Abstract
Laboratory and ad libitum smoking studies have indicated that alcohol consumption increases the frequency and intensity of smoking urges. However, few studies have examined the relation between smoking urges and alcohol use in natural settings during a quit attempt. The purpose of this study was to examine the relationships between smoking urge and alcohol use in women who reported drinking on at least one occasion during the first 7 days of a smoking quit attempt (N = 134). Participants were asked to use a palmtop computer to complete assessments that recorded smoking urges and recent alcohol use. Multilevel analyses examined the relation between smoking urge parameters and alcohol use. Smoking urges were higher during assessments where alcohol had been recently consumed compared to assessments where no alcohol had been consumed. Interestingly, the first urge rating of the day was higher and urges were more volatile on days where alcohol would eventually be consumed as compared to days where no alcohol was consumed. A closer examination of urge parameters on drinking days indicated that smoking urge trajectory was significantly flatter and urge volatility was significantly higher following alcohol consumption. However, smoking urge trajectory also flattened later in the day on nondrinking days. The findings suggest that there may be reciprocal relations between smoking urge and alcohol use (e.g., higher initial urges and more volatile urges may increase the likelihood of alcohol use; and, alcohol use may impact within day smoking urge parameters), and these relations could potentially impact smoking cessation and relapse.
Keywords: Smoking, Smoking urge, Alcohol, Ecological Momentary Assessment, Multilevel Analysis
Introduction
The association between smoking and alcohol use is well documented. Smokers consume more alcohol than non-smokers, and drinkers are more likely to smoke than are non-drinkers (e.g., Bien & Burge, 1990; Dawson, 2000; Friedman, Tekawa, Klatsky, Sidney, & Armstrong, 1991). In controlled laboratory studies, individuals smoke more after consuming alcohol than placebo (e.g., Griffiths, Bigelow, & Liebson, 1976; Mitchell, de Wit, & Zacny, 1995). Increased smoking after drinking has also been repeatedly demonstrated in studies using ecological momentary assessment (EMA) to assess smoking in the natural environment (e.g., Piasecki, McCarthy, Fiore, & Baker, 2008; Shapiro, Jamner, Davydov, & James, 2002; Shiffman et al., 1994; Shiffman et al., 2002; Shiffman & Paty, 2006).
The correlation between alcohol and tobacco use may be due to a cross-drug priming effect, where the use of one substance increases craving for the other (Rohsenow et al., 1997). In laboratory studies, alcohol consumption significantly increases the intensity of smoking urges in moderate to heavy drinkers relative to ingestion of a placebo (Burton & Tiffany, 1997; King, McNamara, Conrad, & Cao, 2009). Similar relationships are reported in chippers (Epstein, Sher, Young, & King, 2007; Sayette, Martin, Wertz, Perrott, & Peters, 2005), light smokers (e.g., King & Epstein, 2005), and heavy smokers (e.g., Sayette et al., 2005). Moreover, the quantity of alcohol consumed is positively correlated with subsequent smoking urges (Epstein et al., 2007; King & Epstein, 2005), and studies using EMA to assess behaviors in their natural contexts indicate that alcohol use is associated with more frequent and greater self-reported urges to smoke (e.g., Delfino, Jamner, & Whalen, 2001; Piasecki et al., 2008).
The association between alcohol use and smoking urge is especially important during a smoking cessation attempt. Smokers required to abstain from smoking who then receive alcohol have higher urges to smoke than those who receive placebo (Epstein et al., 2007; Kirchner & Sayette, 2007). Other research demonstrates that the odds of relapse are higher on days when alcohol is consumed as compared to non-drinking days (e.g., Kahler, Spillane, & Metrik, 2010; Shiffman, 1982; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996). One hypothesis is that drinking during a smoking quit attempt could activate brain reward pathways common to both drugs or cue urges to smoke due to previously repeated pairings of alcohol and tobacco use (e.g., Little, 2000; Rose et al., 2004; Zacny, 1990). Preliminary support for this hypothesis comes from a recent study demonstrating that smoking urges mediate the relation between postcessation alcohol use and smoking relapse at the one year follow-up (Hendricks, Delucchi, Humfleet, & Hall, 2012).
Other studies suggest that stressors may induce alcohol consumption (e.g., Brady & Sonne, 1999; Frone, 2008; Pelham & Lang, 1999; Sayette, 1999). Quitting smoking often induces a considerable amount of stress and negative affect in addition to urges to smoke. Thus, during a smoking cessation attempt, individuals may use alcohol in an attempt to cope with cessation induced stress, negative affect, and urges to smoke, consistent with the tension reduction hypothesis (Conger, 1956; Sayette, 1999). Such an effect could serve to create a “vicious” cycle in which greater smoking urges lead to alcohol consumption, that in turn, leads to greater urges to smoke and higher likelihood of relapse. However, to date few data exist to address this hypothesis and no studies have yet used EMA to assess the relation between smoking urges and alcohol use early in the quitting process, when smoking relapse is most likely (e.g., Brandon, Tiffany, Obremski, & Baker, 1990; Garvey, Bliss, Hitchcock, Heinold, & Rosner, 1992). Better understanding the association of alcohol use with urges to smoke in smokers’ natural settings could help to inform future efforts to reduce smoking relapse.
Study Purpose
Prior research has indicated that women may have greater difficulty quitting smoking than men (e.g., Scharf & Shiffman, 2004; Wetter et al., 1999), and therefore, may benefit from different interventions than men. The current study examined the relation between urge to smoke and alcohol consumption using EMA among women trying to quit smoking. Data were collected in a randomized clinical trial that aimed to evaluate the efficacy of an individually tailored palmtop computer delivered treatment that specifically focused on the reduction of smoking relapse in women (Wetter et al., 2011).
The current study compared: 1) urge ratings recorded during assessments when alcohol was recently consumed with those recorded during assessments when no alcohol was consumed, 2) smoking urge intercept, trajectory, and volatility recorded on drinking days with those recorded on non-drinking days, and 3) within day urge trajectory and volatility recorded prior to alcohol consumption with those recorded following alcohol consumption. We hypothesized that:
Urge to smoke and alcohol use would be positively related. Specifically, smoking urges would be higher during assessments where alcohol was recently consumed as compared to assessments where no alcohol was consumed.
Participants would attempt to reduce smoking urges through the consumption of alcohol. Thus, smoking urge parameters (e.g., intercept, slope, and volatility) would be higher on drinking than on non-drinking days.
Alcohol would have a priming effect on smoking urges. Thus, within day smoking urge parameters (i.e., urge slope and volatility) would significantly increase following the consumption of alcohol.
