Abstract
Introduction
Alcohol use poses a major threat to the health and well being of rural African American adolescents by negatively impacting academic performance, health, and safety. However, rigorous economic evaluations of prevention programs targeting this population are scarce.
Methods
Cost-effectiveness analyses were conducted of SAAF-T relative to an attention-control intervention (ACI), as part of a randomized prevention trial. Outcomes of interest were the number of alcohol use and binge drinking episodes prevented, one year following the intervention. Incremental cost-effectiveness ratios (ICERs) and cost-effectiveness acceptability curves (CEACs) were used to determine the cost-effectiveness of SAAF-T compared to the ACI intervention.
Results
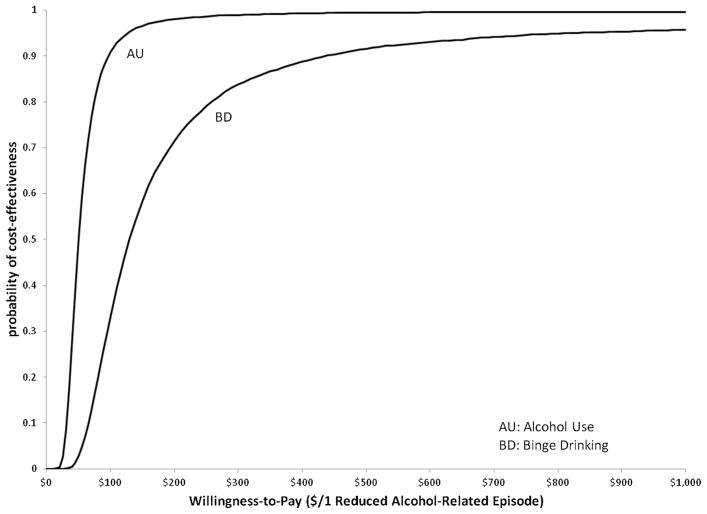
For the 473 participating youth completing baseline and follow-up assessments, the incremental per participant costs were $168, while the incremental per participant effects were 3.39 episodes of alcohol use prevented and 1.36 episodes of binge drinking prevented. Compared to the ACI intervention, the SAAF-T program cost $50 per reduction in an alcohol use episode and $123 per reduced episode of binge drinking. For the CEACs, at thresholds of $100 and $440, SAAF-T has at least a 90% probability of being cost-effective, relative to the ACI, for reductions in alcohol use and binge drinking episodes, respectively.
Conclusions
The SAAF-T intervention provides a potentially cost-effective means for reducing the African American youths’ alcohol use and binge drinking episodes.
Keywords: Alcohol, Prevention, Costs, Cost-effectiveness analysis, Economic evaluation, Rural African-American youth
1. Introduction
1.1. Adolescent alcohol use
In the United States, 30% of teens have used alcohol by the eighth grade and 69% have used by the twelfth grade (Johnston et al., 2013). Alcohol use during this period has negative implications for both society and the adolescent alcohol consumer. The economic burden to society from adolescent alcohol use was estimated to be $20.3 billion (in 2001), which is $26.3 billion in 2012 US$, including health care costs, productivity losses, criminal justice costs, and crime victim costs (Miller et al., 2006). These costs are borne by the individual, taxpayers, insurance companies, and other members of society affected by the individuals’ actions. For the adolescent consumer, alcohol use can negatively impact his or her academic achievement, health, and safety. Research suggests an association with lower school attendance and altered brain function (Masten et al., 2009); an increased risk of injuries (Bingham et al., 2009; Hingson and Zha, 2009; Istre et al., 2007; Lee, 2009; Roudsari et al., 2009); risky sexual behavior (Morrison-Beedy et al., 2011; Naimi et al., 2003; Strachman et al., 2009); and interpersonal violence (Howard et al., 2008; Mohler-Kuo et al., 2004).
The negative consequences to the adolescent alcohol consumer, as well as to society, increase with each episode of use. For example, Miller et al. (2007a) found that high school drinkers were two to five times more likely (three to ten times more likely for binge drinkers) than nondrinkers to ride with someone who had been drinking, participate in risky sexual behaviors, use tobacco, fight, attempt suicide, and use other illicit drugs. In a systematic review of cohort studies for adolescent drinking and subsequent adult outcomes, McCambridge et al. (2011) linked adolescent alcohol use, particularly binge drinking, to alcohol problems in adulthood, as well as psychiatric problems, poor educational attainment, and an increase in the number of sexual partners.
African Americans report somewhat lower rates of alcohol use early in adolescence. However by the end of high school, rates are similar among African Americans and other racial ethnic groups (French et al., 2002). Regardless of the relative rates of alcohol use, mounting evidence indicates that the consequences of use are greater for African Americans than for their European American peers (Wallace et al., 2002). African Americans experience more negative consequences per ounce of alcohol consumed than do European Americans including trouble at school and with the police, alcohol-related death, and dependency (Galea and Rudenstine, 2005; Jones-Webb, 1998; Welte and Barnes, 1987). Racial disparities are also evident in African Americans’ access to substance abuse treatment (Kline, 1996; Lowman and Le Fauve, 2003; Schmidt et al., 2006) and prevention (Brody et al., 1997) services. These findings underscore the importance of prevention efforts that target African American adolescents.
