Abstract
This research utilizes a laboratory experiment to evaluate the effectiveness of alternative public policies targeted at increasing the rate of deceased donor organ donation. The experiment includes treatments across different default choices and organ allocation rules inspired by the donor registration systems applied in different countries. Our results indicate that the opt-out with priority rule system generates the largest increase in organ donation relative to an opt-in only program. However, sizeable gains are achievable using either a priority rule or opt-out program separately, with the opt-out rule generating approximately 80% of the benefits achieved under a priority rule program.
Keywords: Health, Organ Donation, Laboratory Experiment, Government Policy, Public Health
1. Introduction
Between 2000 and 2011 the annual number of deceased organ donors within the United States (U.S.) increased from 5,985 to 8,125 (Scientific Registry of Transplant Recipients (SRTR) 2012). Although this represents a 36% increase in deceased donors, it has not kept pace with the rapidly risen waiting list. During this same time interval the number of patients waiting for an organ transplant has increased from 74,635 to 112,971 patients, a 51% increase (SRTR 2012). Both in absolute and relative terms there is an ever-increasing gap between the number of deceased donor organs and those waiting for a transplant.1 Despite the large need for transplantable organs, only 42.7% of residents in the U.S. over the age of 18 are registered organ donors.2 Clearly, the current organ supply system in the United States fails to produce an adequate supply to satisfy the demand for transplantable organs and there is an increasing need to close this gap and increase human welfare. In this paper we experimentally investigate whether or not changes in the organ donation default choices as well as organ allocation rules can effectively increase organ donation and facilitate the closing of this gap.
The experimental design is inspired by different donor registration and organ allocation systems currently applied in other countries. The U.S. system serves as a baseline for comparison where current donor registration is an opt-in program and the organ allocation system does not assign priority to those who are willing to be donors themselves. We compare this institution to an opt-out donor registration system inspired by the current system in Spain and Austria, an opt-in with a priority allocation rule inspired by Israel and an opt-out with priority rule system inspired by Singapore. Our results indicate that the opt-out system with priority rule generates the largest donation rates, with the largest marginal gains arising from the priority rule allocation system. Our results are consistent with the findings of Kessler and Roth (2012) who found that a priority rule allocation program will increase donation rates, but we complement their finding to encompass the opt-out rule which is currently being utilized in other countries.
Although there are a large number of living donors within the U.S., there is currently 0.8 living donors for each deceased donor, we focus on deceased donation as the number of potential deceased donors is far above the number of current deceased donors and many types of organ transplantation rely exclusively on deceased donation.3 Approaches to increase the organ supply from deceased donation broadly fall into two classes: improving the donation rates of eligible deceased donors and enlarging the pool of potential donors. The donation rates can be improved by increasing the consent rates from the potential donors’ next-of-kin. Since first drafted in 1968, the Uniform Anatomical Gift Act (UAGA) established that an individual’s statement of intent to be an organ donor is legally binding (Bonnie et al., 2008). However, it is still common practice to ask the permission of the deceased’s next-of-kin to donate their organs. Along this vein, the department of Health and Human Service (HHS) passed regulation that requires all hospitals to report all deaths to the Organ Procurement Organization (OPO).4 This regulation increases the opportunity that the deceased’s next-of-kin is contacted for organ donation.
Policymakers have made efforts to increase the donation rate through regulation and improvements to the organ procurement system. In the U.S. an organ procurement organization (OPO) is in charge of the procurement of deceased-donor organs. There are 58 such organizations from different regions throughout the U.S. and each regional OPO obtains direct contact with the deceased’s next-of-kin. In April 2003, HHS launched the Organ Donation Breakthrough Collaborative to improve the donation rate.5 The goal of the collaborative is to encourage the adoption of “best practices” for increasing access to transplantable organs. Recent research suggests that the collaborative has increased organ donation within the U.S. (Howard et al., 2007; Shafer et al., 2008).
Another approach to increase the organ supply is to enlarge the pool of potential donors or generating a higher registration rate among the population. Our experiment is targeted at this mechanism for increasing the organ supply as we measure the relative effectiveness of potential policy changes that target increasing the number of potential donors. Our paper is novel in that we conduct a controlled laboratory experiment to compare policy regimes under different institutions of organ donor registration that currently exist in the world today. Results from the experiment will inform the discussion of possible changes in organ donation public policy by allowing us to determine the relative gains achievable under each policy alternative while controlling for other external factors that may impact donation rates. We consider two highly publicized proposals: changing the default rule for organ donor registration and changing the organ allocation rule.
