Abstract
Enteric diseases are often caused by poor hygiene and can contribute to stunting. From 50 randomly selected villages in Bangladesh, we collected quantitative and qualitative data on handwashing linked to child feeding to integrate handwashing promotion into a young child complementary feeding program. Most participants stated that the community knew the importance of handwashing with soap before food preparation and feeding a child, but had not developed the habit. We observed no handwashing with soap at these key times; sometimes hands were rinsed with water only. Most participants cited the unavailability of soap and water near the cooking place as a barrier to handwashing before food preparation. Most caregivers ranked nurturing messages as the best motivator to encourage handwashing with soap. An integrated intervention should include having soap and water available near the food preparation area and should use nurturing themes to encourage habitual handwashing with soap.
Introduction
Child malnutrition contributes to more than one-third of the total child mortality globally.1 In Bangladesh, 43% of children less than five years of age meet the World Health Organization criteria for moderate or severe stunting.2,3 Diarrhea, intestinal parasitic infection, and environmental enteropathy are often attributed to poor hygiene,4–6 and may contribute to stunting through chronic gut inflammation and poor absorption of nutrients.7 The World Health Organization and the United Nations Children's Fund recommend the introduction of complementary food starting at six months of age to help promote child growth.3 Studies have shown that diarrheal incidence increases at the age when complementary foods are usually introduced.8–10 Contaminated complementary food is believed to be an important contributor to diarrhea in low-income settings.9,11 Diarrhea is closely associated with the dose of ingested bacteria.12–14 In one study in Bangladesh, 40% of complementary foods were contaminated with a high concentration of pathogenic bacteria.12
Unhygienic preparation of foods can cause contamination. Food contact with unwashed hands can be a source of diarrhea pathogens.8–10 Once complementary foods are contaminated with pathogenic bacteria, the bacteria can rapidly multiply within the foods.15,16 An ethnographic study conducted in Ceará State in northeastern Brazil found that hygiene practices during complementary food preparation was poor and that hands can be a source of food contamination.17
Complementary feeding may not promote optimum childhood growth if consuming contaminated foods result in repeated bouts of illness.18 In rural Bangladesh, children experienced significantly less diarrhea when caregivers washed at least one hand with soap before food preparation compared with children in households where caregivers did not wash hands; 3.7% versus 12.5%.19 Because interventions promoting handwashing with soap reduce childhood diseases consistently,20–23 encouraging caregivers to wash their hands with soap before preparing food and before child feeding may reduce pathogen transmission, reduce illness, and could improve child growth.24
Although in Bangladesh preparing food, serving food, feeding children, and eating food with bare hands is a common practice, most handwashing promotion has focused on fecal contact. There is limited understanding of the determinants of handwashing with soap around food preparation and before child feeding.25 A better understanding of the context of handwashing at these key times could help to develop effective interventions to improve hand hygiene practices. This study aimed to collect baseline data on community perceptions, practices, motivators and barriers to handwashing with soap before food preparation and before child feeding with the purpose of aiding the development of an integrated handwashing and infant and young child feeding intervention.
Materials and Methods
Data collection methods.
During December 2010–January 2011 the field team used a variety of data collection methods, including surveys, observations, structured exercises, in-depth interviews, and focus group discussions to serve different objectives (Table 1). Social scientists, epidemiologists, public health specialists, and statisticians contributed to development of a questionnaire and qualitative guidelines. A sociologist (FAN), along with four anthropologists who had extensive experience in collecting qualitative data, collected the qualitative data. An epidemiologist (LU) led the quantitative data collection.
Table 1.
Data collection methods, Bangladesh
| Instrument (sample size) | Main objective(s) | Type of data collected | Type of question |
|---|---|---|---|
| Survey (350) | To explore knowledge, perceptions, reported practices and barriers to washing hands during food preparation and child feeding, food contamination perceptions | Demographic characteristics of respondents, infant and young child feeding practices, perceived methods to prevent food contamination, perception about handwashing, knowledge of causes of diarrhea, sources and access to information on child health care, and existing handwashing facilities and barriers, sources of information on child health care | Open-ended, statement that ask whether agreed or disagreed, questions for which a yes/no response was required |
| Video data collection of caregivers of children with a mean age of 15 months (12) | To explore actual handwashing practices during food preparation and child feeding | Handwashing practices related to food preparation and child feeding | Not applicable |
| Exercise for ranking motivations for handwashing (6) | To determine respondents' views of themes that could best encourage people to wash hands with soap | Motivational affect in promoting handwashing with soap | Open-ended |
| In-depth interview and focus group discussion of caregivers of children with a mean age of 16 months. In depth interviews (24); focus group discussion (6) with 56 participants (23 males and 33 females) | Similar to the quantitative survey, but focused to understand the context rather than counting frequency. Moreover, focus group discussions focused on community member suggestions on types of messages and communication channels used to disseminate messages | Knowledge about the relationship between hygiene and diseases, perceptions about food contamination, reported handwashing practices, existing handwashing facilities and barriers, sources of information, and ideas to develop messages and intervention | Open-ended |
Study population, sampling, and data collection.
