Abstract
Aims
To determine how variable stool consistency is in patients with irritable bowel (IBS) and assess the relationship between stool consistency and gastrointestinal symptoms.
Methods
Individuals with a physician diagnosis of IBS were recruited by advertisement. Enrollment questionnaires included the Rome III Diagnostic Questionnaire and IBS Symptom Severity Scale. Then 185 patients meeting Rome criteria for IBS rated the consistency (using the Bristol Stool Scale) of each bowel movement (BM) for 90 days and whether the BM was accompanied by pain, urgency, or soiling. Each night they transferred BM ratings from a paper diary to an internet form and also reported the average daily intensity of abdominal pain, bloating, bowel habit dissatisfaction, and life interference of bowel symptoms. Only the longest sequence of consecutive days of diary data was used in analysis (average of 73 days).
Results
Patients were 89% female with average age 36.6 years. 78% had both loose/watery and hard/lumpy stools; the average was 3 fluctuations between these extremes per month. The proportion of loose/watery stools correlated r=.78 between the first and second months and the proportion of hard/lumpy stools correlated r=.85 between months. Loose/watery stools were associated with more BM-related pain, urgency, and soiling than hard/lumpy or normal stools; however, IBS-C patients had significantly more BM-unrelated abdominal pain, bloating, dissatisfaction with bowel habits, and life interference than IBS-D. Questionnaires overestimated the frequency of abnormal stool consistency and gastrointestinal symptoms compared to diaries.
Conclusions
Stool consistency varies greatly within individuals. However, stool patterns are stable within an individual from month to month. The paradoxical findings of greater symptom severity after individual loose/watery BMs vs. greater overall symptom severity in IBS-C implies different physiological mechanisms for symptoms in constipation compared to diarrhea. Daily symptom monitoring is more sensitive and reliable than a questionnaire.
Introduction
Patients with irritable bowel syndrome (IBS) are subtyped into those with predominant diarrhea (IBS-D), predominant constipation (IBS-C), mixed or alternating bowel habits (IBS-M), and those with no significant abnormalities in their stools (IBS-U)1. The assignment of IBS patients to the appropriate subtype is critical to management because pharmacological treatments for IBS are designed to address either constipation or diarrhea as a means of improving the multiple symptoms of IBS. Lubiprostone2, linaclotide3, and tegaserod4 were developed to treat IBS-C whereas alosetron5 was developed to treat IBS-D, and the use of these drugs in a subtype of IBS different from the one it was developed for is thought to place the patient at risk for worsening bowel symptoms. Thus it is important to know whether patients can be reliably classified into these subtypes and whether the subtypes are stable over time.
Previous studies suggest, however, that IBS subtype classification is not stable: half6 to ¾ of IBS patients7, 8 change their subtype classification over a one-year period. Most of these transitions are between IBS-C and IBS-M or between IBS-D and IBS-M, with relatively few patients transitioning between IBS-D and IBS-C7. This degree of instability raises concerns about the reliability of treatment guidelines based on IBS subtype and suggests that more data is needed on within-subject variability in stool consistency and the relationship between variations in stool consistency and other symptoms of IBS such as pain and bloating.
Limited data are available on the relationship of stool consistency to other IBS symptoms, and the findings are often inconsistent. Hellstrom et al9 reported that pain episodes are more closely associated with loose/watery stools than with hard/lumpy stools, although Ragnarsson10 found no relationship between abdominal pain and defecation. Chang et al11 reported that abdominal distention is more strongly associated with IBS-C than with IBS-D whereas the subjective sensation of bloating without distention is more closely associated with diarrhea; they found that defecation or passing gas relieved both bloating and distention. Other investigators, however, find no association between bowel habits and either distention or bloating12. Urgency is more closely associated with diarrhea than with constipation13.
The primary aims of this 90-day diary study were to (1) characterize the bowel-movement-to-bowel movement and day-to-day variability in stool consistency for IBS patients and (2) describe the association of abnormal stool consistency and IBS subtype with other gastrointestinal symptoms and the interference of abnormal stool consistency in the patient's life. A secondary aim was to determine whether the Rome III classification of IBS patients into IBS-C, IBS-M, and IBS-D subtypes by retrospective questions is confirmed by prospective diary data.
Methods
Individuals with IBS aged18 years and older were enrolled through advertising to complete 90 days of diary recordings of their bowel movements and gastrointestinal symptoms. The study was advertised on the website of the Center for Functional GI & Motility Disorders at UNC-Chapel Hill, on national websites frequented by IBS patients (such as IFFGD.org and IBSgroup.org), and through mass e-mails to staff, students and faculty at UNC-Chapel Hill. Additionally, IBS patients who had registered to participate in research studies in our Center were invited to participate.
Inclusion criteria in the study were age of at least 18 years (no upper limit), daily access to the internet, fulfilling Rome III criteria for IBS1, and having been diagnosed with IBS by a physician. Exclusion criteria were a history of inflammatory bowel disease, celiac disease or lactose intolerance, daily use of IBS prescription medications (lubiprostone, tegaserod or alosetron), and current participation in pharmacologic trials. Subjects were permitted to use anti-diarrheal or laxative medications or antidepressants occasionally, but were asked to refrain from using these drugs as much as possible during the study and to record when they used them in their symptom diary.
A total of 595 potential subjects were screened online for participation in the study, out of which 392 met study criteria and were invited to enroll through the mail. The mailing contained (1) the study consent form and a physician release of information form for verifying IBS diagnosis, both of which the subjects were instructed to sign and return via mail; (2) the printed pocket diary for recording bowel movements and associated symptoms; and (3) instructions and a password for accessing the secure study website to enter study data.
Before beginning to record their bowel symptoms in the diary, subjects completed the Rome III Diagnostic Questionnaire14, the IBS Severity Scale (IBS-SS)15, the IBS Quality of Life questionnaire (IBS-QOL)16, 17, and the Brief Symptom Inventory 18 (BSI-18)18which is a psychological symptom questionnaire.
The Rome III Diagnostic Questionnaire14 includes two questions that are used to determine IBS subtype. One question asks, “In the last 3 months, how often did you have hard or lumpy stools?” and the other asks, “In the last 3 months, how often did you have loose, mushy, or watery stools?” The standard response choices are 0 = “Never or rarely”; 1= “Sometimes”; 2= “Often”, 3= “Most of the time”; and 4= “Always”; although investigators are given the option of substituting a different response scale in which 0= “Never or rarely”; 1= “About 25% of the time”; 2= “About 50% of the time”; 3=“About 75% of the time”; and 4= “Always, 100% of the time”. In this study the standard response scale was used and a response of “Sometimes” was treated as equivalent to 25% of BMs.
