Abstract
Background
Advances in technique, technology, and perioperative care have allowed for the more frequent performance of complex and extended hepatic resections. The purpose of this study was to determine if this increasing complexity has been accompanied by a rise in liver-related complications.
Methods
A large prospective single-institution database of patients who underwent hepatic resection was used to identify the incidence of liver-related complications. Liver resections were divided into an early era and a late era with equal number of patients (surgery performed before or after 18 May 2006). Patient characteristics and perioperative factors were compared between the two groups.
Results
Between 1997 and 2011, 2,628 hepatic resections were performed, with a 90-day morbidity and mortality rate of 37 and 2 %, respectively. We identified higher rates of repeat hepatectomy (12.2 vs 6.1 %; p<0.001), two-stage resection (4.0 vs 1 %; p<0.001), extended right hepatectomy (17.6 vs 14.6 %; p=0.04), and preoperative portal vein embolization (9.1 vs 5.9 %; p<0.001) in the late era. The incidence of perihepatic abscess (3.7 vs 2.1 %; p=0.02) and hemorrhage (0.9 vs 0.3 %; p=0.045) decreased in the late era and the incidence of hepatic insufficiency (3.1 vs 2.6 %; p=0.41) remained stable. In contrast, the rate of bile leak increased (5.9 vs 3.7 %; p=0.011). Independent predictors of bile leak included bile duct resection, extended hepatectomy, repeat hepatectomy, en bloc diaphragmatic resection, and intraoperative transfusion.
Conclusions
The complexity of liver surgery has increased over time, with a concomitant increase in bile leak rate. Given the strong association between bile leak and other poor outcomes, the development of novel technical strategies to reduce bile leaks is indicated.
Keywords: Bile leak, Liver-related complication, Trend, Extended hepatectomy, Complexity
Introduction
The safety of liver resection has improved markedly over the past decades. Now, liver resections can be performed with operative mortality rate of <5 % at high-volume centers.1–3 These improvements have paralleled the better understanding of liver anatomy and physiology, more careful patient selection, and advances in surgical technique and perioperative care. Our group has reported on hemostatic approaches for liver resection to reduce intraoperative blood loss and the need for perioperative blood transfusions.1 We have also extensively reported on strategies to reduce the risk of hepatic insufficiency after major hepatectomies (e.g., use of portal vein embolization (PVE) and accurate definition of future liver remnant volume).4–7
Despite an overall decrease in complications following liver resection, the incidence of bile leak still remains considerable, ranging among 2.6 and 33 % in the largest series.2,8–11 Bile leak remains a major cause of postoperative morbidity, often leading to a prolonged hospital stay, delayed removal of abdominal drains, and need for additional diagnostic tests and interventions, with a related mortality ranging from 0 to 39 %.2,9–11
At our institution, the progressive expansion of indications for liver resection has led to an increasingly complex surgical practice, with greater use of extended hepatectomies, repeat hepatectomies, and two-stage resections.12–15 This experience provides an opportunity to reevaluate the morbidity associated with hepatic resection in a contemporary series from a high-volume center. The major objective of this study was to evaluate how the scope and frequency of liver-related complications have changed with the evolution of our surgical practice.
Material and Methods
Patients and Preoperative Care
After approval from the Institutional Review Board of MD Anderson Cancer Center, prospectively collected clinicopathological data of 2,628 liver resections performed in our institution between January 1998 and October 2011 were reviewed. Patients who underwent only an ablative procedure (e.g., cryotherapy, radiofrequency, and ethanol ablation) or a wedge biopsy without resection were not included in the analysis. To analyze the changes in our practice and their impact on short-term outcomes over time, cases were divided into two groups with equal numbers of patients (1,314 liver resections each): an early era and a late era (resection performed before/on and after 18 May 2006).
The preoperative assessment of patients in this series included medical history and physical examination, liver function tests (aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, bilirubin, albumin, and coagulation tests), and computed tomography using a liver protocol (rapid injection of 3 to 5 ml/s of intravenous contrast and 2.5- to 5-mm cuts through the liver). In patients scheduled to undergo major liver resection, the future liver remnant volume was calculated as previously described.4,7 If the calculated standardized future liver remnant volume was inadequate (<20 % of the total liver volume in patients with normal liver, <30 % in patients with fibrosis or liver injury, or <40 % in patients with cirrhosis), preoperative PVE was performed.1,5,13,16 In patients with liver injury, degree of cirrhosis was classified using the Child–Pugh system; liver resection was generally offered only to Child A and B patients without ascites or encephalopathy. In jaundiced patients, endoscopic or percutaneous biliary drainage was performed preoperatively to achieve a total bilirubin level of <2 mg/dl.12
Operations
A standardized operative technique was used. An inverted T-shaped subcostal incision was used during the earlier years. More recently, a reversed L-shaped right upper quadrant incision was performed.17 Intraoperative ultrasonography with a 5- to 7.5-MHz probe (Aloka Co. Ltd., Tokyo, Japan) was used to detect nodules that were not identified by preoperative imaging studies and to delineate the anatomic relationships between the intrahepatic vasculobiliary structures and tumors. The liver was mobilized by dividing the round, triangular, and falciform ligaments as appropriate. Operative procedures were selected on the basis of disease extent and location, and margins were evaluated intraoperatively.1
The parenchymal transection technique was chosen by the surgeon on the basis of the tumor size, the anticipated extent of the resection, and the condition of the liver parenchyma. For major hepatectomies, hemi-Glisson pedicle occlusion was used, with or without intermittent total hepatic pedicle occlusion (Pringle maneuver) for periods of up to 15 min, alternating with 5 min of restored inflow. Postoperative drains were used selectively and at the surgeon’s discretion.
