws with partial threads in the setting of C2 pedicle fractures has proven useful in patients with pseudarthrosis after failure of conservative treatment or with contraindication for the use of “halo vest,” such as for skull fractures, great scalp lacerations, or C2–C3 sublaxation.12 In the anatomical study of Xu et al,11 the average medial angulation of the pedicle was 30 degrees and the rostrocaudal inclination was 20 degrees cephalad to the transverse plane. They also reported that the proper screw entry point based on these angles was located at a point 5 mm inferior to the superior border of the C2 lamina and 7 mm lateral to the lateral border of the spinal canal. In an effort to test these values, in a later study, Ebraheim et al compared the screws placed using the above values with those placed using the superomedial border of the pedicle as a guide.17 They found a higher incidence of cortical breaching using the structured approach and recommended that C2 pedicle screws be placed using visualization of the pedicle.
In the anatomical study by Howington et al,16 screws were placed under direct visualization, and the angles as well as the distance to the entry point from structures routinely encountered at time of surgery were then measured. The average mediolateral angulation in their study measured 35.2 degrees, and the average rostrocaudal angulation measured 38.8 degrees. The mediolateral angulation differed slightly from the previous guideline, but the rostrocaudal inclination was almost twice that of the previous study. Such differences in angulation likely accounted for the increased incidence of cortical breaching in previous studies.
In our study, the average medial-lateral angulation was 35 degrees and was 38.6 degrees in the rostrocaudal plane. The average screw length was 16.5 mm, which was consistent with that of Howington et al's study16 but inconsistent with that mentioned in most textbooks as being 20 degrees of angulations in both planes, possibly due to the fracture line(s) with change in the local anatomy added to the individual anatomical variations. We chose the superomedial border of the pedicle as a guide for screw placement instead of a structured algorithmic approach that fails to take into account individual anatomical variations. We also relied on the preoperative 3D CT scans, which revealed anatomical variations and the fracture lines. As such, this allowed the surgeon to modulate the degrees of angulations bilaterally from various dimensions (rostrocaudal/mediolateral).
The structured method described by Xu et al revolves around the intersection of imaginary planes,11 which often contributes to poor screw placement and increased risk of neurovascular injury. Using the superomedial surface of the pedicle as a guide, one has an increased likelihood of locating the optimal entry point, but at times, the anatomy may be distorted. In such cases, one needs reliable aids in locating the entry site. By measuring distances between structures routinely encountered during surgery and the entry points, we were able to establish an almost standard set of guidelines. The average distance from the midline to the entry point in Xu et al's study was 26 mm, and the average distance from the C2–C3 joint line to the entry point was 9 mm. If the surgical dissection extends laterally to the medial aspect of the vertebral artery, then the surgeon may use that landmark as a guide. We found the average distance from that point to our entry site to be 14 mm. These values, like the ones set before by Xu et al, have the drawback of not taking into account individual variations and for that reason should not be used blindly.11 As a consequence to that, direct visualization of the superomedial border of the pedicle is needed to decide the entry point, and the proper preoperative surgical planning using 3D CT scan imaging for evaluating the best screw length and degrees of angulations is highly recommended for safety.
Various navigation systems are now available to aid pedicle screw placement. Navigation replaces fluoroscopy and generates 3D volumetric data set that may be viewed as axial, coronal, and sagittal images of the spine, similar CT. The data set can be downloaded for real-time intraoperative navigation.18 The use of this system was associated with a low rate of pedicle screw misalignment. The time for placing screws was less than what previously reported with CT navigation.18
Conclusion and Recommendations
There were many explicit limitations in our study, such as the small number of patients; the single-center, single-surgeon; retrospective design; very short follow-up (as short as 3 months); lack of standardized outcomes measures; and lack of standardized criteria to assess fusion status. Nonetheless, based on the frequent observations of the bony anatomical variations and the lines of fractures brought about by trauma, the classic 20-degree inclinations in both trajectories previously suggested should be reconsidered. However, fixed angles of angulations cannot be generalized. As a consequence, we conclude that accurate preoperative planning could be obtained with the use of 3D reconstructed CT images that can predict the best screw length needed for the procedure, depending on the size of the patient's axis vertebra, and the best angulations for the safety of the neighboring neurovascular structures. Hence, it is important to understand the patient's individual anatomy, as this is the ultimate guide to proper placement despite understanding the angles. Anatomical landmarks can therefore be well seen and demarcated through the use of intraoperative fluoroscopy or image-guided navigation techniques.