1.2. Alcohol prevention and economic evaluations
For the several million African American families with adolescents living in rural environments, no data exist on the economic impact of preventing alcohol use. Historically, rural residence was a protective factor for adolescent alcohol use; however, recent studies indicate they use alcohol at similar rates to those in inner cities (Kogan et al., 2006; NCASA, 2000). To address these needs, the Strong African American Families-Teen program (SAAF-T) was developed and tested in a randomized prevention trial (Kogan et al., 2012). SAAF-T is a developmentally appropriate adaptation of the Strong African American Families program, a similar intervention for preadolescents with proven efficacy in the prevention of alcohol use and conduct problems (Beach et al., 2008; Brody et al., 2010, 2006, 2004, 2005; Murry et al., 2007).
Although SAAF-T has proven efficacious (Brody et al., 2012), an economic evaluation has not been conducted. Economic evaluations are critical for policymakers at local, state, and national levels; potential program providers in social service agencies; and families in need of prevention services. Increasingly, governmental funding sources require, in addition to efficacy data, economic evaluations of programs to justify allocation of resources to providers (Pentz et al., 2006). Despite this need, economic evaluations of evidence based substance use prevention programs and especially those targeting African Americans are scarce. Although subject to methodological limitations, extant studies that have been conducted suggest that alcohol prevention programming is a sound investment of public health resources (Holder, 2000; Medina-Mora et al., 2010; Miller et al., 2007b; Mitchel et al., 1984; Pacileo and Fattore, 2009; Pentz, 1998; Plotnick, 1994; Spoth et al., 2002; Tricker and Davis, 1988). However, these studies are subject to a number of limitations including the retrospective assessment of costs, a lack of person-level costs and outcomes, and inappropriate control groups. As a result of these deficiencies, the National Institute on Drug Abuse has placed a high priority on economic analyses of interventions designed to prevent alcohol use (French and Drummond, 2005; National Institute on Drug Abuse, 2004).
In previous studies, the cost-effectiveness of alcohol use prevention programming has either been based on single-group design (e.g., Mitchel et al., 1984) or compared to a no-treatment control group (e.g., Pentz, 1998). In the first case, the effectiveness is biased because it is not known whether an untreated population also would have changed. This design often overestimates treatment effects. Although the second design is stronger, a no-treatment group does not represent high school students’ real-world experiences (Ramsey et al., 2001), as most receive some prevention information. For a more realistic comparison, participants in this study were randomized to either SAAF-T or an attention-control intervention (ACI). This is a superior design, providing both a stronger basis for inferring intervention causality through controlling the effects of time and attention (Devaney and Rossi, 1997; Dunford, 2000) and a context for economic evaluation that reflects real-world experiences, thus increasing the ecological validity (Ramsey et al., 2005).
The hypothesis that SAAF-T is cost-effective in deterring alcohol use relative to the ACI is tested in this study. The analyses were conducted from the societal perspective, including all costs related to implementing the program. Outcomes were alcohol use and binge drinking episodes in the year following the intervention. The results of this study are critical for dissemination of alcohol prevention programs in general, and those targeting African American youth in particular.
2. Methods
2.1. Study sample
Participants included 502 African American adolescents and their primary caregivers recruited from public school lists in 6 rural counties and 40 sites in central Georgia. The intervention was implemented from January 2008 to May 2009; detailed information regarding participant recruitment and enrollment, intervention implementation and fidelity, and data collection procedures have been published elsewhere (Kogan et al., 2012). Participants were randomized to receive SAAF-T or an ACI. The primary objective of SAAF-T is to reduce substance use among rural African American adolescents. SAAF-T is a form of family skills training (Kumpfer and Alvarado, 2003), an approach that integrates individual adolescent skill building, parenting skills training, and family interaction training. The ACI was designed to promote good nutrition, exercise, and informed consumer behavior among adolescents. To provide a stringent efficacy evaluation, both programs provided five, two-hour weekly meetings with separate, concurrent training sessions for parents and youth, followed by a joint parent-youth session during which families practice the skills they learned in their separate sessions. Cost-effectiveness analyses were conducted for the 473 families (94% of randomized families) that completed baseline and follow-up assessments. These participants did not differ from those who left the study on baseline alcohol use or demographic variables.
2.2. Outcomes
Outcome data were collected from 2007 to 2010. Adolescents were assessed one to three months prior to the start of the intervention (pretest) and fifteen to eighteen months after the intervention (follow-up). Items used to evaluate adolescent alcohol use and binge-drinking episodes were based on the public health literature (DiClemente et al., 2001) and the investigators’ previous research with a similar population (Brody et al., 2006; Wills et al., 2000, 2003). Adolescents self-reported, on a scale ranging from 0 to 6 (0: none, 1: 1 to 3 times, 2: 4 to 7 times, 3: 8 to 12 times, 4: 13 to 20 times, 5: 21 to 29 times, and 6: 30 or more times), how often he or she consumed at least one drink of alcohol (episodes of alcohol use) over the past three months. The same scale was used for how often he or she consumed three or more drinks at one time (episodes of binge drinking) over the past three months. Although self-report measures are susceptible to social desirability bias, previous research supports their validity in gathering information about the use of alcohol (Elliott et al., 1983; Smith et al., 1995; Williams et al., 1995).