Liver resections were classified according to the Brisbane 2000 Terminology.18 Associated procedures were defined as any additional hepatic and extrahepatic procedures performed. Associated liver procedures were defined as any liver-specific procedures performed in addition to the main resection (e.g., wedge resection, portal lymph node dissection, en bloc diaphragmatic resection, and vascular or biliary reconstruction). Associated nonliver procedures were defined as any additional abdominal extrahepatic procedure (gastric, duodenal, pancreatic, bowel, uterine and adnexal, adrenal, mesenteric, kidney, and spleen resections). Hepatic artery pump placement, ablative procedures, cholecystectomy, peritoneal biopsy, colostomy/ileostomy reversal, liver wedge biopsy, and abdominal hernia repair were not considered additional procedures.
Postoperative Care
Following operation, patients were typically monitored overnight in the recovery room and then transferred to the ward. When utilized, abdominal drains were removed prior to discharge, assuming the output was nonbilious and non-purulent. In case of suspected bile leak, the level of bilirubin in the abdominal drainage fluid was determined. Symptomatic postoperative fluid collections identified on imaging were drained percutaneously under ultrasound/CT guidance.
Postoperative Morbidity and Mortality
Postoperative complications included postoperative adverse events resulting from the liver resection or associated procedure. Complications were classified according to the Dindo Classification19: grade I and II complications were defined as minor complications and grade III, IV, and V complications were defined as major complications. Postoperative mortality was defined as any death that occurred within 90 days after operation. Perihepatic abscess, hemorrhage, liver insufficiency, and bile leak were defined as liver-related complications. Perihepatic abscess/collection was defined as a nonbilious collection requiring drainage. Hemorrhage was defined as bleeding requiring reoperation. Hepatic insufficiency was defined as a peak of serum bilirubin level >7 mg/dl at any time postoperatively, according to our previously published criteria.20 Bile leak was defined as bilirubin concentration in the drain fluid at least three times the serum bilirubin concentration on or after postoperative day 3 when fluid was analyzed or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis.21
Statistical Analysis
Statistical analysis was performed with SPSS statistical software (version 17.0; SPSS Inc., Chicago, IL, USA). Continuous data were expressed as the mean and standard deviation and compared with the Mann–Whitney U test. Categorical data were compared by the chi-square or Fisher exact test as appropriate. Variables with a significant impact on postoperative bile leak on univariate analysis were entered into multivariate analysis in a backward stepwise manner until all variables remaining in the model were significant. Multivariate analysis was performed by logistic regression. p<0.05 was considered statistically significant in all analyses.
Results
Patient Cohort and Outcomes
The mean age at the time of the liver resection was 57 years (±12.8). Patients were male in 52.3 % of cases. Repeat hepatectomy and planned second-stage hepatectomy were performed in 241 (9.2 %) and 66 (2.6 %) patients, respectively. PVE preceded liver resection in 227 (8.6 %) cases. Major liver resection was performed in 1,503 (57.2 %) patients, including 421 (16 %) extended right hepatectomies, 137 (5.2 %) extended left hepatectomies, 703 (26.7 %) right hepatectomies, 211 (8 %) left hepatectomies, and 31 (1.2%) mesohepatectomies. Monosegmentectomies or bisegmentectomies and wedge resections were performed in 586 (22.3 %) and 570 (21.8 %) patients, respectively (Table 1).
Table 1.