The IBS-SS questionnaire15 consists of 5 equally weighted questions about IBS symptoms in the last 10 days. The average severity of abdominal pain, average severity of bloating, dissatisfaction with bowel habits, and interference of symptoms with activities of daily life are queried on 0-100 mm visual analog scales. A fifth question asks about the number of days of abdominal pain in the last 10 days, and the response is multiplied by 10 to give this question the same weight as the other 4.
After completing these baseline questionnaires, subjects began the 90-day diary recording period in which they reported on every bowel movement (BM) throughout each day in a pocket-sized diary notebook. They rated the stool consistency of each BM on the 7-point Bristol Stool Scale19 by referring to pictures and verbal descriptors in their diary book, and reported (yes/no) any associated symptoms of urgency, pain, or fecal soiling. Each night, the subjects were asked to transfer their diary ratings for that day to a secure website, where they also rated on a 0-10 scale their global 24-hour symptoms of abdominal pain, bloating, dissatisfaction with their BMs, and life interference from bowel symptoms (the same symptoms included in the IBS-SS15 questionnaire), and life stress. They were also asked to report any medications used during the day. If subjects failed to complete the online diary on any given day, they were reminded to do so by study staff the next day via e-mail. They could then enter their data for the previous day, but were only allowed to enter data for one retrospective day. If subjects missed more than three days of diary recordings, their participation was terminated.
The study participants were paid one dollar for each diary day they completed to compensate them for their time and effort, and they also received an additional bonus of $30 for every 30 days of the total 90-day diary period that they completed without interruptions. The study was reviewed and approved by the Biomedical Institutional Review Board at the University of North Carolina at Chapel Hill.
Data Analysis
Data from all subjects who completed a minimum continuous diary record period of at least 21 days were analyzed. This resulted in an analysis sample of 185 patients. For each patient record analyzed, only the single longest continuous stretch of diary days was selected for analysis; i.e., no interrupted date sequences were used in the analyses. The average length of the continuous diary records submitted to analysis was 72.9 days (median 86 days, range 21-106 days; a few subjects continued diary data entry longer than the required 90 days). The diary periods analyzed contained an average of 133.2 consecutive BMs.
To characterize bowel-movement-to-bowel-movement and day-to-day variability in stool consistency (Aim 1), we calculated the proportion of BMs and days with each stool consistency in the whole group of 185 IBS patients. To address the secondary aim – validation of the Rome classification of IBS patients into subtypes – we compared the IBS-subtypes assigned based on the diary data to the subtypes based on the Rome III Diagnostic Questionnaire completed at enrollment. In both cases, patients were classified as IBS-D if they had >25% loose/watery BMS and <25% hard/lumpy BMS; IBS-C if they had <25% loose/watery BMs and >25% hard/lumpy BMs; IBS-M if they had >25% loose/watery BMs and >25% hard/lumpy BMs; and IBS-U if they had <25% loose/watery and <25% hard/lumpy BMs. Patients who took laxatives or antidiarrheal medications were excluded from this analysis. To investigate the relationship between stool consistency and gastrointestinal symptoms such as pain and bloating, we first examined the associations between these symptoms and stool types in the pooled sample of all 185 IBS patients. Next we compared symptom severity in IBS subtypes defined by the Rome III Diagnostic Questionnaire.
A separate analysis was performed to assess the stability of bowel habits and IBS symptoms by comparing the first and second 30-day periods of diary records for the same subject. This analysis was limited to the 135 subjects who had at least 60 days of uninterrupted diary entries. For this analysis the IBS-SS index was computed based on the diary data as follows: for daily questions on abdominal pain severity, bloating severity, dissatisfaction with bowel habits, and interference with activities of daily life, the average severity score for the 30 day period was used in the computation of the IBS-SS, and the proportion of days with any pain was multiplied by 100.
Two post-hoc analyses were performed to follow up on the paradoxical finding that on average, IBS-C patients had more severe symptoms of pain, bloating, bowel habit dissatisfaction, and life interference than IBS-D patients, although when individual BMs were compared to each other, loose/watery stools triggered more intense symptoms than hard/lumpy or normal consistency stools. The first analysis was an ANOVA comparing IBS-subtypes on days without any BM, and the second analysis compared pain and bloating by paired t-tests on cumulative days of constipation (hard/lumpy stools or no BM) for patients with IBS-C.
Chi-square tests were used to compare subgroups on categorical variables. Analysis of variance tests with Bonferroni-adjusted post-hoc tests were used to compare mean scores on continuous variables between and within subgroups. Correlations between variables were assessed by the Spearman nonparametric correlation coefficient.
Results
Subject characteristics
Of the 392 subjects who met inclusion criteria and were invited to participate in the study, 206 (52.5%) enrolled and started diary entries. Non-participants were not significantly different from participants with respect to age, sex, or frequency of self-reported bowel symptoms (abdominal pain, loose/watery stools or hard/lumpy stools in the past 3 months) on screening questionnaires. Seven enrolled subjects dropped out after beginning the diary recordings, and 5 others were dismissed due to low compliance with diary entries. Another 9 subjects completed the 3-month study but were not included in the data analysis because their diary records did not meet the criterion of 21 consecutive days of complete data.
Average age of the 185 patients included in the analyses for this study was 36.6 years (range 19 to 70). The sample was 88.6% females (164/185). The Rome III IBS subtype distribution based on the Rome III Diagnostic Questionnaire18 was 31.9% IBS-D, 55.1% IBS-M, and 12.4% IBS-C. Only one subject (0.5%) had IBS-U. Self-described races of participants were 94.1% Caucasian, 2.7% African-American, 0.5% Asian, and 2.7% mixed race. Age and race were equivalent between bowel subtype groups (Table 1), but sex distribution was not (Chi-square=0.007): the IBS-D subgroup had a higher proportion of males than IBS-C or IBS-M.
Table 1.
