Abstract
Gastrointestinal mucormycosis is an uncommon, life-threatening, angioinvasive infection with only one previous report of disease involving the jejunum. We present a case of invasive jejunal mucormycosis and review the literature, highlighting the rare clinical presentation and the value of molecular diagnostic methods. Given the global increase in patient populations at risk of mucormycosis, clinicians need to maintain a high index of suspicion and perform timely and appropriate evaluation to improve patient outcome.
Keywords: Gastrointestinal, Jejunum, Mucormycosis, Rhizopus
1. Introduction
Fungi of the subphylum Mucoromycotina, order Mucorales cause mucormycosis—a rare, often fatal, angioinvasive infection, primarily of immunocompromised hosts [1]. Rhizopus species are the predominant human pathogens, commonly inhabiting soil, animal feces and decaying vegetative matter [2,3]. While any organ system may be affected, rhino-orbital-cerebral and pulmonary infections dominate the literature [2,4].
Gastrointestinal mucormycosis is the most uncommon clinical presentation being particularly rare in industrialized nations. In previous series, gastrointestinal disease has accounted for 4%–7% of all cases [2,4] with only one previous report of disease involving the jejunum [5]. Nonetheless, the incidence of gastrointestinal mucormycosis appears to be on the rise, highlighted by an increase in the number of cases indexed on PubMed—50 publications between 2000 and 2011 compared with eight between 1959 and 1989 [6].
We present a case of invasive intestinal mucormycosis in an adult male and review the literature, highlighting the rare clinical presentation and the value of molecular diagnostic methods in the management of invasive fungal infection.
2. Case
The patient, a 59 year old man who lives in rural South Australia, was retrieved to a metropolitan tertiary hospital for investigation and management of an acute abdomen in November 2011 (day 0). This occurred on the background of a past medical history significant for alcohol misuse, chronic lumbar back pain (requiring opioid analgesia) and irritable bowel syndrome. He reported longstanding alternating bowel habit and abdominal bloating with previously unremarkable upper gastrointestinal endoscopy and colonoscopy.
Importantly, 12 days prior to admission (day-12), the patient was diagnosed with Salmonella enteritis after developing acute diarrhea. Stool microscopy and culture confirmed growth of S. typhimurium.
On this occasion, the patient presented with an acute abdomen complicated by septic shock and multiorgan dysfunction. Clinical examination demonstrated peritonism with diffuse abdominal tenderness, rebound tenderness and guarding. Inflammatory markers were elevated (absolute neutrophil count 14.5×109/L [N 1.8–7.5]; C-reactive protein 150 mg/L [N<8.0]). Emergency laparotomy (day 0) revealed generalized peritonitis and small bowel obstruction in the right iliac fossa secondary to acute adhesions. The proximal small bowel was reported to be “dilated and fragile” leading to perforation as it was manipulated. A 5 cm segment of macroscopically ischemic jejunum was resected.
Histological examination of the resected jejunum revealed marked edema with inflammatory cells infiltrating the wall, but not involving the serosa. Micro-abscesses and granulomata were noted predominantly in the submucosa. Diastase treated sections stained with Periodic-acid-Schiff demonstrated focally-branching, thin-walled, infrequently septate hyphae with occasional bulbous dilatations typical of the order Mucorales (Fig. 1). On the serosal surface, there was purulent inflammation. Within the pus, using the same stain, there were small, regular hyphae consistent with Candida species (Fig. 2). These elements invaded the outer serosa, but were not present in the other layers of the jejunum or the lumen. There were no fissures, caseous necrosis or vascular lesions to suggest any other etiology of the jejunitis.
Fig. 1.
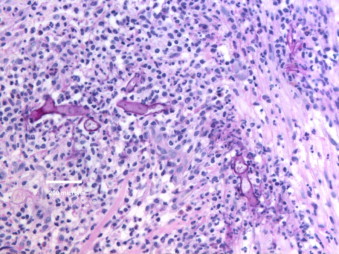
Fungal elements consistent with Mucorales in the wall of the jejunum. Diastase-periodic acid-Schiff stain.
Fig. 2.
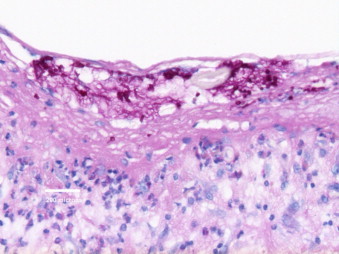
Fungal elements consistent with Candida sp. in purulent exudate on the serosa of the jejunum. Diastase-periodic acid-Schiff stain.
