Abstract
Traumatic abdominal wall hernias (TAWHs) are rare. They can arise from either high or low impact trauma and can be associated with significant associated injury. We present the case of a 27-year-old male involved in a high-impact road traffic accident resulting in a TAWH. He sustained significant disruption to the abdominal wall and sustained injuries to the thoracic cage. Operative management was undertaken with a porcine dermal collagen mesh, using a bridge technique.
INTRODUCTION
Traumatic abdominal wall hernia (TAWH) has been defined as ‘herniation through disrupted musculature and fascia associated with adequate trauma, without skin penetration, and no evidence of a prior hernia defect at the site of injury’ [1]. They are rare and over the past century ∼50 have been reported in the literature [2]. TAWH predominantly affect men of working age and can have a significant socioeconomic impact.
Debate surrounds management strategies. Some reports advocate a conservative approach with operative intervention at a later stage if indicated, whereas others have promoted immediate surgical intervention. We present a case of a 27-year-old male with significant disruption to his anterior abdominal wall with associated thoracoabdominal injuries who was managed operatively.
CASE REPORT
A 27-year-old male with no past medical history was the driver and sole occupant of a car which crashed through a fence at 80 kph and hit a lamp post. He was wearing a seatbelt, the airbags did not deploy and despite the significant intrusion into the passenger space, he extricated himself unaided. He was resuscitated according to Advanced Trauma Life Support® principles. The primary survey identified decreased air entry at the base of the right lung and right-sided abdominal and lower chest tenderness. Abrasions were evident over the anterolateral abdominal wall and a large, right-sided abdominal swelling was noted.
Trauma series computed tomography (CT) scans demonstrated a flail segment between the sixth and eight ribs with disruption of the intercostal muscles and a small right haemothorax (Fig. 1a). In the abdomen, there was hepatic contusion with an intrinsic liver injury (Fig. 1b). Blood was noted around the liver with minor active haemorrhage. The right abdominal wall was ruptured—the right rectus abdominis muscle had been torn from its costal attachments to the midpoint. The hepatic flexure of the colon had herniated through the intercostal muscles of the eighth and ninth ribs and was lying adjacent to the fractured ribs (Fig. 1c). Both small and large bowel had herniated through the abdominal wall lateral to rectus abdominis, but remained covered by external oblique (Fig. 1d). Herniation of small and large bowel immediately adjacent to the fractured ribs raised the suspicion of occult bowel injury not detected on CT.
Figure 1:
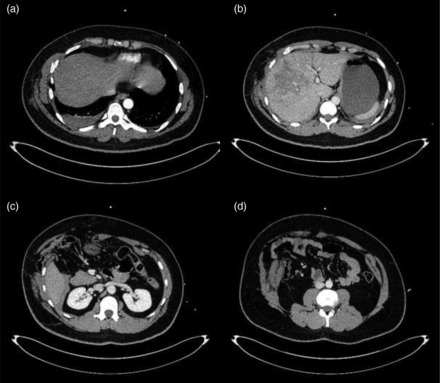
(a–d) Initial CT imaging performed as part of the secondary survey.
The operative management was undertaken by both thoracic and abdominal surgeons. The ribs were re-opposed with absorbable polyglycolic acid sutures and a chest drain inserted. At laparotomy, it was noted that the hernia sac contained omentum, the bowel having reduced spontaneously under general anaesthesia. A small rent in the mesentery of the proximal small bowel was noted. The abdominal defect was repaired with a 20 × 30 cm sheet of cross-linked acellular porcine dermal collagen (Permacol™, Covidien, Gosport, Hants, UK) which was sutured to the margins of the fascial defect with interrupted nylon sutures, using a ‘bridge’ technique, with a 5-cm underlay on the left.
Post-operatively, the patient was managed in the intensive care unit for 24 h. A seroma that developed at the hernia site after 1 week was treated conservatively. Impaired abdominal wall function, particularly reduced mobility, was noted post-operatively. Sitting up from lying down position and hip flexion caused difficulty, but improved with intensive physiotherapy. He was discharged home 9 days after admission.
Six weeks after discharge, he was well with good mobility. He had a persistent seroma at the hernia site. A repeat CT of the thorax and abdomen at 10 weeks demonstrated no residual defect in the anterior abdominal wall and resolution of the seroma (Fig. 2).
Figure 2:
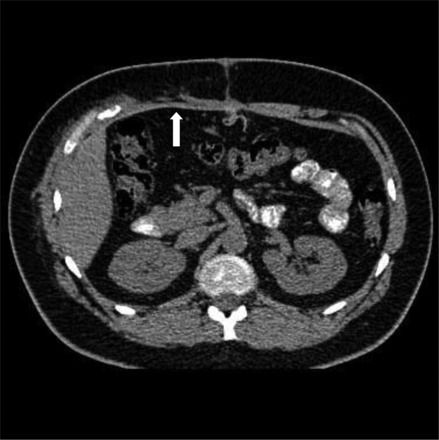
CT at 10 weeks after the injury and primary repair. The mesh is seen in the anterior abdominal wall (arrow).