Quantitative survey.
The objectives of the quantitative survey were to explore caregivers' knowledge, perceptions, reported practices and barriers to washing their hands before food preparation and feeding a child. In addition, we explored sources of and access to information on handwashing and preferred communication channels to receive messages.
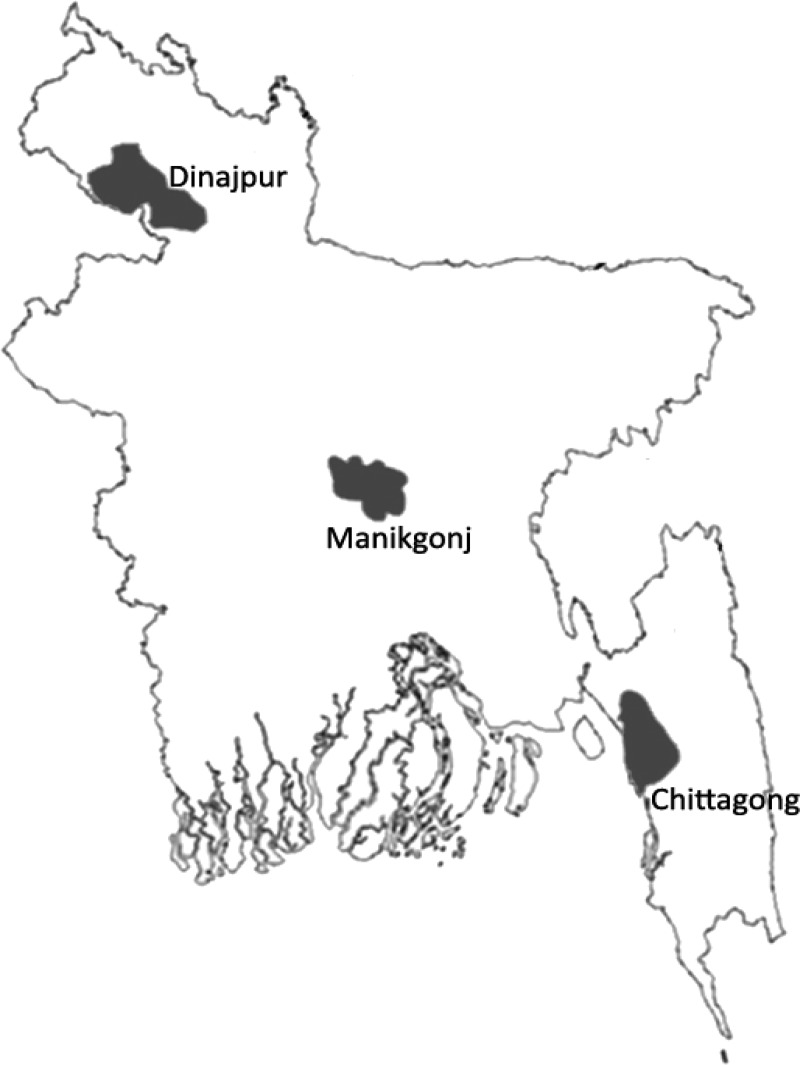
Through a multi-stage sampling process, we randomly selected 50 rural villages within three purposively selected districts situated in different parts in Bangladesh (Chittagong, Dinajpur, and Manikganj Districts) (Figure 1). Based on the population size of the three selected districts, we randomly selected one sub-district from Manikganj District and two sub-districts each from Dinajpur and Chittagong Districts. From each of these five sub-districts, we randomly selected two unions, the subunit of a district, to give a total of 10 unions. Unions with < 10 villages or that were part of an intervention study related to complementary feeding were excluded from the listing used for random selection. From 10 selected unions, we randomly selected 5 villages for a total of 50 villages.
Figure 1.
Bangladesh map and study areas.
For the quantitative survey, we identified the compound (group of houses surrounding a yard with occupants that share a familial relationship and typically share access to water and latrines) at the eastern most extreme of the village. The field team assessed whether there was an eligible household within the compound that had a child 6–24 months of age who was currently receiving complementary food. If so, the field workers invited the child's caregiver to participate in the study. If there was more than one eligible caregiver in the compound, the field worker invited the caregiver of the youngest child to participate. If no household was eligible within that compound, then the field workers proceeded to the next closest compound and again sought to enroll an eligible household. The study team administered a structured questionnaire to each caregiver, which took approximately 45 minutes. This process was repeated at the next closest compound until 7 households were enrolled from the each 50 villages to include a total of 350 caregivers.
