Abstract
To improve U.S. pain education and promote inter-institutional and inter-professional collaborations, the NIH Pain Consortium has funded 12 sites to develop Centers of Excellence in Pain Education (CoEPE). Each site was given the tasks of development, evaluation, integration, and promotion of pain management curriculum resources, including case studies that will be shared nationally. Collaborations among schools of medicine, dentistry, nursing, pharmacy, and others were encouraged. The John D. Loeser CoEPE is unique in that it represents extensive regionalization of health science education, in this case in the region covering the states of Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI). This paper describes a blueprint of pain content and teaching methods across the University of Washington’s six health sciences schools and provides recommendations for improvement in pain education at the prelicensure level. The Schools of Dentistry and Physician Assistant provide the highest percentage of total required curriculum hours devoted to pain compared with the Schools of Medicine, Nursing, Pharmacy, and Social Work. The findings confirm paucity of pain content in health sciences curricula, missing International Association for the Study of Pain (IASP) curriculum topics, and limited use of innovative teaching methods such as problem-based and team-based learning.
Indexing: pain education, curriculum, health sciences, prelicensure, teaching methods, WWAMI
Introduction
Over 100 million Americans experience serious acute pain, cancer pain, and chronic, non-cancer pain. Multiple reports indicate that there is room for significant improvements in pain care, and the U.S. Institute of Medicine has called for a “cultural transformation” in how pain is assessed and treated.16 According to the National Institutes of Health (NIH), pain is one of the nation’s most pressing national public health problems and is now considered a “grand challenge.”22 A grand challenge has been described as an important problem that could be solved with a specific scientific or technological innovation that would have a high likelihood of global impact and feasibility.10 The barriers to improvements in pain care have been well documented and include knowledge deficits of health care professionals, yet there persists a paucity of pain content in most prelicensure curricula across the health sciences clinical programs. Education is an essential part of the necessary cultural transformation in pain care; improvements in curriculum are needed for generalists and pain specialists particularly at the undergraduate and prelicensure levels.2,16,18,28,34
More specifically, education in pain medicine has been characterized as inadequate and fragmented, needing improvements in scope, content, and duration.3,5,19,29,33 A survey of 117 U.S. and Canadian medical schools21 found that while most provided some pain content embedded in general courses, many topics recommended in the International Association for the Study of Pain (IASP) core curriculum15 received little to no coverage. In general, Canadian schools provided more extensive pain education than did their U.S. counterparts. Similarly, a study of Finnish undergraduate medical school education reported that conventional topics such as anatomy and physiology were well covered but found a lack of teaching about the concept of multidisciplinary care in pain management and a need for improvement in teaching quality and methods.24 Indeed, many practicing physicians in the United States, including community family practitioners and internists and academic attending physicians for medical residents, report their own training as inadequate to manage chronic pain.6,7,31
Training for pain management has also been found to be inadequate in undergraduate nursing,8 physician assistant,32 pharmacy,12,35 physical and occupational therapy,27 and dentistry1 programs. A survey of undergraduate pain curricula3 in 108 programs in the United Kingdom across dentistry, medicine, midwifery, nursing, occupational therapy, pharmacy, physiotherapy, and veterinary science found that pain education accounted for less than 1% of program hours for some disciplines, and only one school had fully implemented the IASP core curriculum.
In order to improve pain education and promote inter-institutional and inter-professional collaborations, the NIH Pain Consortium awarded funding to 12 sites across the United States to develop Centers of Excellence in Pain Education (CoEPEs). Each CoEPE is given the tasks of development, evaluation, integration, promotion, and distribution of pain management curriculum resources for medical and other health sciences schools. Collaborations among schools of medicine, dentistry, nursing, and/or pharmacy are encouraged, as are inter-institutional collaborations. CoEPEs are encouraged to support inter-professional education, with medical, dental, nursing and/or pharmacy students, for example, being taught within the same classes, where collaboration across disciplines during management of patients’ pain could be one topic of education (e.g., how communication among doctors, nurses, dentists, and pharmacists is important in effective pain treatment). Integrating and sharing case-based scenarios that cover the breadth of pain knowledge serves as the core component of the program.