Method
Participants
Participants were 302 female smokers recruited from the Seattle metropolitan area between 1999 and 2002. All participants were enrolled in a smoking cessation study that utilized an individually tailored, palmtop computer delivered treatment (Wetter et al., 2011). Women were eligible to participate if they were between 18 and 70 years of age, smoked at least 10 cigarettes per day, had an expired breath carbon monoxide level ≥ 10 parts per million (ppm), and could speak, read, and write in English. Participants were excluded if they reported: 1) current use of tobacco products other than cigarettes, 2) current use of bupropion, 3) contraindication for nicotine patch use, or 4) current psychiatric disorders (i.e., substance use disorder, anxiety disorder, major depression, eating disorder) as assessed with a shortened version of the Primary Care Evaluation of Mental Disorders (PRIME-MD; Spitzer, Kroenke, Williams, & and the Patient Health Questionnaire Primary Care Study, 1999). Further details of the design and participant flow through the parent study are available elsewhere (Cofta-Woerpel et al., 2011; Wetter et al., 2011). Participants who reported consuming alcohol on at least one occasion during the first 7 days of a quit attempt (n = 134) were included in the current study.
Procedure
Women were recruited through media advertisements (print and radio) and were screened over the phone. Eligible participants attended an orientation session, at which time they set a quit date. All participants received a palm-top personal computer (PPC; Casio model E-10), were instructed on how to use the PPC, and were instructed to carry the PPC with them at all times. The PPC’s were used to conduct daily EMA assessments.
The benefits of EMA over traditional retrospectively recalled assessments has been described in detail (e.g., Shiffman, 2009; Shiffman et al., 1997). Briefly, EMA allows ecologically valid data collection about behaviors, thoughts, and feelings and involves repeated administration of assessments in near real time, in participants’ natural environments. Moments are sampled on either an event or random schedule and event and time-based assessments are combined and compared, within and across participants. EMA is commonly used to describe smoking topology and the predictors of smoking urges, lapse, and relapse (e.g., Cofta-Woerpel et al., 2011; Javitz, Lerman, & Swan, 2012; Piasecki, Jorenby, Smith, Fiore, & Baker, 2002, 2003), often disconfirming conventional wisdom about the relationships between these variables (Shiffman, 2009). In the current study, participants were asked to complete four computer-initiated, random assessments cued by the PPC each day during the participant’s normal waking hours. In addition, participants were asked to complete a “temptation” assessment each time they experienced an urge to smoke. Participants completed EMAs for 7 consecutive days beginning on their quit day. Information from these assessments was used to tailor a subsequent PPC delivered treatment (see Wetter et al., 2011 for details about the PPC treament). Project staff were available to answer any questions related to the use of the PPC.
Participants were compensated based on the percentage of random assessments completed (50%-69%: a $10 gift certificate, 70%-89%: a $25 gift certificate, ≥90%: a $50 gift certificate). Participants were not compensated for completing urge assessments. The average amount of time required to complete each assessment ranged from two to four minutes.
All participants received smoking cessation treatment based on the Smoking Cessation Clinical Practice Guideline recommendations (Fiore et al., 1996). Treatment included five one-hour group counseling sessions and six weeks of 21-mg nicotine patch. The first counseling session occurred 3 days prior to the quit date and the last occurred on day 7 post-quit.
Baseline Survey Measures
Standard self-report data were collected at baseline, including participants’ demographic characteristics (age, marital status, education, income, and race/ethnicity), smoking characteristics, and level of nicotine dependence (assessed via the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991).
Ecological Momentary Assessment Measures
Participants completed both computer-initiated random assessments and participant-initiated urge assessments for 7 consecutive days beginning on their quit date. All EMA assessments were date and time stamped, in order to examine the effects of Day of Assessment (i.e., day 1 through day 7) and Time of Assessment on smoking urge. An additional predictor, Daily Drinking Status (i.e., drinking day vs. non-drinking day) was created using information from the “alcohol consumption” item. Drinking days refer to days in which participants indicated that they consumed alcohol at one or more assessments and non-drinking days refer to days in which participants indicated that they did not consume any alcohol. During each random and urge event EMA assessment, participants rated their current urge to smoke (“How strong is your urge to smoke”) on a five point scale that ranged from “no urge” to “severe urge.” Each participant also indicated “yes” or “no” to the following item: “I am currently or have recently been drinking alcohol.”
Follow-up Measures
At each in person counseling session (i.e., days 3, 5, and 7), participants self-reported their smoking status and provided a breath sample for biochemical confirmation. Persons who self-reported not smoking and had CO levels of < 10 ppm were considered abstinent.
Data Analysis Plan
Taking into account the dependent nature of nested longitudinal EMA data (i.e., assessment ratings nested within days nested within participants; see Raudenbush & Bryk, 2002), the PROC MIXED procedure in SAS (Littell, Milliken, Stroup, Wolfinger, & Schabenberger, 2006) was used to conduct linear multilevel modeling (LMM) analyses. LMM efficiently handles unbalanced designs and missing data without excluding participants or imputing values (Gibbons et al., 1993; Gibbons, Hedeker, Waternaux, & Davis, 1988). LMMs were used to:1) estimate the effects of Alcohol Consumption (i.e., alcohol consumption at the time of assessment vs. non alcohol consumption at the time of assessment) and Day of Assessment (i.e., assessment day 1 through day 7) on individual EMA urge ratings recorded across the 7-day assessment period; and, 2) estimate the effects of Daily Drinking Status (i.e., drinking day vs. non-drinking day) and Order of Assessment (i.e., first through last assessment of the day) on individual EMA urge ratings recorded within a single day.
Preliminary analyses of an intercept-only model (i.e., a model with no predictors) found that an unstructured covariance matrix fit the correlation structure in the dataset best. A standard approach to model building was followed in which the main effect of predictors and their interaction terms were entered into the model, in a stepwise fashion, to predict smoking urge ratings. Under the assumption that the effects of the predictors on urge were the same for all participants, all predictors were initially entered as fixed-effect predictors. However, the nested data structure might reveal that the effects of predictors on urge vary across participants. Therefore, to allow the relationship between the predictors and urge to be different for each participant, random effects for predictors were entered into the models (see Hedeker, Mermelstein, Berbaum, & Campbell, 2009 for a discussion of modeling random effects in EMA smoking data). A log likelihood ratio test evaluated if adding these random effects significantly improved the model goodness-of-fit over models in which predictor effects were fixed.