2.3. Costs
Cost data were collected following best practice guidelines (Foster et al., 2007; Haddix et al., 2003), with full details provided elsewhere (Corso et al., 2013). The cost study considered only the final two rounds (out of five) of the intervention during which all costs were collected prospectively, including a rigorous collection of personnel time by activity category. Therefore, for that study, only 199 families at 16 sites in four counties were considered. Many categories of costs for the first three rounds could still be collected with a similar methodological rigor as the prospective collection (including site and ancillary services, supplies, equipment, overhead, and transportation), while the remaining costs (personnel and training) were estimated through multiple imputation (outlined below). Programmatic costs were collected as economic costs including all program implementation costs, participant costs, and donated resources. Program implementation costs included personnel resources, site and ancillary services, supplies, equipment, travel, and overhead. During the two rounds of prospective collection, personnel involved in delivery (facilitators) and administration of the intervention completed daily or weekly time logs. In this way, all research specific time was excluded from the final analysis. Non-personnel resources were valued through inspection of site agreements and billing documents that provided actual expenditure information for all five rounds of the intervention. Participant time spent participating in the program was valued using individual participant attendance at intervention sessions and participants’ self-reported wage rates. Corso et al. (2013) reported total site-level costs of $16, 251 for SAAF-T and $14,102 for the ACI resulting in a difference of $2149. The mean number of participants assigned to each site was 12.6 for SAAF-T and 12.1 for the ACI. Personnel time was the largest proportion of total costs (~25%) with training costs (including personnel time), participant time, and site-level services providing most of the remaining costs (~15–20% each).
Because personnel time was only assessed for two of five rounds of the intervention, missing cost data were imputed using cutting-edge statistical methods; for full information see Corso et al. (2013). The missing cost data were determined by multiple imputation, using the mi impute chained command in STATA version 12 (StataCorp 2011). The truncated regression method with a lower bound of zero was utilized rather than the traditional regression method to eliminate instances of imputed negative costs. Univariate imputation of each category of costs included group-specific covariates such as a dummy variable signifying SAAF-T/ACI, when groups met, the number of families, facilitator experience, and the number of groups a facilitator was concurrently leading. Once total programmatic costs were determined for each site (N = 40), these costs were divided among the participants assigned to that site. Direct service provision costs were divided among participants based on their attendance of sessions while overhead and administrative costs were evenly divided among all assigned participants.
2.4. Cost-effectiveness analysis
2.4.1. Incremental costs
For this study, incremental costs are the estimated difference in the value of resources needed (at the participant level) to deliver SAAF-T relative to those needed to deliver the ACI. Because the programmatic costs were right-skewed, the incremental costs of SAAF-T relative to the ACI were determined using a generalized linear model (GLM) with a gamma distribution and log link function (McCullagh and Nelder, 1989). GLMs have been suggested as an alternative method to log-transforming skewed cost data commonly arising in healthcare and public health applications (Blough and Ramsey, 2000; Diehr et al., 1999). Final incremental cost estimates were determined using combination rules for multiple-imputed data outlined by Rubin (1987) and implemented in STATA version 12 (StataCorp 2011). Combination rules provide a method for determining estimates of variance by considering both within observation variability and the variability between the datasets resulting from multiple imputations.
2.4.2. Incremental effects
For this study, incremental effects are the estimated difference in the number of alcohol use or binge drinking episodes at follow-up for a SAAF-T participant relative to an ACI participant. The number of episodes was reported within a range (e.g., 1–3 times). As a result, the main outcome variables were analyzed with interval regression. In the interval regression analysis, this difference is estimated as the regression coefficient on the Intervention assignment variable. To account for an entire year of potential drinking episodes, the self-reported “previous 3 months” of usage was multiplied times four. This assumes constant drinking behavior across time, with no seasonal effects. To account for potentially different drinking behavior at baseline, pretest measures of alcohol use or binge drinking were included in the regression.
2.4.3. Incremental cost-effectiveness analysis
The incremental cost-effectiveness ratio (ICER) represents the incremental costs divided by the incremental effects and describes the additional cost per additional outcome prevented when comparing one intervention (SAAF-T) to another (ACI). There is no exact method for estimating ICER confidence intervals (Chaudhary and Stearns, 1996; Van Hout et al., 1994); therefore, bootstrapping with 10,000 replications was used to estimate the uncertainty around the ICER estimates. The bootstrapped cost-effect pairs (the mean estimate of incremental costs and incremental effects resulting from each bootstrap replication) were used to create cost-effectiveness acceptability curves (CEACs), a means to illustrate the uncertainty around the parameter estimates by plotting the probability that an intervention is cost-effective at different threshold values (Briggs and Fenn, 1998; Fenwick et al., 2001). To determine the cost-effectiveness acceptability curves, the incremental net benefit (INBλ= ΔE ·λ − ΔC) was calculated for a given threshold value (λ), for every bootstrapped cost-effect pair (ΔC, ΔE). The probability that SAAF-T is cost-effective at each value of λ was calculated as the number of cost-effect pairs with a positive, INBλ divided by the total number of cost-effect pairs (10,000). This process was repeated from values of λ = $0 to λ = $1000 in $50 increments. In this study, threshold values correspond to the amount a decision maker would be willing to pay to prevent episodes of alcohol use or binge drinking in this population.