The purpose of this study was to develop an assessment of pain content and teaching methods across the six health sciences schools at the University of Washington (UW) to discover gaps and opportunities for improvement. The UW represents a unique and extensive regionalization of health sciences education in Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI).30 The WWAMI program connects students across a five-state region, offering great potential for pain management learning and multisite teaching of inter-professional team training using portable, case-based curriculum materials that can further be incorporated into prelicensure programs across the country.
Materials and Methods
Setting
At the UW, courses are executed according to a quarter system. Each quarter represents 10 weeks of instruction. Excluding credits and hours for clinical experience where pain content would be variable and difficult to measure, the total number of available hours of instruction for any topic in each profession is as follows. The School of Dentistry offers a 4-year program encompassing a total of 213 credits. The School of Nursing offers a 2-year course of study encompassing a total of 65 credits. The School of Medicine offers a 4-year prelicensure program encompassing a total of 149 credits. The School of Pharmacy offers a 3-year program encompassing 124 credits. The School of Physician Assistant offers a 2-year program encompassing 85 credits. The School of Social Work offers a 2-year graduate program encompassing a total of 49 credits.
Procedure
An e-mail with a link to a Catalyst WebQ survey was sent to the CoEPE’s contact person at the UW Schools of Dentistry, Nursing, Medicine, Pharmacy, Physician Assistant, and Social Work. The e-mail included an information statement about the study and asked the contact person to complete a survey regarding the school’s curriculum. The survey included nine questions for each required preclinical course, including the school, the course name, which year in the program the course was offered, the total number of hours for all pain content provided in each course, a checklist for pain topics covered, and a checklist for teaching methods including definitions (Table 1). The checklist of pain topics included 15 major topic areas with 62 subtopics. This checklist was modified from a previously established list used by the Johns Hopkins curriculum development team to assess pain education in U.S. and Canadian medical schools.21 The modified checklist was reviewed by pain experts for content and face validity. The following teaching methods were evaluated: case-based learning,26 didactic teaching,4 problem-based learning,9 simulation-based learning,17 team-based learning,23 clinical experiences,20 and other. The survey was administered in August and October 2012. Each contact person completed the individual school’s assessment with input from course directors and instructors. The results were reviewed for face content validity, prompting, in some cases, follow-up by telephone or e-mail to the school’s contact person. The University of Washington Institutional Review Board approved this study.
Table 1.
Checklist of Definitions of Teaching Methods
| Teaching Method | Description |
|---|---|
| Case based learning (CB) | Use of real or simulated stories that include patient problems/symptoms. |
| Students analyze these, and working in small groups, arrive at a solution by applying course concepts and evidence found in the literature. | |
| Didactic (D) | A power point presentation or lecture that may include brief question and answer session. |
| Problem based learning (P) | Focused, experiential learning that is organized around the investigation of clinical problems. Learner groups are presented with a case and set their own learning objectives, often dividing the work, teaching each other, guided. |
| Simulation based learning (S) | Simulations, can be low-tech or high tech, duplicate clinical scenarios and allow learners to engage in activities that approximate realistic situations. |
| Team based learning (T) | Teacher-directed method for incorporating small-group active participation in large-group educational setting. Learners must actively participate in and out of class (preparation and discussion). Shift away from facts to application. |
| Clinical Experiences (CE) | Observation of and practice in inpatient and/or outpatient healthcare. |
| Other (O) |
Data from the WebQ survey were transferred to an Microsoft Excel file and descriptive statistics were performed. To ensure that calculations represented the pain content received by all students, the frequency of pain management teaching was calculated only from required courses and did not include clinical time or elective courses; pain content covered during clinical time or elective courses would vary among students. The percent of time spent covering pain topics was calculated by dividing the pain curriculum hours by the total curriculum hours for each health sciences school.