Demographic characteristics and symptoms at enrollment.
| Total sample (N=185) | IBS-D (n=59) | IBS-M (n=102) | IBS-C (n=23) | |
|---|---|---|---|---|
| Age; mean (S.D.) | 36.59 (12.16) | 39.47 (11.71) | 35.63 (12.36) | 33.43 (11.43) |
| Gender (% female) | 88.60% | 77.97%* | 94.12% | 91.30% |
| Race (% white) | 94.10% | 94.90% | 92.20% | 100% |
| Overall IBS Severity; mean(S.D.) | 258.04 (96.91) | 248.64 (106.34) | 260.29 (88.34) | 272.17 (109.54) |
| Abdominal pain severity; mean (S.D.) | 5.17 (2.32) | 4.93 (2.46) | 5.26 (2.23) | 5.39 (2.37) |
| Bloating severity; mean (S.D.) | 4.56 (2.90) | 4.41 (2.96) | 4.48 (2.74) | 5.30 (3.47) |
| Dissatisfaction with bowel habits; mean (S.D.) | 6.29 (2.71) | 6.14 (2.76) | 6.49 (2.57) | 5.78 (3.19) |
| Interference of bowel symptoms with life activities mean (S.D.) | 4.82 (2.89) | 4.78 (3.14) | 4.91 (2.66) | 4.52 (3.26) |
| Health-related quality of life score - IBS-QOL; mean (S.D.) | 58.66 (18.79) | 59.69 (19.89) | 57.24 (18.09) | 62.34 (18.80) |
| Psychological Distress BSI-18 Global Symptom Index scale; mean T-score (S.D.) | 56.01 (10.40) | 57.58 (9.15) | 59.17 (9.37) | 57.28 (9.60) |
| Somatization Scale of BSI- 18; mean T-score (S.D.) | 58.13 (8.68) | 56.59 (9.40) | 58.64 (7.90) | 59.78 (9.84) |
| Life stress in past 10 days - 0-10 ratings; mean (S.D.) | 4.86 (2.86) | 4.24 (3.10) | 5.14 (2.58) | 5.22 (3.22) |
IBS-D less than IBS-C or IBS-M, p<.05.
The average IBS Severity Score on retrospective questionnaires completed at enrollment was 248.6, which is in the moderate range according to published guidelines for this scale15: 23.2% had scores in the mild range (≤175), 42.7% in the moderate range (>175 and <300) and 34.1% in the severe range (≥300). The IBS-D, IBS-M and IBS-C subgroups had equivalent mean scores both on overall IBS severity and the individual bowel symptoms measured by the IBS-SS at screening, and they did not differ significantly either in quality of life, psychological distress or life stress ratings (Table 1).
Medication use
Of the total analysis sample of 185 individuals, 28 (15.1%) used anti-diarrheal medications during the study, 25 (13.5%) used laxatives, and 2 (1.1%) used both. Eleven subjects reported using antidepressants at least once but 45 did not respond to this question. One hundred thirty subjects (70.3%) used neither laxatives nor anti-diarrheal medications during the diary recording period.
Distribution of Stool Consistency Ratings across Bowel Movements
In the total sample of 185 IBS patients, the majority (58.1%) of BMs received Bristol Stool Scale ratings of 3-5 which define the normal range. Loose/watery stools and hard/lumpy stools were about equally represented (20.5% and 21.2% respectively). Average stool frequency was 1.80 per day.
To ensure that the use of laxatives or anti-diarrheal medications by 30% of the patients in the study did not bias this general characterization of stool consistency patterns in IBS, we repeated the analysis of stool consistency ratings across BMs after excluding all patients who reported using anti-diarrheal medications or laxatives. This changed the results very little: 59.3% of BMs were of normal consistency, 20.4% were loose/watery and 20.3% were hard/lumpy. Average stool frequency was 1.79 BMs/day in those taking no laxatives or antidiarrheal medications.
Fluctuations between loose/watery stools (Bristol Stool Scores of 6 or 7) and hard/lumpy stools (Bristol Stool Scores of 1 or 2) were common even among patients who took no laxatives or antidiarrheal medications. In this group of 130 individuals, only 13 (10%) had no loose/watery stools in their diary records, and only 17 (13.1%) had no hard/lumpy stools. Fluctuations between loose/watery and hard/lumpy stools occurred in 77.7% of these patients, and all patients averaged 2.98 fluctuations per 30 days (range 0 to 15.51).
Although most subjects showed a mixture of stool types, they showed distinct individual patterns which were stable from the first month to the second month. (The third month was not included in this analysis because many subjects did not complete 3 full months of uninterrupted data.) As shown in Table 2, the proportion of BMs rated loose/watery correlated 0.783 between the first and second months, and the proportion of BMs rated hard/lumpy correlated 0.852 between the first and second months. Symptoms of pain, bloating, bowel habit dissatisfaction, and life interference were also highly correlated between the first and the second month.
Table 2. Stability of Stool Consistency and Bowel Symptoms from Month to Month, and Comparison of Diary Ratings to IBS-SS Questionnaire.
| Variable | Means & Standard Deviations | Correlations | ||||
|---|---|---|---|---|---|---|
| Baseline Questionnaires | 1st Month | 2nd Month | Baseline vs. 1stmo | Baseline vs. 2ndmo | 1stmo vs. 2ndmo | |
| BMs/day | -- | 1.87 (1.01)* | 1.77 (0.96) | -- | -- | .881 |
| Loose/watery BM proportion | -- | 0.21 (0.21) | 0.19 (0.20) | -- | -- | .783 |
| Hard/lumpy BM proportion | -- | 0.23 (0.24) | 0.22 (0.25) | -- | -- | .852 |
| IBS-SS | 253.33 (94.96)# | 197.67 (70.57) | 196.32 (75.65) | .628 | .504 | .871 |
| Pain severity | 5.08 (2.35)# | 3.42 (1.88) | 3.37 (1.97) | .370 | .285 | .843 |
| Pain proport-ion of days | 0.48 (0.28)# | 0.81 (0.24) | 0.81 (0.26) | .459 | .463 | .851 |
| Bloating severity | 4.46 (2.84)# | 3.60 (2.23) | 3.63 (2.25) | .611 | .485 | .862 |
| Bowel habit dissatisfaction | 6.23 (2.62)# | 4.64 (1.95) | 4.56 (2.19) | .513 | .373 | .829 |
| Life interference | 4.73 (2.87) | 2.98 (1.80) | 2.90 (1.84) | .559 | .464 | .816 |
Baseline value different from both 1st month value and 2nd month value, p<.001;
First month value different from second month value, p<.05.