In addition, an urge volatility index was calculated for each participant using the successive change approach recommended by Trull and colleagues (see Jahng, Wood, & Trull, 2008). The successive change approach quantifies volatility by taking into account observations’ variability and temporal dependency over time by calculating the squared difference between successive observations. However, to accommodate the fact that in EMA research, observations are often unevenly spaced over time, an adjustment was made in which the squared difference between two successive observations was divided by the temporal difference between those two observations (see Jahng et al., 2008). A daily volatility index was then computed by averaging all the adjusted squared successive differences within a day. Furthermore, to compare urge volatility reported by smokers before they drank with that reported by smokers after they drank, drinking days were divided into pre-drinking and post-drinking periods and separate urge volatility indices were calculated for each period. LMMs were used to examine the effect of alcohol consumption on urge volatility before and after drinking on days that participants consumed alcohol.
Finally, a two-rate piecewise model (Raudenbush & Bryk, 2002), a special case of LMM, was used to compare urge trajectories before and after drinking on days that participants consumed alcohol. That is, using the time of the first alcoholic drink of a day as the transition point, a day was split into pre-drinking and post-drinking periods. Urge trajectories were estimated for pre-drinking and post-drinking periods and then compared to determine if alcohol use had an impact on these urge parameters.
Results
Participant characteristics are shown in Table 1. During the first week post-cessation, 134 participants reported having at least one alcoholic drink and were included in the analytic sample. Participants completed 5,625 random and temptation assessments on a cumulative 926 days of monitoring. Most participants (92%) completed assessments on each day of EMA monitoring period, while 8% of participants completed assessments on 6 out of 7 days and one participant completed assessments on 5 out of 7 days. The majority of completed assessments (n = 2,973; 53%) were initiated by participants in response to smoking urges (i.e., temptation assessments), and the remaining assessments (n = 2,652; 47%) were randomly initiated by the PPC. On average, participants completed 20.03 (SD = 4.49) random assessments and 22.17 (SD = 11.72) temptation assessments during the 7-day monitoring period.
Table 1.
Demographic characteristics of participants
| Measure | Participants (n = 134) |
|---|---|
| Age in years, mean (standard deviation) | 41.24 (10.26) |
| Gender: Female, n (%) | 134 (100%) |
| Ethnicity/race *, n (%) | |
| Caucasian | 100 (81%) |
| Other | 23 (17%) |
| Education, n (%) | |
| ≤High school | 16 (12%) |
| Some college | 72 (54%) |
| ≥College graduate | 46 (34%) |
| Marital status **, n (%) | |
| Single | 39 (29%) |
| Married/living with partner | 51 (38%) |
| Divorced/separated/widowed | 41 (31%) |
| Depression history **, n (%) | 38 (28%) |
| Smoking variables | |
| Typical smoking rate, mean (SD) | 20.15 (7.32) |
| FTND score, mean (SD) | 4.90 (1.93) |
1 participant did not report this information
3 participants did not report this information
FTND = Fagerström Test for Nicotine Dependence
The overall compliance rate for random assessments was 79.2% (range: 27 – 100%). Approximately 34% of the participants completed less than 75% of their scheduled random assessments. No significant association was found between the number of completed random assessments and the number of completed temptation assessments initiated by participants.
Out of the 5,625 completed assessments, 433 (7.7%) were completed by participants after they had recently consumed alcohol. Participants indicated that they consumed alcohol on 268 (29%) of the 926 days of monitoring. Assessments in which participants reported recent alcohol use were generally later in the day than assessments in which alcohol was not recently consumed, F (1, 5478) = 331.12, p < .0001. Participants completed more assessments on days (mean = 7.07, standard error [SE] = .21) when alcohol was consumed than days when alcohol was not consumed (mean = 5.65, SE = .17; t = 8.31, p < .0001). More specifically, participants initiated significantly more temptation assessments on drinking (mean = 3.98; SE = .18) than on non-drinking days (mean = 2.89; SE = .15; t = 7.37, p < .0001); and completed more random assessments on drinking days (mean = 3.08; SE =.08) than on non-drinking days (mean = 2.76; SE = .08; t = 4.17, p < .01).
Urge Ratings at Drinking and Non-drinking Assessments across the 7-day EMA Period
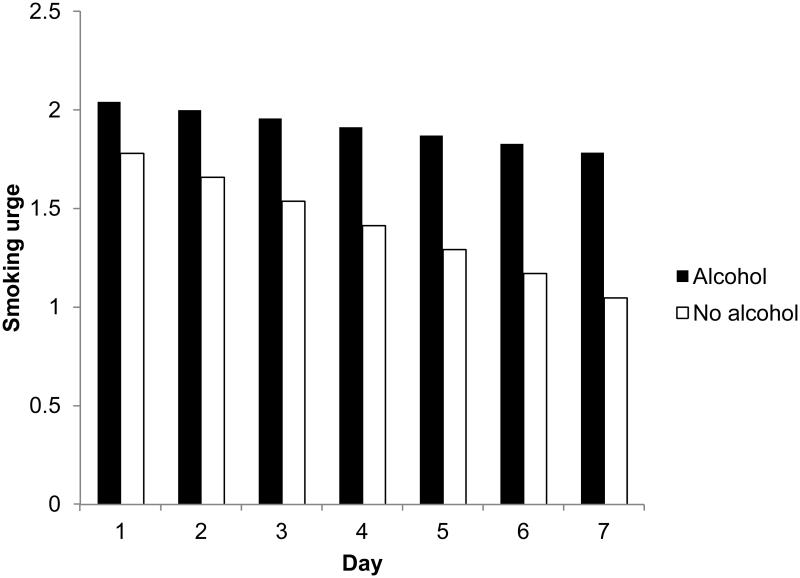
To examine the hypothesis that urges would be higher during assessments where alcohol was recently consumed as compared to assessments where no alcohol was consumed, three-level LMMs were constructed (i.e., assessment ratings nested within Day of Assessment nested within persons) with Alcohol Consumption and Day of Assessment as predictors of smoking urge. We compared models that assumed the effect of predictors on urge to be constant across participants (i.e., fixed effects) with those that assumed the effect of predictors on urge to be varied (i.e., random effects). Adding random effects for both Alcohol Consumption and Day of Assessment significantly improved model fit as compared to models that included: 1) only the random effect for Alcohol Consumption (Δχ2 = 23.9, p < .01), 2) only the random effect for Day of Assessment (Δχ2 = 29.3, p < .01), and 3) both Alcohol Consumption and Day of Assessment treated as fixed effects (Δχ2 = 53.4, p < .01). Using the best-fitting model, we found a significant Alcohol Consumption × Day of Assessment interaction effect on urge ratings, F (1, 5476) = 5.81, p = .02. As indicated in Figure 1, smoking urge ratings where participants reported recent alcohol consumption were significantly higher than those recorded when participants reported no alcohol consumption, t (5476) = 2.68, p < .001. Furthermore, smoking urges recorded when participants reported recent alcohol consumption remained relatively constant (rate of change = −.04), whereas smoking urges recorded at assessments where no alcohol was consumed dropped across the 7 day monitoring period (rate of change = −.12). These rates of change were significantly different from one another, t (5476) = 2.41, p = .02. Results remained significant after controlling for relevant covariates (i.e., lapse status, time of assessment, and number of assessments completed per day).