Changing the default rule affects decision-making. Economists have highlighted the substantial role that defaults play in numerous areas, including health care plans (Samuelson and Zeckhauser, 1988), automobile insurance (Johnson et al., 1993), retirement saving plans (Madrian and Shea, 2001) and consent to online privacy policies (Johnson et al., 2002). Results show that people often choose the default option to which they are assigned, suggesting that changing the default choice of the organ donation question may influence donation decisions. The U.S. operates an opt-in policy regime so that the individual must self-select and register to be an organ donor. In other words, the current default choice in the U.S. is non-donor. One proposed policy alternative is to change the default option to being a donor, what is referred to as an opt-out system. Under an opt-out regime, an individual must self-select out of being an organ donor.
Altering the default choice influences donation decisions through various channels (Johnson and Goldstein, 2003). First, the default may be considered as the recommended action by the policy-maker. For example, if the default is that an individual has consented to be a donor, potential donors might believe being a donor is recommended by policy-makers. Second, accepting the default may involve less effort for the individual making decisions. Psychologically, the organ donation decision may induce stress from thoughts of dying or pain suffered by family members should their organs be donated. Researching the information about organ donation and filling out registration forms also involves time and physical effort. These costs are upfront burdens placed upon organ donor registration and intensified when the default option is non-donor (captured by the opt-in rule within our experiment).
Several European countries like Spain and Austria have adopted an opt-out system for organ donation, while some other European countries like Germany and the United Kingdom have opt-in default options. With data reported in Gäbel (2002), Johnson and Goldstein (2003; 2004) compare donor registration rates across European countries with different default options. They find higher registration rates in countries where the default choice is being a donor (opt-out). One potential problem of this method is the assumption that all other observable characteristics can be controlled for and that the unobservable characteristics, such as network ties to recipients, educational attainment, and income (Healy, 2006), are not correlated with donor registration across countries.6 We provide support for these empirical results using a laboratory setting where outside confounders do not exist.
Changing the organ allocation rule is another potential way to increase the pool of registered donors. The current organ allocation system in U.S. is organized by the United Network for Organ Sharing (UNOS). UNOS maintains a national waiting list. Transplant candidates on the list are ranked, among other things, according to the candidate’s health condition, physical compatibility between the donor and the candidate (i.e., the Human Leukocyte Antigen (HLA) matching),7 their distance from the potential donor, the patient’s preferences for particular donor types (i.e., is the patient willing to accept an Extended Criteria Donor (ECD) organ) and how long the candidate has been on the waiting list. When a transplantable organ becomes available, the opportunity goes to the highest-ranked person on the list. Under the current allocation system utilized by UNOS an individual is not given priority if they have elected to be a potential donor. A proposed change is to utilize a priority rule for allocation.8
A priority rule allocation system gives individuals who are on the organ waiting list and are registered organ donors precedence for transplantable organs. In other words, the priority rule establishes the top criterion for ranking on the waiting list by whether a person is registered as an organ donor or not. Individuals who are registered donors rank higher on the waiting list than those who are not, despite their medical condition or other differences. The supporters of the priority rule believe that the current organ allocation system in the U.S. does not provide enough incentive for organ donation because it relies purely on altruistic motives. The priority rule motivates an individual to donate by connecting the potential of helping others to the potential of helping one’s self. The results from our experiment validate this motivation.
Israel and Singapore are examples of countries that have adopted a priority rule for their national donation system. Israel has been using the priority rule system since 2010 (Lavee et al., 2010).9 However, Israeli citizens need to elect to be included as a registered donor to receive priority over those not willing to be donors. Singapore passed the Human Organ Transplant Act (HOTA) in 1987, which applies the priority rule with an opt-out system.10 In Singapore, citizens are assumed to be organ donors, but any person who objects to HOTA can elect not to be included. If a person objects to donate his organs upon death, he automatically gives up priority for receiving an organ should they need one in the future. Therefore, the policy currently implemented in Singapore combines all the features that may increase organ donation over the current U.S. paradigm.