Qualitative video data collection.
Video observations preceded other qualitative data collection. The objective of the video observations was to explore actual handwashing practices before food preparation and child feeding. From the 50 villages that had been selected to participate in the survey, we randomly selected 12 villages and then systematically selected one caregiver from each village by starting from the western-most point of the village and enrolling a caregiver from the fifth compound that met the eligibility criteria. If there was more than one eligible caregiver in the compound, the field worker followed the same procedure as for the survey team. If we could not enroll a caregiver from the fifth compound, we moved to the next closest compound until we found an eligible caregiver.
To video record caregiver activities, we recruited community women who had completed at least secondary school to conduct the videotaping. We trained them to use the camera and viewfinder and explained the activities they should focus during the video sessions. We then had each woman make a short trial film to ensure quality. The local videographers recorded caregiver activities for 5–6 hours starting in the early hours of the morning. The field team observed that the early morning was the time when a greater number of activities related to using the toilet, cleaning a child's anus, preparing food, and child feeding occurred.
Ranking motivations for handwashing.
We conducted a ranking activity to explore caregivers' views on the type of themes that would best act as motivators to encourage people to wash their hands with soap. For the ranking activity, we randomly selected 6 caregivers from among the 12 that participated in the video data recording. The day after the video data collection, pictures of persons in different situations that emphasized different motivators for handwashing at key times by eliciting six feelings: nurture, disgust, attraction, affiliation, status, and purity were shown to the caregivers (Hygiene Center's Tools for Schools toolkit; London School of Hygiene and Tropical Medicine, London, United Kingdom). The picture cards also contained text that described a motivation for handwashing, for example, the nurture pictures contained “My child is my pride and joy, I wash my hands to protect my child.” After describing the pictures and text, we asked caregivers to rank each picture according to its motivational effect on promoting handwashing with soap, and to explain why those pictures were motivating.
In-depth interviews.
The objective of the in-depth interviews was to understand community perceptions, practices and barriers to washing hands with soap before food preparation and child feeding. The field team purposively selected eight mothers, eight fathers, and eight grandmothers from different social groups for a total 24 interviews. In each of the 12 villages, the field team selected two eligible informants by using the compounds included for the video component as the starting point and then selecting the subsequent fifth and tenth compound. The field team recorded the in-depth interviews using a digital audio recorder. After 24 in-depth interviews we found data saturation, and no more interviews were conducted.
Focus group discussions.
Focus group discussions aimed to gather community ideas on the types of messages that would be culturally appropriate and the communication channels that could best disseminate handwashing and infant and young child feeding messages. During the focus group discussions, we also collected data on issues raised during in-depth interviews to assess the representativeness of ideas, attitudes, and perceptions that emerged. For the focus groups, we purposively selected six villages in which we had conducted the survey but had not conducted in-depth interviews, videoing, or ranking activity. Three focus group discussions (one focus group per village) were held with family members from eligible households, including mothers, fathers, grandmothers, and grandfathers. Three additional focus group discussions (one focus group in each of the other three villages) took place with community members including religious leaders, village doctors, school teachers, school management committee president or members, community leaders, trained birth attendants, and traditional healers. Eight to 11 persons participated in each focus group discussion.
Data analysis.
Audio recorded data from in-depth interviews and focus group discussions were transcribed in Bengali. We then coded the data using a guideline based on our research objectives. We translated the coded data into English and then manually analyzed and summarized it. Although we analyzed each in-depth interview and each focus group discussion separately, in the findings we have drawn inferences collectively. We reviewed the video observations of recorded handwashing opportunities and behaviors, especially those just before preparing food and feeding a child. For food preparation opportunities, we counted events when foods came into contact with bare hands and were not further cooked, e.g., mashing foods; mixing salad; and events related to cutting vegetables, fish, or meat.
The survey data were analyzed by using Stata/SE 10.0 for Windows (Stata Corp LP, College Station, TX). Summary data were expressed as frequencies (percentages). Differences in proportions were examined using the chi-square test.
Protection of study participants.
We explained the research study objectives to the participants. Before taking part in the study, participants provided written informed consent. The study was reviewed and approved by the Academy for Educational Development Institutional Review Board.
Results
Of the 350 respondents enrolled across the three districts for the quantitative survey, 341 (97%) caregivers were the child's mother, 167 (48%) of the mothers had more than a primary education, and the household monthly income of most (216 of 350, 62%) of households was less than US $100 (8,000 Taka) (Table 2). There were some differences among the participants by district (Table 2). A total of 56 participants (23 males and 33 females) took part in our focus group discussions.
Table 2.