Results
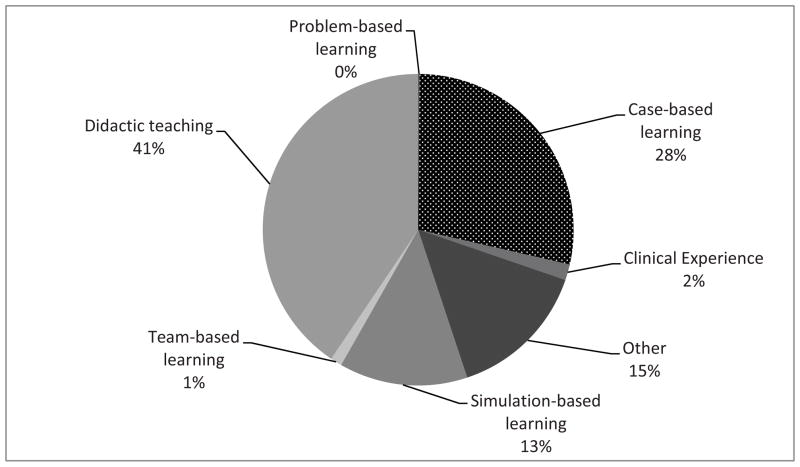
Across six different UW health sciences schools, pain teaching hours ranged from 0 – 145 hours, Social Work, 0 hours; Nursing, 8 hours; Pharmacy, 21 hours; Medicine, 28 hours; Dentistry, 117 hours; Physician Assistant, 145 hours. Figure 1 shows each health sciences school and the percentage of total (required) curriculum dedicated to covering pain topics. Identifiable pain content appears to be largely integrated in pharmacotherapeutics and human behavior courses with little to no pain content provided in ethics, community health, and clinical introduction courses.
Figure 1. Percentage of Total Required Curriculum Hours Dedicated to Covering Pain Topics.
Frequency histogram of pain teaching hours, showing the percentage of the total required curriculum in each UW health sciences school that is dedicated to covering pain topics.
SW = Master of Social Work
BSN = Bachelor of Science in Nursing
DDS = Doctor of Dental Surgery
MD = Doctor of Medicine
PA = Physician Assistant
PharmD = Doctor of Pharmacy
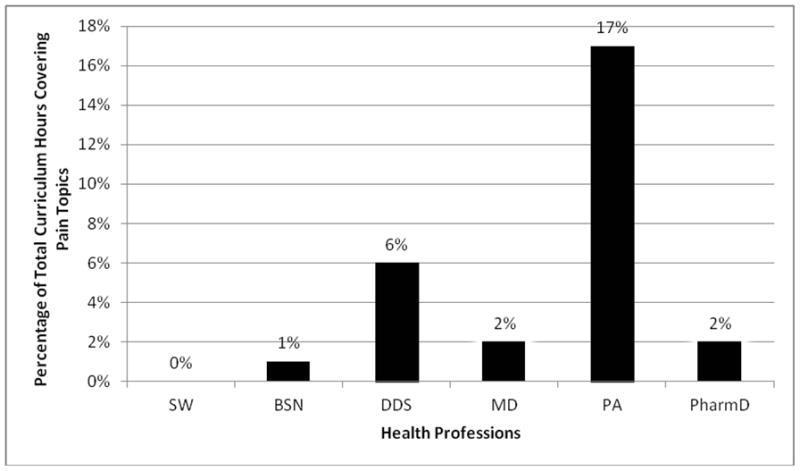
The teaching methods used to deliver pain content varied. Figure 2 demonstrates how the total amount of time spent teaching pain topics (303 hours) was delivered to students across all health sciences schools. Faculty reported that didactic lectures (36%) were the dominant format used to deliver pain management education. Case-based learning (26%) was the second most common format used, and there were no faculty who reported using problem-based learning.
Figure 2. Percentage of Total Required Pain Education Hours by Teaching Method.