Our experimental design complements the recent work of Kessler and Roth (2012). Kessler and Roth designed a laboratory experiment to test for changes in the decision to register as a donor using alterations in the allocation rule (i.e., priority rule) and financial incentives (i.e., a rebate and discount). As mentioned earlier, Kessler and Roth illustrate that organ donation rates will increase if one elects to utilize a priority rule for organ allocation. Our research extends this research in two important dimensions. One, we investigate whether or not the results expressed in Kessler and Roth (2012) are a construct of the neutral framing used in their experiment as the terms “organ” and “organ donation” are not used. Secondly, we investigate whether or not the utilization of an opt-out versus an opt-in decision rule combined with a priority rule can yield further increases in organ donation. The later being extremely important as it investigates the marginal effects of other countries policies on the organ donation decision.
Our research can be used to further inform the policy debate surrounding the current organ donation system. We not only compare the alternative policies (opt-out and priority allocation rules) to the current U.S. donation system, but we also test the relative effectiveness of different alternative policies in an effort to decompose their marginal effects. In addition, we further evaluate the combination of the opt-out and priority allocation rule. The opt-out with priority system, as discussed by Breyer and Kliemt (2007) and utilized by Singapore, provides a dual-incentive for donation: avoiding the cost of opting-out and receiving priority on the waiting list. A concern with combining the opt-out and priority allocation system is that the priority rule cannot prevent the free-rider problem if the introduction of the opt-out system has already generated sufficient organ supply (Breyer and Kliemt, 2007). Investigating this using observational data would be infeasible but within our experiment we can investigate whether or not this concern is valid. Our result suggests that the combination of opt-out and priority rule is significantly more effective in increasing registration rates than each of the other separable policies.
An additional advancement we make is that the instructions to subjects in our experiment are stated in terms of “organs.” The framing choice that should be applied in the experimental study of policy evaluation is controversial (Abbink and Hennig-Schmidt, 2006; Cason and Raymond, 2011). The reason we choose descriptive framing here is that we believe the organ donation decision involves significant psychological costs that cannot be captured using abstract terms. To measure the impact of framing on experimentally-observed donation decisions, we included an additional treatment, in which the instructions are stated in abstract terms. By doing this, we are able to discuss the impact on the decision to donate “tokens” or donate “organs.” Our results indicate that descriptive framing increases the rate of donor registration.
In the following section, we present our behavioral hypotheses. In Section Two, we outline the experimental design utilized to investigate our hypotheses on the impact that the opt-out versus opt-in and priority allocation rules have on the organ donation decision. In Section Three we discuss the results from the experiment and in the final section we summarize our findings.
2. Behavioral Hypotheses
We designed an incentivized laboratory experiment to evaluate the relative effectiveness of different organ donation mechanisms. We adopted a two-by-two design illustrated in Table 1 with the dimensions being the opt-in versus opt-out decision rule combined with the presence or absence of the priority allocation rule.
Table 1.
Two-by-Two Experimental Design
| Opt-in | Opt-out | |
|---|---|---|
| Without Priority Rule | Control Treatment | Opt-out Treatment |
| With Priority Rule | Priority Treatment | Opt-out with Priority Treatment |
The Control treatment models the current status quo of the U.S. donation system, where subjects are non-donors by default and no one is granted priority for being a registered donor. The Opt-out treatment is different from the Control treatment only in the default choice of the donation decision. As we discussed, there are costs associated with making an active organ donation decision. In our experiment, we model these costs as a simple monetary cost, which is charged if a subject deviates from the default. Being an organ donor in the Opt-out treatment is less costly than in the Control treatment. This leads to the first hypothesis:
Hypothesis 1: Ceteris paribus, changing the default choice of the donation decision from opt-in to opt-out increases the donor registration rate.
The only difference between the Control treatment and the Priority treatment is the organ allocation rule. In the Priority treatment, subjects who are registered donors receive priority when they need an organ, while non-donors are only able to access available organs when the needs of the registered donors on the waiting list are satisfied. Under the priority rule, donors can jump in front of non-donors on the waiting list. That is, the priority rule increases the probability that donors who need an organ will receive one if they are registered donors. This leads to our second hypothesis:
Hypothesis 2: Ceteris paribus, changing the organ allocation rule by adding donors’ priority increases the donor registration rate.
In addition to comparing each alternative mechanism with the current status quo, we are also interested in the relative effectiveness of changing the default choice and changing the organ allocation rule. More formally, we test the following hypothesis:
Hypothesis 3: Ceteris paribus, changing the current status quo to the opt-out system yields the same level of increase in the donation rate as changing to the priority rule system.