Figure 1.
Smoking urge ratings at assessments when alcohol was consumed were significantly higher than ratings at assessments when alcohol was not consumed.
Urge Intercepts and Trajectories on Drinking Versus Non-drinking Days
To examine the hypothesis that smoking urge parameters (e.g., intercept, slope, and volatility) would be higher on drinking than on non-drinking days, we regressed within-day urge trajectories on Daily Drinking Status and Order of Assessment. The model with random effects for Order of Assessment significantly improved the model’s fit over the model in which all predictors were treated as fixed effects (Δχ2 = 36.0, p < .01). The log likelihood test indicated that adding random effects for Daily Drinking Status effect did not significantly improve model fit (Δχ2 = 3.8, ns), and therefore, the random slope parameter for Daily Drinking Status was not added into the final model.
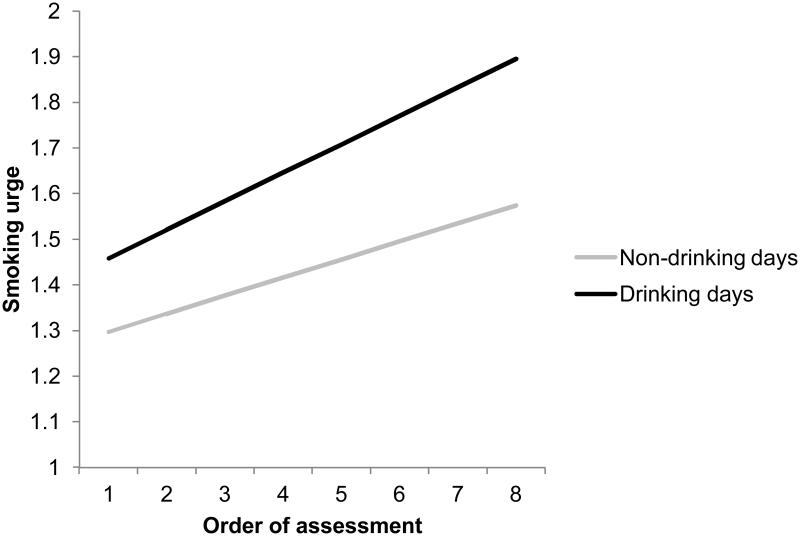
Using the best-fitting model, we found a significant Daily Drinking Status main effect (F (1, 5483) = 28.84, p < .0001), such that participants reported higher urges to smoke on drinking days than non-drinking days. In addition, the main effect for Order of Assessment was significant (F (1, 5483) = 51.05, p < .0001). This finding indicated that smoking urge ratings were higher later in the day than earlier in the day. The interaction between Daily Drinking Status and Order of Assessment was not significant (F (1, 5482) = 2.76, p = .091). Figure 2 shows that participants reported significantly higher urge ratings on drinking days (simple intercept = 1.46) than on non-drinking days (simple intercept = 1.28; t (5483) = 5.37, p < .0001). Adding participant lapse status and number of non-drinking assessments completed per day as covariates did not significantly alter the results.
Figure 2.
Smoking urge intercept was higher on drinking days (simple intercept = 1.46) than on non-drinking days (simple intercept = 1.28). However, smoking urge trajectories were not different on drinking (simple slope = .062) and non-drinking days (simple slope = .039). Smoking urge was measured on a five point scale that ranged from “no urge” to “severe urge.” Order of assessment refers to the first through last assessment of a day.
Urge Volatility on Drinking Versus Non-Drinking Days
To examine urge volatility, we calculated a mean daily urge volatility index for each participant for each day using Jahng’s equation (Jahng et al., 2008). The use of a daily mean urge volatility index resulted in a two-level data structure where daily urge volatility indices were nested within participants. Therefore, we used 2-level LMMs to examine the effects of alcohol consumption on urge volatility. After regressing the daily urge volatility index on Daily Drinking Status, we found that adding a random slope effect for Daily Drinking Status did not significantly improve model fit (Δχ2 = 3.78, ns), and therefore, a random effect parameter was not added to the model. The final model indicated a significant main effect of Daily Drinking Status, F (1, 771) = 11.60, p < .001. Thus, participants’ urge volatility index was significantly higher on drinking days (volatility index estimate = 1.99) than on non-drinking days (volatility index estimate = 1.58, t [771] = 3.33, p < .001). This effect remained significant after controlling for relevant covariates (i.e., lapse status and number of non-drinking assessments completed per day).
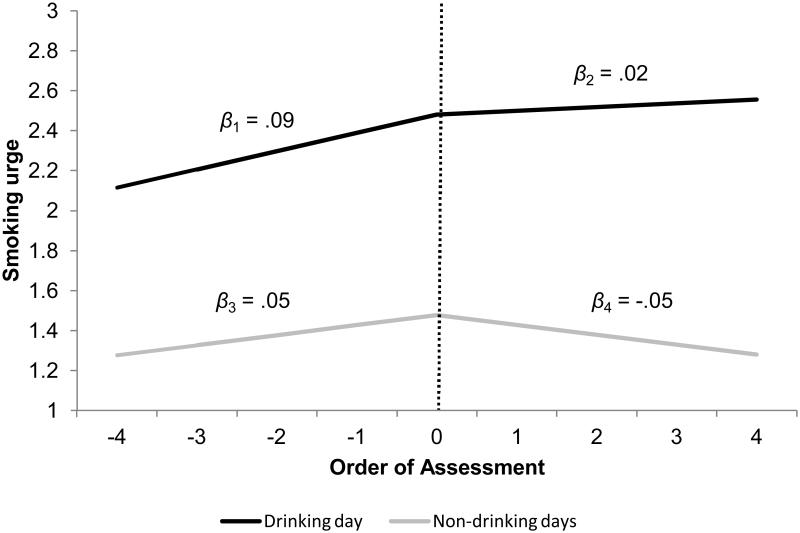
Urge Trajectory and Volatility before and after First Alcoholic Drink
To examine the hypothesis that within day smoking urge parameters (i.e., urge slope and volatility) would significantly increase following the consumption of alcohol, we used the time of first alcoholic drink as the transition point to divide drinking days into separate pre-drinking and post-drinking periods. Two-rate piecewise models were employed to estimate separate trajectories for each period. Because participants took their first alcoholic drink at different times and time correlated positively with smoking urge, the trajectories were estimated while controlling for the time of the first alcohol drink. The results showed that on days that participants consumed alcohol, urge trajectory significantly increased prior to their first drink, t (1715) = 5.98, p < .0001 (see Figure 3). After their first drink, the post-drinking trajectory flattened significantly from that of the pre-drinking period, t (1715) = −2.40, p < .05. This finding was counter to our hypothesis that drinking would increase smoking urge trajectory. We repeated the final model analyses after adding participant lapse status and number of drinking and non-drinking assessments completed per day as covariates. Adding these covariates did not significantly alter the results.
