Abstract
Objective:
To characterize the present state of brain death (BD) determination in actual practice relative to contemporary American Academy of Neurology (AAN) guidelines.
Methods:
We reviewed the charts of all adult (16 years and older) BD organ donors during 2011 from 68 heterogeneous hospitals in the Midwest United States. Data were collected across 5 categories: guideline performance, preclinical testing, clinical examination, apnea testing, and use of ancillary tests. Practice within categories and overall adherence to AAN guidelines were assessed.
Results:
Two hundred twenty-six BD organ donors were included. Practice exceeded recommendations in guideline performance but varied widely and deviated from AAN guidelines in all other categories. One hundred two (45.1%) had complete documentation of brainstem areflexia and absent motor response. One hundred sixty-six (73.5%) had completed apnea testing. Of the 60 without completed apnea testing, 56 (93.3%) had ancillary tests consistent with BD. Overall, 101 (44.7%) strictly and 84 (37.2%) loosely adhered to contemporary AAN guidelines.
Conclusions:
There is wide variability in the documentation of BD determination, likely reflecting similar variability in practice. This is a call for improved documentation, better uniformity of policies, and comprehensive and strategically targeted educational initiatives to ensure consistently contemporary approaches to BD determination in every patient.
In 1981, the Uniform Determination of Death Act defined brain death (BD) as the “irreversible cessation of all functions of the entire brain, including the brain stem” with the same legal and medical legitimacy as the traditional cardiopulmonary standard, but only asserted that the determination be made “in accordance with accepted medical standards.”1 Time has led to expanding awareness and acceptance of BD worldwide.2 The American Academy of Neurology (AAN) published and revised practice parameters in 1995 and 2010, respectively.3,4
It has been shown that official hospital policies for determining BD at top-rated neurology departments vary widely and often deviate from AAN guidelines in multiple domains of the process.5 The absence of clear and uniform expectations could hypothetically predispose to misdiagnosis or, conversely, deter unfamiliar physicians from pursuing the diagnosis altogether. Furthermore, the variability in official policies may perpetuate confusion about BD, create ambivalence about the importance of BD determination,6 and hinder the manner in which it is explained to grieving families.
The lack of uniformity among institutional policies does not necessarily reflect variability in approaches to BD determination in practice. To date, there is no systematic study that has scrutinized approaches to BD determination in actual practice.
Our study examined the approaches to BD determination in adults (16 years and older) at a cross-section of regional academic and nonacademic medical centers in the Midwestern United States to assess the uniformity in BD determination in practice and compare the diagnostic methods presently used with contemporary AAN guidelines.
METHODS
We retrospectively reviewed the charts of all adult BD organ donors in 2011 from 68 hospitals and medical centers in 2 states. Organ donors were chosen as our study population because of the uniformity of available medical records and the high standards for BD documentation required in organ donation cases.
Deidentified data were abstracted from medical records that included BD and preceding clinical notes, medication administration logs, and imaging reports, as well as Organ Procurement Organization–generated BD checklists. Select data relevant to several important aspects of BD determination were collected across 5 categories: guideline performance/physician specialty, preclinical testing, clinical examination, apnea testing, and ancillary testing. In the category of preclinical testing, core body temperature and serum sodium near the time of BD determination were chosen as sample indicators from the AAN list of potential examination confounders because of both their relevance and consistent availability in our dataset.
In the clinical examination category, the presumption was made that all patients had coma of known etiology and focus was placed instead on documentation of the appropriate clinical examination (absence of pupillary, oculocephalic, oculovestibular, corneal, gag, and cough reflexes, as well as motor response to pain) as outlined in the updated AAN guidelines. For the purposes of the study, facial and peripheral motor responses to pain were grouped together and documentation of either was accepted as satisfactory for that aspect of the examination. Therefore, a complete clinical examination had 7 features instead of 8 as in AAN guidelines. Reflexes were considered “redundant” if they tested similar parts of brainstem function (i.e., oculovestibular and oculocephalic; gag and cough).