The Opt-out with Priority treatment combines the effect of changing both the default choice (reducing the cost of donor registration) and changing the organ allocation rule (increasing the benefit of donation). It would be expected that the dual-incentives working congruently will be more effective than in the singular case. There is some concern, however, that if the change to an opt-out default choice increases donation registration significantly such that individuals are gaining very little from the priority allocation rule, then the combination of the policies may not result in higher donation rates (Breyer and Kliemt, 2007). In this case, the dual-incentives will not be more effective. We test the following hypothesis on the combination of the opt-out and priority allocation rule:
Hypothesis 4: Ceteris paribus, changing the default choice and the organ allocation rule together generates the same level of increase in the donor registration rate as changing only one of them.
The framing of the decision task may impact the decision to be donor or not within the experiment. An additional advantage of our experiments is the ability to formally investigate the framing effect. We conducted an additional treatment, a neutral framing of the Control treatment (opt-in combined without priority), to investigate the impact that our contextual framing of the decision process had on subject behavior. This generates our final research hypothesis:
Hypothesis 5: Ceteris paribus, subjects behave the same when the experiment is framed in abstract terms as when the experiment is framed in term of organs.
3. Experimental Design
There were 30 rounds in each session of the experiment and a finite number of periods in each round. Subjects were unaware of the number of rounds, but they were informed at the beginning of the experiment that only one round would be randomly selected for payment at the end of the experiment. Each subject was a virtual human in the lab who had one A organ and two B organs.11 In each period, subjects had a 10% probability of an A organ failure and a 20% probability of a B organ failure (both B organs fail together).12 If a subject encountered an A organ failure, she ceased to participate in that round. Whenever a subject’s B organs failed, she was placed on a waiting list to receive one B organ donated by another subject.13 Subjects waiting for a B organ were not subjected to the probability of an A organ failure. Each subject with a B organ failure had up to 5 periods to stay on the waiting list. If they did not receive a B organ within this time period, they ceased to participate in that round.
At the beginning of each round, subjects were asked to make a decision about whether they wanted to register as an organ donor (the opt-in rule) or withdraw from the donor registry (the opt-out rule). Since we only focus on the donor registration decision not the procurement process, we utilized a strong version of donation in our experiment in which registering as a donor implies being a donor upon death in the experiment.
Subjects were told that they would earn $3 in each period that they had one active A organ and at least one active B organ. However, subjects were not able to earn any money when they were on the waiting list or no longer actively participating in the round. All donation decisions were made at the beginning of each round before knowing whether or not they would have an organ failure. All subjects were told that if they chose to be a donor and their A organ failed first each of their B organs would be donated to one of the subjects who were on the waiting list in that period. However, if their B organs failed first, their active A organ could not be donated. In addition, if they received a B organ from others, the donated B organ could not be donated again.
There were costs involved with the donation decision.14 Subjects were told that they had to pay $0.75 to make an active donation decision (override the default choice). This cost can be thought as the psychological and physical costs associate with overriding the default choice, which was charged regardless of the donation outcome. Subjects were also told that the act of donating organs would cost them $2.25. This donation cost can be thought as the psychological costs of organ procurement. Thus, one’s payoff for each round is equal to the earnings in that round minus the costs they incurred for overriding the default decision as well as donating organs. At the end of the experiment, only one round was randomly selected for payment. Subjects were told at the beginning of the experiment that if in the selected round their payoff was negative the extra costs would be charged from their $10 show-up fee.
After making the donation decision at the beginning of each round, subjects observed their outcome for each period, their earnings each period, and their accumulated earnings for that round. After experiencing a B organ failure, the subject began to receive the waiting list information. The waiting list information provide subjects with information on how many periods they had been waiting, their rank on the waiting list and whether they received a B organ in that period. A screenshot of the information screen presented to the subjects is shown in Figure 1. Subjects who ceased to participate in the round were not able to observe any more information until a new round started.
Figure 1.
Illustration of the Decision Screen Used in the Experiment
To investigate our five experimental hypotheses we conducted four organ-framed treatments — the Control treatment, the Opt-out treatment, the Priority treatment and the Opt-out with Priority treatment — and one neutral-framed treatment.15 In the following, we provide more detail on the five different treatments used in the experiment.
In the Control treatment, subjects were not organ donors by default. Those who wished to register as donors were charged $0.75 to change their status. Subjects were told that being an organ donor might potentially affect others’ earnings. The donation decision was described in the experiment as follows:
“In this round, you are not an organ donor by default. If you want to change your status to be a donor, please check the box below; otherwise, please leave it empty.
□ I hereby agree to donate my organs after I cease to participate in this round.”
