Abstract
A common trunk of the left pulmonary vein is an anatomical variation in the pulmonary vessels and may be incidentally transected during left upper lobectomy. Difficulty in reconstruction of the left inferior vein often requires completion pneumonectomy. We herein describe a patient with lung cancer in the left upper lobe of the lung. His common trunk of the left pulmonary vein was incidentally transected with a mechanical stapler during a thoracoscopic left upper lobectomy. The concomitantly transected inferior pulmonary vein was augmented with a cuff technique using an orifice of the superior vein followed by end-to-end anastomosis. The postoperative course was uneventful. This technique should also be considered in patients with lung cancer when a right upper lobe tumor is invading the right superior trunk branching pulmonary veins to the upper and middle lobes.
INTRODUCTION
There is a wide range of anatomical variations in the pulmonary vessels. Incidental vessel injury caused by some of these variations may require more extensive lung resection than would be necessary without repair during pulmonary resection.
We herein describe a patient with a common trunk of the left pulmonary vein that was incidentally transected with a mechanical stapler during a left upper lobectomy. We also describe the reconstruction procedures that were successfully used for the concomitantly transected inferior pulmonary vein.
CASE REPORT
A 62-year-old man complained of cough and bloody sputum and consulted our hospital. Chest computed tomography (CT) showed a nodule with a diameter of 15 mm in the left upper lobe. Pathologic study of a specimen obtained by transbronchial biopsy showed small cell lung cancer. Positron emission tomography and brain magnetic resonance imaging revealed a clinical stage of T1N0M0 as categorized by the 7th edition of the union for international cancer control (UICC) classification.
Thoracoscopic left upper lobectomy was performed. The common trunk of the left pulmonary vein was misidentified as a superior pulmonary vein until incidental transection with an endostapler during port access surgery. The caliber change between the common trunk and the inferior pulmonary vein was marked. Thoracoscopic surgery was converted to open thoracotomy. The left upper bronchus and pulmonary arteries to the left upper lobe were transected with endostaplers, and the common trunk of the pulmonary vein was left intact. The left main pulmonary artery was then clamped under intravenous heparin injection to achieve an activated coagulation time of 200 s. Annuloplasty of the inferior pulmonary vein was completed during intermittent declamping of the left pulmonary artery. The orifice of the inferior pulmonary vein was augmented by a cuff technique using an orifice of the superior pulmonary vein, as shown in Fig. 1. The staples on the stump of the left common pulmonary vein on the atrial side were removed to adjust the augmented orifice of the left inferior pulmonary vein under partial clamping of the left atrium following pericardiectomy. End-to-end anastomosis was completed using running sutures with a 4-0 polypropylene thread. The anticoagulant therapy was continued until 2 months after surgery. The postoperative course was uneventful, and the patient was discharged on postoperative day 14. A pathologic study showed stage T1N2M0 small-cell carcinoma as categorized by the 7th edition of the UICC classification. Postoperative enhanced CT demonstrated successful reconstruction of the left common trunk (Fig. 2).
Fig. 1.
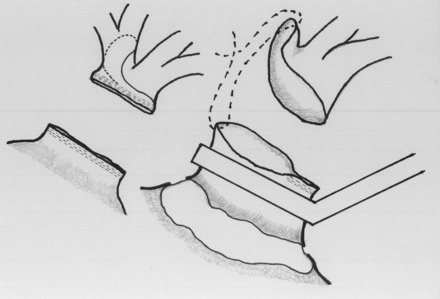
Orifice of an inferior pulmonary vein was augmented with a cuff technique using the orifice of a superior pulmonary vein. The augmented orifice was anastomosed to the common pulmonary vein on the left atrial side after removal of staples as long as necessary under a partial clamp of the left atrium following pericardiotomy.
Fig. 2.
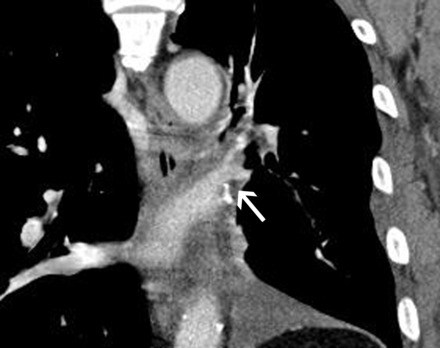
Postoperative enhanced CT showing (frontal view) successful reconstruction of an inferior pulmonary vein (arrow).
DISCUSSION
The branching pattern of the pulmonary vessels is variable. Pulmonary vein variations such as upper lobe venous drainage posterior to the intermediate bronchus [1] and a common trunk of the left pulmonary vein [2] may cause lethal complications during and after anatomical pulmonary resection. Based on CT findings, a common trunk of the left pulmonary vein reportedly occurred with a frequency of 14% among 201 cases [3]. Although three-dimensional CT and multidetector CT have been developed to detect pulmonary vessel variations preoperatively, incidental transection of the common trunk may be unavoidable when the pulmonary vein is anteriorly transected with no identification of the inferior vein during left upper lobectomy. Furthermore, the use of video-assisted surgery and endoscopic devices has become more widespread, and skin incisions and exposure of anatomical structures have become more limited [2]. The inferior pulmonary vein should always be identified during left upper lobectomy. A previous paper reported that the orifice of the inferior pulmonary vein was augmented with the use of a pericardial patch followed by anastomosis when the common trunk was incidentally transected [2]. In this report, annuloplasty of the inferior pulmonary vein with a cuff technique using an orifice of the superior pulmonary vein allowed for much easier performance of end-to-end anastomosis, leading to successful reconstruction without a patch or prosthesis. This augmented technique may also be applicable to patients with lung cancer in the right upper lobe when the tumor is invading the right common superior trunk branching pulmonary veins to the upper and middle lobes.
References
- 1.Asai K, Urabe N, Yajima K, Suzuki K, Kazui T. Right upper lobe venous drainage posterior to the bronchus intermedius: preoperative identification by computed tomography. Ann Thorac Surg. 2005;79:1866–71. doi: 10.1016/j.athoracsur.2004.12.014. doi:10.1016/j.athoracsur.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura T, Koide M, Nakamura H, Toyoda F. The common trunk of the left pulmonary vein injured incidentally during lung cancer surgery. Ann Thorac Surg. 2009;87:954–5. doi: 10.1016/j.athoracsur.2008.07.054. doi:10.1016/j.athoracsur.2008.07.054. [DOI] [PubMed] [Google Scholar]
- 3.Marom EM, Herndon JE, Kim YH, McAdams HP. Variations in pulmonary venous drainage. Variations in pulmonary venous drainage to the left atrium: implication for radiofrequency ablation. Radiology. 2004;230:824–9. doi: 10.1148/radiol.2303030315. doi:10.1148/radiol.2303030315. [DOI] [PubMed] [Google Scholar]