Patient and operative characteristics in the entire study period and in the two eras
| Total (n=2,628), n (%) | Early era (n=1,314), n (%) | Late era (n=1,314), n (%) | p value | |
|---|---|---|---|---|
| Age | 57 (±12.8) | 56.7 (±13.2) | 56.3 (±12.5) | 0.267 |
| Diabetes | 295 (11.5) | 137 (10.4) | 158 (12) | 0.194 |
| Hypertension | 1,049 (40.9) | 439 (33.4) | 610 (46.4) | <0.001 |
| ASA score >2 | 1,719 (66.6) | 668 (52.7) | 1,051 (80) | <0.001 |
| Obesity (BMI>30) | 704 (29.8) | 306 (23.2) | 398 (30.3) | 0.019 |
| Sex male | 1,374 (52.3) | 679 (51.7) | 695 (52.9) | 0.559 |
| Cirrhosis | 82 (3.1) | 50 (3.8) | 32 (2.4) | 0.043 |
| Jaundice | 64 (2.4) | 33 (2.5) | 31 (2.4) | 0.795 |
| Positive hepatitis serology | 90 (3.4) | 56 (4.3) | 34 (2.6) | 0.018 |
| Repeat hepatectomy | 241 (9.2) | 80 (6.1) | 161 (12.2) | <0.001 |
| Previous PVE | 226 (8.6) | 77 (5.9) | 149 (11.4) | <0.001 |
| Two-stage hepatectomy | 66 (2.5) | 13 (1) | 53 (4) | <0.001 |
| Major hepatectomy | 1,503 (57.2) | 796 (60.5) | 707 (53.8) | <0.001 |
| Meso-hepatectomy | 31 (1.2) | 14 (1.1) | 17 (1.3) | 0.718 |
| Right hepatectomy | 703 (26.8) | 396 (30.2) | 307 (23.3) | <0.001 |
| Left hepatectomy | 211 (8) | 116 (8.8) | 95 (7.2) | 0.129 |
| Extended hepatectomy | 558 (21.2) | 270 (20.6) | 288 (21.9) | 0.417 |
| Extended right hepatectomy | 421 (16) | 191 (14.6) | 230 (17.6) | 0.04 |
| Extended left hepatectomy | 137 (5.3) | 79 (6) | 58 (4.4) | 0.073 |
| Caudate resection | 122 (4.6) | 48 (3.7) | 74 (5.6) | 0.016 |
| Associated procedures | 1,102 (41.9) | 486 (37) | 616 (46.8) | <0.001 |
| Liver-associated procedures | 730 (27.8) | 118 (9) | 156 (11.9) | 0.016 |
| Bile duct resection | 131 (5) | 74 (5.6) | 57 (4.3) | 0.125 |
| Additional wedge resection | 268 (10.2) | 111 (8.5) | 157 (11.9) | 0.003 |
| Portal lymph node dissection | 468 (17.8) | 196 (14.9) | 273 (20.8) | <0.001 |
| En bloc diaphragm resection | 123 (4.7) | 49 (3.7) | 74 (5.6) | 0.021 |
| Nonliver-associated procedures | 506 (19.3) | 226 (17.2) | 280 (21.3) | 0.008 |
| Operation time (min) | 211 (±126.1) | 205.5 (±127.7) | 216 (±124.5) | 0.019 |
| Operation time≥180 min | 1,332 (50.7) | 620 (47.2) | 712 (54.1) | <0.001 |
| Blood loss (ml) | 405 (±580) | 440 (±594) | 370 (±563) | 0.002 |
| Blood loss≥1,000 ml | 188 (7.2) | 137 (10.5) | 51 (3.9) | <0.001 |
| Pringle | 1,692 (58.7) | 852 (65.1) | 840 (63.9) | 0.534 |
| Intraoperative transfusion | 358 (12.4) | 209 (16.4) | 149 (11.4) | <0.001 |
Data are expressed as absolute numbers (percentage) or means (±standard deviation)
ASA American Society of Anesthesiologists, BMI body mass index, PVE portal vein embolization
The indication for liver resection was colorectal liver metastases (CRLM) in 1,509 cases (57.4 %), hepatocellular carcinoma in 182 cases (6.9 %), benign tumors in 67 cases (2.3 %), biliary tract tumors (Klatskin, intrahepatic cholangiocarcinoma, and gallbladder carcinoma) in 201 cases (7.6 %), neuroendocrine tumor metastases in 216 cases (8.2 %), and other malignancies in 453 cases (17.3 %). Rates of complications, major complications, and mortality following liver resection were 36.2, 14.2, and 2.3 %, respectively. The rate of liver-related complications was 9.8 % and included 126 cases of bile leak (4.8 %), 75 cases of hepatic insufficiency (2.6 %), 16 cases of hemorrhage (0.6 %), and 76 cases of perihepatic abscess/collection (2.9 %) (Table 2).
Table 2.
