Abstract
Despite its success, Medicare Part D has been widely criticized for the gap in coverage, the so-called “doughnut hole”. We compare the use of prescription drugs among beneficiaries subject to the coverage gap with usage among beneficiaries who are not exposed to it. We find that the coverage gap does, indeed, disrupt the use of prescription drugs among seniors with diabetes. But the declines in usage are modest and concentrated among higher cost, brand-name medications. Demand for high cost medications such as antipsychotics, antiasthmatics, and drugs of the central nervous system decline by 8% to 12% in the coverage gap, while use of lower cost medications with high generic penetration such as beta blockers, ACE inhibitors and antidepressants decline by 3% to 4% after reaching the gap. More importantly, lower adherence to medications is not associated with increases in medical service use.
Keywords: Medicare Part D, Coverage gap
1. Introduction
By most metrics, the Medicare drug benefit (Part D) has been a success. Launched in January 2006, the program offers Medicare beneficiaries the option of enrolling in a prescription drug plan administered by a private company. More than 90 percent of Medicare beneficiaries have drug coverage at least as generous as the standard Part D benefit, and about 9 out of 10 Part D enrollees report being satisfied with their plan (Research 2011). At the same time, the costs of the program have been far lower than predicted—as much as 40% below what the Congressional Budget Office originally projected. Lower program costs are largely attributable to competition between plans, high rates of generic drug use, and the preference of beneficiaries for lowpremium plans.
Yet despite its success, Medicare Part D has been widely criticized for the gap in coverage—the so-called “doughnut hole”—affecting a large fraction of enrollees. Under the government’s 2012 standard benefit design, beneficiaries not receiving subsidies face a deductible, followed by a 25% co-insurance rate. But once they have spent a cumulative total of $2,930 on prescription drugs in a given plan year, they must start paying the full cost of their medications. Only after a beneficiary reaches a “catastrophic” limit of $4,700 in out-of-pocket spending (or $6,658 in total drug spending under the standard benefit) does coverage resume, with minimal cost-sharing thereafter. Although most companies offering Part D drug plans modify the standard design, they usually retain the coverage gap. Thus, many beneficiaries with moderate to high drug expenses, particularly the chronically ill, face breaks in coverage and out-of-pocket costs that may alter their demand for drug therapies. If the gap is prompting beneficiaries to use pharmaceuticals differently—especially if it leads them to discontinue an effective therapy—this could have important health consequences.
While the coverage gap is being phased out under the Patient Protection and Affordable Care Act, many beneficiaries will continue to face a break in coverage until 2020. Further, the coverage gap provides a natural experiment to assess how seniors respond to changes in the spot price of their medications. Prior work on the demand for prescription drugs has focused on the response of non-elderly populations to increases in fixed dollar copayments. By contrast, the Part D coverage gap is temporary, changing both the spot price of a medication as well as the expected future price given of a drug if the beneficiary reaches the catastrophic threshold. We know far less about the price elasticity of demand of seniors in this context and how they might respond to cycling in and out of coverage over the course of the year. For example, how frequently do seniors switch to lower cost drugs or discontinue use of a medication altogether when reaching the gap? Do gap-induced changes in medication use persist in the next year or do beneficiaries switch to more generous plans? Further, do changes in prescription drug use affect the demand for medical services? Recent evidence suggests that the introduction of Part D led to substantial reductions in Part A&B spending (McWilliams, Zaslavsky et al. 2011). The reduction in medical service use may be even larger if beneficiaries do not cycle into and out of drug coverage.
In this paper, we compare changes in prescription drug use before and after reaching the coverage gap for two distinct groups of beneficiaries: 1) those eligible for the full low-income subsidy (LIS), who face minimal cost-sharing throughout the year and thus are unaffected by the coverage gap; and 2) non-subsidized beneficiaries who pay the full cost of brand name drugs or all medications in the gap. We focus on beneficiaries with diabetes given it is major risk factor for a wide range of other health conditions. If the coverage gap has deleterious effects on health, it should be evident in this sample of beneficiaries.
We find that the coverage gap had a relatively modest effect on medication use, but the demand response was strongly correlated with price. Use of statins ($65), oral hypoglycemics ($50/month), and calcium channel blockers ($46) declined by 4% to 6% in the coverage gap, while use of lower cost medications such as ACE inhibitors/ARBs ($30), beta blockers ($27) and diuretics ($8) declined by just 1% to 3% in the gap.1 This pattern was consistent across other drugs classes not used to treat diabetes. For example, beneficiaries with diabetes reduced their use of high cost, brand-dominant medications such as anti-asthmatics ($127), antipsychotics ($213), and other central nervous system drugs ($150) by 10% to 15% in the coverage gap. By contrast, use of less expensive medications with high generic penetration such as antidepressants ($49) and analgesics ($53) declined by 3% to 5% in the gap. Further, we found no evidence that reductions in medication use in the coverage gap affected medical service use that year or in the next year.
Previous Research
Medicare Part D
The coverage gap changes the price of a drug in more complex ways than a typical increase in a fixed dollar copayment. During the coverage gap, both the spot price and the expected future price of a drug are affected. Once a non-subsidized beneficiary (non-LIS) reaches the coverage gap, each prescription he fills is likely to cost more. Yet at the same time, each fill increases the likelihood of reaching the catastrophic threshold, which lowers the expected price of future prescriptions that year. Moreover, any price change in the gap is temporary since benefits reset at the beginning of the next calendar year. How beneficiaries respond to more complex price changes is unclear.
Most research to date examines how the introduction of Part D affected prescription drug use and beneficiaries out-of-pocket (OOP) expenditures (Lichtenberg and Sun 2007); (Yin, Basu et al. 2008); (Ketcham and Simon 2008); (Levy and Weir 2008); (Joyce, Goldman et al. 2009); (Kaestner and Khan 2012). Most of these studies find that the availability of government subsidized drug coverage is associated with higher pharmaceutical use and lower out-of-pocket spending, with more pronounced effects for low-income beneficiaries. The exception is work by Levy and Weir (Levy and Weir 2008), who find that Part D has only a small effect on medication use based on patient self-reports in the Health and Retirement Study.
Only a few studies have directly examined the impact of the coverage gap. Zhang et al. (Zhang, Donohue et al. 2009) compare Medicare beneficiaries in employer-sponsored drug plans with enrollees in a Medicare Advantage prescription drug (MA-PD) plan, looking at changes in prescription drug use before and after entering the coverage gap. The majority of enrollees in the MA-PD plan have some generic drug coverage while in the gap. They find that in comparison to a group with employer-provided coverage, seniors without gap coverage reduce their monthly use of prescription drugs by 14 percent, whereas those with generic coverage in the gap reduce their use by just 3 percent. The primary limitation of this study is that the sample is restricted to those that remain in the coverage gap through the end of the year. Thus, the highest users of prescription drugs and most price inelastic beneficiaries are excluded from the analysis (i.e. those most likely to reach catastrophic threshold). As a result, their estimates likely overstate the impact of the coverage gap on all beneficiaries.
Polinski et al. (Polinski, Shrank et al. 2011) use data from CVS Caremark to assess rates of medication switching and discontinuation. They compare Part D beneficiaries “exposed” and “unexposed” to the coverage gap, where the latter are defined as those receiving some form of low-income subsidy (partial or full). They find that beneficiaries exposed to the coverage gap have twice the hazard rate of discontinuing a drug, but do not present baseline rates of cessation. Further, they find that beneficiaries exposed to the coverage gap are much less likely to switch medications. This finding is counterintuitive given the potentially large increases in spot prices facing beneficiaries exposed to the gap. The authors suggest that exposed beneficiaries may switch to lower-cost brand or generic versions before they reach the threshold to prevent or delay entering the gap. However, they do not present any evidence to support this hypothesis. Nor is it consistent with beneficiary surveys that show only 40 percent of beneficiaries were aware of a coverage gap in 2006, and those that were, had little understanding of how it worked or whether they were personally at risk of entering the gap (Hsu, Fung et al. 2008).
Hoadley et al. (Hoadley, Summer et al. 2011) use data from IMS Health to measure the fraction of Part D enrollees who reach the coverage gap and how prescription drug use changes during the gap. They compare beneficiaries who do not receive the low-income subsidy (non-LIS) with two control groups; beneficiaries who receive the subsidy (LIS) and commerciallyinsured seniors. They find that nearly one in five non-LIS enrollees (19%) reached the coverage gap in 2009, and one in six of those (3%) reached the catastrophic threshold. Prescription drug use, as measured by the number of scripts, declined by 7% to 8% in the coverage gap, while total drug spending declined by 13% to 16%. The primary limitation of this analysis is that the IMS data do not capture the universe of Part D claims, although their difference-in-differences approach should mitigate the extent of any measurement error.