Following the approach used in the previous study on outcomes (Brody et al., 2012), we controlled for SES risk factors and gender in the assessment of incremental costs and effects. The SES risk factors index was developed from the self-reported responses of each adolescent’s primary caregiver in six categories: family poverty based on federal guidelines, caregiver unemployment, receipt of Temporary Assistance for Needy Families, caregiver single parenthood, caregiver education level less than high school graduation, and caregiver-reported inadequacy of family income. A dichotomous variable was formed with a value of 1 for responses matching each of the aforementioned categories (i.e. a value of 1 for an unemployed caregiver or a value of 1 for a caregiver reporting a middle-school level of education) and 0 otherwise. These variables were summed to form the SES risk index, which had a range of 0 to 6. Higher values of the index corresponded to a lower SES. Finally, dummy variables were created for Intervention assignment (SAAF-T = 1; ACI = 0) and Gender (males = 1; females = 0).
For this intervention, families were randomized to either SAAF-T or the ACI following recruitment and then were assigned to a site (non-randomly) based on the county and day of the week the family could attend sessions. In a randomized prevention trial where the intervention is offered in multiple sites, intra-class correlation can be an issue potentially resulting in significant site-level effects, which could inflate the type 1 error rate (Pals et al., 2008). However, our analyses found no significant intra-class correlation among the participants and therefore an adjustment is not included here. All analyses were conducted with STATA, version 12 in 2012.
3. Results
Table 1 reports the results of the interval regressions on the study outcomes and the GLM regression on programmatic costs. The coefficient on Intervention assignment in the interval regression was the estimate for incremental effectiveness. In each of these analyses, this coefficient was negative, indicating that at follow-up the adolescents that received SAAF-T reported fewer episodes of alcohol use and binge drinking compared to their ACI counterparts. The Intervention assignment coefficient was statistically significant at the p < 0.01 level for prevention of alcohol use episodes (−0.847) and at the p < 0.05 level for prevention of binge drinking episodes (−0.341). It is standard practice in cost-effectiveness analyses for a desirable incremental effectiveness to be positive therefore, the sign on the regression coefficient was inverted for use as an incremental effect. The coefficient on Intervention assignment in the GLM regressions was the estimate of incremental costs and was statistically significant at $168 (p < 0.05), indicating that SAAF-T requires more implementation resources than the ACI.
Table 1.
Regression results (N = 473) including 95% confidence interval for the intervention assignment coefficient.
| Variables | Alcohol use interval regression | Binge drinking interval regression | Programmatic costs GLM regression |
|---|---|---|---|
| Constant term | 0.670 | 0.487* | 1272** |
| Intervention assignmenta | −0.847** (−1.46, −0.233) | −0.341* (−0.737, 0.0549) | 168** (97.6, 238) |
| Covariates | |||
| Gender | 0.809** | 0.0751 | −40.8 |
| SES risk | 0.161 | −0.0063 | −51.1** |
| Pretest alcohol use | 1.50** | ||
| Pretest binge drinking | 1.20** | ||
GLM, generalized linear model.
p < 0.10.
p < 0.05.
Provides the incremental effectiveness of SAAF-T relative to the ACI for alcohol use and binge drinking episodes in the last three months. For purposes of the cost-effectiveness analyses, we multiplied the coefficient of intervention status by four to estimate the incremental effects (i.e. number of reduced episodes over the past year).
Table 2 presents the incremental costs, incremental effects, and ICERs for SAAF-T relative to the ACI for both alcohol use and binge drinking outcomes. The difference in costs was $168. The difference in alcohol use effects between the two interventions was 3.39 fewer episodes reported for SAAF-T participants. The ICER for SAAF-T relative to the ACI was $50 per each reduced episode of alcohol use over the past year. The difference in binge drinking effects between the two interventions was 1.36 fewer episodes of binge drinking for SAAF-T participants. As a result, the ICER for SAAF-T relative to the ACI was $123 per each reduced episode of binge drinking over the past year.
Table 2.
Incremental cost-effectiveness estimates with 95% confidence intervals.
| Outcome measure | ΔC | ΔE | ICER |
|---|---|---|---|
| # Episodes of alcohol use | $168 ($97.6, $238) | 3.39 (0.932, 5.84) | $49.6a |
| # Episodes of binge drinking | $168 ($97.6, $238) | 1.36 (−0.220, 2.95) | $123b |
ΔC, incremental costs; ΔE, incremental effects; ICER, incremental cost-effectiveness ratio.
$ per reduced episode of alcohol use.
$ per reduced episode of binge drinking.
Fig. 1 presents the CEACs for alcohol use (upper curve) and binge drinking (lower curve) with the probability that SAAF-T was cost-effective relative to the ACI, plotted from a willingness to pay of $0 to $1000 per reduced episode. There is little uncertainty that SAAF-T is cost-effective for either outcome by a threshold of $440 per reduced alcohol-related episode. Furthermore, there is less uncertainty that SAAF-T is cost-effective in reducing episodes of alcohol use with over a 90% probability by a threshold of $100.
Fig. 1.
Cost-effectiveness acceptability curves plotting the probability of cost-effectiveness for both alcohol use and binge drinking episodes prevented, over a range of willingness-to-pay values.
4. Discussion
Alcohol use poses a significant threat to the wellbeing of adolescents in general, and rural African American youth in particular. In response to the need for efficacious prevention programs for rural African Americans, SAAF-T was developed and evaluated in an attention controlled randomized prevention trial with 502 families. In contrast to extant economic studies, we investigated the cost effectiveness of SAAF-T using a design that included a societal perspective, randomization to treatment or attention control, and prospective, person-level assessment of costs. Compared to the ACI youth, SAAF-T youth reported significantly fewer alcohol use and binge drinking episodes in the year following the intervention. The incremental effects for alcohol use and binge drinking were 3.39 and 1.36 fewer episodes, respectively. The SAAF-T intervention was $168 per participant more expensive to implement compared to the ACI. As a result, the ICERs were $50 per each reduced episode of alcohol use and $123 per each reduced episode of binge drinking over the past year.