Indications, pathologic characteristics, and outcomes in the entire study period and in the two eras
| Total (n=2,628), n (%) | Early era (n=1,314), n (%) | Late era (n=1,314), n (%) | p value | |
|---|---|---|---|---|
| Surgical indication | ||||
| HCC | 182 (6.9) | 100 (6.2) | 82 (7.6) | 0.163 |
| Colorectal metastases | 1,509 (52.3) | 723 (55.1) | 786 (59.8) | 0.015 |
| Biliary tumors | 201 (7.6) | 99 (7.8) | 102 (7.5) | 0.834 |
| Other malignancies | 453 (17.3) | 234 (17.8) | 219 (16.7) | 0.428 |
| Benign | 67 (2.3) | 53 (4) | 14 (1.1) | <0.001 |
| NET metastases | 216 (8.2) | 104 (7.9) | 112 (8.5) | 0.578 |
| Number of tumors | 2.5 (±3.23) | 2.3 (±2.6) | 2.6 (±3.9) | 0.021 |
| Multiple tumors | 1,194 (46.7) | 573 (44.8) | 621 (48.6) | 0.057 |
| Tumors≥3 | 447 (17.5) | 202 (15.8) | 245 (19.2) | 0.025 |
| Diameter (mm) | 25 (1–250) | 37.6 (±35) | 36.2 (±32.7) | 0.664 |
| Diameter≥30 mm | 1,194 (46.8) | 613 (48) | 581 (48.7) | 0.239 |
| Steatosis>30 % | 318 (18.1) | 155 (11.8) | 163 (12.4) | 0.643 |
| Complications | 964 (36.7) | 396 (30.2) | 568 (43.2) | <0.001 |
| Major complications | 372 (14.1) | 187 (14.2) | 185 (14) | 0.898 |
| Liver-related complications | 257 (9.8) | 134 (10.2) | 123 (9.4) | 0.313 |
| Bile leak | 126 (4.8) | 49 (3.7) | 77 (5.9) | 0.011 |
| Hepatic insufficiency | 75 (2.6) | 51 (3.1) | 34 (2.6) | 0.408 |
| Hemorrhage | 16 (0.6) | 12 (0.9) | 4 (0.3) | 0.045 |
| Perihepatic abscess/collection | 76 (2.9) | 48 (3.7) | 28 (2.1) | 0.02 |
| Nonliver-related complication | 707 (26.9) | 262 (20) | 445 (33.8) | <0.001 |
| Urinary | 106 (3.7) | 21 (1.6) | 86 (6.5) | <0.001 |
| Cardiac | 70 (3) | 19 (1.4) | 59 (4.5) | <0.001 |
| Respiratory | 159 (6.1) | 78 (5.9) | 81 (6.2) | 0.814 |
| Length of hospital stay (days) | 8 (±5.9) | 8.2 (±6.4) | 7.8 (±5.4) | 0.015 |
| Mortality | 60 (2.3) | 32 (2.4) | 28 (2.1) | 0.597 |
Data are expressed as absolute numbers (percentage) or means (±standard deviation)
HCC hepatocellular carcinoma, NET neuroendocrine tumor
Comparison of Two Eras
A comparison of clinical and pathologic features during the two eras is summarized in Tables 1 and 2. The frequency of preoperative hypertension, ASA score >2, and body mass index >30 increased in the late era (p< 0.001). Compared to the early era, we performed more repeat hepatectomies (161 vs 80, p<0.001) and more two-stage hepatectomies (53 vs 13, p<0.001) and we employed more frequently preoperative PVE (150 vs 77, p<0.001) during the late era. Major hepatectomies decreased in the late era (707 vs 796, p<0.001), as a consequence of a decreased number of right hepatectomies (307 vs 396, p<0.001). However, in the late era, the number of extended right hepatectomy increased significantly (230 vs 191, p=0.04), as well as the number of caudate resections (74 vs 48, p=0.016) and of en bloc diaphragm resections (74 vs 49, p=0.021) (Fig. 1).
Fig. 1.
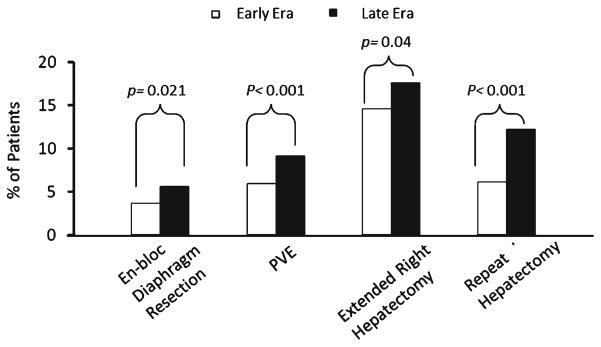
Comparison of surgical complexity between the early era and the late era
Associated liver and nonliver procedures increased in the late era (p=0.016 and p=0.008, respectively). Mean operative time increased from 205 to 216 min (p=0.019). We also observed a reduction of intraoperative estimated blood loss (EBL), from a mean of 440 to 370 ml (p=0.002) in the late era. The number of patients requiring transfusion decreased in the late era, from 209 to 149 (p<0.001). More patients in the late era were treated for CRLM (786 vs 723, p=0.015). Overall complication rate increased from 30.2 to 43.2 % (p<0.001); however, major complications and mortality rates did not change significantly. The rate of liver-related complications did not change significantly in two eras (p=0.313). Comparisons of rates of specific liver-related complication revealed a stable incidence of hepatic insufficiency (p=0.408), decreasing incidences of perihepatic abscess/collection and hemorrhage (p=0.02 and p= 0.045, respectively), and an increasing incidence of bile leak (from 3.7 to 5.9 %, p=0.011) (Fig. 2).