Distribution of stool consistency ratings across days
The questions used to subtype IBS patients as IBS-D, IBS-C, or IBS-M usually ask about the proportion of BMs that are loose/watery and the proportion of BMs that are hard/lumpy. However, this could misrepresent usual bowel habits if loose/watery BMs tend to cluster together, occurring multiple times a day for a few days with such clusters separated by several days of normal stools, in contrast to constipation which may be associated with relatively infrequent hard/lumpy stools. To test this, we calculated the proportion of days with only normal consistency stools, proportion of days with only loose/watery stools, proportion of days with only hard/lumpy stools, and the proportion of days with both loose/watery and hard/lumpy stools. This analysis (Table 3) showed that that day-to-day variability in stool consistency was similar to BM-to-BM variability. There were only normal stools on 39.4% of days, only loose/watery stools on 20.1% of days, and only hard/lumpy stools on 21.8% of days. Both loose/watery and hard/lumpy stools were reported within the same day on 1.8% of days. There were also 16.9% of days with no BM.
Table 3. Relative Frequency of Days with Hard/Lumpy, Loose/Watery, Mixed, Normal Consistency and No Stools by IBS-Subtype and Overall.
| IBS Subtype | % of days with hard/lumpy stools but no loose/watery stools | % of days with loose/watery stools but no hard/lumpy stools | % of days with both hard/lumpy and loose/watery stools | % of days with only normal consistency stools | % of total diary days with NO BM |
|---|---|---|---|---|---|
| IBS-D | 12.1%C,M | 28.7%C,M | 1.9% | 42.3% | 15.0%C |
| IBS-M | 24.5%C,D | 18.6%C,D | 1.9% | 40.0% | 16.3% |
| IBS-C | 35.7%D,M | 4.7%D,M | 0.9% | 33.8% | 24.9%D |
| All IBS | 21.8% | 20.1% | 1.8% | 39.4% | 16.9% |
Significantly different from IBS-C;
Significantly different from IBS-D;
Significantly different from IBS-M, all at p<.05 Bonferroni adjusted.
Classification of IBS patients into subtypes by the Rome III Diagnostic Questionnaire compared to classification based on the daily stool diary
When the Rome questionnaire was used to classify patients, the largest subgroup was IBS-M (56.2%) and only one patient was classified as IBS-U (see last column of Table 4). However, when the stool diary was used to classify patients, very few met criteria for IBS-M (4.6%), and IBS-U became the largest group (35.4% of patients; see first row of Table 4). This occurred because the Rome questionnaire over-estimated the proportion of BMs that were loose/watery and the proportion that were hard/lumpy. As a consequence, patients who were classified as IBS-D by the questionnaire for the most part remained IBS-D or were reclassified as IBS-U based on the stool diary, and similarly, patients classified as IBS-C by the questionnaire remained IBS-C or were reclassified as IBS-U. The results of the two methods of subtyping patients were modestly but significantly related (Chi-square = 19.595; df = 9; p=.021; Spearman rho=0.265, p<0.001).
Table 4.
Relationship between IBS-subtypes defined by Rome III Diagnostic Questionnaire (RDQ) and subtyped defined by the stool diary.
| Diary IBS-U | Diary IBS-D | Diary IBS-M | Diary IBS-C | TOTAL | |
|---|---|---|---|---|---|
| RDQ IBS-U | 1 | 0 | 0 | 0 | 1 (0.8%) |
| RDQ IBS-D | 14 | 19 | 2 | 5 | 40 (30.8%) |
| RDQ IBS-M | 26 | 21 | 4 | 22 | 73 (56.2%) |
| RDQ IBS-C | 5 | 1 | 0 | 10 | 16 (12.3% |
| TOTAL | 46 (35.4%) | 41 (31.5%) | 6 (4.6%) | 37 (28.5%) | 130 (100%) |
Sex and age differences in stool characteristics
Women (n=164) had a higher proportion of BMs rated hard/lumpy compared to the 21 men (22.5% vs. 11.4%, t=2.727, p=.011), but there were no significant sex differences in the proportion of BMs that were loose/watery (24.3% vs. 20.0%), the frequency of fluctuations between hard/lumpy and loose/watery stools (3.02 vs. 2.90 times per month), or average stool frequency (1.81 vs. 1.79 stools per day for men vs. women). IBS patients who were older than the median age of 35 years had significantly more BMs per day than younger subjects (1.94 vs. 1.64, t=2.185, p=.030), but there were no age related differences in stool consistency. When the subset of 20 subjects who were aged 55 or older were compared to younger subjects, no differences in stool consistency or stool frequency were observed. The frequency of fluctuations between hard/lumpy stools and loose/watery stools was not correlated with age, sex, overall IBS severity, abdominal pain, bloating, life stress or psychological symptoms, but a higher frequency of fluctuation was weakly correlated with poorer IBS-QOL scores (Spearman rho = -0.19, p=0.009).
The association between stool consistency and other bowel symptoms
The symptoms of urgency, pain, and soiling were queried at each BM. When the data were combined for all IBS subtypes, loose/watery BMs were associated with more symptoms than hard/lumpy stools for urgency, 79.6% vs. 28.8%, (p<0.0001); for pain and discomfort, 72.9% vs. 52.5%(p<0.0001); and for soiling (incontinence), 5.2% vs. 1.6% (p=0.004).
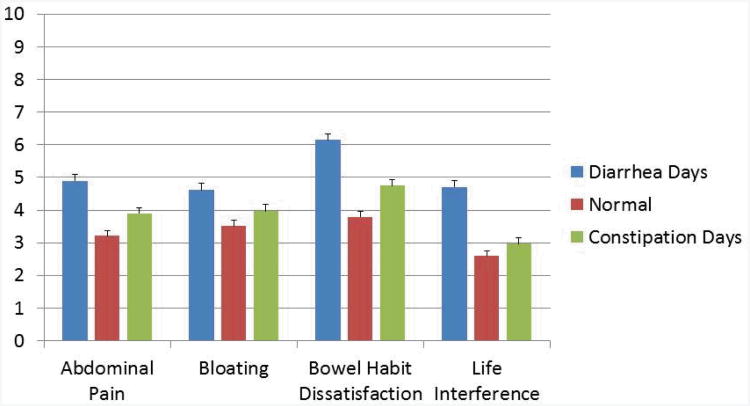
Other bowel symptoms – abdominal pain, dissatisfaction with bowel function, interference with life activities, and bloating – were assessed retrospectively for the past 24 hours at the end of each day rather than at each BM. These symptoms were averaged and compared across all patients for (a) diarrhea days, defined as days with one or more loose/watery bowel movements but no hard/lumpy bowel movement; (b) days with normal stool consistency; and (c) constipation days, defined as days with one or more hard/lumpy bowel movements but no loose/watery bowel movements (Figure 1). The small number of days on which both loose/watery and hard/lumpy bowel movements occurred (average of 1.3 days per subject or 1.8% of all diary days) were excluded from this analysis. Abdominal pain, bloating, dissatisfaction with bowel function, and interference with life activities were all rated as significantly more severe during diarrhea days, while constipation days had significantly less severe symptoms than diarrhea days but more severe symptoms than days with normal stool consistency.