Unfortunately, the surgical specimen arrived in formalin and so was unsuitable for culture. A formalin-fixed, paraffin-embedded (FFPE) tissue block was sent to the mycology laboratory at the Centre for Infectious Diseases and Microbiology (Westmead Hospital, Westmead NSW) (day +2) for pan-fungal polymerase chain reaction (PCR) and internal transcribed spacer 1 (ITS1) sequencing (with the method described in Ref. [7]). Two fungi were amplified, purified and sequenced individually with identification of Candida albicans and a Rhizopus species (BLASTN sequence analysis, BioManager, ANGIS). Sequencing could not differentiate between R. oryzae and R. sexualis given their identical ITS1 sequences. Final results were available on day +25.
In the interim (day +11), the patient deteriorated with development of abdominal pain, hemodynamic instability and clinical signs of peritonism. A 2nd laparotomy revealed ileal perforation with a collection tracking from an ileal loop in the right iliac fossa to the anterior abdominal wall. “Fragile”, “edematous” small bowel was again noted. A 30 cm segment of ileum was resected with creation of a functioning end-ileostomy and venting ileostomy. Histological examination of the resected ileum did not identify invasive fungal elements. Culture of the ileal tissue demonstrated growth of multi-resistant Pseudomonas aeruginosa (sensitive only to colistin). Fungal culture was negative at 4 weeks.
After the initial laparotomy and receipt of histological findings, antifungal therapy was commenced with voriconazole (day +1). In the setting of clinical deterioration, this was substituted for intravenous liposomal amphotericin B (LAmB) 5 mg/kg daily (day +11). The patient tolerated 5 weeks of LAmB before developing acute kidney injury. Salvage therapy was commenced with oral posaconazole 200 mg four times per day (day +49). Given concerns regarding absorption, therapeutic drug monitoring was undertaken. The patient achieved appropriate posaconazole levels of 1.8–1.9 mg/L.
The patient was assessed for clinical risk factors associated with mucormycosis. Malnutrition related to alcohol misuse and recent S. typhimurium enteritis were the only risk factors identified. Although he brewed his own beer, he was unable to quantify his daily intake. No corticosteroid or immunosuppressive therapy had been administered. Investigations for occult malignancy, diabetes mellitus and human immunodeficiency virus were negative. There was no evidence of iron overload.
At day +224, the patient remains on posaconazole. Antifungal therapy will continue for a minimum of 12 months. There is no evidence of relapse or recurrence with resolution of abdominal symptoms, normal stomal output and normal inflammatory markers.
3. Discussion
Gastrointestinal mucormycosis is an uncommon, life-threatening infection with only one previous report of disease involving the jejunum [5]. In the largest series to date by Roden et al., 66 cases (66/929 [7%]) were gastrointestinal; there was frequent dissemination to non-contiguous organs (25/66 [38%]); and mortality was high (56/66 [85%]) related to bowel perforation and upper gastrointestinal hemorrhage [2]. A recent retrospective review by Lanternier et al. of 101 cases (60 proven, 41 probable) of mucormycosis in France between 2005 and 2007 revealed four gastrointestinal and one hepatic infection [4]. Gastrointestinal infection may be more common in the pediatric population with the only large series by Zaoutis et al. documenting 157 cases of mucormycosis with 21% involving the gastrointestinal system; mortality was 100% [8]. All parts of the alimentary tract may be affected. In a series of 87 cases, the stomach (50 cases) and colon (28 cases) were the most frequently involved sites; duodenal (two cases) and jejunal (one case) infection were very rare [5]. To the best of our knowledge, this is the second case of jejunal infection in the literature.
The diagnosis of gastrointestinal mucormycosis is often delayed because of the non-specific presentation; abdominal pain, distention and vomiting are the most common presenting symptoms [3]. Infection may present with an abdominal mass (appendiceal, cecal or ileal) mistakenly thought to be an intra-abdominal abscess [3]. Individual patient populations present with specific disease phenotypes; premature neonates develop necrotizing enterocolitis while neutropenic hosts may present with masses, febrile neutropenia, typhlitis or hematochezia [3]. Gastrointestinal mucormycosis can also involve the liver, spleen and pancreas. The pathologic hallmark of mucormycosis is infarction of host tissue resulting from angioinvasion by hyphae. This gives rise to necrotic ulcers with resultant acute abdominal pain, hematemesis, perforation and peritonitis. Given the rapid progression, prognosis is poor. Only 25% of cases are diagnosed antemortem [3].