Figure 3.
Smoking urge trajectory before alcohol consumption (slope =.09) was significantly different from that after alcohol consumption (slope = .02) on drinking days. Smoking urge trajectory before the “cut-point” (slope =.05) was significantly different from that after the “cut-point” (slope = -.05) on non-drinking drinking days. The dotted line indicates the time of first alcoholic drink/cut-point. Smoking urge was measured on a five point scale that ranged from “no urge” to “severe urge.” In this figure, the order of assessment is centered on the time of first alcoholic drink, with negative values indicating to pre-drinking/cut-point assessments and positive values indicating post-drinking/cut-point assessments.
LMM was also used to compare urge volatility before and after a participant consumed alcohol. Only days in which participants consumed alcohol and completed two or more assessments before and after alcohol consumption were included in this analysis (i.e., urge volatility cannot be calculated with only one assessment). This resulted in 117 days of data collected from 80 participants (original N = 134). Earlier analyses showed that smoking urges were higher later in the day as compared to urges recorded earlier in the day. To control for the possibility that smoking urges also became increasingly volatile as a day progressed, daily trajectories of smoking urge volatility were computed for each participant and included in the analysis as a covariate. Controlling for the trajectories of urge volatility and the time of first alcohol drink, results revealed that on any given drinking day, urge volatility measured during the post-drink period (β = 1.48) was significantly higher than that measured in the pre-drink period (β = 0.88), F (1, 140) = 4.93, p < .05. Analyses were repeated after controlling for lapse status and number of drinking assessments completed per day. Including these covariates did not significantly modify these results.
Post Hoc Analyses
Finally, we examined the trajectory and volatility of smoking urges on days where alcohol was not consumed. Using the mean time of first drink on drinking days as a standard cut-point, we split non-drinking days into two periods. We then used a two-rate piecewise model to estimate separate trajectories for the pre cut-point and post cut-point periods. Results indicated that smoking urge increased prior to the cut-point on non drinking days (t = 5.47, p < .0001), and significantly flattened during the post cut-point period (t = −3.15, p < .01). Thus, results mirrored the analysis that compared urge trajectory before and after the first drink on drinking days (i.e., smoking urge trajectory was significantly flatter during the post cut-point period as compared to the pre cut-point period). Follow-up analyses indicated that the pre drinking trajectory (drinking days) was not different from the pre cut-point trajectory (non-drinking days), F (1, 3086) = 1.36, p =.24, and the post drinking trajectory was not different from the post cut-point trajectory (non drinking days), F (1, 1694) = 0.53, p = .47 (see Figure 3).
Discussion
The current study examined the relation between alcohol use and urge to smoke during the first week of smoking cessation among women participating in treatment. There were four key findings. First, overall smoking urge ratings were higher during assessments where alcohol was recently consumed than when no alcohol had been consumed. Second, the reduction in smoking urge ratings across the first postcessation week was greater for nondrinking assessments than drinking assessments. Third, smoking urge parameters (i.e., intercept, volatility) were higher on drinking days than non-drinking days. Findings indicate that smoking urges were of greater intensity and showed greater volatility on drinking days than non-drinking days even before the individual began to drink, suggesting that alcohol consumption could have been a response to adverse smoking urge trajectories rather than vice versa. Finally, although within day smoking urge trajectory did not increase following alcohol consumption, urge volatility did increase following alcohol consumption. The findings of this study expand upon previous work showing relationships between smoking urges and alcohol use, and have important implications for understanding the association between alcohol use and smoking urges.
The first key finding was that across the first 7 days of a quit attempt, smoking urge was higher at assessments where alcohol had recently been consumed than at assessments where alcohol had not been consumed. In addition, urge to smoke, as reported during assessments where no alcohol was consumed, attenuated across the first week post-cessation. This finding is consistent with previous research showing that smoking urges spike soon after the onset of abstinence and then attenuate across the first week post-cessation (e.g., Piasecki et al., 2000). However, smoking urges recorded after consuming alcohol remained relatively high across the entire 7 day EMA period. Thus, one way that alcohol use may increase the likelihood of relapse is by engendering urges later in the cessation process that are similar in severity to those experienced immediately after quitting
Regardless of daily drinking status, overall urge to smoke increased as the day progressed (see Figure 2). This finding is consistent with previous work that has examined within day smoking urge following smoking cessation (Teneggi et al., 2002). However, urge to smoke started higher (as measured by the intercept), and urge volatility was significantly greater on days where alcohol would eventually be consumed than days where no alcohol was consumed. The difference in the rate of increase in urge ratings within drinking versus nondrinking days (i.e., slope) approached significance, suggesting that urge severity may increase at a greater rate on drinking days as compared to non-drinking days. In other words, stronger, more volatile, and increasingly severe urges to smoke may be harbingers for alcohol consumption in women during the early phase of a smoking quit attempt. Although few studies have examined the prospective relation between smoking urges and subsequent alcohol use, Cooney and colleagues (2007) demonstrated that alcohol dependent individuals undergoing concurrent alcohol and smoking cessation treatments were more likely to have an alcohol relapse during periods of high smoking urges as compared to periods of low urges to smoke. In addition, Palfai, Monti, Ostafin, and Hutchison (2000) found that acute tobacco deprivation was related to increased urges to consume alcohol in a sample of “hazardous drinkers.” Those findings, coupled with the results of this study, suggest that abstinent smokers may consume alcohol in an attempt to cope with greater smoking urge severity that occurs prior to drinking onset. Similarly, smokers may attempt to dampen urge volatility or an increase in urge magnitude across the course of a day by drinking. To the best of our knowledge, the current study is the first to find that smoking urges may actually increase the likelihood of alcohol consumption during a smoking cessation attempt. These findings are relatively unique and may provide support for the cross-drug coping hypothesis (see Monti, Rohsenow, Colby, & Abrams, 1995). More research is needed to examine whether smoking urges actually drive alcohol use during a smoking cessation attempt.