Figure 1.
Comparison of bowel symptoms of IBS patients on days with diarrhea, constipation or normal stool consistency. Means and standard errors are shown. All paired comparisons between Diarrhea Days, Normal Stool Days, and Constipation Days are significant at p<.05.
Association of IBS symptoms with IBS subtypes
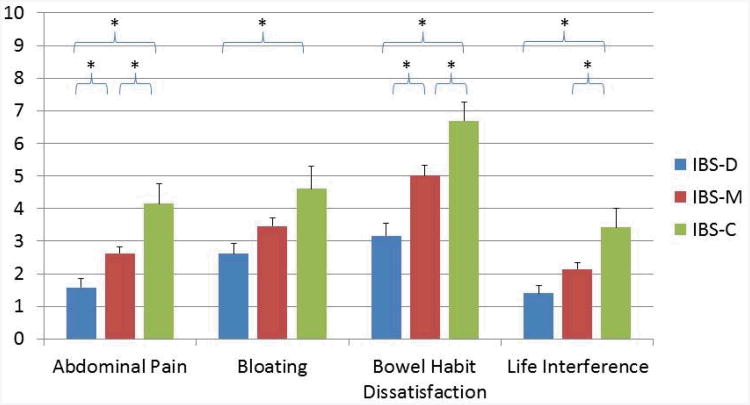
Table 5 compares IBS subtypes (subtype classification based on Rome III Diagnostic Questionnaire) with respect to the average severity of abdominal pain, bloating, dissatisfaction with bowel habits, and interference with life activities across all days. For all 4 symptoms IBS-C patients reported significantly more symptom severity than IBS-D patients. This is contrary to what one might expect because loose/watery BMs were more frequently associated with pain and other symptoms than hard/lumpy stools (Figure 1). It suggests the hypothesis that symptom distress in IBS-C patients is unrelated to the occurrence of a BM. To test this hypothesis, we compared the IBS subtypes with respect to the severity of their IBS symptoms on days when they did not have BMs. Figure 2 supports this post hoc hypothesis by showing that all 4 symptoms were more severe in IBS-C patients compared to IBS-D patients on days when no BMs occurred.
Table 5.
Overall Association of IBS Subtype with Symptoms of IBS.
| Symptoms | All IBS | IBS-D | IBS-M | IBS-C |
|---|---|---|---|---|
| Abdominal pain | 3.44 (1.91) | 2.91 (1.74) | 3.51 (1.77) | 4.52 (2.47)D |
| Bloating | 3.80 (2.17) | 3.30 (1.92) | 3.87 (2.10) | 4.79 (2.79)D |
| Dissatisfaction with bowel habits | 4.55 (2.01) | 3.80 (1.95) | 4.74 (1.93 | 5.65 (1.97)D,M |
| Interference with life activities | 2.97 (1.80) | 2.57 (1.61) | 3.03 (1.72) | 3.71 (2.40)D |
Significantly different from IBS-D;
Significantly different from IBS-M.
Figure 2.
Symptom severity in different IBS subtypes on days with no bowel movements. Brackets show comparisons that are significant at p<.05.
Effects of cumulative days without a bowel movement on IBS symptoms in patients with IBS-C
The observation that on days with no BMs, IBS-C patients have worse symptoms than IBS-D or IBS-M patients (Figure 2) suggests that, in IBS-C, symptoms may result from the cumulative distention of the bowel with stool. To test this hypothesis, we performed another post-hoc test to determine whether the severity of pain and bloating increased with the cumulative number of days without a BM in patients with IBS-C. The data support this hypothesis: Average daily pain ratings (0-10 scale) were 4.1 after one day without a BM, 5.0 after 2 days with no BM, 5.7 after 3 days, 7.5 after 4 days, and 7.2 after 5 days. Day 1 pain ratings were significantly different from Day 4 and Day 5 by paired t-tests (p<.05). Similarly, average daily bloating ratings (0-10 scale) were 4.5 on the first day without a BM, 5.6 after 2 days, 5.9 after 3 days, 6.4 after 4 days, and 6.3 after 5 days. Paired t-tests showed that Day 1 bloating ratings were significantly different from Day 5 (p<.05). The number of IBS-C patients available for analysis was 16 for Day 2, 12 for Day 3, 6 for Day 4, and 3 for Day 5.
Differences between retrospective IBS symptom severity scores and diary based symptom severity scores
Analysis of the diary data showed that the IBS symptoms that make up the IBS Severity Scale differ significantly between the IBS subtypes, whereas at enrollment when subjects completed the IBS-SS retrospectively, no such differences between subtypes were found. To understand this discrepancy a post-hoc analysis was performed. When IBS-SS scores were computed based on diary responses and compared for the first and second month of diary days, the correlation between Month 1 and Month 2 was r=0.871 (Table 2). The correlation between scores on the baseline retrospective IBS-SS questionnaire and the diary based IBS-SS scores, on the other hand, were lower at r=0.618 for Month 1 and r=0.524 for Month 2.
Discussion
In this diary study, 185 well-characterized IBS patients provided Bristol Stool scores and other symptom ratings on consecutive BMs for an average of 73 consecutive days, yielding data on 24,642 stools. The principal findings from this large database were as follows:
The majority (58.2%) of all stools are normal in consistency (Bristol Stool Scores of 3-5).
Most IBS patients (77.7%) have both loose/watery stools and hard/lumpy stools, and they fluctuate between these extremes an average of 3 times per month. These frequent stool consistency fluctuations occur naturally in all IBS subtypes and are not due to taking laxatives or antidiarrheal medications.
Individual patients have stable distributions of stool types: the proportion of BMs that are loose/water correlates 0.783 between successive months and the proportion of BMs that are hard/lumpy correlates 0.852 between months.