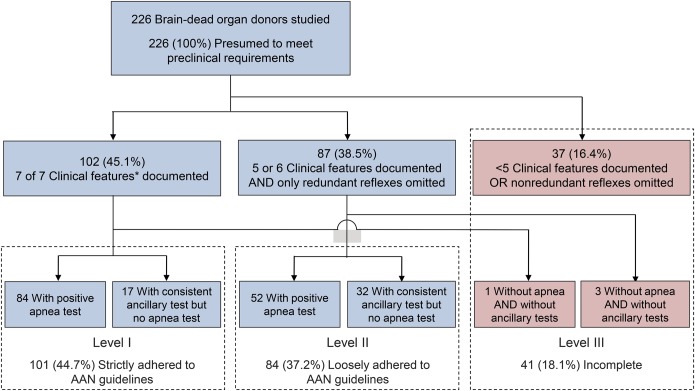
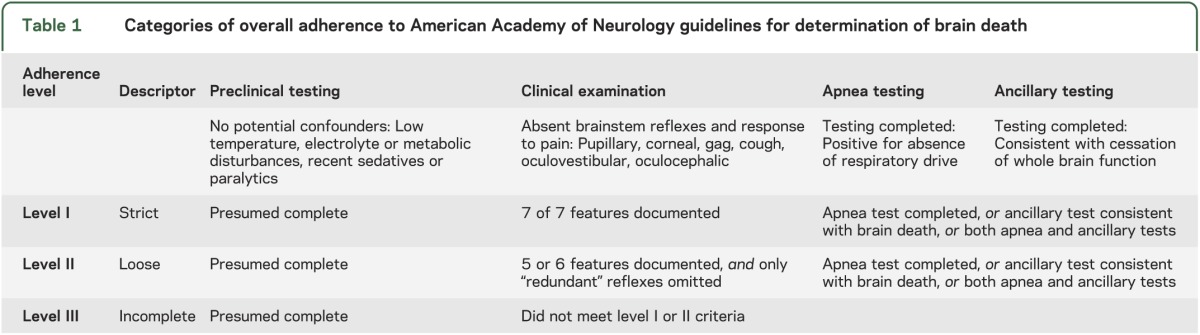
Finally, we assessed overall approach to BD determination grossly by evaluating clinical examination, apnea testing, and ancillary testing categories together for each subject and assigning them to 1 of 3 levels: level I (“strictly adherent”), level II (“loosely adherent”), and level III (“incomplete”) (table 1).
Table 1.
Categories of overall adherence to American Academy of Neurology guidelines for determination of brain death
All charts were thoroughly reviewed, and relevant documentation was accepted from any part of the record and from any member of the medical team. Categorization in cases of ambiguity regarding treating physician compliance erred toward presuming compliance. Blanket statements such as “no neurologic function” or “all reflexes negative” were not accepted if relevant findings were not documented explicitly somewhere in the chart. When available, reports from ancillary testing were reviewed and interpreted according contemporary AAN guidelines. Organ Procurement Organization–generated BD checklists were utilized only for recording the specialty of the physician of record diagnosing BD and verifying data abstracted directly from donor-hospital notes because of the variability in the intensity of completion of these checklists and the absence of any validation of the accuracy of the process.
Summary statistics relevant to variability in practice and adherence to AAN guidelines were generated.
Standard protocol approvals, registrations, and consents.
The project was exempted from approval by the institutional review board because all subjects were deceased.