Demographic characteristic of households participating in the survey, Bangladesh
| Characteristic | Manikgonj, n = 70, no. (%) | Dinajpur, n = 140, no. (%) | Chittagong, n = 140, no. (%) | All, n = 350, no. (%) |
|---|---|---|---|---|
| Child caregivers | ||||
| Mother of child | 69 (99) | 134 (96) | 138 (99) | 341 (97) |
| Monthly household income* | ||||
| < US $100 (8,000 Taka) | 26 (37) | 111 (80) | 79 (56) | 216 (62) |
| ≥ US $100 (8,000 Taka) | 44 (63) | 29 (20) | 61 (44) | 134 (38) |
| Education of mother of child* | ||||
| No formal education | 5 (7) | 23 (16) | 39 (28) | 67 (19) |
| Primary level | 31 (44) | 42 (30) | 43 (31) | 116 (33) |
| Above primary level | 34 (49) | 75 (54) | 58 (41) | 167 (48) |
| Education of father of child | ||||
| No formal education | 14 (20) | 38 (27) | 35 (25) | 87 (25) |
| Primary level | 27 (39) | 39 (28) | 46 (33) | 112 (32) |
| Above primary level | 29 (41) | 63 (45) | 59 (42) | 151 (43) |
| Water source for drinking/cooking | ||||
| Tube well | 70 (100) | 140 (100) | 127 (90) | 337 (96) |
| Household sanitation facilities* | ||||
| Improved sanitation | 50 (71) | 61 (44) | 28 (20) | 139 (40) |
| Unimproved sanitation | 20 (29) | 29 (21) | 100 (71) | 149 (43) |
| No latrine access | 0 | 50 (36) | 12 (9) | 62 (18) |
| Household assets* | ||||
| TV | 44 (63) | 37 (26) | 49 (35) | 130 (37) |
| Mobile | 63 (90) | 74 (53) | 104 (74) | 241(69) |
| Bicycle | 16 (23) | 86 (61) | 29 (21) | 131 (37) |
| Motorcycle | 7 (10) | 15 (11) | 4 (3) | 26 (7) |
| Electricity | 53 (76) | 25 (18) | 76 (54) | 154 (44) |
Statistically significantly lower income, fewer assets, and facilities and lower education among households from Dinajpur compared with Manikganj or Chittagong (P < 0.05).
Food contamination, handwashing perceptions, and practices.
During in-depth interviews, although most informants related food contamination with dust or dirt, almost half of the informants also related food contamination with feeding their child without washing hands with soap. Some informants suggested other causes for food contamination such as flies landing on food and not reheating stored food properly (Table 3). Participants in focus group discussions related similar ideas. Of 350 surveyed respondents, the five most frequent methods described to prevent food contamination were washing utensils with soap and water (215, 61%); washing vegetables, fish, and meat (197, 56%); washing hands with soap before feeding a child (192, 55%); cleaning the food preparation area (165, 47%); and washing hands with soap before food preparation (129, 40%). Most informants linked the need for handwashing mainly to remove visible dust/dirt on hands and also to remove germs.
Table 3.
Methods of child food contamination described during in-depth interviews, Bangladesh
| Answers | No. informants* (n = 24) no. (%) |
|---|---|
| Dust/dirt touches food | 18 (75) |
| Feeding child without washing hands with soap | 11 (46) |
| Touching the food with dirty hands | 9 (38) |
| Flies land on food | 9 (38) |
| Stored food is not reheated properly | 9 (38) |
| Leftover food is rotten and becomes contaminated | 3 (13) |
| Animal licks/nibbles the food | 3 (13) |
| Belief that a child's food will be contaminated if the child eats in the presence of non-family members | 2 (8) |
| Vegetables are not washed properly before cooking | 1 (4) |
Multiple responses allowed.
One 50 year-old grandmother from Manikganj said “If someone does not wash hands before feeding then dirt will go into the stomach and it will create disease like diarrhea, dysentery, typhoid, stomachache, and worms.” Another 27-year-old mother from Dinajpur said “When I see that my hands are clean, I don't wash hands. Actually, I wash my hands with soap before cooking and feeding whenever I see dirt in my hands.”