Fig. 2.
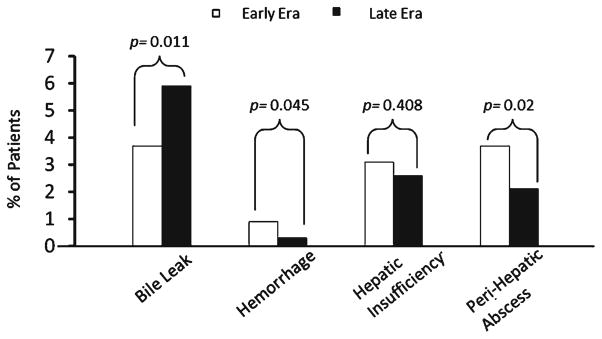
Comparison of liver-related complications between the early era and the late era
Further, when we excluded 131 patients who underwent a bilio-enteric anastomosis, a significant increase in bile leak rates persisted (3.3 % [40/1198] in the early era vs 5.2 % [62/1197] in the late era, p=0.034). This difference remained significant when patients were stratified by type of resection (minor vs major). Patients who underwent major resection in the late era had a higher bile leak rate than those who underwent a major resection in the early era (9.2 % [57/623] vs 4.7 % [35/ 743], p=0.005).
Risk Factors for Bile Leak
On univariate analysis, several variables were associated with bile leak, including preoperative jaundice, PVE, liver resection performed for biliary tumors, repeat hepatectomy, two-stage resection, extended right or left hepatectomy, caudate resection, en bloc diaphragm resection, bile duct resection and reconstruction, liver-associated procedures, operative duration >180 min, EBL >1,000 ml, tumor diameter ≥30 mm, portal lymph node dissection, and intraoperative transfusion. On multivariate analysis, repeat hepatectomy, bile duct resection, intraoperative transfusion, en bloc diaphragm resection, and extended right and left hepatectomies were associated with an increased risk of bile leak (Table 3).
Table 3.
Univariate and multivariate analysis of bile leak risk factors
| Variables | Univariate analysis
|
Multivariate analysis
|
|||
|---|---|---|---|---|---|
| Bile leak
| |||||
| No (n=2,502), n (%) | Yes (n=126), n (%) | p value | Risk ratio (95 % confidence interval) | p value | |
| Age>65 | 698 (27.9) | 29 (23) | 0.232 | ||
| Sex: male | 1,305 (52.2) | 69 (54.8) | 0.568 | ||
| Diabetes | 285 (11.7) | 10 (8.2) | 0.44 | ||
| Hypertension | 991 (40.6) | 58 (47.5) | 0.27 | ||
| ASA score>2 | 1,627 (66.2) | 92 (74.2) | 0.065 | ||
| BMI>30 | 692 (29.2) | 36 (30) | 0.853 | ||
| Preoperative jaundice | 50 (2) | 14 (11.1) | <0.001 | NS | |
| PVE | 199 (8) | 27 (21.4) | <0.001 | NS | |
| Indication | |||||
| HCC | 174 (7) | 8 (6.3) | 0.794 | ||
| Colorectal | 1,445 (57.8) | 64 (50.8) | 0.123 | ||
| Biliary tumors | 181 (7.2) | 20 (15.9) | <0.001 | NS | |
| Other malignancies | 432 (17.3) | 21 (16.7) | 0.862 | ||
| Benign tumors | 63 (2.5) | 4 (3.2) | 0.648 | ||
| NET metastases | 207 (8.3) | 9 (7.1) | 0.652 | ||
| Repeat hepatectomy | 223 (8.9) | 18 (14.3) | 0.041 | 2.078 (1.208–3.590) | 0.009 |
| Second-stage hepatectomy | 56 (2.2) | 10 (7.9) | <0.001 | NS | |
| Right hepatectomy | 669 (26.7) | 34 (27) | 0.952 | ||
| Left hepatectomy | 205 (8.2) | 6 (4.8) | 0.167 | ||
| Extended right hepatectomy | 375 (15) | 46 (36.5) | <0.001 | 2.689 (1.726–4.189) | <0.001 |
| Extended left hepatectomy | 118 (4.7) | 19 (15.1) | <0.001 | 4.399 (2.485–7.788) | <0.001 |
| Caudate resection | 105 (4.2) | 17 (13.5) | <0.001 | NS | |
| Associated procedures | 1,041 (41.6) | 61 (48.4) | 0.131 | ||
| Liver procedures | 683 (27.3) | 45 (35.7) | 0.042 | NS | |
| Bile duct resection | 107 (4.3) | 24 (19) | <0.001 | 4.195 (2.397–7.339) | <0.001 |
| Lymph node dissection | 447 (17.9) | 31 (24.6) | 0.056 | ||
| Additional wedge resection | 263 (10.5) | 5 (4) | 0.018 | NS | |
| En bloc diaphragm resections | 111 (4.4) | 12 (9.5) | 0.008 | 2.226 (1.153–4.295) | 0.017 |
| Pancreatic/duodenal resection | 48 (1.9) | 2 (1.6) | 0.837 | ||
| Operation time≥180 min | 1,249 (49.9) | 83 (65.9) | <0.001 | NS | |
| Blood loss≥1,000 ml | 169 (6.8) | 19 (15.1) | <0.001 | NS | |
| Intraoperative transfusion | 320 (13) | 38 (30.6) | <0.001 | 2.234 (1.450–3.443) | <0.001 |