Cost Offsets
If the gap is prompting beneficiaries to use pharmaceuticals differently—especially if it leads them to discontinue an effective therapy—this could have important health consequences. In fact, cycling into and out of coverage may be more disruptive to care plans than a stable benefit with higher coinsurance. There is limited evidence on the link between cost-sharing for prescription drugs and health. While initial studies find mixed evidence on this issue (Johnson, Goodman et al. 1997); (Motheral and Fairman 2001); (Fairman, Motheral et al. 2003), several recent studies find that that increasing co-payments for drugs increases the use of other medical services. Gaynor et al. (Gaynor, Li et al. 2007) examine the effects of changes in pharmaceutical co-payments by private employers. They find that increasing co-payments leads to a decrease in drug spending, but about one-third (35%) of the savings in drug expenses are offset by increases in medical spending. Moreover, the demand response to higher copayments was stronger in the next year. Chandra et al. (Chandra, Gruber et al. 2007) take a similar approach in examining the price responsiveness of retired public employees in California. They find that moving from a $0 to a $10 co-payment for prescription drugs is associated with a 20% reduction in physician visits. Further, increasing co-payments for physician visits (by an average of $6) reduces use of prescription drugs by 20%. They also find that higher co-payments for outpatient visits and prescription drugs are associated with increases in hospitalization rates, with the largest effects among the sickest patients. Finally, Zhang and colleagues (Zhang, Donohue et al. 2009) examine changes in spending on prescription drugs and other medical services in the two years before and after Part D. They find that enrollment in Part D is associated with increases in prescription drug use and reductions in medical spending for those with no or minimal drug coverage before the implementation of Part D.
Data and Methods
Data & Study Sample
We use a twenty percent sample of Medicare beneficiaries through a re-use agreement with the National Bureau of Economic Research (NBER). This dataset links enrollment and Part A and B claims for traditional fee-for-service Medicare enrollees (1992–2008) to Part D claims from 2006 to 2008. The additional years of Part A and B data improve our measurement of disease incidence/prevalence and risk adjustment. The pharmacy data include all the key elements related to prescription drug events (e.g., drug name; National Drug Code (NDC); dosage; supply; date of service; cost of ingredients; dispensing fees; excluded expenses; and payments made by the beneficiary, plan, and other third-party coverage).
The Part A data include information about inpatient hospital stays, including length of stay, diagnosis-related group (DRG), department-specific charges, and up to ten individual procedure codes and diagnostic codes. Part B information includes claims submitted by physicians and other health providers and facilities for services reimbursed by Part B. Each claim contains diagnostic (ICD-9-CM) and procedure (CPT-4) codes, dates of service, demographic information on beneficiaries, and a physician identification number. Data from outpatient hospital stays, stays at skilled nursing facilities, home hospice care, and durable medical equipment are also included. All of these claims are linked with the beneficiary's vital status. The denominator file contains demographic information about every beneficiary ever entitled to Medicare, including state and county codes, zip code, date of birth, date of death, sex, race, and age.
We identify seniors (age 65+) with diabetes on the basis of at least one inpatient or skilled nursing facility diagnosis, or two or more outpatient diagnoses of diabetes at least five days apart. Once identified, individuals are assumed to have diabetes in subsequent years. We also assume that any enrollee with a Part D claim for insulin has diabetes. We restrict our analysis to individuals enrolled in traditional fee-for-service Medicare and a Part D prescription drug plan (PDP). Individuals are required to have the same Part D contract/plan for the entire year. In 2008, 29.8% of beneficiaries enrolled in the same PDP plan for the whole year had diabetes based on these definitions. The final study sample consists of 609,723 Medicare beneficiaries with diabetes in 2006, 673,646 beneficiaries in 2007, and 714,403 beneficiaries in 2008.
Phases of Coverage
Each pharmacy claim includes the amount of the low-income subsidy; the true out-of-pocket (TrOOP) amount; and a field that indicates in which benefit phase a claim was made: deductible, pre-coverage gap, coverage gap, or catastrophic phase (or straddles two phases). For each individual, the particular coverage phase in their part D plan is clearly defined in the data on the basis of spending levels: Entry into the gap is based on total annual drug spending, whereas exit (and entry into the catastrophic phase) is based on the beneficiary’s TrOOP amount. Thus we can identify the exact date that non-LIS beneficiaries enter and exit the coverage gap, and the dates LIS beneficiaries not subject to the gap reach the same levels of spending associated with entrance and exit from the gap. Most analyses include all beneficiaries, regardless of whether their spending is high enough to reach the catastrophic threshold. While beneficiaries that reach the catastrophic threshold may respond differently to the coverage gap, excluding them is likely to overestimate the true impact of the coverage gap on Medicare beneficiaries.
Beneficiary Groups
The Part D data categorize beneficiaries into four groups: 1) dual-eligibles (individuals who qualify for both Medicare and Medicaid), 2) full low-income subsidy (LIS), 3) partial low-income subsidy (Partial LIS), and 4) non-low-income subsidy (Non-LIS). In general, the dual-eligibles are a particularly vulnerable subgroup of Medicare beneficiaries. They tend to be poor, younger, in worse health, and much more likely than other beneficiaries to have cognitive or mental impairments. For these reasons, we exclude them from our analysis. We also exclude beneficiaries receiving Part D subsidies on a sliding scale (the partial LIS group). Partial subsidies cover 25%, 50%, or 75% of the regional benchmark threshold, depending on the beneficiary’s individual income level, or if he or she is part of a couple, the couple’s combined income. Although the average coinsurance rate for Part D drugs is about 15% for this group as a whole, there is considerable heterogeneity across beneficiaries.
In this paper, we focus on group (2), beneficiaries eligible for the full low-income subsidy (LIS), and group (4), non-LIS beneficiaries. For beneficiaries receiving the full low-income subsidy (group 2), patient cost-sharing is minimal and constant throughout the year. These beneficiaries are not subject to the coverage gap even when their level of drug spending reaches the coverage gap threshold (e.g. $2,400 in 2007). As a result, we do not expect the medication use to change before and after reaching the various (hypothetical) coverage thresholds. We use the LIS as controls and compare their medication use before and after reaching the gap to non-LIS beneficiaries who can face vastly different spot prices over the course of the year and spending distribution. We briefly discuss each group below.
LIS Beneficiaries
To protect low-income seniors from high drug expenses, the federal government pays their monthly premiums and deductibles, as well as almost all of their drug costs throughout the year. In 2010, individuals with incomes less than 150% of the poverty level and modest assets (less than $8,100 for an individual or $12,910 for a couple) qualified for the low-income subsidy. These LIS beneficiaries may choose to enroll in any Part D plan. However, their premiums are covered only up to a “benchmark” amount. This amount is calculated separately for each of 34 PDP regions across the country and is based on the average premium bid for the basic benefit by stand-alone prescription drug plans and Medicare Advantage prescription drug plans. Stand-alone PDPs with monthly premiums below the benchmark amount are called “benchmark plans.” These plans qualify to automatically enroll LIS beneficiaries and receive the full subsidy for their premiums. If LIS beneficiaries enroll in a non-benchmark prescription drug plan, they must pay the amount of the premium above the benchmark. LIS beneficiaries pay modest copayments for each medication included on their insurance plan’s formulary and the full cost of any drugs not on the formulary. In 2010, their copayments were $2.50 for generic drugs and $6.30 for brand-name drugs, up to $6,440 in total spending. After that point, their co-payments dropped to $0. As of 2011, more than 10 million beneficiaries were receiving the low-income subsidy (Kaiser Family Foundation 2011).
Non-LIS Beneficiaries
Although non-LIS beneficiaries enroll in plans with a variety of benefit designs, almost all of them face the coverage gap in some form. Under the government’s standard Part D benefit, non-LIS beneficiaries are responsible for 100% coinsurance payments while in the coverage gap. In 2006, and to a lesser extent 2007, several prominent insurers, including Humana and Sierra Rx, offered gap coverage of brand-name drugs in some plans. But due to adverse selection, these plans suffered large losses and were discontinued after a year. Since then, any coverage in the gap has generally applied to generic drugs only.2 About 26% of stand-alone prescription drug plans currently offer some coverage for the gap—primarily limited to generic drugs (Kaiser Family Foundation 2011). Given the heterogeneity in gap coverage within the non-LIS group, we examined beneficiaries separately, according to whether or not they had some coverage in the gap.