RESULTS
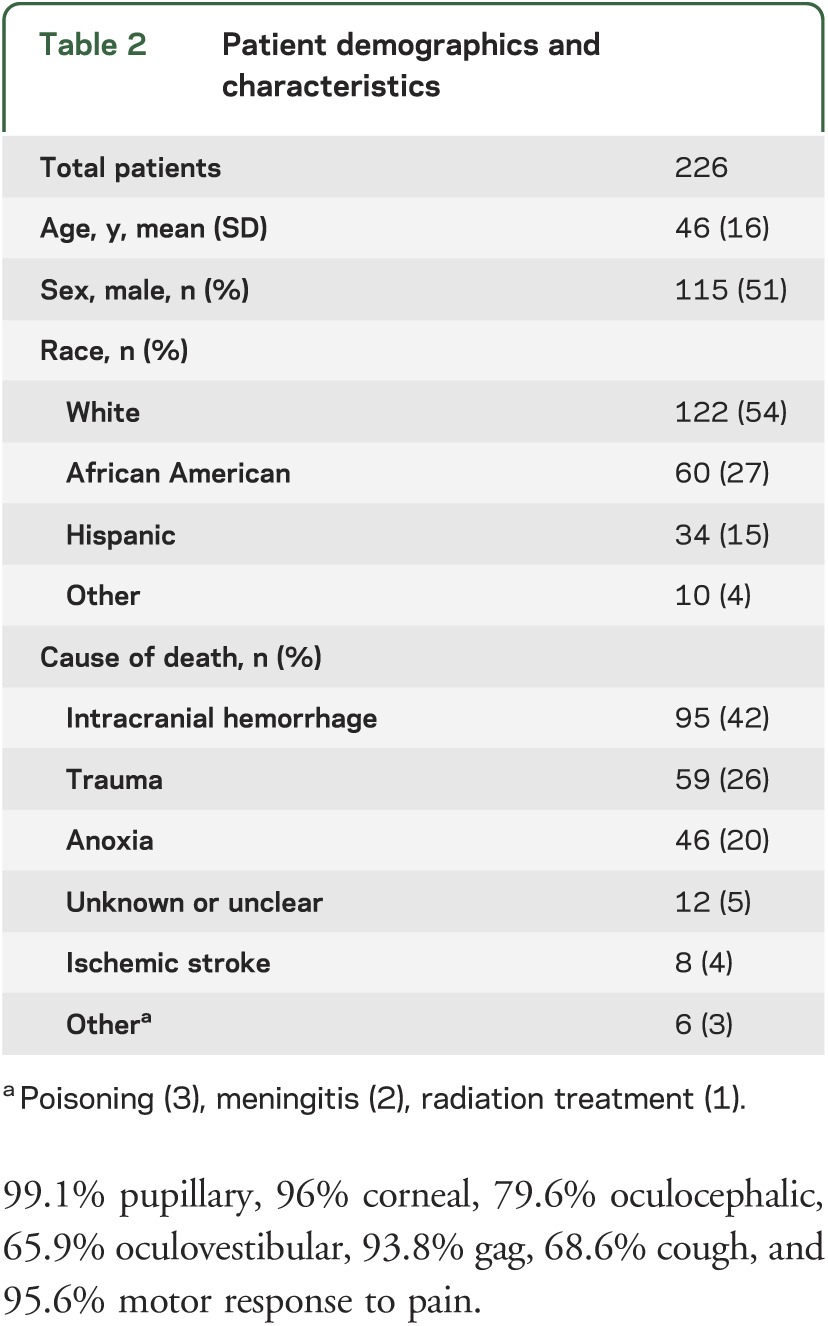
Data were collected for 226 of 228 adult BD organ donors. Two were excluded because of grossly incomplete medical records. Subjects were referred for donation from 68 different institutions. The mean number of BD organ donors per referring institution in 2011 was 3.2 ± 3.4 (range 1–20). The mechanism of injury leading to BD was intracranial hemorrhage in 95 (42%), trauma in 59 (26.1%), anoxia in 46 (20.4%), unknown or unclear in 12 (5.3%), ischemic stroke in 8 (3.5%), poisoning in 3 (1.3%), meningitis in 2 (0.9%), and radiation therapy in 1 (0.4%) (table 2).
Table 2.
Patient demographics and characteristics
Guideline performance/physician specialty.
The specialties of physicians of record determining BD varied widely (figure 1). The care of 214 of 226 subjects (94.7%) involved a neurologist, neurosurgeon, or both.
Figure 1. Specialty of physician of record determining brain death.
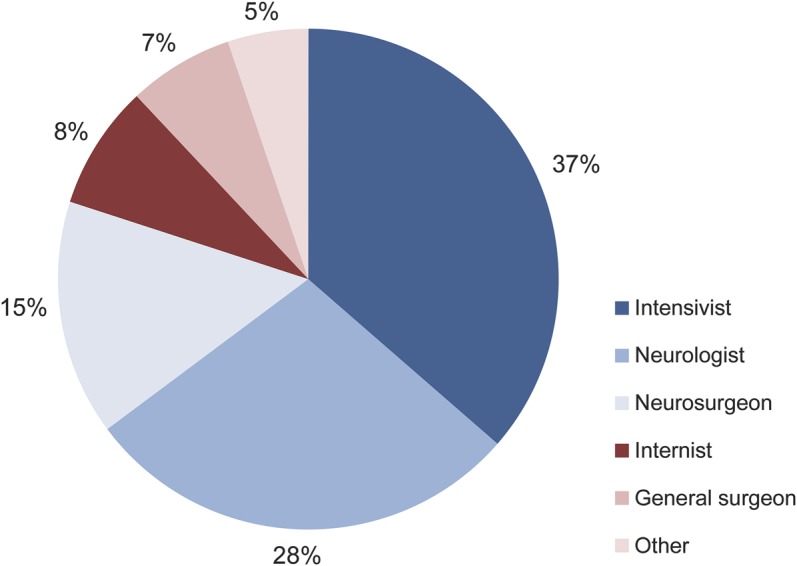
Other: trauma surgeon (5), emergency (3), anesthesiologist (1), family practitioner (1), geriatrician (1), transitional year (1), vascular surgeon (1). For subjects with more than one diagnosing physician, the specialties of both physicians were included (n = 250).