Gastrointestinal mucormycosis is acquired by ingestion of pathogens in foods such as fermented milk, dried bread products and fermented porridge [3]. Alcoholic drinks derived from corn may promote gastric mucormycosis [3]. R. oryzae has been used in the production of alcohol in Asia and Africa. Use of spore-contaminated herbal and homeopathic remedies has been implicated. Oliver et al. reported a case of Mucor indicus hepatic mucormycosis in a bone marrow transplant recipient following ingestion of naturopathic therapy, with M. indicus identified by PCR in both the liver abscess and naturopathic compound [9]. Nosocomial transmission is a concern. Maravi-Poma et al. reported a case series of gastrointestinal mucormycosis transmitted by sporangiospore contaminated wooden tongue depressors [10]. Consumption of “home-brewed” beer was the probable source in our patient. Unfortunately, neither the alcohol nor the equipment used for brewing was available for confirmatory testing and concerns remain for re-infection.
There is a clear relationship between specific clinical risk factors and site of infection. For example, rhino-orbital-cerebral infection is associated with uncontrolled diabetes mellitus (specifically ketoacidosis), while pulmonary infection is associated with neutropenia, hematological malignancy and transplantation (hematopoetic stem cell [HSCT] and solid organ [SOT]); both are associated with corticosteroid use [3]. Historically, gastrointestinal mucormycosis has been described in premature neonates and malnourished children with diarrhea [2]. After 1990, infection was documented in diverse populations including patients with traditional risk factors for mucormycosis (hematological malignancy, transplantation [SOT and HSCT], diabetes mellitus, corticosteroid therapy) and patients with pre-existing peptic ulceration [6]. Cases of gastrointestinal mucormycosis with concurrent typhoid fever and gastroenteritis have been documented in children [11]. In our case, malnutrition related to alcohol misuse and impaired mucosal integrity following S. typhimurium enteritis appear to have facilitated hyphal invasion and placed the patient at risk of invasive intestinal mucormycosis.
An important observation in gastrointestinal mucormycosis is its frequent occurrence in a host without classical risk factors [2]. The underlying immunologic defects that are responsible for predisposing different populations to mucormycosis are not well understood. While it is clear that individuals who lack phagocytes or have impaired phagocytic function are at higher risk, there is no definitive explanation for why most people have innate immunity to these fungi.
The successful management of mucormycosis requires 1. early diagnosis, 2. reversal of predisposing risk factors (where possible), 3. surgical debridement and 4. prompt antifungal therapy [12]. There are no recommendations specific to gastrointestinal infection.
Initiation of polyene therapy within 5 days of diagnosis of mucormycosis has been associated with improved survival (82.9% versus 48.9% survival at 12 weeks [13]) highlighting the need for clinical suspicion and early diagnosis. While diagnosis relies upon identification of organisms in tissue by histopathology, confirmation is difficult given frequent absence of growth on culture. Other diagnostic modalities are necessary.
Development of molecular methods based on PCR appears promising and was employed successfully in our case. The ITS1 and ITS2 regions (400–600 base pairs) are variable between most fungal species and are useful targets for species identification [14]. In our case, a FFPE tissue block was the only specimen available. Nucleic acids are heavily modified and damaged in FFPE tissue with the extracted DNA often damaged and fragmented. However, the product remains suitable for short PCR amplifications and as such, PCR and sequencing was performed of the ITS1 region only with the caveat that this provides lower species resolution than ITS1–5.8S-ITS2 sequencing. Despite this, we achieved a clinically meaningful result.
Other molecular techniques are in development. For example, Kasai et al. have developed two real-time quantitative PCR assays targeting the 28S rRNA gene for diagnosis of mucormycosis caused by Rhizopus, Mucor and Cunninghamella species [15]. While these assays have performed well in rabbits with experimental pulmonary and disseminated mucormycosis, there is no data regarding gastrointestinal infection.
Thrombosis and necrosis result in poor tissue penetration and delivery of antifungal therapy to the infected site. Debridement of necrotic tissue appears to be critical for complete eradication. In a multivariate logistic regression model, surgery as a component of primary therapy reduced mortality [2]. Given the mortality attributable to gastrointestinal mucormycosis, aggressive surgical intervention is paramount. Timely resection of infected tissue was critical in our patient.
Primary antifungal therapy for mucormycosis should be based on a polyene in most cases [11]. LAmB is the preferred agent given favorable toxicity profile, superior central nervous system (CNS) penetration and greater efficacy in murine models and retrospective human studies as compared with conventional amphotericin B (AmB) [16]. The optimal dosages for treatment of mucormycosis are not known, but starting dosages of 5–7.5 mg/kg/day for LAmB and amphotericin B lipid complex (ABLC) are commonly used. Whether higher doses (i.e., LAmB 10 mg/kg/day) provide any additional benefit (particularly in CNS infection) is uncertain [11].