Prescription Drug Use
We compare medication use before and after reaching the gap for LIS and non-LIS groups. We focus on beneficiaries with diabetes because nearly one out of every three Medicare dollars is spent treating the disease or its sequelae. If the coverage gap has deleterious effects on health, it should be evident in this sample of beneficiaries. For each subgroup, we estimate the demand response for diabetes-related and nondiabetes-related drug classes. The set of nine diabetes-related classes include: oral hypoglycemic agents, ACE inhibitors, calcium channel blockers, diuretics, beta blockers, angiotensin II receptor blockers (ARBs), statins, loop diuretics, digitalis glycosides, and a combination of antihypertensives).3 We combine ACE inhibitors and ARBs into a single class because they are commonly considered therapeutically interchangeable. The set of other drugs we analyze consist of the nine most prevalent nondiabetes-related classes used by this set of beneficiaries: antidepressants, antipsychotics, other central nervous system medications, antiasthmatics, platelet aggregation inhibitors, antiulcerants, anticonvulsants, opioid analgesics, and hormones/synthetics/modifers. We estimate changes in prescription drug use before and after reaching the coverage gap, for each therapeutic class. We restrict the sample to brand-dominant classes when examining switching behavior from brand to generic products.
Empirical Approach
We use a before and after design with a comparison group to examine the effect of the coverage gap on medication use. The control group consists of full LIS beneficiaries who are unaffected by the coverage gap (it is simply a hypothetical threshold for these beneficiaries). There are two treatment groups: 1) non-LIS beneficiaries with generic-only coverage in the gap (heretofore “generic-only coverage group”); and 2) non-LIS beneficiaries with no coverage in the gap (heretofore “no coverage group”). A difference-in-differences approach can be incorporated into a regression framework to control for observed differences across groups.
Yijt = β0 + β1 (Coverage Gap)it+ β2 (Generic Only)it + β3 (No Coverage)it + β4 (CG *Generic Only)it + β5 (CG * No Coverage) it + β6 Xit + β7 Zt + νijt
where Yit reflects medication use by person i, in class j, at time (t); Coverage Gap is a binary indicator that equals 1 for prescriptions filled after reaching the coverage gap and 0 before; Xit is a vector of patient characteristics and health conditions; and Z is a vector of month dummies. The two treatment groups are captured by binary indicators for “generic only” and “no coverage” in the gap. The key parameters of interest, β4 and β5, capture differences in medication use before and after reaching the coverage gap for the generic only and no coverage groups, relative to LIS beneficiaries. The key outcome measures are (1) monthly medication use, by class and drug type (brand/generic); and (2) Part A and B utilization, including inpatient admissions, outpatient visits, and emergency departments visits. Other measures include the change in medical service use before and after reaching the coverage gap, as well as change in medical service use in the next year.
We measure changes in medication adherence using the Medication Possession Ratio (MPR), which is the fraction of days that a patient “possess” or has access to medication, as measured by prescription fills. For example, a patient who fills a 30-day script on April 1st and refills the prescription on May 10th would have an MPR of 75%, since they possessed 30 pills over a 40 day span. Due to the nature of claims data, this measure does have some drawbacks; for instance, patients are not observed using the prescription, only filling it. However, using a difference-in-difference approach should mitigate any potential bias due to measurement error. For each drug class, we compute the total days supply of medications before and after reaching the coverage gap to compute the percentage of compliant days for each individual in the sample. We estimate changes in overall medication use (MPR), as well as the generic dispensing rate (GDR), overall and by therapeutic class.
Poor adherence to medications can come about through three different behavioral pathways: reduced initiation of drug therapies, worse adherence among existing users, or more frequent discontinuation of therapy. In this paper, we focus on changes in medication adherence, conditional on use (i.e. we ignore the impact of the coverage gap on the decision to initiate a new therapy). We examine the fraction of beneficiaries that reduce medication use or increase use of generic drugs after reaching the coverage gap. We also measure the fraction of beneficiaries who stop using a class of medication after reaching the gap and the extent to which they restart use in the first 90 days of the next year. We measure discontinuation by comparing medication use within a therapeutic class in the 90 days prior to a beneficiary’s index date (gap date) and after reaching the gap. For example, a beneficiary observed taking an oral hypoglycemic, an antihypertensive, and a statin before reaching the gap, but only an oral hypoglycemic and an antihypertensive after entering the gap (for the remainder of the year) would be categorized as having discontinued one medication within the relevant classes.4 Conditional on stopping, we then measure the fraction of beneficiaries that resume use in the first 90 days after coverage resumes the following year. We also examine the extent to which patients switch plans and move to more generous plans after reaching the gap in the prior year.
Given that 2006 was the initial year of the program and that beneficiaries could enroll up to May 15th (partial year of coverage), we restrict most of our analyses of gap behavior to 2007 and 2008. Nonetheless, we use the 2006 data to categorize beneficiaries and for risk adjustment, as well as in assessing plan switching and enrollment decisions. We examine changes in medical service use by type of service (inpatient, outpatient and emergency department) using the primary ICD-9 diagnosis code. In some analyses, we examine diabetes-related utilization only (e.g., neuropathies, retinopathy, amputation and cardiovascular outcomes) to more precisely target the effects of the coverage gap.
We include binary indicators for the most common comorbid conditions on the basis of the presence of ICD-9 diagnostic codes in the medical claims. These include twenty conditions defined in the Chronic Conditions Warehouse (CCW), as well as hypertension, hyperlipidemia, asthma, gastro-intestinal disorders. The models also include a set of monthly time dummies, a binary indicator for beneficiary type (generic-only and no gap coverage), and plan fixed-effects. We then used the results from these models to predict the monthly use of prescription drugs by LIS and non-LIS beneficiaries overall, and for each of nine therapeutic classes.
Many states have pharmaceutical assistance programs (SPAPs) to help their residents pay for prescription drugs. Some states terminated their SPAPs after the introduction of Part D, while others continued to offer prescription drug subsidies as a supplemental benefit or as “wrap around” coverage to Part D. We include binary indicators for the (14) states that offer some form of supplemental drug coverage to Part D.
Alternative Control Group
Patients fail to adhere to their medications for numerous reasons. The simplest and most common explanation is that they forget. Other important factors for non-adherence include schedule disruptions, side-effects, and out-of-pocket costs. The validity of the difference-in-difference approach assumes that variation in prescription drug use between beneficiary groups (LIS and non-LIS) before and after reaching the coverage gap only reflects price changes. However, it is possible that there are unobserved differences in medication adherence across groups that is changing differentially over time. To test the appropriateness of the LIS as a control group, we re-estimate the models using alternative controls: seniors with employerprovided insurance. These seniors have drug coverage at least as generous as the standard Part D benefit, but are not subject to the coverage thresholds or any other aspect of Part D. As such, they face the same out-of-pocket price over the course of the year and their medication use should not change when drug spending reaches the Part D coverage gap thresholds.
2. Results
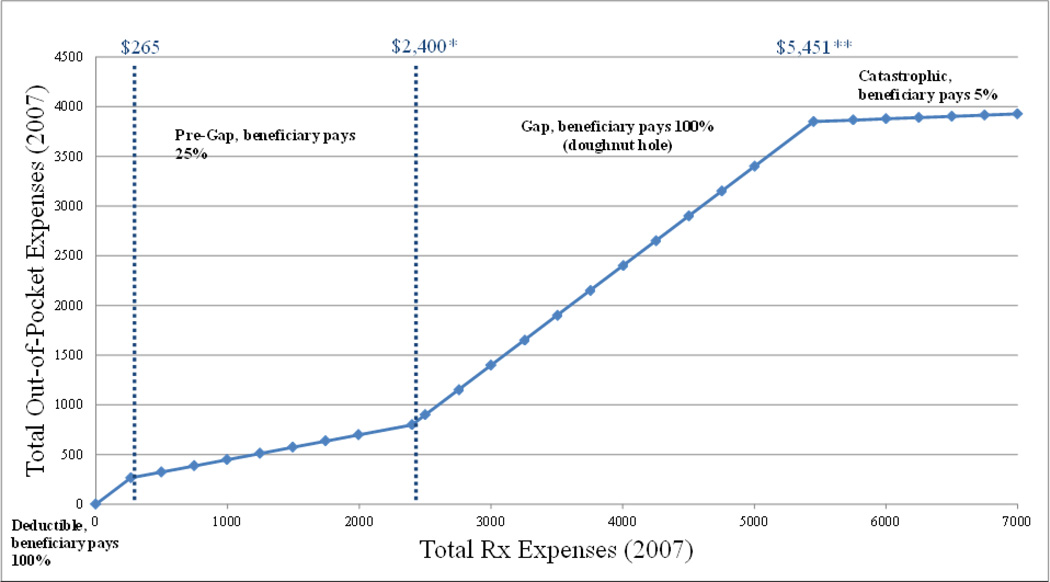
Figure 1 illustrates the non-linear price schedule of the standard Part D benefit. Under the 2007 standard design, beneficiaries not receiving subsidies face a deductible, followed by a 25% co-insurance rate. But once they have spent a cumulative total of $2,400 on prescription drugs in a given year, they must start paying the full cost of their medications. Only after a beneficiary reaches a “catastrophic” limit of $3,850 in out-of-pocket spending (or $5,451 in total drug spending under the standard benefit) does coverage resume, with minimal cost-sharing thereafter. A completely myopic beneficiary would view the spot price in each phase as the true price. By contrast, a future looking individual with moderate to high drug expenses that are likely to exceed the coverage gap (or catastrophic threshold) would be less sensitive to fluctuations in the spot price and less likely to change his use of prescription drugs in response. Thus, prescription drug use and spending of the 41% of non-LIS beneficiaries who reach the coverage gap in 2007 depends on how they take into account the non-linear price schedule they face.