Although the trajectory of smoking urges continued to rise slightly following the consumption of the first alcoholic beverage, the trajectory actually flattened out post drink. Post-hoc analyses which split nondrinking days into two parts (i.e., pre cut-point and post cut-point) revealed that smoking urge trajectory also flattened during the post cut-point period on nondrinking days. Since the post cut-point and post drinking trajectories were both flatter than the pre cut-point and pre drinking trajectories, it is likely that some variable other than alcohol caused the post drink/post cut-point smoking urge trajectories to flatten. At least at a superficial level, the observed flattening of the urge slope following drinking appears contrary to our hypothesis and previous studies that suggest that the consumption of alcohol tends to increase the urge to smoke (e.g., King & Epstein, 2005; Kirchner & Sayette, 2007; Ray et al., 2007). Urge severity did continue to increase post drinking, but the trajectory of the increase was less than what it was prior to drinking, and in fact, post hoc analyses showed similar effects of time of day on urge trajectory on nondrinking days. Thus, it may be the case that alcohol consumption exerts little effect on smoking urge trajectory, or that the time of day exerts a stronger effect than does alcohol use. Although some previous work has indicated that alcohol use may increase the urge to smoke, most of these studies have been conducted in laboratory settings with smokers who were not attempting to quit smoking (e.g., Burton & Tiffany, 1997; King et al., 2009; Sayette et al., 2005). However, one recent study showed that greater postcessation drinking was related to increased positive reinforcement smoking urges (using a recall measure), which resulted in lower smoking abstinence at the one year follow-up (Hendricks et al., 2012). Teasing apart the effect of alcohol use on smoking urge trajectories in the real world during a quit attempt will require careful, focused investigations in the future.
Finally, alcohol use may have had an effect on subsequent urge volatility. Specifically, self-reported urges became more volatile following alcohol consumption. However, this volatility analysis was limited by the fact that approximately 40% of the participants were excluded due to the limited number of assessments that were completed before and after drinking occurred. In addition, other analyses indicated that smoking urges tended to increase as the day progressed. Thus, the post-alcohol increase in urge volatility may simply be an artifact of higher urges later in the day, although we attempted to control for this possibility by including the slope of within day urge volatility as a covariate in an analysis that compared urge volatility before and after drinking. The results were unchanged - urge volatility significantly increased following alcohol consumption. Unfortunately, additional post-hoc analyses aimed at determining if urge volatility similarly increased on nondrinking days were not possible because only 22% of the nondrinking day volatility data were available.
The current study has a number of limitations. First, although previous research has indicated that women may be at greater risk for smoking relapse than men (e.g., Scharf & Shiffman, 2004; Wetter et al., 1999), little work has been done to identify mechanisms linking gender and smoking relapse. The findings of this study may suggest that women undergoing a smoking cessation attempt may use alcohol as a way to cope with heightened smoking urges, and it is possible that this may increase their likelihood of smoking relapse. Considering previous research that suggests that the causes of substance relapse among men and women may differ (Walitzer & Dearing, 2006), results of this study may not be generalizable to men. Second, our ability to examine the relation between smoking urge and alcohol use was limited to the first week post-cessation because EMAs were only collected during this period. Although it is extremely important to gain a clearer understanding of the early post-cessation period (i.e., half of all smoking relapses occur during the first week post-cessation; see Garvey et al., 1992), the relation between alcohol use and smoking urges in the moderate and longer term post-cessation should be a focus of future EMA studies. A third limitation concerns the compliance rate with assessments. Specifically, participants completed more temptation assessments on drinking days as compared to non drinking days. This finding may be due to the fact that participants reported higher urges on drinking days as compared to non drinking days. Controlling for number of assessments completed on each day of monitoring did not significantly impact results. Our ability to identify pre/post drinking differences in the trajectory and volatility of smoking urges was limited by the fact that alcohol consumption generally occurred later in the day, which reduced the number of post drinking assessments available for analysis. In addition, our finding that urge volatility increased following alcohol use was also limited because we were unable to determine whether similar increases in urge volatility occurred on nondrinking days. This limitation may be difficult to address without a very intensive monitoring protocol given that people tend to drink alcohol later in the day. Despite the limitations of this study, findings provide insights into the complex relation between alcohol and smoking motivation and may inform the development and design of future studies that seek to understand the reciprocal relationships between these factors during smoking quit attempts.
Previous research has indicated that urge to smoke (e.g., Allen, Bade, Hatsukami, & Center, 2008; Hendricks et al., 2012; Piasecki et al., 2002, 2003) and alcohol use (e.g., Hendricks et al., 2012; Kahler et al., 2010; Shiffman et al., 1996) predict smoking relapse in men and women. Furthermore, smoking urge intercepts and volatility during the first postcessation week have both been related to relapse (Cofta-Woerpel et al., 2011; Javitz, Lerman, & Swan, in press; Piasecki et al., 2003) and these parameters might reflect mechanisms that account for at least part of the association of alcohol use and relapse to smoking. To the best of our knowledge, this is the first study to find that smoking urge parameters (i.e., intercept, volatility) differ on drinking versus non-drinking days in meaningful ways. The current findings add to previous research by highlighting several potential mechanisms through which alcohol use may increase the likelihood of smoking relapse (i.e., through increasing smoking urges, decreasing the post-quit attenuation of smoking urges that tends to occur naturally over time, and increasing urge volatility post drinking). If replicable, the current findings suggest that alcohol consumption should continue to be discouraged (see Fiore et al., 2008) during periods of heightened smoking urge as drinking may increase the volatility of urge swings, and potentially increase the likelihood of relapse.
Perhaps more importantly, and a more novel finding, is that in addition to being a precipitant of smoking urges, alcohol use may be a consequence of elevated, volatile, and escalating urges to smoke. Thus, individuals undergoing a smoking quit attempt may consume alcohol in an effort to cope with those urges to smoke. If true, the recommendation to avoid alcohol during a cessation attempt would not address the fact that alcohol use may be a consequence rather than a cause of increased urge to smoke. Thus, identifying the determinants of why smoking urge parameters are more adverse on drinking days even prior to drinking, or identifying algorithms signaling these adverse patterns could potentially facilitate new or more intensive intervention efforts aimed at reducing urges, subsequent alcohol use, and potential increases in relapse likelihood.