Almost one-fifth of the informants from in-depth interviews reported that they washed their hands with soap before preparing food for a child. During the survey, we asked in an open-ended question “When do you wash your hands with soap?”, 63 (18%) of 350 respondents reported washing hands with soap before preparing food for a child. Among surveyed respondents, when we asked the open-ended question “How and why do children sometimes get diarrhea?”, only 51 (15%) of 350 reported that not washing hands with soap before food preparation and feeding a child could cause diarrhea. However, when we asked “Do you agree or disagree that handwashing with soap and water before preparing a child's food reduces illness”, 336 (96%) of 350 agreed. Most (231 of 350, 66%) surveyed respondents agreed with the statement that “within this community most people are not in the habit of washing their hands with soap before preparing food.” During video observations among the 12 caregivers, we observed 12 opportunities for handwashing with soap before preparing foods (which were not further cooked). In 7 of these 12 opportunities participants did not wash their hands at all, and on 5 opportunities they washed hands with water alone. When we asked the surveyed respondents, “Did you wash your hands with soap before the last episode of child feeding?”, 123 (35%) of 350 said “yes” and almost one-third of the in-depth interview informants reported that they always washed their hands with soap before feeding a child. In the analysis of the video data of 12 caregivers, we observed 27 opportunities for handwashing with soap before feeding a child. However, during 15 of the 27 opportunities, participants did not wash their hands, and during 12 opportunities they washed hands with water alone.
Barriers.
Informants from in-depth interviews and participants of focus group discussions stated that the absence of soap and water near the cooking place was a barrier to handwashing with soap during food preparation. A 27-year-old father from Chittagong District said “soap is not available in the kitchen where my wife prepares food and feeds our child.” A 30-year-old mother of an 11-month-old child from Dinajpur District also stated “My toilet and bathing room are in two different directions…, so I could not wash my hands with soap all the time.”
Informants mentioned other barriers such as lack of habit, lack of understanding of the importance of using soap before food preparation and when feeding a child, and having no previous adverse experience when not washing hands with soap. One 37-year-old man participating in a focus group discussion in Chittagong District explained “People do not have the habit of practicing handwashing with soap. For years people are habituated in washing hands with only water.”
Most (210 of 350, 60%) surveyed respondents agreed with the statement that “the unavailability of soap and water near the cooking place was a physical barrier to handwashing before food preparation.” For 337 (96%) of 350 households surveyed, a shallow tube well located near their home was their water source. Most (312 of 350, 89%) of households found water present at the place that they specified for handwashing before food preparation on the survey day. We observed that 335 (95%) of 350 had soap in their houses but only 128 (37%) of 350 households had soap present at the specific place for handwashing before food preparation. In the survey, 159 (45%) of 350 of the household handwashing places were situated more than 10 steps away from the food preparation area.
Motivators.
In the ranking activity, five of six caregivers ranked the nurturing message as the best motivator to encourage hand washing with soap, and four caregivers ranked the disgusting message as the second best motivator. Participants in the ranking activity said that other motivators could also be helpful to motivate people to wash hands with soap, but the nurturing-related motivators would work best because the child is the first priority to a mother. One 19-year-old mother from Chittagong District stated “If I feed my child without washing hands with soap then filth could enter the child's stomach which can cause child illness. So I need to wash my hands with soap, as I love my baby more than any other thing. This nurture related picture reminds me the same.”
Acceptable and feasible messages and channels.
Focus group participants emphasized that messages could be disseminated through dramas, videos, television programs, cultural programs, and interpersonal communication. One female participant in a focus group discussion in Chittagong District said “It is possible to inform all people through TV. But you have to present it in the advertisement intervals. Especially on Friday and Saturday people enjoy watching films.”
The interviewed informants and focus group participants mentioned that doctors would be the best and most appropriate person to disseminate advice about handwashing. One 26-year-old father from Dinajpur District said “I think the doctor will do this better as people pay attention to them, because doctors belong to the health sector.”
More than half (187 of 350, 53%) of the surveyed respondents mentioned that a visit by a health worker would be the most influential method to disseminate information related to handwashing, child feeding, and food contamination, where 113 (32%) of 350 suggested that television would be the most influential medium. Among surveyed respondents, 134 (38%) of 350 reported that they watched television regularly, and 72 (21%) of 350 reported that they watched television at least once in a week. Among the respondents who watched television, 90 (41%) of 221 reported their favorite programs were dramas and films.
Discussion
Responses from our participants highlighted a contrast in people's minds about the importance of handwashing and food contamination: they related contamination with the introduction of dust/dirt and also with germs but apparently did not consider that hands could be vehicle of germs in the absence of visible dirt. Although a large proportion of surveyed respondents stated the importance of handwashing with soap before food preparation and feeding a child, most reported that the majority of persons in their community were not habituated in this practice. Our observation findings confirmed that persons did not wash their hands with soap before food preparation or before feeding a child, which was similar to other studies also conducted in Bangladesh, in which structured observations of caregivers found that 49% washed their hands with water only and 50% did not wash hands at all.19,26
According to study participants, the availability of soap and water for washing hands at the most convenient location will likely enable handwashing with soap, especially before food preparation and feeding a child. In other contexts, making handwashing easier improved hand hygiene practices,27–29 which is consistent with behavior change theory that stresses the physical environment support as an important component for interventions targeting desired behavior.30–32 The unavailability of soap and water together at food preparation/feeding area may contribute to infrequent handwashing with soap at key times to prevent complementary food contamination. A previous study conducted in rural Bangladesh found that the presence of water and soap at the handwashing place doubled the probability of washing both hands with soap.33 The suggestion by study participants to encourage the installation of a handwashing station (that has flowing water and a source of soap) near food preparation areas might reduce these important barriers, especially because soap was available in almost every home.