Figure 1.
Standard Part D Benefit Has a Non-linear Price Schedule (2007)
* Entry into coverage gap conditional on reaching a true out-of-pocket expense of $798.75 in 2007
** Entry into catastrophic phase gap conditional on reaching a true out-of-pocket expense of $3,849.75
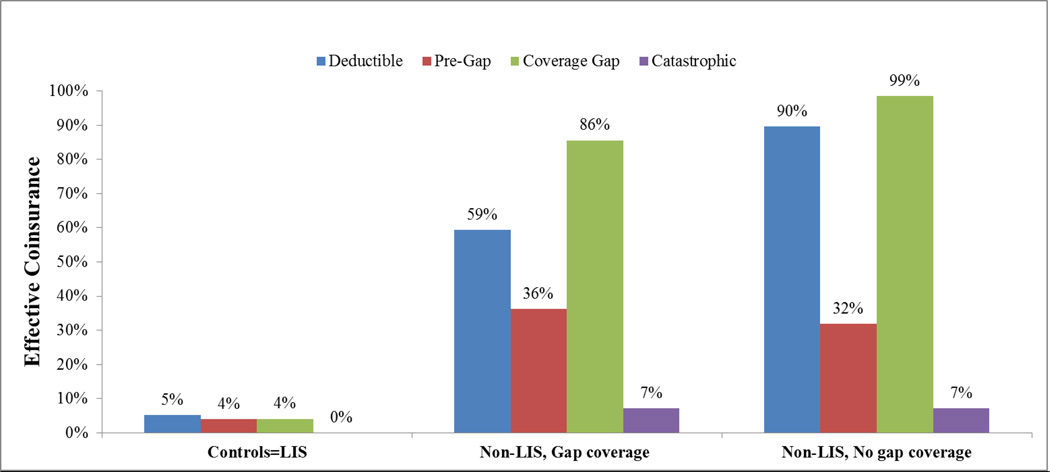
Figure 2 shows the average coinsurance rates faced by different beneficiaries in 2007 across the four phases of the Part D benefit design: deductible, pre-gap, coverage gap, and catastrophic. The figure illustrates the variation we utilize to understand the effects of discrete changes in out-of-pocket costs on beneficiaries use of prescription drugs and medical services. The average coinsurance rate of LIS beneficiaries is below 5% across all phases; in the catastrophic phase, the rate is zero. In contrast, non-LIS beneficiaries with generic gap coverage have an average coinsurance rate of 59% in the deductible phase, 36% in the pre-gap phase, 86% in the coverage gap, and 7% in the catastrophic phase. Non-LIS beneficiaries without gap coverage face the highest coinsurance rates: 90% in the deductible phase, 32% in the pre-gap phase, 99% in the coverage gap and 7% in the catastrophic phase. The reason the coinsurance rate is less than 100% during the deductible phase and in the coverage gap for non-LIS beneficiaries is due to the prerogative of insurance companies to vary the plan design from the government’s standard plan. For example, some Part D plans that provide generic coverage in the gap also cover the cost of generic drugs during the deductible phase. In addition, beneficiaries who are ineligible for the federal government’s low-income subsidy may qualify for state programs that provide coverage for a subset of medications. Such state programs lower coinsurance rates, on average, to 85% in the deductible phase and 89% in the coverage gap.
Figure 2.
Percent of Drug Costs Paid by Beneficiaries, by Coverage Phase
NOTE: Sample is individual with diabetes and ages 65 and older. LIS=Low Income Subsidy. Year: 2007
Table 1 summarizes the characteristics of the LIS and non-LIS beneficiaries, as well as our alternative control group of seniors with employer-provided insurance. On average, LIS and non-LIS beneficiaries are of similar age: 75 years old on average. However, the income and asset requirements to qualify for the full Part D subsidy suggest that these groups are different in other ways. For example, LIS beneficiaries are more likely to be female, non-white, regionally located in the West, and less healthy (as measured by the number of comorbid conditions) than non-LIS beneficiaries and the privately insured. Only 30% of LIS beneficiaries are male and 47% are white compared to 42% and 88%, respectively for non-LIS beneficiaries without gap coverage. The LIS group also tends to be sicker, as measured by the number of comorbid conditions. Low-income beneficiaries with diabetes average 6.6 comorbidities on average, compared to 6.3 and 5.9 for non-LIS beneficiaries with generic and no gap coverage, respectively.
Table 1.
Beneficiary Characteristics, by Coverage Group
| LIS | Non-LIS, Gap coverage |
Non-LIS, No gap coverage |
Employer- provided |
|
|---|---|---|---|---|
| Demographics (%) | ||||
| Age (years) | 74.8 | 74.6 | 75.6 | 75.4 |
| Male | 29.9 | 43.4 | 42.4 | 52.1 |
| White | 46.5 | 91.4 | 87.8 | N/A |
| Black | 19.1 | 4 | 5.8 | N/A |
| Hispanic | 21.6 | 2.6 | 4.2 | N/A |
| By region (%)* | ||||
| Northeast | 20.2 | 14.2 | 21.8 | 23.2 |
| Midwest | 15.3 | 33.8 | 25.7 | 40.5 |
| South | 39.7 | 37.6 | 37.7 | 30.8 |
| West | 24.6 | 14.2 | 13.6 | 5.0 |
| Comorbidities | ||||
| No. of conditions (mean) | 6.6 | 6.3 | 5.9 | N/A |
| Number of observations | 264,716 | 74,503 | 334,427 | 72,456 |
| Part A&B utilization in 2005** (mean) | ||||
| No. of office visits | 8.6 | 9.5 | 8.5 | 8.2 |
| No. of ED visits | 0.7 | 0.5 | 0.4 | 0.6 |
| No. of inpatient stays | 0.4 | 0.4 | 0.3 | 0.3 |
| No. of Inpatient days | 2.4 | 2.2 | 1.7 | 2.1 |
| Part A and B spending in 2005** (mean $) | ||||
| Total | 11,006 | 10,588 | 8,500 | 15,867 |
| Inpatient | 4,000 | 4,080 | 3,127 | 4,982 |
| Outpatient | 4,949 | 5,064 | 4,255 | 8,204 |
| Other | 2,057 | 1,444 | 1,117 | 2,681 |
| Number of observations | 224,832 | 67,895 | 311,949 | 58,677 |
NOTE: Sample is individuals with diabetes and ages 65 and older. Year: 2007; comorbid conditions are any diagnosis years 2002 – 2007
Percentages may not add up to 100 because a small number of cases did not report region.
If covered by FFS Medicare Part A & B in 2005
Table 2 shows the percent of beneficiaries that reach the threshold level of spending for the coverage gap and catastrophic phase in 2007 and 2008. In 2007, LIS (58%) and non-LIS beneficiaries with generic coverage (56%) are much more likely to reach the coverage gap threshold, and reach the gap earlier in the year than non-LIS beneficiaries without coverage (40%). This pattern is repeated in 2008. In both years, LIS beneficiaries are more likely to reach the catastrophic level of spending (21–22%) compared to the non-LIS with generic coverage and no coverage. Complicating these results is the fact that beneficiaries can change categories from year to year. For example, non-LIS beneficiaries that reach the gap in 2007 are more likely to switch to a plan with gap coverage in the next year. As a result, some of the cross-year differences are likely to reflect compositional changes in the beneficiary groups. To control for this, the last two rows of Table 2 condition on remaining in the same beneficiary group over the two year period. These findings suggest that non-LIS beneficiaries without gap coverage (in both years) are more likely to reduce their drug spending in the next year after reaching the coverage gap. For example, 38.8% of the no coverage group reaches the gap in 2007, while just 33.7% do so in 2008. In contrast, a slightly higher fraction of LIS and non-LIS with generic coverage reach the gap in 2008 compared with 2007.