Graph of teaching methods used to deliver required pain content at UW health sciences schools, showing the percentage of the total amount of time spent teaching pain topics (total 303 hours) by delivery method.
The 20 pain subtopics most commonly covered by the UW health sciences schools are listed in Table 2. The subtopics are listed in order of decreasing frequency of representation. The pain subtopics most commonly included in curricula included pain-/symptom-focused interviews; principles of analgesia and mechanisms of placebo effects; clinical psychological approaches to care; counseling and shared decision making; conservative pain treatments; and evidence-based CAM; NSAIDs/COX inhibitors; nociceceptive pain; inflammatory pain; rehabilitation for pain problems; neuromodulation; and neuropathic pain.
Table 2.
The 20 Most Frequently Reported Pain Subtopics Across Curriculum of Six Health Sciences Schools
| Subtopic in Pain | # of Courses with Subtopic as a Required Topic |
|---|---|
| Pain/symptom-focused interviews (QRST approach) | 12 |
| Principles of analgesia and mechanisms of placebo effects | 11 |
| Clinical psychological approaches to care | 10 |
| Counseling and shared decision making | 9 |
| Conservative pain treatments and evidenced-based CAM | 9 |
| NSAIDs/COX inhibitors | 9 |
| Nociceptive pain | 8 |
| Inflammatory pain | 8 |
| Rehabilitation for pain problems | 7 |
| Neuromodulation | 7 |
| Neuropathic pain | 7 |
| Pain incidence and causes | 6 |
| Pain, disability, and pain economics | 6 |
| Opioids | 6 |
| Headache | 6 |
| Pain emergencies | 6 |
| Interpretation of pain and disease | 6 |
| Orofacial pain | 6 |
| Musculoskeletal pain and arthritis | 6 |
| Other | 6 |
Discussion
This study of curriculum in a large, regional health sciences program showed wide variation in the amount and focus of pain education in the current curriculum, with the physician assistant curriculum most likely to cover pain management topics. The relatively high proportion of pain education material in the PA curriculum was related to recent PA student requests to increase instruction in pain related topics and integration of material into a strong behavioral science curriculum making identification of pain specific hours difficult. These findings demonstrate the fragmentation and lack of depth in pain education across multiple health sciences schools.
New approaches to pain education in U.S. health sciences schools need to be developed in response to the increasing evidence of inadequate and insufficient pain education and outcomes. Decisions about curriculum content and structure best follow a structured assessment of current pain curriculum. Prelicensure inter-professional pain education is a critical step to ensuring that health professionals entering practice are competent in patient-centered collaboration.13 Thus it is crucial to evaluate pain management curriculum across the broadest range of health sciences schools. Faculty educators from the UW’s Schools of Dentistry, Nursing, Medicine, Pharmacy, Physician Assistant, and Social Work participated in this CoEPE curriculum blueprint assessment, which aims to strategically direct its pan-institutional pain education quality improvement effort.
In the current era of information overload and high competition for limited curriculum time and resources, the quality and character of pain education, rather than just the quantity of didactic hours of instruction, is increasingly important. This assessment of UW health sciences schools adds new information to the Johns Hopkins report21 about other health sciences programs and teaching methods used to deliver pain content. Based on these findings, increased pain education in the form of problem- and team-based learning is needed. The IASP long ago published curriculum topic outlines for first professional programs (prelicensure/undergraduate/entry-practice level) to facilitate dentistry, medicine, nursing, occupational therapy, pharmacy, physical therapy, psychology, and social work pain education. In 2012, IASP released a first ever inter-professional pain curriculum outline based on four core domains of its previously recommended discipline-specific curriculum: (a) multidimensional nature of pain, (b) pain assessment and measurement, (c) management of pain, and (d) clinical conditions.14 A review of this study’s findings reveals significant gaps across and within schools’ pain content in this regard. For example, there is very limited coverage on the ethics of pain in any of the health sciences schools, although this is suggested in the IASP’s multidimensional nature of pain domain. The pain curriculum across the six health sciences schools provides limited inter-professional learning experiences to students, despite the IASP’s recommendation for such collaboration in the domain of pain assessment and measurement. There is also limited course content on the specialty topics of geriatric, pediatric, acute, visceral, and cancer pain despite IASP recommendations for coverage in the clinical conditions domain.