Limitations to the study include that we collected data from only three rural sites and among a small number of participants. However, we selected these sites from three different areas of the country, which were typical of Bangladeshi rural communities in terms of water points and latrine facilities (shared tube wells with hand pump, shared latrines, which were both situated outside the household), and we enrolled a mixture of study participants from different social groups. Because our study participants had similar practices, along with similar perceptions about food contamination, barriers to handwashing with soap, what messages motivated practice, and which channels to use to promote handwashing with soap, our findings from this formative study provide a foundation to design a behavior change intervention promoting handwashing with soap applicable to rural setting in Bangladesh.
We collected observation data for this study and the physical presence of an observer can influence practice.34 To minimize the reactivity of using an obvious video camera, we hired and trained a woman from the local community to conduct the video recording, thereby helping the process seem more natural when performed by a neighbor. We expected that this activity might create some excitement in the community and create a positive courtesy bias; instead we observed poor hygiene practices. The video recording did not result in behaviors that were consistent with high levels of handwashing with soap reported during interviews.
To integrate handwashing messages into an infant and young child feeding intervention, our findings on food contamination perceptions and physical barriers to handwashing with soap could be used to frame a behavior change intervention that addresses perceptions and barriers noted within these communities. Our findings suggest that an intervention should include messages to encourage washing hands with soap at each key time during food preparation and child feeding, not only when hands are visibly dirty. Further in-depth study would aid the development of specific messages on handwashing before food preparation, including identifying steps in preparation of common foods when handwashing with soap, should be promoted. To address the physical barriers, the intervention should also encourage persons to make soap and water available in food preparation/feeding areas. Installing a handwashing station near the food preparation area could solve the convenience problem and may enhance the regular practice of handwashing with soap. A handwashing station should have a dedicated container to store water and have a tap for dispensing water. A handwashing agent, such as a soap or soapy water (detergent powder plus water), should also be available. A model with these characteristics has been found acceptable in rural and urban communities in Bangladesh (Solawetz KR and others, unpublished data).
Communication messages should include nurture and disgust motivation themes, ranked by our study respondents as powerful motivators to wash hands; other studies using these motivators have shown that they are effective.35–37 We suggest piloting these messages to test those that are culturally compelling38 and refine accordingly. Because these communities are not habituated with handwashing with soap, we recommend designing and implementing a hygiene behavior change intervention for an extended time to motivate the initiation of handwashing with soap and continue repeated practice in their daily life. This recommendation can help to build a mental construct for habitual handwashing with soap that would automatically occur at these two key times: before food preparation and child feeding.39–42 To develop an effective integrated handwashing and infant and young child feeding intervention, we suggest piloting and iteratively revising the intervention based on ongoing evaluation.
ACKNOWLEDGMENTS
We thank the research officers and research assistants for collecting and processing data, and community members for their time. The International Centre for Diarrhoeal Disease Research acknowledges with gratitude the commitment of Gates Foundation through Alive and Thrive to its research efforts.
Footnotes
Financial support: This study was supported by the Gates Foundation through Alive and Thrive.
Authors' addresses: Fosiul A. Nizame, Leanne Unicomb, Muhammad Nuruzzaman, and Probir K. Ghosh, WATSAN Research Group, Centre for Communicable Diseases, International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh, E-mails: fosiul@icddrb.org, leanne@icddrb.org, nuruzzaman@icddrb.org, and probir@icddrb.org. Tina Sanghvi and Sumitro Roy, Alive and Thrive Program/Family Health International, Dhaka, Bangladesh, E-mails: tsanghvi@fhi360.org and suroy@fhi360.org. Peter J. Winch, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mail: pwinch@jhsph.edu. Stephen P. Luby, Woods Institute of the Environment, Stanford University, Yang and Yamazaki Environment and Energy Building, Stanford, CA, E-mail: sluby@stanford.edu.
References
- 1.World Health Organization Children: Reducing Mortality, Fact Sheet No. 178. 2012. http://www.who.int/mediacentre/factsheets Available at. Accessed June 21, 2012.