Table 2.
Percent Reaching Coverage Gap and Catastrophic Phase by Group and Year
| LIS | Non-LIS, Gap coverage |
Non-LIS, No gap coverage |
|
|---|---|---|---|
| 2007 | (n=264,716) | (n=74,503) | (n=334,427) |
| Reached coverage gap | 57.6% | 55.8% | 39.7% |
| Median month (entry CG) | 7.4 | 8.0 | 8.7 |
| Reached catastrophic phase | 21.4% | 8.6% | 5.6% |
| 2008 | (n=270,579) | (n=69,650) | (n=374,174) |
| Reached coverage gap | 56.9% | 58.9% | 32.9% |
| Median month (entry CG) | 7.3 | 8.0 | 8.8 |
| Reached catastrophic phase | 21.9% | 8.6% | 5.4% |
| 2007 (conditional on same group) | (n=208,138) | (n=53,298) | (n=284,364) |
| Reached coverage gap | 57.5% | 58.2% | 38.8% |
| Median month (entry CG) | 7.4 | 8.0 | 8.8 |
| Reached catastrophic phase | 20.9% | 9.0% | 5.2% |
| 2008 (conditional on same group) | (n=208,138) | (n=53,298) | (n=284,364) |
| Reached coverage gap | 58.6% | 59.2% | 33.7% |
| Median month (entry CG) | 7.3 | 8.0 | 8.8 |
| Reached catastrophic phase | 22.6% | 8.9% | 5.6% |
NOTE: Sample is individuals with diabetes and ages 65 and older. Conditional on same group sample consists of individuals staying in the same treatment or control group in both 2007 and 2008. Years: 2007, 2008
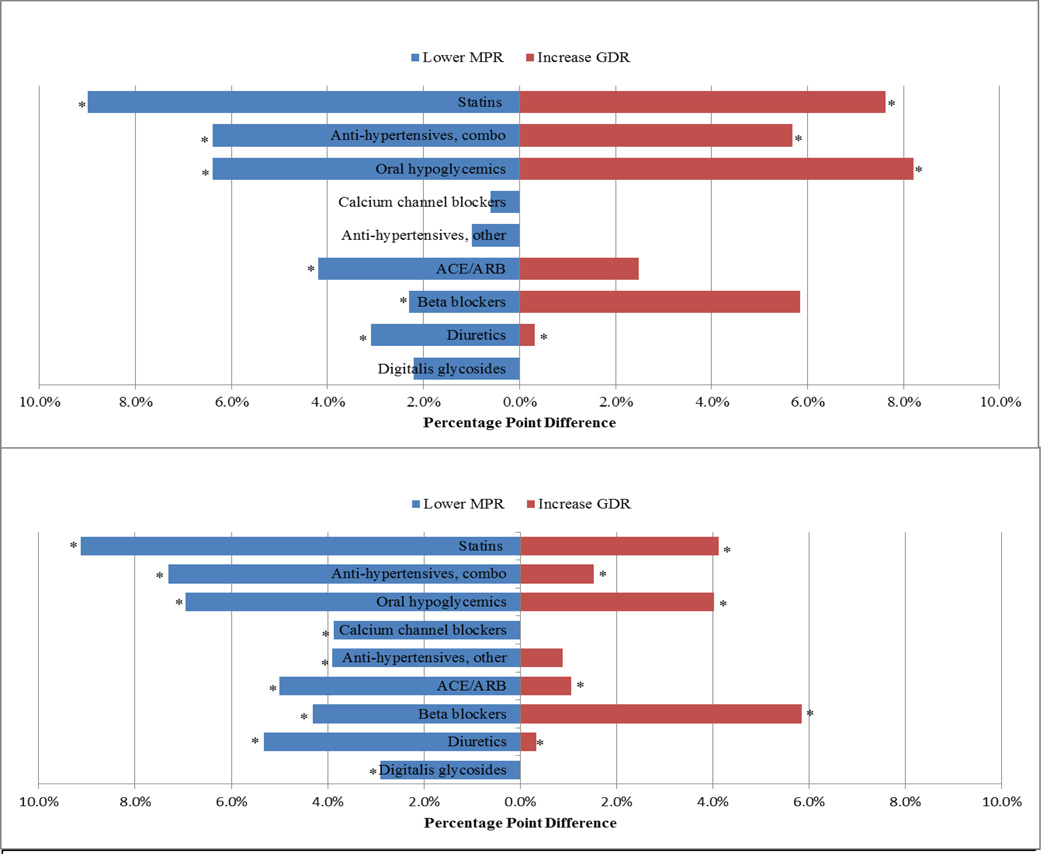
Use of Prescription Drugs
To shed light on specific behavioral responses to the coverage gap, we estimate the fraction of beneficiaries that decrease their medication use or increase their rate of generic use after reaching the coverage gap. We define a decrease in medication use as at least a 2.5 percentage point decrease in MPR after reaching the coverage gap (relative to pre-gap). Similarly, a beneficiary is defined as increasing their generic rate if their GDR increases by 2.5 percentage points or more after reaching the gap (relative to their GDR before the gap). The results shown in Figure 3 reflect unadjusted difference-in-difference estimates at the class-level. The blue bars reflect the additional fraction of non-LIS beneficiaries reducing MPR after reaching the gap (relative to the LIS), and the red bars measure the additional fraction increasing their generic rate after reaching the gap (relative to the LIS). Drug classes are ordered from highest to lowest average price to highlight the correlation between demand response and the average out-of-pocket cost in the coverage gap (see also Appendix Table). We find, for example, that an additional 9 percent of non-LIS beneficiaries reduce their use of statins after reaching the coverage gap (relative to LIS statin-users). However, the demand response is more muted (1%-3%) for lower cost medications such as beta blockers ($27/month), diuretics ($8) and digitalis glycosides ($7). Both non-LIS groups reduce their use of higher cost medications after reaching the coverage gap, but the demand response is larger for those without any coverage in the gap. Depending on the class of medication and the availability of generics, a higher fraction of non-LIS beneficiaries increase their generic rate compared to the LIS (red bars in Figure 3). Further, and not surprisingly, the response is larger for those with generic coverage in the gap.
Figure 3.
A: Behavioral Change to Coverage Gap: Non-LIS, Gap coverage vs. LIS
B: Behavioral Change to Coverage Gap: Non-LIS, No gap coverage vs. LIS
NOTE: Sample is individuals with diabetes and ages 65 and older that reach the coverage gap in 2006 or 2007 Individuals had to stay in coverage gap for at least 40 days. Individuals were considered to lower MPR if they reduced MPR by at least 2.5 percentage points. Individuals were considered to increase GDR if they increased GDR by at least 2.5 percentage points. We dropped insulin from our analysis because it is typically covered under Medicare Part B. * p<.050 relative to LIS group. Years 2006, 2007
Table 3 shows the results of difference-in-difference regressions that model changes in medication adherence (MPR) and generic dispensing (GDR) after reaching the coverage gap,controlling for observed differences in patient demographics, comorbid conditions and Part D plans. Over the 9 diabetes-related classes, average medication use declines in the coverage gap by 2.8 percentage points for non-LIS with generic coverage and by 3.1 percentage points for non-LIS without coverage, relative to the LIS. Moreover, class-level changes are highly correlated with the price of the drug. For example, the use of higher cost medications such as statins ($65/month) falls by 5.0 percentage points in the gap, compared to less than 2 percentage points for beta blockers ($27) and diuretics ($8). In practical terms, these changes translate into statin users taking their medication as prescribed 78% of the time after reaching the gap compared to 83% before the gap. While overall medication use declines, the fraction of drugs dispensed as generic increases in the coverage gap. For example, use of generic statins is 5.4 percentage points higher after reaching the gap for non-LIS beneficiaries with gap coverage and 3.7 percentage points higher for non-LIS beneficiaries without gap coverage, relative to the LIS group.
Table 3.