Footnotes
Disclosures Magdy Assaad El Hawary, None
References
- 1.Wood-Jones F. The ideal lesion produced by judicial hanging. Lancet. 1913;1:53–54. [Google Scholar]
- 2.Garber J N. Abnormalities of the atlas and axis vertebrae—congenital and traumatic. J Bone Joint Surg Am. 1964;46:1782–1791. [PubMed] [Google Scholar]
- 3.Schneider R C, Livingston K E, Cave A JE, Hamilton G. “Hangman's fracture” of the cervical spine. J Neurosurg. 1965;22:141–154. doi: 10.3171/jns.1965.22.2.0141. [DOI] [PubMed] [Google Scholar]
- 4.Apostolides P J, Dickman C A, Golfinos J G, Papadopoulos S M, Sonntag V K. Threaded Steinmann pin fusion of the craniovertebral junction. Spine (Phila Pa 1976) 1996;21:1630–1637. doi: 10.1097/00007632-199607150-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hamblen D L. Occipito-cervical fusion. Indications, technique and results. J Bone Joint Surg Br. 1967;49:33–45. [PubMed] [Google Scholar]
- 6.Leconte P. Paris, France: Masson et Cie; 1964. Fracture et luxation des deux premieres vertebres cervicales; pp. 147–166. [Google Scholar]
- 7.Borne G M, Bedou G L, Pinaudeau M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg. 1984;60:88–93. doi: 10.3171/jns.1984.60.1.0088. [DOI] [PubMed] [Google Scholar]
- 8.Roy-Camille R, Mazel C, Saillant G, Benazet J P. Philadelphia, PA: J.B. Lippincott Co.; 1991. Rationale and techniques of internal fixation in trauma of the cervical spine; pp. 163–169. [Google Scholar]
- 9.Roy-Camille R Saillant G Mazel C Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws In: The Cervical Spine Research Society, ed. The Cervical Spine 2nd ed. Philadelphia, PA: J.B. Lippincott Co.1989390–403. [Google Scholar]
- 10.Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine (Phila Pa 1976) 1999;24:1425–1434. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Xu R, Nadaud M C, Ebraheim N A, Yeasting R A. Morphology of the second cervical vertebra and the posterior projection of the C2 pedicle axis. Spine (Phila Pa 1976) 1995;20:259–263. doi: 10.1097/00007632-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Boullosa J L, Colli B O, Carlotti C G Jr, Tanaka K, dos Santos M B. Surgical management of axis' traumatic spondylolisthesis (Hangman's fracture) Arq Neuropsiquiatr. 2004;62(3B):821–826. doi: 10.1590/s0004-282x2004000500015. [DOI] [PubMed] [Google Scholar]
- 13.Benzel E C. Anatomic consideration of C2 pedicle screw placement. Spine (Phila Pa 1976) 1996;21:2301–2302. doi: 10.1097/00007632-199610010-00028. [DOI] [PubMed] [Google Scholar]
- 14.Karaikovic E E, Daubs M D, Madsen R W, Gaines R W Jr. Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976) 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 15.Panjabi M M, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine (Phila Pa 1976) 1991;16:861–869. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Howington J U Kruse J J Awasthi D Surgical anatomy of the C-2 pedicle J Neurosurg 200195(1, Suppl):88–92. [DOI] [PubMed] [Google Scholar]
- 17.Ebraheim N A, Rollins J R Jr, Xu R, Jackson W T. Anatomic consideration of C2 pedicle screw placement. Spine (Phila Pa 1976) 1996;21:691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 18.Patil S, Lindley E M, Burger E L, Yoshihara H, Patel V V. Pedicle screw placement with O-arm and stealth navigation. Orthopedics. 2012;35:e61–e65. doi: 10.3928/01477447-20111122-15. [DOI] [PubMed] [Google Scholar]