- 2.NIPORT . Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh: National Institute of Population Research and Training; and Calverton, MD: Mitra and Associates and MEASURE DHS, ICF International; 2011. [Google Scholar]
- 3.World Health Organization . Global Strategy for Infant and Young Child Feeding. Geneva: World Health Organization; 2003. [Google Scholar]
- 4.Montville R, Chen Y, Schaffner DW. Glove barriers to bacterial cross-contamination between hands to food. J Food Prot. 2001;64:845–849. doi: 10.4315/0362-028x-64.6.845. [DOI] [PubMed] [Google Scholar]
- 5.Lin A, Arnold BF, Afreen S, Goto R, Huda TM, Haque R, Raqib R, Unicomb L, Ahmed T, Colford JM, Jr, Luby SP. Household environmental conditions are associated with enteropathy and impaired growth in rural Bangladesh. Am J Trop Med Hyg. 2013;89:130–137. doi: 10.4269/ajtmh.12-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNICEF . Mapping India's Children: UNICEF in Action. New Delhi, India: UNICEF; 2004. pp. 32–64. [Google Scholar]
- 7.Humphrey JH. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet. 2009;374:1032–1035. doi: 10.1016/S0140-6736(09)60950-8. [DOI] [PubMed] [Google Scholar]
- 8.Mattioli MC, Pickering AJ, Gilsdorf RJ, Davis J, Boehm AB. Hands and water as vectors of diarrheal pathogens in Bagamoyo, Tanzania. Environ Sci Technol. 2013;47:355–363. doi: 10.1021/es303878d. [DOI] [PubMed] [Google Scholar]
- 9.Motarjemi Y, Kaferstein F, Moy G, Quevedo F. Contaminated weaning food: a major risk factor for diarrhoea and associated malnutrition. Bull World Health Organ. 1993;71:79–92. [PMC free article] [PubMed] [Google Scholar]
- 10.Ehiri JE, Azubuike MC, Ubbaonu CN, Anyanwu EC, Ibe KM, Ogbonna MO. Critical control points of complementary food preparation and handling in eastern Nigeria. Bull World Health Organ. 2001;79:423–433. [PMC free article] [PubMed] [Google Scholar]
- 11.Esrey SA. Food contamination and diarrhoea. World Health. 1990;Jan–Feb:19–20. [Google Scholar]
- 12.Islam MA, Ahmed T, Faruque AS, Rahman S, Das SK, Ahmed D, Fattori V, Clarke R, Endtz HP, Cravioto A. Microbiological quality of complementary foods and its association with diarrhoeal morbidity and nutritional status of Bangladeshi children. Eur J Clin Nutr. 2012;66:1242–1246. doi: 10.1038/ejcn.2012.94. [DOI] [PubMed] [Google Scholar]
- 13.Kothary MH, Babu US. Infective dose of food borne pathogens in volunteers: a review. J Food Saf. 2001;21:49–73. [Google Scholar]
- 14.Levine MM, Black RR, Clements ML, Nalin DR, Cisneros L, Finkelstein RA. Volunteer studies in development of vaccines against cholera and enterotoxigenic Escherichia coli: a review. In: Holme T, Holmgren J, Merson MH, Mollby R, editors. Acute Enteric Infections in Children: New Prospects for Treatment and Prevention. Elsevier/North-Holland Biomedical Press; 1981. pp. 443–459. [Google Scholar]
- 15.Islam MS, Hasan MK, Khan SI. Growth and survival of Shigella flexneri in common Bangladeshi foods under various conditions of time and temperature. Appl Environ Microbiol. 1993;59:652–654. doi: 10.1128/aem.59.2.652-654.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kolvin JL, Roberts D. Studies on the growth of Vibrio cholerae biotype El Tor and biotype classical in foods. J Hyg (Lond) 1982;89:243–252. doi: 10.1017/s0022172400070777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monte CM, Ashworth A, Nations MK, Lima AA, Barreto A, Huttly SR. Designing educational messages to improve weaning food hygiene practices of families living in poverty. Soc Sci Med. 1997;44:1453–1464. doi: 10.1016/s0277-9536(96)00241-9. [DOI] [PubMed] [Google Scholar]
- 18.Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr. 2008;4((Suppl 1)):24–85. doi: 10.1111/j.1740-8709.2007.00124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luby SP, Halder AK, Huda T, Unicomb L, Johnston RB. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: an observational study. PLoS Med. 2011;8:e1001052. doi: 10.1371/journal.pmed.1001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, Hoekstra RM. Effect of handwashing on child health: a randomised controlled trial. Lancet. 2005;366:225–233. doi: 10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]
- 21.Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98:1372–1381. doi: 10.2105/AJPH.2007.124610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts L, Smith W, Jorm L, Patel M, Douglas RM, McGilchrist C. Effect of infection control measures on the frequency of upper respiratory infection in child care: a randomized, controlled trial. Pediatrics. 2000;105:738–742. doi: 10.1542/peds.105.4.738. [DOI] [PubMed] [Google Scholar]