Adjusted Difference-in-difference in MPR, GDR, and Number of Scripts by Drug Class
| MPR | GDR | |||||||
|---|---|---|---|---|---|---|---|---|
| Number of Observations+ |
Average Price ($) |
Average MPR |
Average GDR |
Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
|
| All Classes | −0.028 *** | −0.031 *** | 0.031 *** | 0.020 *** | ||||
| Statins | 469,450 | 65.47 | 0.826 | 0.319 | −0.050 *** | −0.050 *** | 0.054 *** | 0.037 *** |
| Anti-hypertensives, combo | 143,972 | 58.33 | 0.828 | 0.239 | −0.035 *** | −0.037 *** | 0.043 *** | 0.011 |
| Oral hypoglycemics | 378,372 | 49.73 | 0.866 | 0.652 | −0.035 *** | −0.038 *** | 0.040 *** | 0.022 *** |
| Calcium channel blockers | 227,924 | 45.58 | 0.854 | 0.483 | −0.012 ** | −0.024 *** | −0.020 ** | −0.020 *** |
| Anti-hypertensives, other | 46,784 | 37.37 | 0.759 | 0.869 | −0.019 | −0.026 *** | N/A | N/A |
| ACE/ARB | 360,822 | 30.55 | 0.838 | 0.536 | −0.025 *** | −0.027 *** | 0.020 *** | 0.012 ** |
| Beta blockers | 285,208 | 27.31 | 0.835 | 0.551 | −0.015 *** | −0.022 *** | 0.050 *** | 0.051 *** |
NOTE: Sample is individuals with diabetes and ages 65 and older that reach coverage gap in 2007. Differences are in percentage points. GDR for ACE/ARB class is for ACE Inhibitors only since ARB class is brand-dominated. Results are from regression models. Model includes age, sex, race, and indicators for ending in catastrophic phase, age-squared, co-morbid conditions, and plan type. + Number of observations for MPR calculations. Significance levels are indicated as the following
p<.050
p<.010
P<.001. Average cost is empirically derived, for 30-day equivalent. Year: 2007
Table 4 presents results from similar models, but for the 9 largest classes of nondiabetes-related medications. Similar to the results in Table 3, the demand response to the coverage gap is highly correlated with the price of the drug. Use of antipsychotics ($212/month) fall by nearly 10 percentage points after reaching the coverage gap (relative to the LIS), with similar declines in other high cost classes such as antiasthmatics ($127) and antiaggregants ($123). In contrast, the demand response is markedly smaller for drugs costing less than $100 per month, including antidepressants, analgesics, and anticonvulsants. Rates of generic use increase only slightly across all 9 classes, partly due to baseline rates of generic penetration in these classes. There are relatively few generic products available in some classes (antipsychotics, CNS medications, antiasthmatics) and high generic penetration in others (opioid analgesics, anticonvulsants). The coverage gap is likely to have a smaller impact in classes with either extremely low or extremely high generic penetration.
Table 4.
Adjusted Difference-in-difference in MPR, GDR, and Number of Scripts by Non-diabetic Drug
| MPR | GDR | |||||||
|---|---|---|---|---|---|---|---|---|
| Number of Observations+ |
Average Price ($) |
Average MPR |
Average GDR |
Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
|
| All Classes | −0.058 *** | −0.057 *** | 0.016 *** | 0.005 * | ||||
| Antipsychotics, other | 31,974 | 212.56 | 0.790 | 0.054 | −0.096 *** | −0.076 *** | 0.005 | 0.003 |
| CNS medications, other | 73,346 | 149.54 | 0.762 | 0.019 | −0.062 *** | −0.051 *** | 0.000 | 0.000 |
| Antiasthma, other | 64,588 | 126.87 | 0.617 | 0.002 | −0.111 *** | −0.079 *** | 0.004 *** | 0.003 *** |
| Platelet aggregation inhibitors | 134,966 | 123.08 | 0.828 | 0.164 | −0.086 *** | −0.070 *** | −0.017 *** | −0.026 *** |
| Gastric medications, other | 232,756 | 107.92 | 0.747 | 0.241 | −0.109 *** | −0.102 *** | 0.071 *** | 0.042 *** |
| Hormones/synthetics/modifiers, other | 104,964 | 90.04 | 0.757 | 0.104 | −0.072 *** | −0.061 *** | 0.006 | 0.004 |
| Anticonvulsants | 79,738 | 61.19 | 0.725 | 0.804 | 0.004 | −0.030 *** | 0.009 | 0.002 |
| Opioid analgesics | 201,672 | 53.37 | 0.340 | 0.964 | −0.010 * | −0.020 *** | 0.005 | 0.004 |
| Antidepressants, other | 165,736 | 48.54 | 0.783 | 0.619 | −0.028 *** | −0.038 *** | 0.024 ** | 0.009 |
NOTE: Sample is individuals with diabetes and ages 65 and older that reach coverage gap in 2007. Differences are in percentage points. Drug classes selected by overall cost. Results are from regression models. Model includes age, sex, race, and indicators for ending in catastrophic phase, age-squared, co-morbid conditions, and plan type. + Number of observations for MPR calculations. Significance levels are indicated as the following
p<.050
p<.010
P<.001. Average cost is empirically derived, for 30-day equivalent. Year: 2007
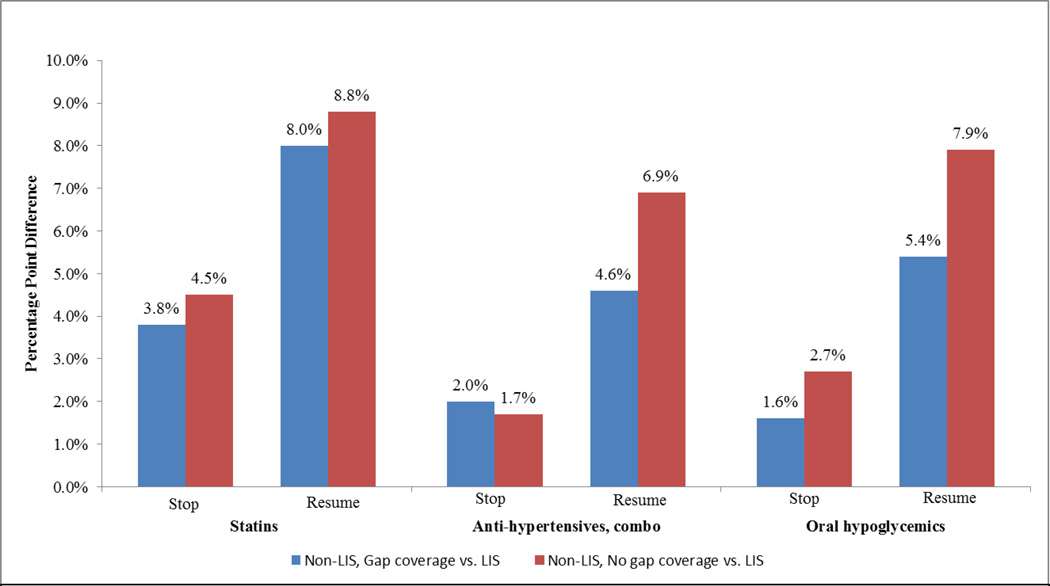
Lower medication adherence may reflect behaviors such as stretching a prescription over more days (e.g. pill-splitting) or stopping a medication altogether. We estimate the fraction of non-LIS beneficiaries that discontinue use of a medication after reaching the coverage gap, as well as the fraction of stoppers who restart use after coverage resumes in the next year, all relative to the LIS. Figure 4 shows the differential rates of starting and stopping for the three most expensive therapeutic classes, where the coverage gap is likely to have its biggest impact (results for all 9 classes are shown in the Appendix). Consistent with prior results, a higher percentage of non-LIS beneficiaries discontinue use of statins, antihypertensives, and oral hypoglycemics after reaching the coverage gap. However, a greater fraction resume use within the first three months of the next year. In the case of statins, about 4 percent more non-LIS than LIS beneficiaries stop taking their cholesterol-lowering medication after reaching the coverage gap, but a greater fraction (8%) resume use once coverage commences in the next year.
Figure 4.
Effect of Coverage Gap on Stopping Therapy and Resuming Therapy
NOTE: Sample for stopping and resumption analyses include beneficiaries age 65 and older with diabetes who reach coverage gap in 2007. Resumption is defined as stopping a drug in the coverage gap in 2007 and resuming in the first quarter of 2008. The therapeutic classes listed above reflect the three most expensive diabetes-related classes. Results for all 9 classes are shown in the appendix. Years: 2007, 2008
Plan Switching
Another potential response to the coverage gap is to switch plans the next year, particularly to a more generous plan with some form of gap coverage. Some degree of plan switching is inevitable, as the set of Part D plans change over time. This is particularly true for the LIS group, who receive full premium support if they enroll in a “benchmark” plan, where the benchmark is determined by the average premium bid for the basic benefit in each region. If LIS beneficiaries enroll in a non-benchmark plan, they are responsible for paying the premium amount above the benchmark threshold. As a result, switching rates are quite high (31%) among the LIS as the set of benchmark plans changes from year to year based on plan bids. Among the non-LIS, 17% of those with gap coverage and 11% without coverage changed plans in 2008. However, among those reaching the coverage gap in 2007, 14.5 and 13.5%, respectively, switched plans the next year (Table 5). Moreover, by doing so, they lowered their out-of-pocket expenses (both premiums and cost-sharing) by an average of $458 (gap coverage) and $153 (no coverage group). Among switchers with generic gap coverage in 2007, the reduction in out-of-pocket expenses was primarily a result of switching to lower premiums plans: 89% of switchers with gap coverage moved to a lower premium plan in 2008. However, among switchers without gap coverage in 2007, 16% moved to a plan with gap coverage in 2008, 24% moved to a lower premium plan, and 26% enrolled in a lower deductible plan.
