Abstract
Fascioliasis is a zoonotic infestation caused by the trematode fasciola hepatica. It presents a wide spectrum of clinical pictures ranging from fever and eosinophilia to ambiguous gastrointestinal symptoms in the acute phase. However, it may often be overlooked, especially in the acute phase, because of uncertain symptoms. Fasciola hepatica can have an initial presentation similar to the presentation of malignancy. Here, we report a case of a hepatic mass caused by fasciola hepatica.
Introduction
Fasciola hepatica, a parasitic flatworm of the class Trematoda, Phylum Platyhelminthes that infects the livers of various mammals, including humans, is exceptionally rare in the United States. However, it is commonly observed in developing countries. The incidence has been increasing since the year 1980. Food-borne trematodiases are a group of neglected tropical diseases.1 The parasite has a complex lifecycle that includes a hepatic phase as well as a biliary phase. In the hepatic phase, the parasite is reported to remain within the liver for 6–9 weeks.2 The triad of fever, right upper quadrant pain, and absolute peripheral blood eosinophilia should raise suspicion of hepatic fascioliasis.3 Here, we present a case of a hepatic mass caused by fasciola hepatica that was initially thought to be a hepatic malignancy.
Case Report
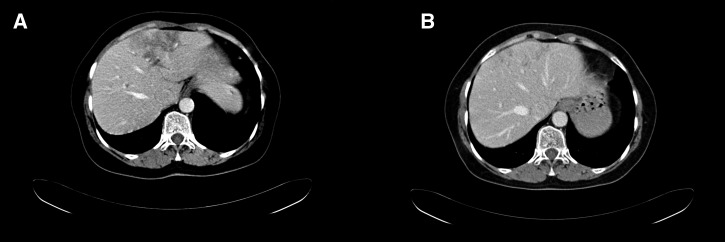
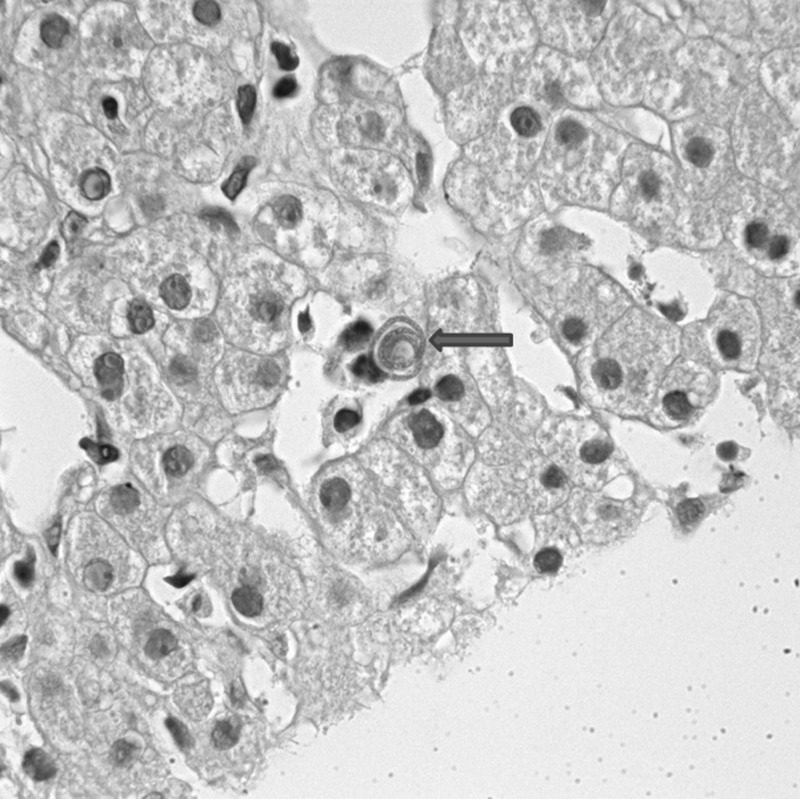
A 48-year-old woman was investigated for abdominal discomfort. The patient with no previous symptoms presented with back pain and abdominal distension. The patient's symptoms had been continuously increasing for the past 5 years. The patient had lost 12 pounds in the past 6 months. The patient also had concurrent nausea and lack of appetite. The patient was first admitted to another hospital, where an ultrasonography (USG) and an abdominal computed tomography (CT) were performed. The USG showed a 38 × 29-mm mass. The CT imaging confirmed this finding by revealing a 3 × 4-cm hypodense lesion in the left lobe of the liver. Also, at the hilus of the liver, a 31-mm lymph node was identified. The imaging studies were repeated after presentation to our institution. The initial pre-treatment CT imaging revealed a 7 × 5.5-cm hypodense solid mass present in the liver segments 2–3 and 4. The mass also was found to cause biliary distension in the left lobe. Furthermore, lymphadenopathy was identified, with the largest lymph node being 2.7 cm in diameter in the portacaval region (Figure 1A ). A complete blood count was performed that revealed eosinophilia (2,900/mm3, N: 0–400/mm3, 36% of leukocytes), which led to the suspicion of a parasitic infection. To establish a definite diagnosis, a biopsy was performed. In the pathological examination, partially granulamatous lesions that consisted entirely of eosinophils and very few mononuclear cells were identified. In the parenchyme, concentric parasite-like structures were observed (Figure 2 ). With a differential diagnosis of fasciola hepatica, serology using Falcon screening test enzyme-linked immunosorbent assay (FAST-ELISA) was performed that established the final diagnosis. Antiparasitic therapy using triclabendazole was initiated. The patient was then discharged and asked to return 3 months later for follow-up. A follow-up CT scan was performed that showed regression of both the mass and the lymphadenopathy (Figure 1B).