| Pringle maneuver | 1,599 (64) | 93 (73.8) | 0.025 | NS | |
| Tumors≥3 | 422 (17.3) | 25 (20.5) | 0.368 | ||
| Tumor diameter≥30 mm | 1,122 (46.2) | 72 (59) | 0.006 | NS | |
Data are expressed as absolute numbers (percentage). Logistic regression multivariate analysis included all variables with p<0.05 in univariate analysis
ASA American Society of Anesthesiologists, BMI body mass index, PVE portal vein embolization, HCC hepatocellular carcinoma, NET neuroendocrine tumor
Discussion
In this study, we reported an increase in the complexity of hepatobiliary surgery at a tertiary referral center, characterized by the more frequent utilization of repeat hepatectomy, extended right hepatectomy, en bloc diaphragmatic resection, and preoperative PVE. Despite this increase in complexity, liver-related complication rates remained stable, except for bile leak rates, which increased significantly, from 3.7 % in the early era to 5.9 % in the late era.
We focused our analysis of outcomes on liver-related complications, which remain to be the most common and serious complications following a liver resection and account for most perioperative deaths. In line with previous large series,22,23 we found that hepatic insufficiency, perihepatic abscess/collection, and hemorrhage rates decreased or remained stable over time. This may reflect ongoing efforts aimed at increasing the safety of liver resection.1,5–7,12 In this context, increasing bile leak rate in the late era is an unexpected result. Few prior studies reported changes in the rate of bile leak over time. Poon et al.23 showed a reduction in bile leak incidence; nevertheless, their analysis did not focus on risk factors for bile leak, and thus, it is difficult to explain this trend. Cescon et al.22 showed increasing bile leak rates presented in the context of a slightly increasing overall morbidity and mortality, which the authors attributed to the expansion of surgical indications in the late period. Finally, Lam et al.24 and Yamashita et al.8 reported decreasing rates of bile leak in the late period, which they attributed to the introduction of intraoperative bile leak tests.
In order to better understand the reason for this increasing bile leak incidence in the late era, we identified independent predictors of bile leak: right and left extended hepatectomies, intraoperative transfusion, bile duct resection, reoperative resection, and en bloc diaphragmatic resection. The frequencies of three of these factors, bile duct resection, left extended hepatectomy, and intraoperative transfusion, did not change significantly over time. Bile duct resection and reconstruction represent an important risk factor for bile leak25; in our series, 18.3 % of patients who underwent biliary reconstruction developed a bile leak. This rate is comparable to those reported by previous studies analyzing such patients.13,26,27 Furthermore, bile leak is more common after extended hepatectomies,10 originating from transected intrahepatic bile ducts, and most often from the closed stump of the right or left major hepatic ducts.24 Recently, a bile leak rate of 28 % has been reported after extended right hepatectomy, preceded by a first-stage procedure involving right portal vein ligation and in situ liver parenchyma splitting to increase left liver hypertrophy.28 The association between intraoperative transfusions and postoperative bile leak has not been completely elucidated as transfusion requirement may be a surrogate factor identifying more technically challenging operations.