Table 5.
Switching Plans in Response to Reaching Coverage Gap
| Non-LIS, Gap coverage | Non-LIS, No gap coverage | |
|---|---|---|
| Switch Plans (%) | 14.5 | 13.5 |
| Change in OOP ($) | −457.95 | −152.86 |
| Change in OOP (%) | −16.8 | −7.3 |
| Do Not Swith Plans (%) | 85.5 | 86.5 |
| Change in OOP ($) | −14.09 | −54.67 |
| Change in OOP (%) | −1.0 | −2.0 |
| Plan Change Type (%) | ||
| Added gap coverage | N/A | 16.3 |
| Lowered premium | 89.0 | 24.0 |
| Lowered deductible | 0.0 | 25.9 |
| Other | 11.0 | 33.8 |
NOTE: Sample is individuals with diabetes and ages 65 and older that reach coverage gap in 2007. Changes are from 2007 to 2008. Changes in out-of-pocket expenditures (OOP) include premiums. Years: 2007, 2008
Use of Medical Services
The primary concern of the coverage gap is that reductions in medication use may adversely affect health, which may increase the use of non-pharmacy services. The panels in Table 6 show the results from regression analyses of changes in medical service use before and after the coverage gap, relative to the LIS group. Irrespective of service type (inpatient, outpatient, ED), or condition (cardiac-related or all), we find no difference in medical service us before and after reaching the coverage gap. Nor do we observe increases in Part A&B use in the next year (results available upon request). There are several possible explanations for these results. First, the demand response to the coverage gap is modest for most diabetes-related medications. While a higher fraction of non-LIS beneficiaries stop taking a statin, antihypertensive or oral hypoglycemic after reaching the gap (Figure 4), many reinitiate use onc coverage resumes in the next year, mitigating potential adverse effects. Second, the marginal beneficiary is only subject to the coverage gap for a limited period of time. Beneficiaries that enter the coverage gap early in the year are likely to reach the catastrophic phase, where insurance coverage is nearly complete (5% coinsurance). Thus, unless they are perfectly myopic the demand response should be moderated. On the other hand, fewer than 2% of those entering the gap in the last half of the year reach the catastrophic threshold. While they are more likely to reduce their use of medications, the median beneficiary is only subject to the gap for 3 months. Third, the adverse effects of poor medication adherence may take more time to manifest. We find no differences in medical service use in the current year or the next year among those reaching the gap, but we do not capture longer term effects from cycling in and out of coverage.
Table 6.
| A: Adjusted Medicare Part A and B Utilization, Diabetes-Related Conditions | ||
|---|---|---|
| Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
|
| Emergency Department Visits Per | ||
| Month | 0.0003 | −0.0001 |
| Outpatient Visits Per Month | 0.0005 | −0.0025 |
| Inpatient Stays Per Month | −0.0005 | −0.0017 *** |
| Inpatient Days Per Month | −0.0008 | −0.0076 * |
| B: Adjusted Medicare Part A and B Utilization, All Conditions | ||
|---|---|---|
| Non-LIS, Gap coverage vs. LIS |
Non-LIS, No gap coverage vs. LIS |
|
| Emergency Department Visits Per | ||
| Month | 0.0013 | −0.0003 |
| Outpatient Visits Per Month | 0.0016 | −0.0056 |
| Inpatient Stays Per Month | −0.0014 | −0.0027 ** |
| Inpatient Days Per Month | −0.0164 | −0.0206 ** |
NOTE: Sample (n = 292,200) is individuals with diabetes and ages 65 and older that reach coverage gap after January and before December in 2007. Individuals had to be enrolled and alive 1/1/07-12/31/07. Significance levels are indicated as the following
p<.050
p<.010
P<.001. Year: 2007
As shown in Table 1, the LIS are different from the non-LIS in many ways: they are obviously poorer, more likely to be female, non-white, and sicker on average. Thus, there may be some concern that they differ in unobserved ways that make them an inappropriate control group. Although their constant level of prescription drug use before and after the coverage gap threshold suggests otherwise, we re-estimate the models using seniors with employer-provided insurance as controls. These seniors have drug coverage at least as generous as the standard Part D benefit, and like the LIS, their demand for prescription drugs should be not be affected by the Part D coverage thresholds. The results presented in Table 7 confirm this. Averaging over the 9 diabetes-related classes, the difference-in-difference estimates for changes in MPR and GDR are very similar to those reported in Table 3, using the LIS as controls.
Table 7.
Adjusted Difference-in-difference in MPR, GDR, and Number of Scripts by Drug for Employer-provided Sample
| MPR | GDR | ||||
|---|---|---|---|---|---|
| Number of Observations+ |
Non-LIS, Gap coverage vs. Employer- Provided |
Non-LIS, No gap coverage vs. Employer-provided |
Non-LIS, Gap coverage vs. Employer-provided |
Non-LIS, No gap coverage vs. Employer-provided |
|
| All Classes | −0.031 *** | −0.035 *** | 0.038 *** | 0.028 *** | |
| Statins | 314,212 | −0.048 *** | −0.048 *** | 0.035 *** | 0.018 *** |
| Anti-hypertensives, combo | 88,904 | −0.039 *** | −0.040 *** | 0.043 *** | 0.01 |
| Oral hypoglycemics | 254,462 | −0.033 *** | −0.035 *** | 0.045 *** | 0.027 *** |
| Calcium channel blockers | 140,588 | −0.003 | −0.015 *** | −0.019 * | −0.019 ** |
| Anti-hypertensives, other | 26,514 | −0.006 | −0.013 | N/A | N/A |
| ACE/ARB | 237,134 | −0.057 *** | −0.059 *** | 0.012 | 0.003 |
| Beta blockers | 188,080 | −0.013 ** | −0.019 *** | 0.095 *** | 0.095 *** |
| Diuretics | 127,760 | 0.005 | −0.006 | N/A | N/A |
| Digitalis glycosides | 39,466 | −0.010 | −0.012 | −0.04 ** | −0.04 ** |
NOTE: Sample is individuals with diabetes and ages 65 and older that reach coverage gap in 2007. Differences are in percentage points. GDR for ACE/ARB class is for ACE Inhibitors only since ARB class is brand-dominated. Results are from regression models. Model includes age, sex, race, and indicators for ending in catastrophic phase, age-squared, co-morbid conditions, and plan type. + Number of observations for MPR calculations. Significance levels are indicated as the following
p<.050
p<.010
P<.001. Average cost is empirically derived, for 30-day equivalent. Year: 2007
3. Conclusion
Despite its success, Medicare Part D continues to be widely criticized for the gap in coverage, supported by several recent studies that find the gap is associated with reduced adherence to drug therapies (Zhang, Donohue et al. 2009); (Hoadley, Summer et al. 2011), (Polinski, Shrank et al. 2011). While reductions in prescription drug use are widely assumed to adversely affect health, there is little reliable evidence to support this contention. We find that the coverage gap does, indeed, disrupt the use of prescription drugs among seniors with diabetes. But the declines in usage are modest and concentrated among higher cost, brand-name medications. Demand for high cost medications such as antipsychotics, antiasthmatics, and drugs of the central nervous system decline by 8% to 12% in the coverage gap, while use of lower cost medications with high generic penetration such as beta blockers, ACE inhibitors and antidepressants decline by 3% to 4% after reaching the gap. More importantly, lower adherence to medications is not associated with increases in medical service use. Part D beneficiaries with diabetes display the same patterns of inpatient, outpatient and emergency department use before and after reaching the coverage gap, as well as the next year, both in absolute levels and relative to the LIS.
These findings do not imply that offering an insurance benefit with a gap in coverage reflects sound public policy. Cycling in and out of coverage may be more disruptive to care plans than a stable benefit with higher coinsurance. However, our results suggest that behavioral responses to the coverage gap may mitigate potential short-term health effects. After reaching the coverage gap, non-LIS beneficiaries are more likely to use lower cost (generic) medications and to switch to more generous plans the next year. And while the non-LIS are more likely to stop taking a medication after reaching the gap, they are more likely to resume therapy once coverage restarts in January.