A common outcome measure is needed to compare the results of this study to other cost effectiveness studies targeting alcohol prevention. However, the literature review did not find any studies that used reduced episodes of either alcohol use or binge drinking as the measure of effectiveness. For example, Spoth et al. (2002), used cases of alcohol-use disorder prevented for a cost-effectivness analysis of the Iowa Strengthening Families Program (ISFP) and the Preparing for the Drug Free Years interventions (PDFY). Youths self-reported the age of initiation which was then used to predict, for each intervention group, the number of expected cases of alcohol use disorder in adulthood. For this study, we chose an effectiveness measure that did not require assumptions about future alcohol misuse.
Whether SAAF-T is likely to be cost-effective depends on the value that decision makers place on reducing drinking episodes in this population. At this time, no consensus threshold values exist for outcomes in alcohol use prevention. However, the variety of negative outcomes associated with adolescent alcohol use suggests that decision makers would have a significant interest in prevention. If the threshold value for a reduced episode of alcohol use is greater than $100 or the threshold value for a reduced episode of binge drinking is greater than $440, SAAF-T is very likely to be cost effective. Prior studies have reported that a reduction in alcohol use and binge drinking in this population would significantly reduce the risk of accidents and injuries, risky sexual behaviors, illicit drug use, and future dependency on alcohol, among other negative consequences. This evidence, together with the high probability of cost-effectiveness at reasonably low threshold values and the relative intensity of the control condition, suggests that the SAAF-T intervention is likely to be cost-effective relative to no prevention intervention.
Despite the methodological rigor of the present analysis, several limitations remain. First, the outcome measures were reported as ordinal variables that required estimation through interval regression of the actual number of episodes of alcohol use and binge drinking self-reported by the participants. Second, the participant’s self-reported use over the past three months rather than the entire year since receiving the intervention raises concerns. However, a search of the literature did not reveal any studies reporting seasonal variations of alcohol use in an adolescent population. Third, costs were collected prospectively for the last two rounds of a five round intervention. Fourth, the population was constrained to several counties in high poverty areas of Georgia, and therefore these results may not be generalizable to other African-American adolescents. Fifth, the outcome measure for this study is unique to other analyses, not allowing for comparisons of these results with other studies. Finally, the cost-effectiveness summary measure did not include productivity losses, health care resource utilization, or savings in criminal justice costs, all of which would be included at the societal perspective (Gold et al., 1996). However, the short analytic horizon of this study (18–21 months) did not produce meaningful differences between SAAF-T and ACI participants.
This study has a number of important strengths. First, the programmatic costs were collected prospectively and the analysis did not rely on a retrospective assessment of project budgets and personnel recall. Second, costs were valued from an economic perspective including opportunity costs such as participant time and donated resources. Because of these first two strengths, the ICERs presented in this study can be compared to other studies that follow best practice guidelines for the collection and estimation of programmatic costs. Third, while the substance abuse treatment literature has examples of studies that include parameter uncertainty and CEACs (see for example Zarkin et al., 2008; Barbosa et al., 2010; Cowell et al., 2012), this study provides the first example, to the best of our knowledge, in the substance abuse prevention literature.
This analysis provides a methodologically sound cost-effectiveness analysis of an alcohol prevention program, a clear deficiency in the literature. Economic evaluation studies focusing on prevention should continue to advance and incorporate best practices into these analyses. Moreover, these studies should strive for a prospective assessment of programmatic costs, taking into account opportunity costs such as participant time, volunteer labor, and donated resources. Whenever possible, costs and outcomes must be connected to participants in the study, allowing for more sophisticated analyses of the uncertainty around the ICER estimates. ICERs and CEACs suggest that compared to the ACI, SAAF-T was likely to be cost-effective in preventing episodes of alcohol use and binge drinking in the year following the intervention. Considering the negative health outcomes associated with adolescent alcohol use, the serious economic consequences that extend to society, and the disparities that African Americans face in both the consequences of use and in access to prevention, SAAF-T holds promise as a cost-effective approach for reducing drinking behavior in this underserved population.
Acknowledgments
Role for funding source
This research was supported by NIH NIDA Grant 5R01DA024644. The funding agency had no involvement in study design, data analysis, interpretation of the results, or decision to submit this article for publication.
No further acknowledgements.
Footnotes
Contributors
All authors contributed to the design and execution of the study. Cost data were collected by JBI under the direction of PSC. Outcome data were collected under the direction of SMK and GHB. Analyses of data and the manuscript draft were produced by JBI, and all authors contributed to and have approved the final manuscript.
Conflict of interest
No conflict declared.