Preclinical testing.
A total of 35 of 226 subjects (15.5%) had documentation of core body temperature lower than 36.0°C, but no patients had temperature below 32.0°C. One hundred fifty-two of 226 subjects (67.3%) had abnormal sodium levels at time of death: 66 (29.2%) with Na+ >155, 20 (8.9%) with Na+ >165, and 9 (4%) with Na+ >170 mEq/L.
Clinical examination.
Testing of the AAN-recommended brainstem reflexes and motor response to pain was documented completely in 102 of 226 (45.1%). One hundred eighty-nine of 226 (83.6%) had at least 5 of the 7 examination features documented absent with only “redundant” reflexes omitted. The frequency of documented absence of the specific reflexes was 99.1% pupillary, 96% corneal, 79.6% oculocephalic, 65.9% oculovestibular, 93.8% gag, 68.6% cough, and 95.6% motor response to pain.
Apnea testing.
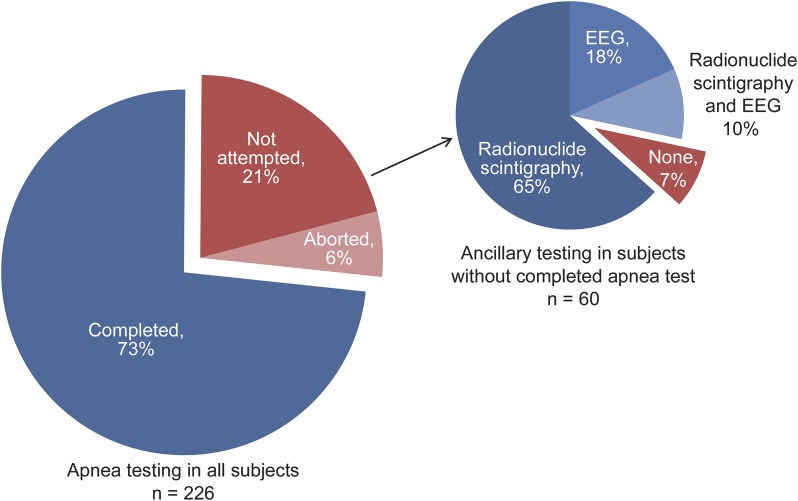
Apnea testing was completed in 166 (73.5%). Thirteen (5.8%) had testing initiated but aborted because of patient instability or technical difficulty. Apnea testing was not attempted in 47 (20.8%) (figure 2).
Figure 2. Apnea testing and performance of ancillary studies in select subjects.
Ancillary testing.
Of 60 patients without a completed apnea test, 56 (93.3%) had ancillary testing consistent with BD. Eleven (18.3%) had EEG consistent with BD, 39 (65%) had radionuclide scintigraphy consistent with BD, and 6 (10%) had both EEG and radionuclide scintigraphy consistent with BD. At least one ancillary test was performed in 148 of 226 patients (65.5%). Radionuclide scintigraphy was performed most frequently (80; 35.4%) followed by EEG (64; 28.3%) and CT angiography (29; 12.8%). The mean number of studies performed per patient was 0.89 ± 0.82 (range 0–4).
Overall adherence to AAN guidelines.
One hundred one of 226 (44.7%) met level I (strict) criteria, 84 (37.2%) met level II (loose) criteria, and 41 (18.1%) met level III (incomplete) criteria (figure 3).
Figure 3. Flowchart evaluating overall adherence to AAN guidelines.
*Clinical features include absence of pupillary, corneal, oculocephalic, oculovestibular, gag, and cough reflexes and motor response to pain. AAN = American Academy of Neurology.