Subjects were also told that if they chose to be an organ donor, after their A organ failed, their active B organs would be donated to those in need in the order of their rank on the waiting list. The rank on the waiting list was determined by the length of time the subjects had been waiting for a B organ. Subjects who had been waiting longer were ranked higher.16 The rank of subjects who had the same waiting time was randomly determined. For example, if there were two subjects on the waiting list and subject 1 had been waiting for 4 periods and subject 2 had been waiting for 3 periods, subject 1 ranked higher than subject 2.
In the Opt-out treatment, subjects were registered organ donors by default. Those who wished to withdraw their donor registry were charged $0.75 to opt out. The choice of this treatment was described as follows:
“In this round, you are an organ donor by default. If you want to change your status to be a non-donor, please check the box below; otherwise, please leave it empty.
□ I hereby object to donate my organs after I cease to participate in this round.”
Unless a subject responded that he or she did not want to be considered a potential organ donor, their active B organs were donated after an A organ failure occurred. Organs were provided to those in need according to their rank on the waiting list. Subjects on the waiting list were ranked by the length of time they had been waiting on the list, and subjects who had been waiting longer were ranked higher.
The Priority treatment is different from the Control treatment only in the ranking rule used for the waiting list. In this treatment, the default option for the donation decision was not to be an organ donor. Before making the donation decision, all subjects were informed that those who chose to be an organ donor would be given priority ranking on the waiting list. Therefore, subjects on the waiting list in this treatment were ranked on the basis of two criteria: first their donation decision, and second the length of time they had been waiting on the list. For example, if subject 1 is a non-donor who had been waiting for 4 periods and subject 2 is a registered donor who had been waiting for 3 periods, subject 2 ranked higher than subject 1.
The Opt-out with Priority treatment is different from the Control treatment in both the default option and the ranking rule on the waiting list. In this treatment, subjects were registered organ donors by default. Before making the donation decision, all subjects were informed that those who withdraw their donor registration would automatically give up their priority ranking on the waiting list. Transplantable organs would be provided to registered donors before non-donors.
The description of the decision environment to the subjects in the four treatments above was stated in terms of organ donations. We conducted an additional treatment — the Neutral treatment, in which the instructions to subjects were neutrally-framed, to control the effect of the experiment framing.
In the Neutral treatment, we adopted the same default option and ranking rule on the waiting list as the Control treatment. The only difference is that the experiment description was phrased in abstract terms, not in terms of organs. Subjects were informed that they would be assigned three tokens in each round: one A token and two B tokens. In each period, each subject had a 10% probability of losing their A token and a 20% probability of losing both B tokens. Subjects would earn $3 in each period that they had one A token and at least one B token. The donation decision in this treatment was described as follows:
“In this round, you are not a donor by default. If you want to change your status to be a donor, please check the box below; otherwise, please leave it empty.
□ I hereby agree to donate my B tokens after I cease to participate in this round.”
We conducted eighteen experimental sessions with 15 subjects in each session. In twelve sessions, subjects played 15 rounds in one of the organ-framed treatments followed by 15 rounds in another one of the organ-framed treatments (for example, subjects participated in the Control treatment for rounds 1–15 and then the Opt-out treatment for rounds 16–30). In these sessions, subjects were stopped after round 15 and told that they would start a new treatment. Subjects were handed the instructions for the new treatment and the experimenter clearly explained all changes in the rules.
In three of the remaining sessions, subjects played the Control treatment in all 30 rounds, while in the last three treatments subjects played the Neutral treatment in all 30 rounds. In these sessions, subjects were also stopped after round 15. They were told that they would start a new treatment, but there were no changes in the rules of the game. The experimenter again reviewed all the rules of the game. All of the treatment combinations used in the experiment are shown in Table 2. Lastly, the selection of which session to conduct among the eighteen sessions was randomly determined prior to subjects entering the experiment laboratory.
Table 2.