While the specific time and methods required to effectively deliver the IASP curriculum have yet to be identified, an implementation model that balances core content with small-group work including case studies can be recommended. It is noteworthy that case-based learning was the second most common teaching method, following traditional didactic lectures. CoEPE cases are being designed to fill gaps in topic coverage including integration of case studies in didactic courses as well as interprofessional team simulation labs.
There are many frameworks that could be used to categorize pain content. We chose one previously used by the Johns Hopkins curriculum development team to assess North American Medical Schools for comparison.21 However, this may be inadequate to address other health sciences programs and disciplines. The Johns Hopkins report relies on use of a centralized repository of curricular information (CurrMIT), whereas our data came from voluntary personal surveys of key personnel in each school, and may be incomplete. Another limitation to the current study is that data was collected at a single university.
In this study, no evaluation data were collected regarding the impact of the current curriculum on the practice of graduates. Although outcomes are not yet known regarding the optimal scope, content, and duration of pain education, it is evident that considerable deficits remain. One area that appears to need improvement is content that is focused on team-based, inter-professional, problem-based learning to facilitate competent professionals who can work together effectively in teams in real-world, complex, clinical situations and environments. Future studies are planned to evaluate outcomes so that recommendations about the optimal amount and type of pain content can be made.
As educators, clinicians, and researchers move forward to improve the pain content in health sciences schools, it is important to first ascertain what the content and teaching strategies are within an institution, so a plan for improvements in content and teaching strategies can be made. Current trends in health sciences education10,25 suggest that relying too heavily upon the didactic lecture format is not a good way to facilitate either retention of materials or development of problem-solving skills.
Incorporating significant changes in pain education, including use of new CoEPE case materials, requires ongoing collaboration among a university’s inter-professional educators, a process now informed by detailed, multidimensional curriculum survey data. Individual educators and curriculum planners and reviewers at the UW and elsewhere can now team together with any or all of the NIH CoEPEs to facilitate and sustain the changes needed to better prepare new generations of health professionals to be competent in pain management.
We believe that a blueprint of existing curricula can serve as a starting point for the changes that must be undertaken if pain management is to improve in our country. The existence of a blueprint permits us to focus on areas of weakness and deliver resources in a targeted fashion. At a future date, data for another blueprint can be collected and contrasted to the blueprint documented in 2012.
Perspective.
Findings confirm paucity of pain education across the health sciences curriculum in a CoEPE that serves a large region in the United States. The data provides a pain curriculum blueprint that can be used to recommend added pain content in health sciences programs across the country.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to report.