DISCUSSION
We discovered wide variability in approaches to BD determination as reflected in medical record documentation.
The AAN guidelines emphasize that BD “is the absence of clinical brain function when the proximate cause is known and demonstrably irreversible.”4 Our finding that the specific mechanism leading to BD was unknown or unclear in 5.3% of patients is awkward. However, the guidelines are ambiguous in this area. For example, a patient with diffuse cerebral edema of severity to cause intracranial circulatory arrest and a clinical examination consistent with BD with all other BD determination prerequisites satisfied may be categorized as the “proximate cause” being cerebral edema even if the specific cause of that edema is unknown or never identified, as may be the case with some rare urea cycle metabolic disorders. Our review suggested that this categorization of mechanism relates to the ambiguity of the diagnostic specificity required in defining the proximate cause of BD.
The care of the vast majority of subjects (94.7%) involved neurologists and/or neurosurgeons, a practice that meets or exceeds the AAN guidelines recommendations. Despite their frequent involvement, however, only 43% of the BD determinations were performed by these specialists.
Regarding preclinical testing, many patients had conditions that the AAN recommends be excluded before BD determination, such as low body temperature and severe electrolyte abnormalities. The significance of this finding is debatable. The 1995 AAN practice parameters recommended that a valid BD examination must be performed only if the core temperature is >32°C. No patients were below that threshold. However, the updated AAN guidelines require a core temperature >36°C, and 15.5% of patients were below that threshold. Although 12.9% of our patients had Na+ >165 mEq/L, the AAN guidelines do not define which specific metabolic aberrations are prohibitive for interpretation of the clinical examination as consistent with BD.
BD determination may proceed in the presence of potential confounding factors, but only if they are recognized and appropriate ancillary testing is used. Because of the retrospective nature of this study, we could not reliably quantify the prevalence of each of the metabolic, electrolyte, or hormonal disturbances that the AAN cautions against, nor assess whether the findings were recognized and adequately addressed when present. However, the significant proportion of patients exhibiting the 2 studied potential confounding factors underscores the need for physician awareness of preclinical testing recommendations and the consideration of ancillary testing in selected cases if correction is not practical or feasible. Even then, the AAN guidelines are not prescriptive of which disturbances and/or their associated severity should challenge BD determination and need to be clarified to guide the integrity of clinical practice.
Demonstration of brainstem areflexia and absence of motor responses to pain are hallmark features of the BD examination and are consistent requirements across institutional protocols, but we found significant variability in the documentation of this portion of BD determination. Only 45.1% of our study population had complete documentation for the absence of all brainstem reflexes and motor responses to pain. Given the uniform importance of the clinical examination, as well as the relative simplicity of this portion of BD determination, this finding at the very least highlights the need for improved documentation. If lack of familiarity with the relevant clinical examinations also contributed to these omissions, then our results suggest the potential utility of education measures and tools such as BD checklists for those physicians primarily responsible for its determination.
Apnea testing is also a fundamental aspect of BD determination. It should be performed in all patients being evaluated for BD barring a specific contraindication, but 20.8% of our cohort did not have apnea testing attempted. It is unclear why there was such a high frequency of unattempted apnea testing in our cohort. The absence of documentation of this phenomenon in the charts of the patients in and of itself defines a need for refinement in documentation if not education of contemporary BD determination practice. When apnea testing cannot be performed or completed for any reason, an ancillary test is recommended,3 but 7% of subjects without a completed apnea test did not have confirmatory ancillary testing. The necessity of apnea testing in BD determination is recognized by both AAN guidelines and all institutional protocols studied in the literature, so its inconsistent use in practice may reflect physician discomfort or lack of familiarity with best practices regarding apnea testing. Educational opportunities and real-time resources for physicians responsible for BD determination may increase both the rate and quality of performance of this universally important aspect of the BD examination.
The use of ancillary testing and its role in BD determination also varied among patients. While most had at least one ancillary test performed, the decision to pursue testing was often not linked to a particular indication, and several subjects who did have indications for an ancillary test (e.g., incomplete apnea testing or severe electrolyte abnormalities) did not have one performed. These results suggest that the current use of ancillary testing in BD determination may be inefficient, or, at times, somewhat arbitrary. There is a tendency to discourage ancillary testing by many physicians expert in BD determination.7 Our results suggest that specific recommendations for appropriate use of ancillary testing could help clarify their role and rational application in selected cases.