Number of Sessions for Each Treatment Combination
| Treatment Rounds 1–15 | Treatment Rounds 16–30 | ||||
|---|---|---|---|---|---|
|
| |||||
| Control | Opt-out | Priority | Opt-out with Priority | Neutral | |
|
|
|||||
| Control | 3 Sessions | 1 Session | 1 Session | 1 Session | No Sessions |
| Opt-out | 1 Session | No Sessions | 1 Session | 1 Session | No Sessions |
| Priority | 1 Session | 1 Session | No Sessions | 1 Session | No Sessions |
| Opt-out with Priority | 1 Session | 1 Session | 1 Session | No Sessions | No Sessions |
| Neutral | No Sessions | No Sessions | No Sessions | No Sessions | 3 Sessions |
To obtain an expected payoff for subjects participating in the experiment we conducted a series of Monte Carlo simulations under the priority rule and no priority rule scenarios. Simulations were not conducted for changes in the default as the difference in expected earnings between these treatments does not depend on the probabilistic failures of an A or B organ. The override cost is a fixed cost this is incurred before the virtual life begins within the experiment. In the non-priority rule treatment the expected payoffs for donors increased from $16.44 to $19.59 when the rate of donation increased from 0.1 to 0.9, whereas it increased from $18.19 to $21.25 for non-donors. In the priority treatment the expected payment for non-donors increased from $16.80 to $19.80 when donation rates increased from 0.1 to 0.9 and from $18.10 to $19.32 for non-donors. Under both the non-priority and priority rule designs the payoffs for non-donors exceeded that of donors, however the marginal increase is lower under the priority rule. This illustrates the incentive to donate under the priority rule treatment.
At the end of each session, the subjects were presented with a brief questionnaire on their demographic characteristics and their involvement with organ donation in their own lives. They received payment after they completed the questionnaire.
4. Results
The experiment was performed at the Georgia State University Experimental Economics Center (ExCEN). Subjects were recruited from the undergraduate student body using a recruiting program that randomly invites registered subjects to participate in the experiment. A total of 270 subjects participated in the experiment and the average payment was $18.03.17 Table 3 presents the descriptive statistics for the experiment. There are 8100 observations at the subject-round level. The average donor registration rate for all treatments is 41.5%. The average donation rates by treatment were as follows: Opt-out with Priority (70.8%), Priority (61.3%), Opt-out (48.8%), Control (25.3%), and Neutral (17.8%). The descriptive statistics clearly indicate that the highest average donation rates arise when the priority rule is utilized. This finding is consistent with that of Kessler and Roth (2012), but the descriptive statistics also illustrate that substantial gains can be achieved using just an opt-out policy.
Table 3.
Descriptive Statistics for the Experiment
| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Round Profit | 8100 | 9.216 | 9.83 | −3 | 87 |
| Round Cost | 8100 | 0.582 | 0.90 | 0 | 3 |
| Payment | 8100 | 18.033 | 9.28 | 7 | 63.25 |
| Flier | 8100 | 0.211 | 0.41 | 0 | 1 |
| Donation Registration Rate | 8100 | 0.415 | 0.49 | 0 | 1 |
| Control Treatment | |||||
| Donation Registration Rate | 2700 | 0.253 | 0.43 | 0 | 1 |
| Opt-out Treatment | |||||
| Donation Registration Rate | 1350 | 0.488 | 0.50 | 0 | 1 |
| Priority Treatment | |||||
| Donation Registration Rate | 1350 | 0.613 | 0.49 | 0 | 1 |
| Opt-out with Priority Treatment | |||||
| Donation Registration Rate | 1350 | 0.708 | 0.45 | 0 | 1 |
| Neutral Treatment | |||||
| Donation Registration Rate | 1350 | 0.178 | 0.38 | 0 | 1 |
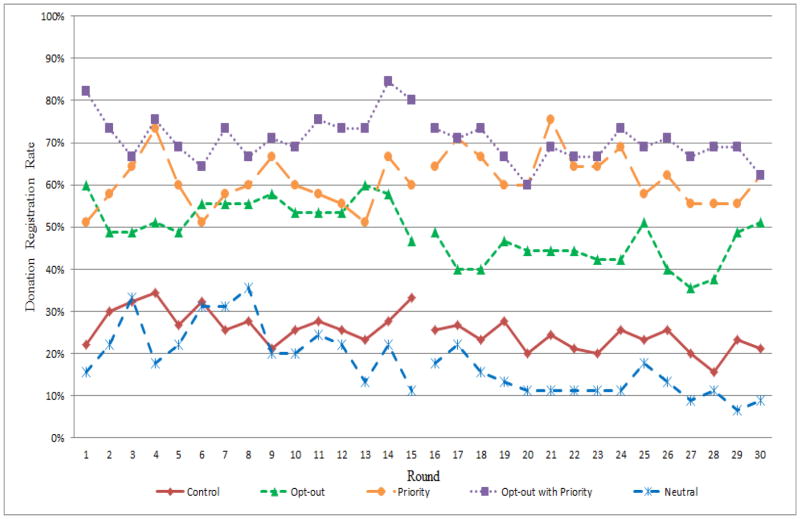
Figure 2 shows the percentage of subjects who were registered organ donors (those who either opted in or did not opt out) in each round of the experiment for each treatment. The line breaks indicate that subjects were stopped after round 15 in each session and then restarted under a new treatment from round 16 through 30. Figure 2 suggests that changing the default option and/or altering the organ allocation rule has a significant positive impact on the donor registration rate across all 30 rounds. The Control treatment lies beneath the three other organ-framed treatments regardless of being played in the first or last 15 rounds. Figure 2 also suggests that the experiment framing plays an important role. The organ-framed treatment generates a higher average donor registration rate than the neutral-framed treatment. This difference in registration rate across treatments is even more notable in the last 15 rounds.