Disclosures
Research reported in this publication was supported by the National Institute of Health Pain Consortium, John D. Loeser Center of Excellence in Pain Education, National Cancer Institute, and National Institute of Nursing Research of the National Institutes of Health under award numbers R42CA141875 and R01NR012450. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Aggarwal VR, Joughin A, Zakrzewska JM, Crawford FJ, Tickle M. Dentists’ and specialists’ knowledge of chronic orofacial pain: Results from a continuing professional development survey. Prim Dent Care. 2011;18:41–44. doi: 10.1308/135576111794065838. [DOI] [PubMed] [Google Scholar]
- 2.Benedetti C, Dickerson ED, Nichols LL. Medical education: A barrier to pain therapy and palliative care. J Pain Symptom Manage. 2001;21:360–362. doi: 10.1016/s0885-3924(01)00274-3. [DOI] [PubMed] [Google Scholar]
- 3.Briggs EV, Carr EC, Whittaker MS. Survey of undergraduate pain curricula in healthcare professionals in the United Kingdom. Eur J Pain. 2011;15:789–795. doi: 10.1016/j.ejpain.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Butler JA. Use of teaching methods within the lecture format. Med Teach. 1992;14:11–25. doi: 10.3109/01421599209044010. [DOI] [PubMed] [Google Scholar]
- 5.Corrigan C, Desnick L, Marshall S, Bentov N, Rosenblatt RA. What can we learn from first-year medical students’ perceptions of pain in the primary care setting? Pain Med. 2011;12:1216–1222. doi: 10.1111/j.1526-4637.2011.01150.x. [DOI] [PubMed] [Google Scholar]
- 6.Darer JD, Hwang W, Hoangmai H, Bass EB, Anderson G. More training needed in chronic care: A survey of U.S. physicians. Acad Med. 2004;79:541–548. doi: 10.1097/00001888-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Dobscha SK, Corson K, Flores JA, Tansill EC, Gerrity MS. Veterans affairs primary care clincians’ attitudes toward chronic pain and correlates of opiod prescribing rates. Pain Med. 2008;9:564–571. doi: 10.1111/j.1526-4637.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 8.Ferrell B, Virani R, Grant M, Vallerand A, McCaffery M. Analysis of pain content in nursing textbooks. J Pain Symptom Manage. 2000;19:216–228. doi: 10.1016/s0885-3924(00)00107-x. [DOI] [PubMed] [Google Scholar]
- 9.Fineout-Overholt E, Stilwell SB, Kent B. Teaching EBP through problem-based learning. Worldviews Evid Based Nurs. 2008;5:205–207. doi: 10.1111/j.1741-6787.2008.00142.x. [DOI] [PubMed] [Google Scholar]
- 10.The Gates Foundation. [Accessed February 25, 2013];Grand challenges in global health. Available at: http://www.grandchallenges.org/about/Pages/Overview.aspx.
- 11.Gruppen LD, Mangrulkar RS, Kolars JC. Competency-based education in the health professions: Implications for improving global health. [Accessed February 25, 2013];Lancet. 2010 376(Appendix):1923–1958. Available at: http://www.healthprofessionals21.org/docs/CompBasedEd.pdf. [Google Scholar]
- 12.Herndon CM, Strassels SA, Strickland JM, Kral LA, Craig DS, Nesbit SA, Finely RS, McPherson ML. Consensus recommendations from the strategic planning summit for pain and palliative care pharmacy practice. J Pain Symptom Manage. 2012;43:925–944. doi: 10.1016/j.jpainsymman.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Hunter J, Watt-Watson J, McGillion M, Raman-Wilms L, Cockburn L, Lax L, Stinson J, Cameron A, Dao T, Pennefather P, Schreiber M, Librach L, Kavanagh T, Gordon A, Cullen N, Mock D, Salter M. An interfaculty pain curriculum: Lessons learned from six years experience. Pain. 2008;140:74–86. doi: 10.1016/j.pain.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 14.International Association for the Study of Pain. [Accessed February 25, 2013];IASP interprofessional pain curriculum outline. Available at: http://www.iaspACCEPTEDMANUSCRIPT11pain.org/Content/NavigationMenu/GeneralResourceLinks/Curricula/Interprofessional/default.htm.