References
- Barbosa C, Taylor B, Godfrey C, Rehm J, Parrott S, Drummond C. Modelling lifetime QALYs and health care costs from different drinking patterns over time: a Markov model. Int J Methods Psych. 2010;19:97–109. doi: 10.1002/mpr.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SRH, Kogan SA, Brody GH, Chen YF, Lei MK, Murry VA. Change in caregiver depression as a function of the strong African American families program. J Fam Psychol. 2008;22:241–252. doi: 10.1037/0893-3200.22.2.241. [DOI] [PubMed] [Google Scholar]
- Bingham CR, Shope JT, Parow JE, Raghunathan TE. Crash types: markers of increased risk of alcohol-involved crashes among teen drivers. J Stud Alcohol Drugs. 2009;70:528–535. doi: 10.15288/jsad.2009.70.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blough DK, Ramsey SD. Using generalized linear models to assess medical care costs. Health Serv Outcomes Res Methodol. 2000;1:185–202. [Google Scholar]
- Briggs A, Fenn P. Confidence intervals or surfaces? Uncertainty on the cost-effectiveness plane. Health Econ. 1998;7:723–740. doi: 10.1002/(sici)1099-1050(199812)7:8<723::aid-hec392>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Brody GH, Chen YF, Kogan SM, Murry VM, Brown AC. Long-term effects of the strong African American families program on youths’ alcohol use. J Consult Clin Psychol. 2010;78:281–285. doi: 10.1037/a0018552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Chen YF, Kogan SM, Yu TY, Molgaard VK, DiClemente RJ, Wingood GM. Family-centered program deters substance use, conduct problems, and depressive symptoms in black adolescents. Pediatrics. 2012;129:108–115. doi: 10.1542/peds.2011-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Murry VM, Gerrard M, Gibbons FX, McNair L, Brown AC, Wills TA, Molgaard V, Spoth RL, Luo Z, Chen YF. The strong African American Families Program: prevention of youths’ high-risk behavior and a test of a model of change. J Fam Psychol. 2006;20:1–11. doi: 10.1037/0893-3200.20.1.1. [DOI] [PubMed] [Google Scholar]
- Brody GH, Murry VM, Gerrard M, Gibbons FX, Molgaard V, McNair L, Brown AC, Wills TA, Spoth RL, Luo Z, Chen YF, Neubaum-Carlan E. The strong African American families program: translating research into prevention programming. Child Dev. 2004;75:900–917. doi: 10.1111/j.1467-8624.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- Brody GH, Murry VM, McNair L, Chen YF, Gibbons FX, Gerrard M, Wills TA. Linking changes in parenting to parent-child relationship quality and youth self-control: the Strong African American families program. J Res Adolesc. 2005;15:47–69. [Google Scholar]
- Brody GH, Neubaum E, Boyd GM, Dufour M. Health consequences of alcohol use in rural America. In: Robertson EB, Sloboda Z, Boyd GM, Beatty L, Kozel NJ, editors. Rural Substance Abuse: State of Knowledge and Issues. Vol. 168. 1997. pp. 137–174. NIDA Res. Mono. [PubMed] [Google Scholar]
- Chaudhary MA, Stearns SC. Estimating confidence intervals for cost-effectiveness ratios: an example from a randomized trial. Stat Med. 1996;15:1447–1458. doi: 10.1002/(SICI)1097-0258(19960715)15:13<1447::AID-SIM267>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Corso PS, Ingels JB, Kogan SM, Foster EM, Chen YF, Brody GH. Economic analysis of a multi-site prevention program: assessment of program costs and characterizing site-level variability. Prev Sci. 2013:1–10. doi: 10.1007/s11121-012-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowell AJ, Brown JM, Mills MJ, Bender RH, Wedehase BJ. Cost-effectiveness analysis of motivational inteviewing with feedback to reduce drinking among a sample of college students. J Stud Alcohol Drugs. 2012;73:226–237. doi: 10.15288/jsad.2012.73.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaney B, Rossi PH. Thinking through evaluation design options. Child Youth Serv Rev. 1997;19:587–606. [Google Scholar]
- DiClemente RJ, Wingood GM, Crosby R, Sionean C, Cobb BK, Harrington K, Davies S, Hook EW, Oh MK. Parental monitoring: association with adolescents’ risk behaviors. Pediatrics. 2001;107:1363–1368. doi: 10.1542/peds.107.6.1363. [DOI] [PubMed] [Google Scholar]
- Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- Dunford FW. The San Diego navy experiment: an assessment of interventions for men who assault their wives. J Consult Clin Psychol. 2000;68:468–476. doi: 10.1037//0022-006x.68.3.468. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Ageton SS, Huizinga D, Knowles BA, Canter RJ. The Prevalence and Incidence of Delinquent Behavior: 1976–1980. Behavioral Research Institute; Boulder, CO: 1983. [Google Scholar]
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10:779–787. doi: 10.1002/hec.635. [DOI] [PubMed] [Google Scholar]
- Foster EM, Porter MM, Ayers TS, Kaplan DL, Sandler I. Estimating the costs of preventive interventions. Eval Rev. 2007;31:261–286. doi: 10.1177/0193841X07299247. [DOI] [PubMed] [Google Scholar]
- French K, Finkbiner R, Duhamel L. Patterns of Substance Use Among Minority Youth and Adults in the United States: An Overview and Synthesis of National Survey Findings. Caliber Associates; Fairfax, VA: 2002. [Google Scholar]