Figure 2.
Percentage of Donors in Each Treatment Reported by Round of the Experiment
To more rigorously investigate the treatment differences a series of probit regressions were estimated to investigate the marginal effect of different mechanisms on organ donation decisions using different levels of experiment and subject control variables and clustering the standard errors at the subject level. The results are illustrated in Table 4.18 The independent variables in the probit regressions include the four treatment dummy variables Opt-out, Priority, Opt-out with Priority, and Neutral corresponding with the different cells of the experimental design (Model 1). The reference group is the donation decision in the Control treatment, which is the opt-in system currently used in the U.S. We further control whether a decision is made in the first 15 rounds or in last 15 rounds of the experiment using a dummy variable interaction term (Model 2). The dummy variable Second Treatment equals to 1 if a treatment is played in the last 15 rounds and it is interacted with the four primary treatment dummies in Model 1. Regression Models 3 and 4 control for the effect of information in the previous round on the current donor registration decision. Earnings Last Round represents earnings from the previous round (Model 3). Received an Organ Last Round is a dummy variable that equals to 1 if the subject received an organ donated by others in the previous round. Benefit of Organ Received Last Round captures the earnings from the previous round after receiving an organ (Model 4). Lastly, regression Model 5 includes demographic control variables Male, White, and Donor in Real Life. The later being a dummy variable indicating that the subject is currently a registered organ donor. The following provides more detailed results from the experiment broken down by our five primary research hypotheses.
Table 4.
Probit Regressions on the Decision to be a Donor or not Within the Experiment
| Probit Estimation | |||||
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Opt-out | 0.249*** (0.046) | 0.269*** (0.061) | 0.258*** (0.063) | 0.247*** (0.063) | 0.252*** (0.062) |
| Priority | 0.365*** (0.040) | 0.323*** (0.052) | 0.322*** (0.054) | 0.312*** (0.054) | 0.315*** (0.053) |
| Opt-out/priority | 0.451*** (0.043) | 0.450*** (0.054) | 0.437*** (0.056) | 0.429*** (0.056) | 0.431*** (0.056) |
| Neutral | −0.098* (0.052) | −0.058 (0.055) | −0.055 (0.056) | −0.055 (0.056) | −0.052 (0.056) |
| Second Treatment | −0.058 (0.038) | −0.062 (0.039) | −0.062 (0.039) | −0.065* (0.039) | |
| Second Treatment* Opt-out | −0.038 (0.083) | −0.030 (0.085) | −0.028 (0.085) | −0.023 (0.085) | |
| Second Treatment* Priority | 0.094 (0.078) | 0.092 (0.079) | 0.090 (0.078) | 0.100 (0.078) | |
| Second Treatment* Opt-out/priority | 0.005 (0.080) | 0.014 (0.080) | 0.009 (0.080) | 0.014 (0.080) | |
| Second Treatment* Neutral | −0.091* (0.054) | −0.093* (0.055) | −0.088 (0.055) | −0.085 (0.054) | |
| Earnings Last Round | 0.003*** (0.001) | 0.002*** (0.001) | 0.001* (0.001) | ||
| Received an Organ Last Round | 0.074*** (0.016) | 0.047** (0.022) | |||
| Benefit of Organ Received Last Round | 0.003* (0.001) | 0.003* (0.002) | |||
| Male | 0.011 (0.036) | ||||
| White | 0.076 (0.054) | ||||
| Donor in Real Life | 0.050 (0.036) | ||||
| Number of Obs. | 8100 | 8100 | 7830 | 7830 | 7801 |
| Pseudo | 0.125 | 0.1297 | 0.1306 | 0.1333 | 0.1385 |
Note: All variables are expressed as marginal values. Clustered errors by individual. Standard errors are in parentheses.
significant at 1 percent level,
significant at the 5 percent level,
significant at the 10 percent level.