The Rome III Diagnostic Questionnaire overestimates the frequency of abnormal stool types but identifies distinct patterns of stool consistency which are correlated with symptoms.
Loose/watery stools are more likely than hard/lumpy stools or normal consistency stools to be accompanied by symptoms of pain, urgency, and fecal incontinence, but…
Paradoxically, however, patients classified as IBS-C by the Rome criteria report more abdominal pain, bloating, dissatisfaction with bowel habits, and life interference than patients meeting Rome III criteria for IBS-D because IBS-C patients have more symptoms between BMs.
Variability in stool consistency within patients
It is commonly assumed (1) that IBS-C patients have almost exclusively hard/lumpy stools or a mixture of hard/lumpy stools and stools of normal consistency, and (2) that medications which cause looser stools are indicated for chronic use in these patients, whereas these medications are not prescribed to patients with mixed stool types. Similarly, medications designed to slow colonic transit and reduce diarrhea are prescribed for chronic use in patients with IBS-D. However, our data show that 77.7% of IBS patients fluctuate between loose/watery stools and hard/lumpy stools, with fluctuations occurring an average of 3 times per month. Only 10% of IBS patients had no loose/watery stools in their diary and only 13.1% had no hard/lumpy stools. These data suggest that daily, fixed-dose drug regimens which ignore the normal fluctuation of stool consistency may expose patients to an increased risk of adverse events, and that “as needed” drug dosing regimens should be considered.
Our findings of frequent fluctuation between loose/water stools and hard/lumpy stools in most IBS patients of all subtypes suggest that fluctuations in stool consistency between extremes might be a defining general characteristic of IBS. Pimentel et al20 also suggested that variability in the form and frequency of stools can be used to identify IBS-D patients and distinguish them from patients with organic causes of diarrhea. However, Pimental used a question on whether stool form and frequency vary within a day, and we found the co-occurrence of loose/watery and hard/lumpy stools within the same day to be relatively rare (1.8% of days).
In view of the frequent fluctuation of bowel habits between stool consistency extremes, one could question whether it is useful to separate IBS patients into subtypes based on the predominant stool type rather than assuming that most IBS patients will alternate and providing instruction for PRN management of both loose/watery and hard/lumpy stool types. However, we also found that the relative frequencies of hard/lumpy stools and of loose/watery stools remains relatively constant from month to month; and that there are significant differences in these relatively stable proportions between IBS-C and IBS-D. This suggests that separating IBS patients into subtypes based on stool consistency may be useful. Other investigators have also reported that IBS patients may change the subtype into which they would be placed by the Rome criteria if assessed over longer intervals of time such as 6 months to a year6,7. These studies used smaller periods of diary records to assess stool characteristics and may have underestimated the degree of stability.
Validation of the Rome III criteria for classification of IBS patients into subtypes
The agreement between classification of subtypes based on the retrospective Rome III Diagnostic Questionnaire and the prospective stool diary was modest (Chi square = 19.60; df = 9; p=.021). Most of the discrepancies appeared to be due to an over-estimation of the frequency of loose/watery and of hard/lumpy stools by the Rome questionnaire. This is shown by the fact that patients classified IBS-D by the Rome questionnaire either remained in that category when classified based on the stool diary, or they were reclassified as IBS-U because the proportion of loose/water BMs was below 25%. Similarly, patients classified IBS-C by the Rome questionnaire either retained this classification or were reclassified IBS-U. These differences may be largely explained by our use of a response scale from the Rome III Diagnostic Questionnaire which asked patients whether they had loose/watery stools (or hard/lumpy stools) “sometimes” or “often” rather than asking them whether this occurred 25% of the time. Patients may have not interpreted “sometimes” as the questionnaire developers intended. This problem can likely be addressed by the use of an alternative response scale for the Rome questionnaire.
Relationship between symptoms and stool consistency
We found that loose/watery bowel movements were more likely than hard/lumpy stools or normal stools to be associated with abdominal pain, urgency, and fecal soiling; and that patients reported more abdominal pain, bloating, dissatisfaction with bowel habits and interference with activities of daily life on days when they experienced loose/watery stools as compared to days on which they experienced hard/lumpy stools or stools of normal consistency (Figure 1). This agrees with previous reports9.
However, we found that the amount of symptoms associated with individual bowel movements is not a good predictor of the overall symptom burden of IBS in general. When all days are averaged together, patients with IBS-C (i.e., patients with chronic constipation) have significantly worse abdominal pain, bloating, dissatisfaction with bowel habits, and interference with life activities than patients with IBS-D (i.e., patients with chronic diarrhea; see Table 5). This suggests that in IBS-D bowel symptoms are triggered by defecation of loose/watery BMs whereas in IBS-C, these symptoms are temporally uncorrelated with defecation and are instead probably related to the chronic distention of the bowel with stool. This interpretation is supported by two post-hoc analyses: When IBS-C patients were compared to IBS-D patients on days when no BMs were reported, IBS-C patients had worse symptoms on those days than patients with IBS-D (Figure 2). Moreover, daily ratings of pain and bloating become progressively more severe with the cumulative number of days IBS-C patients have gone without a BM.
These observations may help clinicians to better understand and communicate with their patients regarding the different effects of diarrhea and constipation on the patient's quality of life. For patients with diarrhea, it is important to focus on the characteristics of the BMs such as urgency, frequency, volume, and association with soiling; modifying these stool characteristics may bring relief. For constipated patients, on the other hand, the patient is likely to be more concerned by the chronic symptoms of bloating, pain, and tenesmus that occur throughout the day and that may not show much change with defecation. These observations on possible different mechanisms for symptoms in IBS-D and IBS-C also have implications for how one might design outcome assessments that are more sensitive to the mechanism of action of drugs developed to treat IBS. For patients with IBS-D and for drugs designed to control diarrhea, it may be appropriate to assess IBS symptoms at the time of defecation whereas for patients with IBS-C and for drugs designed to relieve constipation, it may be more appropriate to emphasize daily symptom assessments that are unrelated to BMs.