Disclosures and Acknowledgements
This research was supported by grants from the National Cancer Institute (R01CA74517 to DWW) and the American Cancer Society (MRSGT-12-114-01-CPPB to MSB, MRSGT-10-104-01-CPHPS to DEK, and MRSG-09-002-01-CPHPS01 to CYL). The MD Anderson Cancer Center is supported by a National Cancer Center Core grant (CA16672). These funding sources had no other role other than financial support.
Footnotes
The research protocol used in this data collection was approved by the IRBs at the University of Texas MD Anderson Cancer Center and the Group Health Research Institute, and all research procedures were fully consistent with Public Health Code of Ethics and American Psychological Association ethical guidelines. All authors have met the requirements for authorship, and the manuscript has been read and approved by each author.
The authors do not have any conflicts of interest pertaining to this work.
References
- Allen SS, Bade T, Hatsukami D, Center B. Craving, withdrawal, and smoking urges on days immediately prior to smoking relapse. Nicotine & Tobacco Research. 2008;10(1):35–45. doi: 10.1080/14622200701705076. [DOI] [PubMed] [Google Scholar]
- Bien TH, Burge R. Smoking and Drinking: A Review of the Literature. Substance Use & Misuse. 1990;25(12):1429–1454. doi: 10.3109/10826089009056229. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sonne SC. The Role of Stress in Alcohol Use, Alcoholism Treatment, and Relapse. Alcohol Research & Health. 1999;23(4):263–271. [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: the process of relapse. Addict Behav. 1990;15(2):105–114. doi: 10.1016/0306-4603(90)90013-n. [DOI] [PubMed] [Google Scholar]
- Burton SM, Tiffany ST. The effect of alcohol consumption on craving to smoke. Addiction. 1997;92(1):15–26. [PubMed] [Google Scholar]
- Cofta-Woerpel L, McClure JB, Li Y, Urbauer D, Cinciripini PM, Wetter DW. Early cessation success or failure among women attempting to quit smoking: Trajectories and volatility of urge and negative mood during the first postcessation week. Journal of Abnormal Psychology. 2011;120(3):596–606. doi: 10.1037/a0023755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger J. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Cooney JL, Pilkey DT, Steinberg HR, Oncken CA. Alcohol and Tobacco Cessation in Alcohol-Dependent Smokers: Analysis of Real-Time Reports. Psychology of Addictive Behaviors. 2007;21(3):277–286. doi: 10.1037/0893-164X.21.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. Drinking as a risk factor for sustained smoking. Drug and Alcohol Dependence. 2000;59(3):235–249. doi: 10.1016/s0376-8716(99)00130-1. [DOI] [PubMed] [Google Scholar]
- Delfino RJ, Jamner LD, Whalen CK. Temporal analysis of the relationship of smoking behavior and urges to mood states in men versus women. Nicotine & Tobacco Research. 2001;3(3):235–248. doi: 10.1080/14622200110050466. [DOI] [PubMed] [Google Scholar]
- Epstein A, Sher T, Young M, King A. Tobacco chippers show robust increases in smoking urge after alcohol consumption. Psychopharmacology. 2007;190(3):321–329. doi: 10.1007/s00213-006-0438-8. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Smoking Cessation: Clinical Practice Guideline No. 18. US Dept of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; Rockville, MD: 1996. AHCPR publication 96-0692. [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Clinical Practice Guideline. Department of Health and Human Services. Public Health Service; Rockville, MD: 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- Friedman GD, Tekawa I, Klatsky AL, Sidney S, Armstrong MA. Alcohol drinking and cigarette smoking: an exploration of the association in middle-aged men and women. Drug and Alcohol Dependence. 1991;27(3):283–290. doi: 10.1016/0376-8716(91)90011-m. [DOI] [PubMed] [Google Scholar]
- Frone MR. Are work stressors related to employee substance use? The importance of temporal context assessments of alcohol and illicit drug use. Journal of Applied Psychology. 2008;93(1):199–206. doi: 10.1037/0021-9010.93.1.199. [DOI] [PubMed] [Google Scholar]
- Garvey AJ, Bliss RE, Hitchcock JL, Heinold JW, Rosner B. Predictors of smoking relapse among self-quitters: a report from the Normative Aging Study. Addictive Behaviors. 1992;17(4):367–377. doi: 10.1016/0306-4603(92)90042-t. [erratum appears in Addict Behav 1992 Sep-Oct;17(5):513. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker D, Elkin I, Waternaux C, Kraemer HC, Greenhouse JB, et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data: Application to the NIMH Treatment of Depression Collaborative Research Program dataset. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker D, Waternaux C, Davis JM. Random regression models: a comprehensive approach to the analysis of longitudinal psychiatric data. Psychopharmacology Bulletin. 1988;24:438–443. [PubMed] [Google Scholar]
- Griffiths RR, Bigelow GE, Liebson I. Facilitation of human tobacco self-administration by ethanol: A behavioral analysis. Journal of the Experimental Analysis of Behavior. 1976;25:279–292. doi: 10.1901/jeab.1976.25-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström tolerance questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Mermelstein RJ, Berbaum ML, Campbell RT. Modeling mood variation associated with smoking: An application of a heterogeneous mixed-effects model for analysis of ecological momentary assessment (EMA) data. Addiction. 2009;104(2):297–307. doi: 10.1111/j.1360-0443.2008.02435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks PS, Delucchi KL, Humfleet GL, Hall SM. Alcohol and marijuana use in the context of tobacco dependence treatment: Impact on outcome and mediation of effect. Nicotine & Tobacco Research. 2012;14(8):942–951. doi: 10.1093/ntr/ntr312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods. 2008;13(4):354–375. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- Javitz HS, Lerman C, Swan GE. Comparative dynamics of four smoking withdrawal symptom scales. Addiction. 2012;107(8):1501–1511. doi: 10.1111/j.1360-0443.2012.03838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javitz HS, Lerman C, Swan GE. Comparative dynamics of four smoking withdrawal symptom scales. Addiction. 107(8):1501–1511. doi: 10.1111/j.1360-0443.2012.03838.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Spillane NS, Metrik J. Alcohol use and initial smoking lapses among heavy drinkers in smoking cessation treatment. Nicotine & Tobacco Research. 2010;12(7):781–785. doi: 10.1093/ntr/ntq083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King A, Epstein AM. Alcohol dose-dependent increases in smoking urge in light smokers. Alcoholism: Clinical & Experimental Research. 2005;29(4):547–552. doi: 10.1097/01.alc.0000158839.65251.fe. [DOI] [PubMed] [Google Scholar]