The role of combination therapy as primary treatment is unclear with no evidence available for gastrointestinal mucormycosis. While general recommendations cannot be issued given lack of data, the most promising strategy appears to be the combination of an echinocandin and lipid-formulation amphotericin B (LFAB). Synergy has been demonstrated in murine models [16]. Evidence in humans is limited to retrospective data for management of rhino-orbital-cerebral disease in patients with diabetes mellitus [17]. Prospective phase III clinical trials are required.
Salvage therapy may be required for refractory disease or for those intolerant of polyenes. Options include posaconazole, adjunctive treatment (recombinant cytokines [G-CSF, GM-CSF, IFN-gamma], granulocyte transfusion) or combination therapy. Adjunctive administration of the iron chelator, deferasirox, was postulated to be of benefit given the role of free iron in the pathogenesis of mucormycosis and success with combination therapy in diabetic mice. Unfortunately, the Phase II Deferasirox-AmBisome Therapy for Mucormycosis (DEFEAT Mucor) trial failed to demonstrate benefit in a randomized cohort of 20 patients with proven or probable mucormycosis [18]. Excess mortality was witnessed in the deferasirox arm (mortality 90 days—82% deferasirox, 22% placebo [p=0.01]) [18]. However, subjects in the deferasirox arm were more likely to have active malignancy, neutropenia or receive corticosteroids. While general application of these results is difficult, adjunctive deferasirox does not appear to be acceptable.
Most of the literature on salvage therapy focuses on posaconazole. A retrospective series documented 60%–70% “success” rates for salvage therapy with single agent posaconazole with the primary end-point reported as a composite of complete and partial response [19]. However, there are concerns regarding the use of posaconazole monotherapy. R. oryzae, the commonest pathogen isolated, may exhibit in-vitro resistance [20]. In mouse models, posaconazole was less effective than polyene monotherapy [20]. Similarly, there was no additional benefit of combination therapy (posaconazole and LFAB) as compared with LFAB monotherapy [20]. In the context of gastrointestinal mucormycosis, posaconazole administration and absorption may be problematic, specifically in the peri-operative period, with therapeutic drug monitoring crucial.
No comparative data exists to guide duration of therapy. Expert opinion recommends that antifungal therapy should be continued until resolution of symptoms and signs, resolution or stabilization of radiographic abnormalities on serial imaging and resolution of underlying immunosuppression [11]. For patients with mucormycosis who are receiving immunosuppressive therapy, secondary antifungal prophylaxis may be continued. In our case, posaconazole will be continued for 12 months, at which time the patients' clinical state will be reassessed.
Given the global increase in patient populations at risk (the epidemic of obesity and type 2 diabetes mellitus, the surge in use of corticosteroid therapy and the ever-expanding population undergoing SOT and HSCT), there is a significant need for improved diagnosis and treatment of mucormycosis. New laboratory diagnostic methods, including molecular and antigenic tools, are required to improve early detection. New antifungal agents and combinations of existing agents should be explored. A promising new agent, isavuconazole, has in-vitro activity against the Mucorales and, importantly in gastrointestinal mucormycosis, an intravenous formulation is in development [16]. Above all, clinicians need to maintain a high index of suspicion and perform timely and appropriate diagnostic evaluation to improve patient outcome.
Conflict of interest
None.
Acknowledgments
The authors would like to acknowledge Dr. Cea-Cea Moller (MBBS FRACS, Royal Adelaide Hospital), Dr. Catriona Halliday (PhD, Centre for Infectious Diseases and Microbiology, Westmead Hospital), Prof. David Ellis (PhD, SA Pathology, Women's and Children's Hospital) and Dr. Ian Parkinson (PhD, IMVS).