Our results may overstate the impact of the coverage gap on prescription drug use if beneficiaries obtain free samples from their providers or pay cash for medications at discount outlets after reaching the gap (Tseng, Brook et al. 2004). An increasing number of retail pharmacies (e.g. Wal-Mart, Target) sell a broad range of generic drugs at $4 per prescription. While there is little empirical data on the extent of this behavior, one study finds that 6% of enrollees purchase prescriptions outside of their plan after reaching the annual benefit limit (Hsu, Price et al. 2006). We observe a substantial and rapidly increasing number of $4 claims in the Part D data, thus the extent of bias from uncaptured claims is likely to be small. Further, since entry into the catastrophic phase is based on accumulating out-of-pocket expenses, beneficiaries have an incentive to purchase all of their medications -- even $4 scripts -- through the Part D program.
Our results capture the effects of the coverage gap across a broad array of drug classes, but for a specific group of beneficiaries with diabetes. Future work should examine demand responses across different beneficiary groups, including minorities and low-income seniors who do not qualify for subsidies. More work is also needed in understanding the extent to which beneficiaries change their prescription drug use in anticipation of the gap and whether these behaviors change over time as beneficiaries gain experience navigating the program. The Part D coverage gap may have long-term consequences on beneficiaries’ health, but at this point they are not evident.
HIGHLIGHTS.
We study Medicare beneficiaries’ drug and medical service use in the Part D coverage gap
Use of high-cost brand name drugs declined modestly in the coverage gap
Beneficiaries switched from brand name drugs to generics in the coverage gap
Lower adherence to medications did not increase use of medical services
Beneficiaries reduced drug expenditures to avoid the coverage gap in subsequent years
Appendix
Appendix Table.
Adjusted Difference-in-Difference in Rates of Stopping Therapy and Resuming Therapy in Response to Coverage Gap
| Statins | Anti- Hypertensive, combo |
Oral Hypoglycemic |
Calcium channel blockers |
Anti- hypertensives, other |
ACE/ARB | Beta Blockers |
Diuretics | Digitalis glycosides |
|
|---|---|---|---|---|---|---|---|---|---|
| Stop | |||||||||
| Non-LIS, Gap coverage vs. LIS | 3.8% | 2.0% | 1.6% | −1.5% | −2.3% | −0.9% | −0.9% | −1.0% | −0.5% |
| Non-LIS, No gap coverage vs. LIS | 4.5% | 1.7% | 2.7% | −0.1% | −0.9% | −0.2% | 0.4% | 0.5% | 0.1% |
| Resume | |||||||||
| Non-LIS, Gap coverage vs. LIS | 8.0% | 4.6% | 5.4% | −0.4% | −3.5% | 5.6% | 4.4% | 1.9% | 1.0% |
| Non-LIS, No gap coverage vs. LIS | 8.8% | 6.9% | 7.9% | 3.7% | −1.5% | 5.8% | 4.9% | 0.7% | 3.7% |
| Number of observations | 245,482 | 76,586 | 195,949 | 122,675 | 27,835 | 207,418 | 153,582 | 117,598 | 29,731 |
NOTE: Sample is individuals with diabetes and ages 65 that reach coverage gap in 2007. Individuals had to stay in coverage gap for at least 40 days. Resumption is defined as stopping a drug in the coverage gap in 2007 and resuming in the first quarter of 2008. Years: 2007, 2008
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Prices reflect the average price paid in the sample for a 30-day supply of medication.
A few plans offered brand coverage in 2008, but for all intents and purposes, coverage of generics only was the norm in 2007–2008. As such, we heretofore refer to the two treatment groups as the: 1) non-LIS with generic gap coverage; and 2) non-LIS without gap coverage.
Insulin is used to identify beneficiaries with diabetes. However, we exclude insulin from demand models because injectable drugs are generally covered under Part B and not Part D.
We restrict our analyses of stopping and resuming to beneficiaries reaching the coverage gap before Nov 15th to allow sufficient time to measure cessation of a therapy.
References
- Chandra A, Gruber J, et al. Patient cost-sharing, hospitalization offsets, and the design of optimal health insurance for the elderly. National Bureau of Economic Research, Inc; 2007. NBER Working Papers: 12972. [Google Scholar]
- Fairman KA, Motheral BR, et al. Retrospective, long-term follow-up study of the effect of a three-tier prescription drug copayment system on pharmaceutical and other medical utilization and costs. Clinical therapeutics. 2003;25(12):3147–3161. doi: 10.1016/s0149-2918(03)90099-3. discussion 3144–3146. [DOI] [PubMed] [Google Scholar]
- Gaynor M, Li J, et al. Substitution, spending offsets, and prescription drug benefit design. Forum for Health Economics & Policy. 2007;10(2) [Google Scholar]
- Hoadley J, Summer L, et al. Understanding the effects of the Medicare Part D coverage gap in 2008 and 2009: Costs and consequences prior to improvements in coverage established by the 2010 Health Reform Law. Program on Medicare Policy. The Kaiser Family Foundation. 2011:1–46. [Google Scholar]
- Hsu J, Fung V, et al. Medicare beneficiaries' knowledge of Part D prescription drug program benefits and responses to drug costs. JAMA. 2008;299(16):1929–1936. doi: 10.1001/jama.299.16.1929. [DOI] [PubMed] [Google Scholar]
- Hsu J, Price M, et al. Unintended consequences of caps on Medicare drug benefits. New England Journal of Medicine. 2006;354(22):2349–2359. doi: 10.1056/NEJMsa054436. [DOI] [PubMed] [Google Scholar]
- Johnson RE, Goodman MJ, et al. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Medical Care. 1997;35(11):1119–1131. doi: 10.1097/00005650-199711000-00004. [DOI] [PubMed] [Google Scholar]
- Joyce GF, Goldman DP, et al. Medicare Part D after 2 years. American Journal of Managed Care. 2009;15(8):536–544. [PMC free article] [PubMed] [Google Scholar]
- Kaestner R, Khan N. Medicare Part D and its effect on the use of prescription drugs and use of other health care services of the elderly. Journal of Policy Analysis and Management. 2012;31(2):253–279. [Google Scholar]
- Kaiser Family Foundation. Fact Sheet. Washington, DC: Kaiser Family Foundation; 2011. The Medicare prescription drug benefit. K. F. Foundation. [Google Scholar]
- Ketcham JD, Simon KI. Medicare Part D's effects on elderly patients' drug costs and utilization. Am J Manag Care. 2008;14(11 Suppl):SP14–SP22. [PubMed] [Google Scholar]
- Levy H, Weir D. The impact of Medicare Part D on drug utilization and out-of-pocket spending: Evidence from the health and retirement study. 2008 [Google Scholar]
- Lichtenberg FR, Sun SX. The impact of Medicare Part D on prescription drug use by the elderly. Health Affairs. 2007;26(6):1735–1744. doi: 10.1377/hlthaff.26.6.1735. [DOI] [PubMed] [Google Scholar]
- McWilliams JM, Zaslavsky AM, et al. Implementation of Medicare Part D and nondrug medical spending for elderly adults with limited prior drug coverage. JAMA. 2011;306(4):402–409. doi: 10.1001/jama.2011.1026. [DOI] [PubMed] [Google Scholar]
- Motheral B, Fairman KA. Effect of a three-tier prescription copay on pharmaceutical and other medical utilization. Medical Care. 2001;39(12):1293–1304. doi: 10.1097/00005650-200112000-00005. [DOI] [PubMed] [Google Scholar]
- Polinski JM, Shrank WH, et al. Changes in drug utilization during a gap in insurance coverage: an examination of the medicare Part D coverage gap. PLoS Med. 2011;8(8):e1001075. doi: 10.1371/journal.pmed.1001075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research K. K. Research. Washington, DC: KRC Research; 2011. Seniors' opinions about Medicare Rx: Sixth year update. [Google Scholar]
- Tseng CW, Brook RH, et al. Cost-lowering strategies used by medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. JAMA. 2004;292(8):952–960. doi: 10.1001/jama.292.8.952. [DOI] [PubMed] [Google Scholar]
- Yin W, Basu A, et al. The effect of the Medicare Part D prescription benefit on drug utilization and expenditures. Annals of Internal Medicine. 2008;148(3):169–177. doi: 10.7326/0003-4819-148-3-200802050-00200. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Donohue JM, et al. The effect of Medicare Part D on drug and medical spending. New England Journal of Medicine. 2009;361(1):52–61. doi: 10.1056/NEJMsa0807998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Donohue JM, et al. The effects of the coverage gap on drug spending: a closer look at Medicare Part D. Health Affairs. 2009;28(2):w317–w325. doi: 10.1377/hlthaff.28.2.w317. [DOI] [PMC free article] [PubMed] [Google Scholar]