DISCUSSION
TAWH remains a rare clinical entity and insufficient evidence exists to provide clear protocols for surgical management. There are three key issues in managing this condition: whether to operate or not, which reconstructive technique to use and which mesh to use, if any.
Operative vs conservative management
There are case reports where a conservative approach has been adopted, although these are mainly in the paediatric group and are secondary to handlebar type injuries with minimal disruption to the abdominal cavity [3, 4]. A conservative or delayed operative management strategy for low energy TAWH may be feasible, but high-energy TAWH are often associated with significant intra-abdominal injuries and an operative approach via midline laparotomy has been advocated [5].
Reconstructive technique
For incisional hernia repair, the use of mesh has become the gold standard because of a significant reduction in recurrence rates compared with primary suture repair. Synthetic meshes are, however, associated with complications including erosion, fistulation and chronic infection. Due to the potential for contamination in cases of high-energy TAWH repair, a primary suture repair technique has been recommended by some authors because of the high (50%) wound infection rate even when mesh was not used [5]. Primary suture repair may not be feasible if there is substantial domain loss. It would also be contraindicated if the lateral abdominal wall muscles have retracted and require component separation, as in our case.
Which mesh?
The potential for contamination, high rates of wound infection and the need to place mesh adjacent to recently herniated bowel raises a debate between the merits of synthetic and biologic meshes. Abdominal wall repair with both absorbable and non-absorbable synthetic meshes in the presence of contamination has led to high rates of mesh infection, fistulation and even death [6]. Biologic meshes provide a collagen scaffold for native tissue to infiltrate and they are remodelled over time. A recent systematic review has demonstrated that cross-linked biologic meshes can be used with low rates of hernia recurrence and few complications [7]. We utilized cross-linked acellular porcine dermis (Permacol™, Covidien, Gosport, Hants, UK), which has been reported to have a degree of resistance to bacterial collagenase activity and the optimum durability for effective hernia repair whilst still allowing native tissue ingrowth [8].
High-energy TAWH present a considerable surgical challenge. Management strategies should be tailored to the individual patient, but tend to favour operative intervention. In view of the high risk of wound infection, biologic meshes may be helpful in the repair of such hernias.
REFERENCES
- 1.Damschen DD, Landercasper J, Cogbill TH, Stolee RT. Acute Traumatic abdominal hernia: case reports. J Trauma. 1994;36:273–6. doi: 10.1097/00005373-199402000-00026. doi:10.1097/00005373-199402000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Henrotay J, Honoré C, Meurisse M. Traumatic abdominal wall hernia: case report and review of the literature. Acta Chir Belg. 2010;110:471–4. doi: 10.1080/00015458.2010.11680658. [DOI] [PubMed] [Google Scholar]
- 3.Yan J, Wood J, Bevan C, Cheng W, Wilson G. Traumatic abdominal wall hernia—a case report and literature review. J Pediatr Surg. 2011;46:1642–5. doi: 10.1016/j.jpedsurg.2011.04.004. doi:10.1016/j.jpedsurg.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Litton k, Izzidien AY, Hussien O, Vali A. Conservative management of a traumatic abdominal wall hernia after a bicycle handlebar injury (case report and literature review) J Pediatr Surg. 2008;43:e31–2. doi: 10.1016/j.jpedsurg.2007.12.059. doi:10.1016/j.jpedsurg.2007.12.059. [DOI] [PubMed] [Google Scholar]
- 5.Lane CT, Cohen AJ, Cinat ME. Management of traumatic abdominal wall hernia. Am Surg. 2003;69:73–6. [PubMed] [Google Scholar]
- 6.Van't Riet M, de Vos van Steenwijk PJ, Bonjer HJ, Steyerberg EW, Jeekel J. Mesh repair for postoperative wound dehiscence in the presence of infection: is absorbable mesh safer than non-absorbable mesh? Hernia. 2007;11:409–13. doi: 10.1007/s10029-007-0240-5. doi:10.1007/s10029-007-0240-5. [DOI] [PubMed] [Google Scholar]
- 7.Smart NJ, Marshall M, Daniels IR. Biologic meshes: a review of their use in abdominal wall hernia repairs. Surgeon. 2012;10:159–71. doi: 10.1016/j.surge.2012.02.006. doi:10.1016/j.surge.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Smart NJ, Bloor S. Durability of biologic implants for use in hernia repair: a review. Surg Innov. 2012;19:221–9. doi: 10.1177/1553350611429027. [DOI] [PubMed] [Google Scholar]