In our study, three predictors of bile leak including extended right hepatectomy, repeat hepatectomy, and en bloc diaphragmatic resection were more common in the late era, partially explaining the observed increase in bile leak rate. We believe that the increasing frequency of these factors is related, in large part, to the expansion of indications for resection of CRLM.14,29 In our series, 1,509 (57.4 %) liver resections were performed for CRLM, representing 55 % and 60 % of indications in the early era and in late era, respectively (p=0.015). The introduction of more effective chemotherapeutic agents, the increasing understanding of tumor biology, and the more liberal use of PVE have allowed for more aggressive surgical approach in patients with bilobar metastatic disease. A sequence of partial hepatectomy, followed by PVE and major liver resection, which was introduced in our later practice,15 as well as the use of repeat resections for liver recurrence,14,30 may provide durable oncological results as shown in previous studies. The increasing rate of bile leak in the late era may be an unanticipated consequence of these otherwise safe strategies.
Our study has some limitations. First, we performed a retrospective analysis of a cohort of patients treated over a 14-year period. This could account for an underestimation of bile leak, related to our intraoperative placement of drains in complex procedures (extended hepatectomies, en bloc diaphragmatic resections, and bile duct reconstruction). Moreover, our bile leak definition does not follow strictly the International Study Group of Liver Surgery criteria21; in our surgical practice, the bilirubin concentration on drain fluid was not measured routinely, but only when the fluid characteristics were suspect for bile leak. Taken together, these could be responsible for some underestimation of the bile leak rate in our patients.
Conclusion
This study demonstrates that, despite technical improvements, the progressive expansion of indications for liver surgery and more aggressive operative strategies are associated with a mild, but significant, increase in the rate of postoperative bile leak. This represents an important and incompletely addressed risk of hepatic resection. In our own experience, bile leak is associated with longer length of hospital stay (12 vs 8 days p<0.001) and increased mortality rate (10.3 vs 1.9 %, p<0.001). These findings are in line with previous studies reporting bile leak-related mortality rates ranging from 0 to 39 %.2,9–11 Given these associations, the development of novel technical strategies to reduce bile leak is indicated.
Acknowledgments
This research was supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant, CA016672.
Footnotes
Conflict of Interest: The authors report no conflicts of interest relevant to this article.
Presented at the 53rd Annual Meeting of the Society for Surgery of the Alimentary Tract, Tuesday, 22 May 2012; Abstract 34.
References
- 1.Palavecino M, Kishi Y, Chun YS, Brown DL, Gottumukkala VN, Lichtiger B, Curley SA, Abdalla EK, Vauthey JN. Two-surgeon technique of parenchymal transection contributes to reduced transfusion rate in patients undergoing major hepatectomy: analysis of 1,557 consecutive liver resections. Surgery. 2010;147:40–48. doi: 10.1016/j.surg.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 2.Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38–46. doi: 10.1016/s1072-7515(00)00261-1. [DOI] [PubMed] [Google Scholar]
- 4.Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IF, Caridi J. Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery. 2000;127:512–529. doi: 10.1067/msy.2000.105294. [DOI] [PubMed] [Google Scholar]
- 5.Ribero D, Abdalla EK, Madoff DC, Donadon M, Loyer EM, Vauthey JN. Portal vein embolization before major hepatectomy and its effects on regeneration, resectability and outcome. Br J Surg. 2007;94:1386–1394. doi: 10.1002/bjs.5836. [DOI] [PubMed] [Google Scholar]
- 6.Kishi Y, Madoff DC, Abdalla EK, Palavecino M, Ribero D, Chun YS, Vauthey JN. Is embolization of segment 4 portal veins before extended right hepatectomy justified? Surgery. 2008;144:744–751. doi: 10.1016/j.surg.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chun YS, Ribero D, Abdalla EK, Madoff DC, Mortenson MM, Wei SH, Vauthey JN. Comparison of two methods of future liver remnant volume measurement. J Gastrointest Surg. 2008;12:123–128. doi: 10.1007/s11605-007-0323-8. [DOI] [PubMed] [Google Scholar]
- 8.Yamashita Y, Hamatsu T, Rikimaru T, Tanaka S, Shirabe K, Shimada M, Sugimachi K. Bile leakage after hepatic resection. Ann Surg. 2001;233:45–50. doi: 10.1097/00000658-200101000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, Takayama T, Makuuchi M. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003;138:1198–1206. doi: 10.1001/archsurg.138.11.1198. [DOI] [PubMed] [Google Scholar]