- 15.Charlton JE, editor. IASP Core Curriculum for Professional Education in Pain. 3. IASP Press; Seattle: 2005. [Google Scholar]
- 16.Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Institute of Medicine, The National Academies Press; Washington DC: 2011. [PubMed] [Google Scholar]
- 17.James D, Nastasic S, Horne R, Davies G. The design and evaluation of a simulated-patient teaching programme to develop the consultation skills of undergraduate pharmacy students. Pharm World Sci. 2001;23:212–216. doi: 10.1023/a:1014512323758. [DOI] [PubMed] [Google Scholar]
- 18.Leila NM, Pirkko H, Eeva P, Eija K, Reino P. Training medical students to manage a chronic pain patient: Both knowledge and communication skills are needed. Eur J Pain. 2006;10:167–170. doi: 10.1016/j.ejpain.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Lippe PM, Brock C, David J, Crossno R, Gitlow S. The first national pain medicine summit—the final summary report. Pain Med. 2010;11:1447–1468. doi: 10.1111/j.1526-4637.2010.00961.x. [DOI] [PubMed] [Google Scholar]
- 20.Massarweh LJ. Promoting a positive clinical experience. Nurse Educ. 1999;24:44–47. doi: 10.1097/00006223-199905000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Mezei L, Murinson BB the John Hopkins Pain Curriculum Development Team. Pain education in North American medical schools. J Pain. 2011;12:1199–1208. doi: 10.1016/j.jpain.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 22.National Institutes of Health. [Accessed February 25, 2013];Blueprint for neuroscience research. Available at: http://neuroscienceblueprint.nih.gov/chronic_pain.htm.
- 23.Parmelee D, Michaelsen LK, Cook S, Hudes PD. Team-based learning: A practical guide. Med Teach. 2012;34:e275–287. doi: 10.3109/0142159X.2012.651179. [DOI] [PubMed] [Google Scholar]
- 24.Poyhia R, Niemi-Murola N, Kalso E. The outcome of pain-related undergraduate teaching in Finnish medical faculties. Pain. 2005;115:234–237. doi: 10.1016/j.pain.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 25.Prober CG, Heath C. Lecture halls without lectures—a proposal for medical education. N Engl J Med. 2012;366:1657–1659. doi: 10.1056/NEJMp1202451. [DOI] [PubMed] [Google Scholar]
- 26.Rybarczyk BJ, Baines AT, McVey M, Thompson JT, Wilkins H. A case-based approach increases student learning outcomes. Biochem Mol Biol Educ. 2007;35:181–186. doi: 10.1002/bmb.40. [DOI] [PubMed] [Google Scholar]
- 27.Scudds RJ, Schudds RA, Simonds MJ. Pain in the physical therapy (PT) curriculum: A faculty survey. Physiother Theory Pract. 2001;17:239–256. [Google Scholar]
- 28.Sessle BJ. Unrelieved pain: A crisis. Pain Res Manage. 2011;16:416–420. doi: 10.1155/2011/513423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tauben DJ, Loeser JD. Pain education at the University of Washington School of Medicine. J Pain. 2013 doi: 10.1016/j.jpain.2013.01.005. Epub ahead of print. ACCEPTED MANUSCRIPT 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.University of Washington. [Accessed March 25, 2013];WWAMI program. Available at: http://www.uwmedicine.org/education/wwami/pages/default.aspx.
- 31.Upshur CC, Bacigalupe G, Luckmann R. “They don’t want anything to do with you”: Patient views of primary care management of chronic pain. Pain Med. 2010;11:1791–1798. doi: 10.1111/j.1526-4637.2010.00960.x. [DOI] [PubMed] [Google Scholar]
- 32.Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21:652–655. doi: 10.1111/j.1525-1497.2006.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vadivelu N, Mitra S, Hines R, Elia M, Rosenquist RW. Acute pain in undergraduate medical education: An unfinished chapter. Pain Pract. 2012;12:663–671. doi: 10.1111/j.1533-2500.2012.00580.x. [DOI] [PubMed] [Google Scholar]
- 34.Watt-Watson J, Hunter J, Pennefather P, Librach L, Raman-Wilms L, Schreiber M, Lax L, Stinson J, Dao T, Gordon A, Mock D, Salter M. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain. 2004;110:140–148. doi: 10.1016/j.pain.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Wenthur CJ, Cross BS, Vernon VP, Shelly JL, Harth BN, Lienhoop AD, Madison RN, Murawski MM. Opinions and experiences of Indiana pharmacists and student pharmacists: The need for addiction and substance abuse education in the United States. Res Social Adm Pharm. 2013;9(1):90–100. doi: 10.1016/j.sapharm.2012.03.003. [DOI] [PubMed] [Google Scholar]