Diary assessment
We also made the serendipitous observation that symptom diaries, when collected in a way that guarantees the symptom reports are made on a daily basis, provide a more sensitive and reliable method of assessing bowel symptoms than does a retrospective questionnaire. Greater sensitivity is shown by the fact that the diary data reveal significant differences between IBS subtypes in their overall IBS-SS scores and in individual IBS symptoms where as the IBS-SS questionnaire given at baseline showed no differences between IBS subtypes. Greater reliability of the diary method is shown by the fact that measures of symptom severity show a stronger correlation between two sequential months of diary recordings (range, .816 to .862) than between the baseline questionnaire and the diary assessments (range, .285 to .628). Table 2 also shows that patients overestimate their pain, bloating, dissatisfaction with bowel habits, and interference with life when they respond on a questionnaire as compared to when they report these symptoms on a daily diary. As a consequence, IBS-SS total scores are significantly greater for the retrospective questionnaire than for the diary method. We infer from these observations that symptom diaries are superior to retrospective questionnaires as outcome measures in treatment trials. The strong correlations between the first and second months suggest that one month of diary data will be adequate for most purposes.
Study strengths and limitations
Other studies have used daily symptom ratings to investigate patterns of stool consistency. However, our methodology has several advantages over comparable prior work: Previous studies have generally relied on paper diaries returned to the investigator at intervals of a few weeks. Paper diaries collected in this way are known to be vulnerable to non-adherence and recollection bias, because many subjects wait until it is time to return the diaries to the investigator and fill out several days retrospectively from memory or leave some days blank21, 22. By contrast, we required patients to report on their bowel symptoms each day via an internet website, reinforced daily completion via telephone and email contact the next day for any missing days, and used only continuous series of diary records for analysis. Additionally, the length of the diary records we collected averaged 73 days in contrast to 7 days23, 24, 14 days7, or 28 days6 in previous studies, providing a broader picture of symptom variation. The reliability of the assessment of symptoms and stool consistency is reflected by the very high degree of comparability of Month 1 and Month 2 data (Table 4).
The limitations of our study include a relatively small group of only 23 IBS-C patients. This small sub-sample limited the statistical power to assess the effects of cumulative days without a BM on symptoms of pain and bloating. A second limitation is that our sample was younger than usually encountered in studies of IBS (median age of 37 compared to 51 years in other studies25). This age difference likely reflects the requirement that patients should have daily internet access in order to participate. Lastly, we used the standard response scale in the Rome III Diagnostic Questionnaire which asks patients whether they have hard/lumpy stools (or loose/watery stools) “Never or rarely”, “Sometimes”, “Often”, etc. instead of the alternative response scales which ask them whether they have hard/lumpy stools “About 25% of the time”, “About 50% of the time”, etc. This likely contributed to the observed tendency for the Rome III Diagnostic Questionnaire to overestimate the frequency of hard/lumpy and loose/watery stools when a response of “sometimes” was equated with 25% of the time. However, the method we used is the current standard form of the Rome questionnaire, and our finding that it substantially over-estimates the amount of hard and loose stools suggests that alternative wording may be needed to subtype IBS.
Summary
We made three key observations that have implications for clinical practice: First, the finding that ¾ of IBS patients fluctuate between the extremes of loose/watery stools and hard/lumpy stools suggests that medications which target diarrhea or constipation may produce fewer side-effects and greater patient satisfaction if dosed “as needed” rather than on a fixed dose. Second, we found that different mechanisms appear to be responsible for pain and other bowel symptoms in diarrhea (defecation-related sensations) vs. constipation (cumulative distention of the bowel). This insight may improve our ability to communicate with patients about the causes of their discomfort and the goals of treatment. Third, we have shown that symptom diaries, collected by internet to guarantee timely reporting, are more sensitive and reliable than questionnaires or interviews for evaluating symptom severity and response to treatment.
Study Highlights.
What is Current Knowledge
IBS patients are sub-classified based on the average frequency of loose or watery stools and the average frequency of hard or lumpy stools.
Classification by predominant stool consistency is critical to management because current IBS drugs were designed to treat either constipation or diarrhea, and there is a risk of adverse events if they are given to patients with the wrong stool consistency.
Reports are inconsistent on the relationship between stool consistency and abdominal pain.
What is New Here
Approximately 78% of IBS patients of all subtypes fluctuate between the extremes of loose/watery stools and hard/lumpy stools; this suggests that IBS drugs might produce better outcomes and fewer side effects if prescribed “as needed” rather than on a fixed dose.
Abdominal pain appears to be caused by different pathophysiological mechanisms in IBS-D and IBS-C: in IBS-D, pain is associated with the passage of a loose/watery stool whereas in IBS-C, pain increases with distention from cumulative days without a stool.
Daily symptom monitoring through the internet is more sensitive and reliable than a questionnaire for assessing individual differences in symptom severity.
Acknowledgments
Financial support: This study was supported by a generous grant from McNeil Consumer Health, Inc, and by grant R01 DK31369 from the NIDDK.
Footnotes
- Olafur S Palsson, PsyD, planned and conducted the study, analyzed and interpreted the data, contributed to drafting the manuscript, and approved the final draft.
- Jeffrey S Baggish, MD, arranged financial support for the study, planned the study, interpreted the data, and approved the final draft.
- Marsha J Turner, MS, contributed to planning and conduct of the study, collecting and interpretation the data, and she approved the final draft.
- William E Whitehead, PhD, planned and conducted the study, collected and interpreted the data, drafted the manuscript, and approved the final draft.
- Dr. Palsson is an author of the Rome III Diagnostic Questionnaire.
- Dr. Baggish was an employee of McNeil Consumer Health during the period this study was carried out.
- Ms. Turner has no competing interests.
- Dr. Whitehead is a member of the Board of the Rome Foundation and an author of the Rome III Diagnostic Questionnaire. He has received honoraria for participation on advisory boards for Takeda Pharmaceuticals and Ono Pharmaceuticals in the past 12 months.