- 23.Niffenegger JP. Proper handwashing promotes wellness in child care. J Pediatr Health Care. 1997;11:26–31. doi: 10.1016/s0891-5245(97)90141-3. [DOI] [PubMed] [Google Scholar]
- 24.Scrimshaw NS, SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr. 1997;66:464S–477S. doi: 10.1093/ajcn/66.2.464S. [DOI] [PubMed] [Google Scholar]
- 25.Usfar AA, Iswarawanti D, Davelyna D, Dillon D. Food and personal hygiene perceptions and practices among caregivers whose children have diarrhea: a qualitative study of urban mothers in Tangerang, Indonesia. J Nutr Educ. 2010;42 doi: 10.1016/j.jneb.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Halder AK, Tronchet C, Akhter S, Bhuiya A, Johnston R, Luby SP. Observed hand cleanliness and other measures of handwashing behavior in rural Bangladesh. BMC Public Health. 2010;10:545. doi: 10.1186/1471-2458-10-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaplan LM, McGuckin M. Increasing handwashing compliance with more accessible sinks. Infect Control. 1986;7:408–410. doi: 10.1017/s019594170006464x. [DOI] [PubMed] [Google Scholar]
- 28.Graham M. Frequency and duration of handwashing in an intensive care unit. Am J Infect Control. 1990;18:77–81. doi: 10.1016/0196-6553(90)90085-7. [DOI] [PubMed] [Google Scholar]
- 29.Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Handwashing compliance by health care workers: the impact of introducing an accessible, alcohol-based hand antiseptic. Arch Intern Med. 2000;160:1017–1021. doi: 10.1001/archinte.160.7.1017. [DOI] [PubMed] [Google Scholar]
- 30.Story M, Neumark-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102((Suppl)):S40–S51. doi: 10.1016/s0002-8223(02)90421-9. [DOI] [PubMed] [Google Scholar]
- 31.Gielen AC, Sleet D. Application of behavior-change theories and methods to injury prevention. Epidemiol Rev. 2003;25:65–76. doi: 10.1093/epirev/mxg004. [DOI] [PubMed] [Google Scholar]
- 32.Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93:1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luby SP, Halder AK, Tronchet C, Akhter S, Bhuiya A, Johnston RB. Household characteristics associated with handwashing with soap in rural Bangladesh. Am J Trop Med Hyg. 2009;81:882–887. doi: 10.4269/ajtmh.2009.09-0031. [DOI] [PubMed] [Google Scholar]
- 34.Cousens S, Kanki B, Toure S, Diallo I, Curtis V. Reactivity and repeatability of hygiene behaviour: structured observations from Burkina Faso. Soc Sci Med. 1996;43:1299–1308. doi: 10.1016/0277-9536(95)00380-0. [DOI] [PubMed] [Google Scholar]
- 35.Porzig-Drummond R, Stevenson R, Case T, Oaten M. Can the emotion of disgust be harnessed to promote hand hygiene? Experimental and field-based tests. Soc Sci Med. 2009;68:1006–1012. doi: 10.1016/j.socscimed.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 36.Scott BE, Schmidt WP, Aunger R, Garbrah-Aidoo N, Animashaun R. Marketing hygiene behaviours: the impact of different communication channels on reported handwashing behaviour of women in Ghana. Health Educ Res. 2007;22:225–233. doi: 10.1093/her/cym056. [DOI] [PubMed] [Google Scholar]
- 37.Scott BE, Curtis V, Rabie T, Garbrah-Aidoo N. Health in our hands, but not in our heads: understanding hygiene motivation in Ghana. Health Policy Plan. 2007;22:225–233. doi: 10.1093/heapol/czm016. [DOI] [PubMed] [Google Scholar]
- 38.Panter-Brick C, Clarke SE, Lomas H, Pinder M, Lindsay SW. Culturally compelling strategies for behaviour change: a social ecology model and case study in malaria prevention. Soc Sci Med. 2006;62:2810–2825. doi: 10.1016/j.socscimed.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 39.Wood W, Tam L, Witt MG. Changing circumstances, disrupting habits. J Pers Soc Psychol. 2005;88:918–933. doi: 10.1037/0022-3514.88.6.918. [DOI] [PubMed] [Google Scholar]
- 40.Wood W, Neal DT. A new look at habits and the habit–goal interface. Psychol Rev. 2007;114:843–863. doi: 10.1037/0033-295X.114.4.843. [DOI] [PubMed] [Google Scholar]
- 41.Verplanken B, Orbell S. Reflections on past behavior: a self-report index of habit strength. J Appl Soc Psychol. 2003;33:1313–1330. [Google Scholar]
- 42.Verplanken B. Beyond frequency: habit as mental construct. Br J Soc Psychol. 2006;45:639–656. doi: 10.1348/014466605X49122. [DOI] [PubMed] [Google Scholar]