- King A, McNamara P, Conrad M, Cao D. Alcohol-induced increases in smoking behavior for nicotinized and denicotinized cigarettes in men and women. Psychopharmacology. 2009;207(1):107–117. doi: 10.1007/s00213-009-1638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner TR, Sayette MA. Effects of smoking abstinence and alcohol consumption on smoking-related outcome expectancies in heavy smokers and tobacco chippers. Nicotine & Tobacco Research. 2007;9(3):365–376. doi: 10.1080/14622200701188893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. Second SAS Institute Inc.; Cary, NC: 2006. [Google Scholar]
- Little HJ. Behavioral mechanisms underlying the link between smoking and drinking. Alcohol Research & Health. 2000;24(4):215–224. [PMC free article] [PubMed] [Google Scholar]
- Mitchell SH, de Wit H, Zacny JP. Effects of varying ethanol dose on cigarette consumption in healthy normal volunteers. Behavioural Pharmacology. 1995;6(4):359–365. [PubMed] [Google Scholar]
- Monti P, Rohsenow D, Colby S, Abrams D. Smoking among alcoholics during and after treatment: Implications for models, treatment strategies, and policy. In: Fertig JB, Allen JP, editors. Alcohol and tobacco: From basic science to clinical practice. U.S. Government Printing Office; Washington, DC: 1995. Vol. NIH Publication No 95-3931. [Google Scholar]
- Palfai TP, Monti PM, Ostafin B, Hutchison K. Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. Journal of Abnormal Psychology. 2000;109(1):96–105. doi: 10.1037//0021-843x.109.1.96. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Lang AR. Can your children drive you to drink? Stress and parenting in adults interacting with children with ADHD. Alcohol Research & Health. 1999;23(4):292–298. [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: II. Improved tests of withdrawal-relapse relations. Journal of Abnormal Psychology. 2002;112(1):14–27. [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: I. Abstinence distress in lapsers and abstainers. Journal of Abnormal Psychology. 2003;112(1):3–13. [PubMed] [Google Scholar]
- Piasecki TM, McCarthy DE, Fiore MC, Baker TB. Alcohol Consumption, Smoking Urge, and the Reinforcing Effects of Cigarettes: An Ecological Study. Psychology of Addictive Behaviors. 2008;22(2):230–239. doi: 10.1037/0893-164X.22.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, et al. Smoking withdrawal dynamics in unaided quitters. Journal of Abnormal Psychology. 2000;109(1):74–86. doi: 10.1037//0021-843x.109.1.74. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd Sage; Newbury Park, CA: 2002. [Google Scholar]
- Ray LA, Miranda R, Jr, Kahler CW, Leventhal AM, Monti PM, Swift R, et al. Pharmacological effects of naltrexone and intravenous alcohol on craving for cigarettes among light smokers: A pilot study. Psychopharmacology. 2007;193(4):449–456. doi: 10.1007/s00213-007-0794-z. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Colby SM, Gulliver SB, Sirota AD, Niaura RS, et al. Effects of Alcohol Cues on Smoking Urges and Topography among Alcoholic Men. Alcoholism: Clinical and Experimental Research. 1997;21(1):101–107. [PubMed] [Google Scholar]
- Rose JE, Brauer LH, Behm FM, Cramblett M, Calkins K, Lawhon D. Psychopharmacological interactions between nicotine and ethanol. Nicotine & Tobacco Research. 2004;6(1):133–144. doi: 10.1080/14622200310001656957. [DOI] [PubMed] [Google Scholar]
- Sayette MA. Does drinking reduce stress? Alcohol Research and Health. 1999;23:250–255. [PMC free article] [PubMed] [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Perrott MA, Peters AR. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychology of Addictive Behaviors. 2005;19(3):263–270. doi: 10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf D, Shiffman S. Are there gender differences in smoking cessation, with and without bupropion? Pooled- and meta-analyses of clinical trials of Bupropion SR. Addiction. 2004;99(11):1462–1469. doi: 10.1111/j.1360-0443.2004.00845.x. [DOI] [PubMed] [Google Scholar]
- Shapiro D, Jamner LD, Davydov DM, James P. Situations and moods associated with smoking in everyday life. Psychology of Addictive Behaviors. 2002;16(4):342–345. doi: 10.1037//0893-164x.16.4.342. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: a situational analysis. Journal of Consulting & Clinical Psychology. 1982;50(1):71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological Momentary Assessment (EMA) in Studies of Substance Use. Psychological Assessment. 2009;21(4):486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Fischer LA, Paty JA, Gnys M, Hickcox M, Kassel JD. Drinking and smoking: A field study of their association. Annals of Behavioral Medicine. 1994;16(3):203–209. [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, et al. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal of Abnormal Psychology. 2002;111(4):531–545. doi: 10.1037//0021-843x.111.4.531. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Hufford M, Hickcox M, Paty JA, Gnys M, Kassel JD. Remember that? A comparison of real-time versus retrospective recall of smoking lapses. Journal of Consulting & Clinical Psychology. 1997;65(2):292–300. doi: 10.1037/0022-006x.65.2.292.a. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty J. Smoking patterns and dependence: Contrasting chippers and heavy smokers. Journal of Abnormal Psychology. 2006;115(3):509–523. doi: 10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting & Clinical Psychology. 1996;64(2):366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, the Patient Health Questionnaire Primary Care Study, G. Validation and Utility of a Self-report Version of PRIME-MD: The PHQ Primary Care Study. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Teneggi V, Tiffany S, Squassante L, Milleri S, Ziviani L, Bye A. Smokers deprived of cigarettes for 72 h: effect of nicotine patches on craving and withdrawal. Psychopharmacology. 2002;164(2):177–187. doi: 10.1007/s00213-002-1176-1. [DOI] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clinical Psychology Review. 2006;26(2):128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender Differences in Smoking Cessation. Journal of Consulting & Clinical Psychology. 1999;67(4):555–562. doi: 10.1037//0022-006x.67.4.555. [DOI] [PubMed] [Google Scholar]
- Wetter DW, McClure JB, Cofta-Woerpel L, Costello TJ, Reitzel LR, Businelle MS, et al. A randomized clinical trial of a palmtop computer-delivered treatment for smoking relapse prevention among women. Psychology of Addictive Behaviors. 2011;25:365–371. doi: 10.1037/a0022797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacny JP. Behavioral aspects of alcohol-tobacco interactions. Recent Developments in Alcoholism. 1990;8:205–219. [PubMed] [Google Scholar]