References
- 1.Kwon-Chung K. Taxonomy of fungi causing mucormycosis and entomophthoramycosis (zygomycosis) and nomenclature of the disease: molecular and mycologic perspectives. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2012;54(S1):S8–S15. doi: 10.1093/cid/cir864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roden M., Zaoutis T., Buchanan W., Knudsen T., Sarkisova T., Schaufele R. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2005;41:634–653. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]
- 3.Petrikkos G., Skiada A., Lortholary O., Roilides E., Walsh T., Kontoyiannias D. Epidemiology and clinical manifestations of mucormycosis. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2012;54(S1):S23–S34. doi: 10.1093/cid/cir866. [DOI] [PubMed] [Google Scholar]
- 4.Lanternier F., Dannaoui E., Morizot G., Elie C., Garcia-Hermoso D., Huerre M. A global analysis of mucormycosis in France: the RetroZygo study (2005–2007) Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2012;54(S1):S35–S43. doi: 10.1093/cid/cir880. [DOI] [PubMed] [Google Scholar]
- 5.Agha F., Horchang L., Boland C.R., Bradley S. Mucormycoma of the colon: early diagnosis and successful management. American Journal of Roentgenology. 1985;145:739–741. doi: 10.2214/ajr.145.4.739. [DOI] [PubMed] [Google Scholar]
- 6.Spellberg B. Gastrointestinal mucormycosis: an evolving disease. Gastroenterology and Hepatology. 2012;8(2):140–142. [PMC free article] [PubMed] [Google Scholar]
- 7.Lau A., Chen S., Sorrell T., Carter D., Malik R., Martin P. Development and clinical application of a panfungal PCR assay to detect and identify fungal DNA in tissue specimens. Journal of Clinical Microbiology. 2007;45(2):380–385. doi: 10.1128/JCM.01862-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaoutis T., Roilides E., Chiou C., Buchanan W., Knudsen T., Sarkisova T. Zygomycosis in children: a systematic review and analysis of reported cases. The Pediatric Infectious Disease Journal. 2007;26(8):723–727. doi: 10.1097/INF.0b013e318062115c. [DOI] [PubMed] [Google Scholar]
- 9.Oliver M.R., Van Voorhis W.C., Boeckh M., Mattson D., Bowden R. Hepatic mucormycosis in a bone marrow transplant recipient who ingested naturopathic medicine. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 1996;22:521–524. doi: 10.1093/clinids/22.3.521. [DOI] [PubMed] [Google Scholar]
- 10.Maravi-Poma E., Rodriguez-Tudela J.L., de Jalon J.G. Outbreak of gastric mucormycosis associated with the use of wooden tongue depressors in critically ill patients. Intensive Care Medicine. 2004;30:724–728. doi: 10.1007/s00134-003-2132-1. [DOI] [PubMed] [Google Scholar]
- 11.Prabhu R.M., Patel R. Mucormycosis and entomophthoracmycosis: a review of the clinical manifestations, diagnosis and treatment. Clinical Microbiology and Infection. 2004;10(S1):31–47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 12.Spellberg B., Walsh J., Kontoyiannis D., Edwards J., Ibrahim A. Recent advances in the management of mucormycosis: from bench to bedside. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2009;48:1743–1751. doi: 10.1086/599105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chamilos G., Lewis R.E., Kontoyiannis D.P. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2008;47:503. doi: 10.1086/590004. [DOI] [PubMed] [Google Scholar]
- 14.Dannaoui E. Molecular tools for identification of zygomycetes and the diagnosis of zygomycosis. Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases. 2009;15(S5):66–70. doi: 10.1111/j.1469-0691.2009.02983.x. [DOI] [PubMed] [Google Scholar]
- 15.Kasai M., Harrington S.M., Francesconi A., Petraitis V., Petraitiene R., Beveridge M. Detection of a molecular biomarker for Zygomycetes by quantitative PCR assays of plasma, bronchoalveolar lavage, and lung tissue in a rabbit model of experimental pulmonary zygomycosis. Journal of Clinical Microbiology. 2008;46:3690–3702. doi: 10.1128/JCM.00917-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spellberg B., Ibrahim A., Roilides E., Lewis R., Lortholary O., Petrikkos G. Combination therapy for mucormycosis: why, what, and how? Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2012;54(S1):S73–S78. doi: 10.1093/cid/cir885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed C., Bryant R., Ibrahim A.S. Combination polyene-caspofungin treatment of rhino-orbital-cerebral mucormycosis. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2008;47:364–371. doi: 10.1086/589857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spellberg B., Ibrahim A.S., Chin-Hong P.V., Kontoyiannia D., Morris M., Fredericks D. The Deferasirox-AmBisome therapy for mucormycosis (DEFEAT Mucor) study: a randomized, double-blinded, placebo-controlled trial. The Journal of Antimicrobial Chemotherapy. 2012;67(3):715–722. doi: 10.1093/jac/dkr375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenberg R., Mullane K., Van Burik A. Posaconazole as salvage therapy for zygomycosis. Antimicrobial Agents and Chemotherapy. 2006;50(1):126–133. doi: 10.1128/AAC.50.1.126-133.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim A.S., Gebremariam T., Schwartz J.A., Edwards jr., JE, Spellberg B. Posaconazole mono- or combination therapy for treatment of murine zygomycosis. Antimicrobial Agents and Chemotherapy. 2009;53:772–775. doi: 10.1128/AAC.01124-08. [DOI] [PMC free article] [PubMed] [Google Scholar]