- French MT, Drummond M. A research agenda for economic evaluation of substance abuse services. J Subst Abuse Treat. 2005;29:125–137. doi: 10.1016/j.jsat.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Galea S, Rudenstine S. Challenges in understanding disparities in drug use and its consequences. J Urban Health. 2005;82:III5–III12. doi: 10.1093/jurban/jti059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. Oxford University Press; New York: 1996. [Google Scholar]
- Haddix AC, Teutsch SM, Corso PS. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. 2. New York: Oxford University Press; 2003. [Google Scholar]
- Hingson RW, Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics. 2009;123:1477–1484. doi: 10.1542/peds.2008-2176. [DOI] [PubMed] [Google Scholar]
- Holder HD. Community prevention of alcohol problems. Addict Behav. 2000;25:843–859. doi: 10.1016/s0306-4603(00)00121-0. [DOI] [PubMed] [Google Scholar]
- Howard DE, Griffin MA, Boekeloo BO. Prevalence and psychosocial correlates of alcohol-related sexual assault among university students. Adolescence. 2008;43:733–750. [PMC free article] [PubMed] [Google Scholar]
- Istre GR, McCoy M, Stowe M, Barnard JJ, Moore BJ, Anderson RJ. The “unintended pedestrian” on expressways. Traffic Inj Prev. 2007;8:398–402. doi: 10.1080/15389580701576431. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O‘Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Drug Use: 2012 Overview, Key Findings on Adolescent Drug Use. Institute for Social Research, The University of Michigan; Ann Arbor: 2013. [Google Scholar]
- Jones-Webb R. Drinking patterns and problems among African-Americans: recent findings. Alcohol Health Res World. 1998;22:260–264. [PMC free article] [PubMed] [Google Scholar]
- Kline A. Pathways into drug user treatment: the influence of gender and racial/ethnic identity. Subst Use Misuse. 1996;31:323–342. doi: 10.3109/10826089609045815. [DOI] [PubMed] [Google Scholar]
- Kogan SM, Berkel C, Chen YF, Brody GH, Murry VM. Metro status and African-American adolescents’ risk for substance use. J Adolesc Health. 2006;38:454–457. doi: 10.1016/j.jadohealth.2005.05.024. [DOI] [PubMed] [Google Scholar]
- Kogan SM, Brody GH, Molgaard VK, Grange CM, Oliver DA, Anderson TN, DiClemente RJ, Wingood GM, Chen YF, Sperr MC. The strong African American families-teen trial: rationale, design, engagement processes, and family-specific effects. Prev Sci. 2012;13:206–217. doi: 10.1007/s11121-011-0257-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. Am Psychol. 2003;58:457–465. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- Lee K. Trend of alcohol involvement in maxillofacial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:E9–E13. doi: 10.1016/j.tripleo.2008.12.020. [DOI] [PubMed] [Google Scholar]
- Lowman C, Le Fauve CE. Health disparities and the relationship between race, ethnicity, and substance abuse treatment outcomes. Alcohol Clin Exp Res. 2003;27:1324–1326. doi: 10.1097/01.ALC.0000080346.62012.DC. [DOI] [PubMed] [Google Scholar]
- Masten A, Faden V, Zucker R, Spear L. A developmental perspective on underage alcohol use. Alcohol Res Health. 2009;32:3–15. [PMC free article] [PubMed] [Google Scholar]
- McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: a systematic review of cohort studies. PLoS Med. 2011;8:e1000413. doi: 10.1371/journal.pmed.1000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. 2. New York: Chapman and Hall; 1989. [Google Scholar]
- Medina-Mora ME, Garcia-Tellez I, Cortina D, Orozco R, Robles R, Vazquez-Perez L, Real T, Chisholm D. Cost-effectiveness study of interventions to prevent alcohol abuse in Mexico. Salud Mental. 2010;33:373–378. [Google Scholar]
- Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007a;119:76–85. doi: 10.1542/peds.2006-1517. [DOI] [PubMed] [Google Scholar]
- Miller TR, Levy DT, Spicer RS, Taylor DM. Societal costs of underage drinking. J Stud Alcohol. 2006;67:519–528. doi: 10.15288/jsa.2006.67.519. [DOI] [PubMed] [Google Scholar]
- Miller TR, Zaloshnja E, Spicer RS. Effectiveness and benefit-cost of peer-based workplace substance abuse prevention coupled with random testing. Accid Anal Prev. 2007b;39:565–573. doi: 10.1016/j.aap.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Mitchel ME, Hu TW, McDonnell NS, Swisher JD. Cost-effectiveness analysis of an educational drug-abuse prevention program. J Drug Educ. 1984;14:271–292. doi: 10.2190/LYPB-TMR5-P7H0-NGJP. [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M, Dowdall GW, Koss MP, Wechsler H. Correlates of rape while intoxicated in a national sample of college women. J Stud Alcohol. 2004;65:37–45. doi: 10.15288/jsa.2004.65.37. [DOI] [PubMed] [Google Scholar]
- Morrison-Beedy D, Carey MP, Crean HF, Jones SH. Risk behaviors among adolescent girls in an HIV prevention trial. West J Nur Res. 2011;33:690–711. doi: 10.1177/0193945910379220. [DOI] [PubMed] [Google Scholar]
- Murry VM, Berkel C, Brody GH, Gibbons M, Gibbons FX. The strong African American families program: longitudinal pathways to sexual risk reduction. J Adolesc Health. 2007;41:333–342. doi: 10.1016/j.jadohealth.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Lipscomb LE, Brewer RD, Gilbert BC. Binge drinking in the preconception period and the risk of unintended pregnancy: implications for women and their children. Pediatrics. 2003;111:1136–1141. [PubMed] [Google Scholar]