- 10.Lo CM, Fan ST, Liu CL, Lai EC, Wong J. Biliary complications after hepatic resection: risk factors, management, and outcome. Arch Surg. 1998;133:156–161. doi: 10.1001/archsurg.133.2.156. [DOI] [PubMed] [Google Scholar]
- 11.Capussotti L, Ferrero A, Vigano L, Sgotto E, Muratore A, Polastri R. Bile leakage and liver resection: Where is the risk? Arch Surg. 2006;141:690–694. doi: 10.1001/archsurg.141.7.690. discussion 695. [DOI] [PubMed] [Google Scholar]
- 12.Vauthey JN, Pawlik TM, Abdalla EK, Arens JF, Nemr RA, Wei SH, Kennamer DL, Ellis LM, Curley SA. Is extended hepatectomy for hepatobiliary malignancy justified? Ann Surg. 2004;239:722–732. doi: 10.1097/01.sla.0000124385.83887.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kishi Y, Abdalla EK, Chun YS, Zorzi D, Madoff DC, Wallace MJ, Curley SA, Vauthey JN. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–548. doi: 10.1097/SLA.0b013e3181b674df. [DOI] [PubMed] [Google Scholar]
- 14.Andreou A, Aloia TA, Brouquet A, Vauthey JN. Recent advances in the curative treatment of colorectal liver metastases. Gastrointest Cancer Res. 2011;4:S2–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Brouquet A, Abdalla EK, Kopetz S, Garrett CR, Overman MJ, Eng C, Andreou A, Loyer EM, Madoff DC, Curley SA, Vauthey JN. High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol. 2011;29:1083–1090. doi: 10.1200/JCO.2010.32.6132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madoff DC, Abdalla EK, Gupta S, Wu TT, Morris JS, Denys A, Wallace MJ, Morello FA, Jr, Ahrar K, Murthy R, Lunagomez S, Hicks ME, Vauthey JN. Transhepatic ipsilateral right portal vein embolization extended to segment IV: improving hypertrophy and resection outcomes with spherical particles and coils. J Vasc Interv Radiol. 2005;16:215–225. doi: 10.1097/01.RVI.0000147067.79223.85. [DOI] [PubMed] [Google Scholar]
- 17.Chang SB, Palavecino M, Wray CJ, Kishi Y, Pisters PW, Vauthey JN. Modified Makuuchi incision for foregut procedures. Arch Surg. 2010;145:281–284. doi: 10.1001/archsurg.2010.7. [DOI] [PubMed] [Google Scholar]
- 18.Strasberg SM For the International Hepato-Pancreato-Biliary Association Terminology Committee Survey. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB. 2000;2:333–339. [Google Scholar]
- 19.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, Abdalla EK, Curley SA, Capussotti L, Clary BM, Vauthey JN. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007;204:854–862. doi: 10.1016/j.jamcollsurg.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 21.Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Buchler MW, Weitz J. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–688. doi: 10.1016/j.surg.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Cescon M, Vetrone G, Grazi GL, Ramacciato G, Ercolani G, Ravaioli M, Del Gaudio M, Pinna AD. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg. 2009;249:995–1002. doi: 10.1097/SLA.0b013e3181a63c74. [DOI] [PubMed] [Google Scholar]
- 23.Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg. 2004;240:698–708. doi: 10.1097/01.sla.0000141195.66155.0c. discussion 708–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lam CM, Lo CM, Liu CL, Fan ST. Biliary complications during liver resection. World J Surg. 2001;25:1273–1276. doi: 10.1007/s00268-001-0109-1. [DOI] [PubMed] [Google Scholar]
- 25.Erdogan D, Busch OR, Gouma DJ, van Gulik TM. Prevention of biliary leakage after partial liver resection using topical hemostatic agents. Dig Surg. 2007;24:294–299. doi: 10.1159/000103661. [DOI] [PubMed] [Google Scholar]
- 26.AJIJ, Appeltans BM, de Jong KP, Porte RJ, Peeters PM, Slooff MJ. Extrahepatic bile duct resection in combination with liver resection for hilar cholangiocarcinoma: a report of 42 cases. J Gastrointest Surg. 2004;8:686–694. doi: 10.1016/j.gassur.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Vauthey JN, Baer HU, Guastella T, Blumgart LH. Comparison of outcome between extended and nonextended liver resections for neoplasms. Surgery. 1993;114:968–975. [PubMed] [Google Scholar]
- 28.Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Horbelt R, Kroemer A, Loss M, Rummele P, Scherer MN, Padberg W, Konigsrainer A, Lang H, Obed A, Schlitt HJ. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405–414. doi: 10.1097/SLA.0b013e31824856f5. [DOI] [PubMed] [Google Scholar]
- 29.Yang AD, Brouquet A, Vauthey JN. Extending limits of resection for metastatic colorectal cancer: risk benefit ratio. J Surg Oncol. 2010;102:996–1001. doi: 10.1002/jso.21701. [DOI] [PubMed] [Google Scholar]
- 30.Mise Y, Imamura H, Hashimoto T, Seyama Y, Aoki T, Hasegawa K, Beck Y, Sugawara Y, Makuuchi M, Nakajima J, Kokudo N. Cohort study of the survival benefit of resection for recurrent hepatic and/or pulmonary metastases after primary hepatectomy for colorectal metastases. Ann Surg. 2010;251:902–909. doi: 10.1097/SLA.0b013e3181c9868a. [DOI] [PubMed] [Google Scholar]