While adherence to AAN guidelines was often high within a single category, analysis of the overall approaches to BD determination showed a more varied picture. It should be our goal that all BD determinations satisfy level I adherence to AAN guidelines, but it is encouraging that 82% of subjects at least met the level I or II criteria. The 18% with level III adherence highlight the ongoing need for comprehensive educational efforts and the potential future role for tracked performance parameters regarding the approach to BD determination and its documentation. Our categorization likely yields a conservative underestimate of the proportion of diagnoses falling short of contemporary guidelines, because we only evaluated practice in select portions of BD determination and did not include prerequisites or consider quality of adherence in any of categories in the overall assessment.
Our findings provide a rough snapshot of the current state of the documentation of BD determination in practice at a cross-section of hospitals in the United States within one geographic region. While previous research has demonstrated that institutional policies vary significantly across medical centers, this study is the first to assess the variability that exists in actual practice. Until now, one could claim that practice was more advanced than hospital policies, as is often the case.
Our study was only in organ donors (not in all BD patients), but it is reasonable to expect that the level of adherence to protocol and thoroughness of examination and documentation would be at least as high as for nondonor patients because of both the additional ethical responsibility associated with donation and the high degree of scrutiny and compliance requirements in organ donation cases. The validity and translatability of our findings is bolstered by the fact that our study population was from a large number of heterogeneous institutions across 2 states that perform a wide range (in number) of BD determinations in a given year.
Because we relied on medical record documentation, our results strictly describe the current state of the documentation of the approach to BD determination. There is no reason to believe that patients were wrongly diagnosed as BD. In fact, to the contrary, all reviewed charts consistently documented victims of catastrophic brain injury with findings consistent with BD, albeit with incompletely documented evaluations. But at the very least, even if BD determination is actually congruent with contemporary guidelines in practice, the documentation falls short of what should be permissible for such an important diagnosis.
If the documentation analyzed in our study reflects practice, even in part, then constructive changes are necessary to improve uniformity and completeness of BD determination. In general, we need to provide clearer expectations and make support available to physicians who are making this difficult and uncommon diagnosis. Some changes and tools that may be helpful as we embrace this challenge include mandatory universal adoption of contemporary AAN guidelines (or similar) at US institutions, use of BD checklists, increased educational opportunities for physicians who may be called upon to make a determination of BD, and easy access to practical resources and real-time assistance with BD determination. Advancing our efforts toward better education, practice, and documentation in this area is essential to maintaining well-earned public trust and ensuring a complete and thorough approach to BD determination for every patient who dies in this manner.
GLOSSARY
- AAN
American Academy of Neurology
- BD
brain death
AUTHOR CONTRIBUTIONS
Claire N. Shappell, BA: design, data collection, data analysis, manuscript. Jeffrey I. Frank, MD: design, data review, data analysis, manuscript. Khalil Husari, MD: data collection, manuscript. Matthew Sanchez, BS, Fernando Goldenberg, MD, and Agnieszka Ardelt, MD, PhD: data analysis, manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1. Guidelines for the determination of death: report of the medical consultants on the diagnosis of death to the President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. JAMA 1981;246:2184–2186 [PubMed] [Google Scholar]
- 2. Wijdicks EF. Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology 2002;58:20–25 [DOI] [PubMed] [Google Scholar]
- 3. Practice parameters for determining brain death in adults (summary statement). The Quality Standards Subcommittee of the American Academy of Neurology. Neurology 1995;45:1012–1014 [DOI] [PubMed] [Google Scholar]
- 4. Wijdicks EF, Varelas PN, Gronseth GS, et al. ; American Academy of Neurology Evidence-based guideline update: determining brain death in adults—report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2010;74:1911–1918 [DOI] [PubMed] [Google Scholar]
- 5. Greer DM, Varelas PN, Haque S, et al. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology 2008;70:284–289 [DOI] [PubMed] [Google Scholar]
- 6. Joffe AR, Anton N, Mehta V. A survey to determine the understanding of the conceptual basis and diagnostic tests used for brain death by neurosurgeons in Canada. Neurosurgery 2007;61:1039–1045 [DOI] [PubMed] [Google Scholar]
- 7. Wijdicks EF. The case against confirmatory tests for determining brain death in adults. Neurology 2010;75:77–83 [DOI] [PubMed] [Google Scholar]