Reference List
- 1.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. In: Drossman DA, Corazziari E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, Whitehead WE, editors. Rome III: The Functional Gastrointestinal Disorders. Third. Vol. 2006. McLean, VA: Degnon Associates; pp. 487–555. [Google Scholar]
- 2.Drossman DA, Chey WD, Johanson JF, Fass R, Scott C, Panas R, Ueno R. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome--results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther. 2009;29:329–341. doi: 10.1111/j.1365-2036.2008.03881.x. [DOI] [PubMed] [Google Scholar]
- 3.Johnston JM, Kurtz CB, MacDougall JE, Lavins BJ, Currie MG, Fitch DA, O'Dea C, Baird M, Lembo AJ. Linaclotide improves abdominal pain and bowel habits in a phase IIb study of patients with irritable bowel syndrome with constipation. Gastroenterol. 2010;139:1877–1886. doi: 10.1053/j.gastro.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 4.Muller-Lissner SA, Fumagalli I, Bardhan KD, Pace F, Pecher E, Nault B, Ruegg P. Tegaserod, a 5-HT(4) receptor partial agonist, relieves symptoms in irritable bowel syndrome patients with abdominal pain, bloating and constipation. Aliment Pharmacol Ther. 2001;15:1655–1666. doi: 10.1046/j.1365-2036.2001.01094.x. [DOI] [PubMed] [Google Scholar]
- 5.Camilleri M, Northcutt AR, Kong S, Dukes GE, McSorley D, Mangel AW. Efficacy and safety of alosetron in women with irritable bowel syndrome: a randomised, placebo-controlled trial. Lancet. 2000;355:1035–1040. doi: 10.1016/S0140-6736(00)02033-X. [DOI] [PubMed] [Google Scholar]
- 6.Garrigues V, Mearin F, Badia X, Balboa A, Benavent J, Caballero A, Dominguez E, Diaz-Rubio M, Roset M, Figueras M, Cucala M. Change over time of bowel habit in irritable bowel syndrome: a prospective, observational, 1-year follow-up study (RITMO study) Aliment Pharmacol Ther. 2007;25:323–332. doi: 10.1111/j.1365-2036.2006.03197.x. [DOI] [PubMed] [Google Scholar]
- 7.Drossman DA, Morris CB, Hu Y, Toner BB, Diamant N, Leserman J, Shetzline M, Dalton C, Bangdiwala SI. A prospective assessment of bowel habit in irritable bowel syndrome in women: defining an alternator. Gastroenterol. 2005;128:580–589. doi: 10.1053/j.gastro.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Dorn SD, Morris CB, Hu Y, Toner BB, Diamant N, Whitehead WE, Bangdiwala SI, Drossman DA. Irritable bowel syndrome subtypes defined by Rome II and Rome III criteria are similar. J Clin Gastroenterol. 2009;43:214–220. doi: 10.1097/MCG.0b013e31815bd749. [DOI] [PubMed] [Google Scholar]
- 9.Hellstrom PM, Saito YA, Bytzer P, Tack J, Mueller-Lissner S, Chang L. Characteristics of Acute Pain Attacks in Patients With Irritable Bowel Syndrome Meeting Rome III Criteria. Am J Gastroenterol. 2011 doi: 10.1038/ajg.2011.78. [DOI] [PubMed] [Google Scholar]
- 10.Ragnarsson G, Bodemar G. Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS). Patients' description of diarrhea, constipation and symptom variation during a prospective 6-week study. Eur J Gastroenterol Hepatol. 1998;10:415–421. doi: 10.1097/00042737-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Chang L, Lee OY, Naliboff B, Schmulson M, Mayer EA. Sensation of bloating and visible abdominal distension in patients with irritable bowel syndrome. Am J Gastroenterol. 2001;96:3341–3347. doi: 10.1111/j.1572-0241.2001.05336.x. [DOI] [PubMed] [Google Scholar]
- 12.Houghton LA, Lea R, Agrawal A, Reilly B, Whorwell PJ. Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit. Gastroenterol. 2006;131:1003–1010. doi: 10.1053/j.gastro.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Bharucha AE, Seide BM, Zinsmeister AR, Melton LJ., III Insights into normal and disordered bowel habits from bowel diaries. Am J Gastroenterol. 2008;103:692–698. doi: 10.1111/j.1572-0241.2007.01631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson WG, Drossman DA, Talley NJ, Walker L, Whitehead WE. Rome III diagnostic questionnaire for the adult functional GI disorders (including alarm questions) and scoring algorithm. In: Drossman DA, Cprazzoaro E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, Whitehead WE, editors. Rome III: The Functional Gastrointestinal Disorders. III. Vol. 2006. McLean, VA: Degnon Associates, Inc.; pp. 917–951. [Google Scholar]
- 15.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Alimentary Pharmacology & Therapeutics. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 16.Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, Jia H, Bangdiwala SI. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95:999–1007. doi: 10.1111/j.1572-0241.2000.01941.x. [DOI] [PubMed] [Google Scholar]
- 17.Patrick DL, Drossman DA, Frederick IO, Dicesare J, Puder KL. Quality of life in persons with irritable bowel syndrome - Development and validation of a new measure. Digestive Diseases and Sciences. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 18.Derogatis LR. BSI 18 Brief Symptom Inventory 18: Administration, scoring, and procedures manual. NCS Pearson,Inc; 2000. [Google Scholar]
- 19.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scandinavian Journal of Gastroenterology. 1997;32:920–924. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 20.Pimentel M, Hwang L, Melmed GY, Low K, Vasiliauskas E, Ippoliti A, Yang J, Lezcano S, Conklin JL, Sahakian A. New clinical method for distinguishing D-IBS from other gastrointestinal conditions causing diarrhea: the LA/IBS diagnostic strategy. Dig Dis Sci. 2010;55:145–149. doi: 10.1007/s10620-008-0694-z. [DOI] [PubMed] [Google Scholar]
- 21.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. BMJ. 2002;324:1193–1194. doi: 10.1136/bmj.324.7347.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazze RS, Shamoon H, Pasmantier R, Lucido D, Murphy J, Hartmann K, Kuykendall V, Lopatin W. Reliability of blood glucose monitoring by patients with diabetes mellitus. Am J Med. 1984;77:211–217. doi: 10.1016/0002-9343(84)90693-4. [DOI] [PubMed] [Google Scholar]
- 23.Walter SA, Kjellstrom L, Talley NJ, Andreasson AN, Nyhlin H, Agreus L. Prospective diary evaluation of unexplained abdominal pain and bowel dysfunction: a population-based colonoscopy study. Dig Dis Sci. 2011;56:1444–1451. doi: 10.1007/s10620-010-1468-y. [DOI] [PubMed] [Google Scholar]
- 24.Walter SA, Kjellstrom L, Nyhlin H, Talley NJ, Agreus L. Assessment of normal bowel habits in the general adult population: the Popcol study. Scand J Gastroenterol. 2010;45:556–566. doi: 10.3109/00365520903551332. [DOI] [PubMed] [Google Scholar]
- 25.Whitehead WE, Levy RL, Von KM, Feld AD, Palsson OS, Turner M, Drossman DA. The usual medical care for irritable bowel syndrome. Aliment Pharmacol Ther. 2004;20:1305–1315. doi: 10.1111/j.1365-2036.2004.02256.x. [DOI] [PubMed] [Google Scholar]