Figure 1.
(A) Abdominal CT examination showed a 7 × 5.5-cm hypodense solid mass present in the liver. (B) A follow-up CT scan showed regression of the liver mass.
Figure 2.
A liver biopsy was evaluated for eosinophilic granuloma and concentric parasite-like structures.
Discussion
Fascioliasis is uncommon in developed countries but more commonly seen in developing countries. The identification of fasciola hepatica eggs in the stool is a standard method for the diagnosis of fascioliasis. The parasites do not pass eggs in the acute stage of the disease before they become adults, although the symptoms of the disease are the most severe at this time. Additionally, parasite eggs may not be detected when the parasite lays eggs in intervals, which was observed in cases of chronic fascioliasis, when the parasite has an ectopic location.4 Humans are infected by eating water plants. Fascioliasis may cause a wide variety of clinical signs ranging from asymptomatic infection to severe liver cirrhosis. Fasciola hepatica has two phases: the acute (hepatic) and chronic (biliary) phases. Nausea, fever, right hypochondrium pain, hepatomegali, and hypereosinophilia with or without urticaria are seen in the acute phase.5 However, in the chronic phase, worms or eggs may obstruct the extrahepatic biliary ducts, causing symptoms of biliary tree obstruction. Also, invasion of the gallbladder may cause colelithiasis-like symptoms. In the majority of cases, diagnosis of infection as the acute or chronic phase is difficult, because the symptoms of both phases overlap. In non-endemic areas, diagnosis of fascioliasis can be difficult and usually is delayed, because the disease is not often encountered; also, the symptoms may be confused with other hepatic or biliary disorders.6 Extrahepatopancreatobiliary sites of infection can also occur. Many cases of ectopic fascioliasis have been reported in the literature. There are reported cases of invasion of the heart, brain, lungs, skin, eye, stomach, and intestinal wall and presentation as visceral larva migrans.7
Serologic tests that are essential for diagnosing acute fascioliasis include FAST-ELISA, indirect hemagglutination, complement fixation, indirect immunofluorescence (IIF), counterelectrophoresis, and double diffusion. However, despite the fact that these tests are quite sensitive, they may cross-react with other parasitic infections, such as echinococcus, which is relatively common in Turkey.8 Immunoserological tests are valuable in the early hepatic stage, but ELISA testing is more rapid and reliable.9 Successful treatment correlates with a decline in ELISA titers, with antibodies detectable for years after infection. FAST-ELISA has a sensitivity rate of 95%, although the exact specificity has not been determined.10,11
Triclabendazole has been shown to be very effective against fasciola hepatica infections. The drug is administered at a dose of 10 mg/kg for 1 or 2 days, and it is well-tolerated. We followed a similar treatment protocol.12
While evaluating patients with liver masses with concurrent hypereosinophilia, it is important include parasitic infections in the differential diagnosis, especially in patients residing in or coming from developing nations. Our patient was initially considered to be a case of primary or secondary hepatic malignancy. However, serological studies performed after the pathological examination revealed a parasitic infection. Triclabendazole was administered, which resulted in a complete regression of the radiologically identified mass.