- National Institute on Drug Abuse. 2004 Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. National Institutes of Health; Bethesda, MD: 2004. [Google Scholar]
- National Center on Addiction and Substance Abuse. Center on Addiction and Substance Abuse, 2000 No Place to Hide: Substance Abuse in Mid-size Cities and Rural America. Columbia University; New York: 2000. [Google Scholar]
- Pacileo G, Fattore G. Alcohol abuse prevention in young people: an economic simulation. J Subst Use. 2009;14:385–392. [Google Scholar]
- Pals SL, Murray DM, Alfano CM, Shadish WR, Hannan PJ, Baker WL. Individually randomized group treatment trials: a critical appraisal of frequently used design and analytic approaches. Am J Public Health. 2008;98:2120–2120. doi: 10.2105/AJPH.2007.127027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentz MA. Costs, benefits, and cost-effectiveness of comprehensive drug abuse prevention. In: Bukoski WJ, Evans RI, editors. Cost-Benefit/Cost-Effectiveness Research of Drug Abuse Prevention: Implications for Programming and Policy. National Institutes of Health; Rockville, MD: 1998. pp. 111–129. [Google Scholar]
- Pentz MA, Jasuja GK, Rohrbach LA, Sussman S, Bardo MT. Translation in tobacco and drug abuse prevention research. Eval Health Prof. 2006;29:246–271. doi: 10.1177/0163278706287347. [DOI] [PubMed] [Google Scholar]
- Plotnick RD. Applying benefit-cost analysis to substance use prevention programs. Subst Use Misuse. 1994;29:339–359. doi: 10.3109/10826089409047385. [DOI] [PubMed] [Google Scholar]
- Ramsey SD, McIntosh M, Sullivan SD. Design issues for conducting cost-effectiveness analyses alongside clinical trials. Annu Rev Public Health. 2001;22:129–141. doi: 10.1146/annurev.publhealth.22.1.129. [DOI] [PubMed] [Google Scholar]
- Ramsey SD, Wilke R, Briggs W, Brown R, Buxton M, Chawla A. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health. 2005;8:521–533. doi: 10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- Roudsari B, Ramisetty-Mikler S, Rodriguez LA. Ethnicity, age, and trends in alcohol-related driver fatalities in the United States. Traffic Inj Prev. 2009;10:410–414. doi: 10.1080/15389580903131506. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons; New York: 1987. [Google Scholar]
- Schmidt L, Greenfield T, Mulia N. Unequal treatment – racial and ethnic disparities in alcoholism treatment services. Alcohol Res Health. 2006;29:49–54. [PMC free article] [PubMed] [Google Scholar]
- Smith GT, McCarthy DM, Goldman MS. Self-reported drinking and alcohol-related problems among early adolescents – dimensionality and validity over 24 months. J Stud Alcohol. 1995;56:383–394. doi: 10.15288/jsa.1995.56.383. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Guyll M, Day SX. Universal family-focused interventions in alcohol-use disorder prevention: cost-effectiveness and cost-benefit analyses of two interventions. J Stud Alcohol. 2002;63:219–228. doi: 10.15288/jsa.2002.63.219. [DOI] [PubMed] [Google Scholar]
- Strachman A, Impett EA, Henson JM, Pentz MA. Early adolescent alcohol use and sexual experience by emerging adulthood: a 10-year longitudinal investigation. J Adolesc Health. 2009;45:478–482. doi: 10.1016/j.jadohealth.2009.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricker R, Davis LG. Implementing drug education in schools: an analysis of the costs and teacher perceptions. J Sch Health. 1988;58:181–185. doi: 10.1111/j.1746-1561.1988.tb05856.x. [DOI] [PubMed] [Google Scholar]
- Van Hout BA, Al MJ, Gordon SG, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ. 1994;3:309–319. doi: 10.1002/hec.4730030505. [DOI] [PubMed] [Google Scholar]
- Wallace JM, Bachman JG, O‘Malley PM, Johnston LD, Schulenberg JE, Cooper SM. Tobacco, alcohol, and illicit drug use: racial and ethnic differences among US high school seniors, 1976–2000. Public Health Rep. 2002;117:S67–S75. [PMC free article] [PubMed] [Google Scholar]
- Welte JW, Barnes GM. Alcohol-use among adolescent minority-groups. J Stud Alcohol. 1987;48:329–336. doi: 10.15288/jsa.1987.48.329. [DOI] [PubMed] [Google Scholar]
- Williams CL, Toomey TL, McGovern P, Wagenaar AC, Perry CL. Development, reliability, and validity of self report alcohol-use measures with young adolescents. J Child Adolesc Subst Abuse. 1995;4:17–40. [Google Scholar]
- Wills TA, Gibbons FX, Gerrard M, Brody GH. Protection and vulnerability processes relevant for early onset of substance use: a test among African American children. Health Psychol. 2000;19:253–263. doi: 10.1037//0278-6133.19.3.253. [DOI] [PubMed] [Google Scholar]
- Wills TA, Gibbons FX, Gerrard M, Murry VM, Brody GH. Family communication and religiosity related to substance use and sexual behavior in early adolescence: a test for pathways through self-control and prototype perceptions. Psychol Addict Behav. 2003;17:312–323. doi: 10.1037/0893-164X.17.4.312. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Aldridge A, Mitra D, Mills MJ, Couper DJ, Cisler RA. Cost and cost effectiveness of the COMBINE study in alcohol-dependent patients. Arch Fam Med. 2008;2008:1214–1221. doi: 10.1001/archpsyc.65.10.1214. [DOI] [PMC free article] [PubMed] [Google Scholar]