Footnotes
Authors' addresses: Bülent Yılmaz and Seyfettin Köklü, Department of Gastroenterology, Hacettepe University School of Medicine, Ankara, Turkey, E-mails: bulent.yilmaz@hacettepe.edu.tr and gskoklu@yahoo.com. Gökhan Gedikoğlu, Department of Pathology, Hacettepe University School of Medicine, Ankara, Turkey, E-mail: gokhan@gmail.com.
References
- 1.Fürst T, Keiser J, Utzinger J. Global burden of human food-borne trematodiasis: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:210–221. doi: 10.1016/S1473-3099(11)70294-8. [DOI] [PubMed] [Google Scholar]
- 2.Yen TJ, Hsiao CH, Hu RH, Liu KL, Chen CH. Education and imaging: hepatobiliary and pancreatic: chronic hepatic abscess associated with fascioliasis. J Gastroenterol Hepatol. 2011;26:611. doi: 10.1111/j.1440-1746.2011.06679.x. [DOI] [PubMed] [Google Scholar]
- 3.Arslan F, Batirel A, Samasti M. Fascioliasis: 3 cases with three different clinical presentations. Turk J Gastroenterol. 2012;23:267–271. doi: 10.4318/tjg.2012.0388. [DOI] [PubMed] [Google Scholar]
- 4.Apt W, Aguilera X, Vega F, Miranda C, Zulantay I, Perez C, Gabor M, Apt P. Treatment of human chronic fascioliasis with triclabendazole: drug efficacy and serologic response. Am J Trop Med Hyg. 1995;52:532–535. doi: 10.4269/ajtmh.1995.52.532. [DOI] [PubMed] [Google Scholar]
- 5.Marcos LA, Tagle M, Terashima A, Bussalleu A, Ramirez C, Carrasco C, Valdez L, Huerta-Mercado J, Freedman DO, Vinetz JM. Natural history, clinicoradiologic correlates, and response to triclabendazole in acute massive fascioliasis. Am J Trop Med Hyg. 2008;78:222. [PubMed] [Google Scholar]
- 6.Kaya M, Beştaş R, Cetin S. Clinical presentation and management of Fasciola hepatica infection: single-center experience. World J Gastroenterol. 2011;28:4899–4904. doi: 10.3748/wjg.v17.i44.4899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rashed AA, Khalil HH, Morsy AT. Zoonotic ectopic fascioliasis: review and discussion. J Egypt Soc Parasitol. 2010;40:591–608. [PubMed] [Google Scholar]
- 8.Apt W, Aguilera X, Vega F, Miranda C, Zulantay I, Perez C, Gabor M, Apt P. Treatment of human chronic fascioliasis with triclabendazole: drug efficacy and serologic response. Am J Trop Med Hyg. 1995;52:532–534. doi: 10.4269/ajtmh.1995.52.532. [DOI] [PubMed] [Google Scholar]
- 9.Espinoza JR, Maco V, Marcos L, Saez S, Neyra V, Terashima A, Samalvides F, Gotuzzo E, Chavarry E, Huaman MC, Bargues MD, Valero MA, Mas-Coma S. Evaluation of Fas2-ELISA for the serological detection of Fasciola hepatica infection in humans. Am J Trop Med Hyg. 2007;76:977–982. [PubMed] [Google Scholar]
- 10.Hillyer GV, Soler de Galanes M, Rodriguez-Perez J, Bjorland J, Silva de Lagrava M, Ramirez Guzman S, Bryan RT. Use of the Falcon assay screening test-enzyme-linked immunosorbent assay (FAST-ELISA) and the enzyme-linked immunoelectrotransfer blot (EITB) to determine the prevalence of human fascioliasis in the Bolivian Altiplano. Am J Trop Med Hyg. 1992;46:603. doi: 10.4269/ajtmh.1992.46.603. [DOI] [PubMed] [Google Scholar]
- 11.Carnevale S, Rodriguez MI, Santillan G, Labbe JH, Cabrera MG, Bellegarde EJ, Velasquez JN, Trgovcic JE, Guarnera EA. Immunodiagnosis of human fascioliasis by an enzymelinked immunosorbent assay (ELISA) and a micro-ELISA. Clin Diagn Lab Immunol. 2001;8:174–177. doi: 10.1128/CDLI.8.1.174-177.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization Fascioliasis Infection with the “Neglected” Neglected Worms. 2009. http://www.who.int/neglected_diseases/integrated_media/integrated_media_fascioliasis/en/index.html Available at. Accessed June 4, 2011.