Focusing on our first research hypothesis the results for the experiment validate our hypothesis that the opt-out rule generates a higher donor registration rate than the opt-in rule. Figure 2 illustrates that the opt-out rule has a significant positive impact on the donor registration rate in all rounds. Across all rounds, the Opt-out treatment has an average donation rate of 48.8%, which is almost twice the average donation rate of 25.3% in the Control treatment. Over the first 15 rounds, the Opt-out treatment had an average donation rate of 53.8%, while the Control treatment had a much lower average rate of 27.7%. Over rounds 16–30, the Opt-out treatment had a rate of 43.9%, while the Control treatment only had a rate of 22.9%.
The probit regressions in Table 4 also support our first research hypothesis. The positive and highly statistically significant coefficient on the Opt-out dummy variable in regression Model 1 indicates that subjects are about 25% more likely to register as a donor in the Opt-out treatment than in the Control treatment across all 30 rounds. Furthermore, this finding is robust to the additional controls used in the other econometric specifications (Models 2 through 5). This represents an almost 100% increase in the donor registration rate over the 25.3% donor registration rate observed in the Control treatment. This finding suggests that a significant increase in the donation rate can be achieved by just introducing the opt-out rule.19
In order to test our second research hypothesis we compare the Control treatment (the baseline opt-in without priority system) with the Priority treatment as well as the Opt-out treatment with the Opt-out with Priority treatment. A statistically significant and higher donor registration rate for the Priority and Opt-out with Priority treatments, relative to the Control and Opt-out treatments respectively, will support our second research hypothesis. Figure 2 illustrate that the Priority treatment has a higher average donor registration rate than the Control treatment in all rounds. The average donation rate for the Priority treatment is 61.3% over all rounds, 59.6% over the first 15 rounds, and 63.0% over the last 15 rounds. A higher donation rate is also observed in the Opt-out with Priority treatment when compared to the Opt-out treatment. The average donation rate for this treatment was 70.8% over all rounds, 73.2% for the first 15 rounds and 68.4% for last 15 rounds.
The probit results illustrate the treatment differences. The statistically significant and positive coefficient on Priority indicates that the donation rate increases by between 31.5% and 36.5%, depending on the model assumptions. The statistically significant and positive coefficient on Opt-out with Priority indicates that the donation rate increases by between 42.9% and 45.1%, depending on the model assumptions. Both of these coefficients are interpreted relative to the Control treatment so the relative gains observed under the Opt-out with Priority treatment must be purged of the Opt-out effect solely to be comparable to the Control versus Priority treatment. This said, the marginal differences between the Opt-out treatment and the Opt-out with Priority treatment are not as large as the marginal differences between the Control treatment and the Priority treatment. The donor registration rate increased by 45% going from the Opt-out treatment to the Opt-out with Priority treatment whereas it increased by 142% going from the Control treatment to the Priority treatment.
Both of these results are consistent with those observed in Kessler and Roth (2012) as it is clearly evident that changing the allocation rule to a priority rule will increase the donor registration rate.20 This said, these comparisons do raise the question of whether or not just using the Opt-out rule is capable of providing a similar gain as that observed when altering the allocation rule. This is more formally investigated under our third research hypothesis.
Our previous research hypotheses have illustrated that altering either the organ allocation rule, using a priority rule system, or the default choice, going from an Opt-in to an Opt-out program, will increase the organ donor registration rate. The results clearly indicate that the organ donation rate is greater when comparing either the Opt-out treatment or the Priority treatment with the Control (opt-in) treatment. From a public policy perspective it may be of interest whether or not the relative gains are comparable, as both policies require different forms of administrative change that may or may not be more palatable for different administrations and the populous. On average going from the Control treatment to the Opt-out treatment increased the organ donation rate from 25.3% to 48.8% whereas going to the Priority treatment increased it to 61.3%. This provides the first evidence that does not support our third research hypothesis that they generate equivalent marginal gains in the organ donor rate. Our regression results further confirm this observation. Comparing the coefficient on the Opt-out treatment with the Priority treatment illustrates that in all the models estimated the Priority treatment coefficient is statistically significant and greater than the Opt-out treatment coefficient (p<0.01). Therefore, our third research is not supported.
Despite our failure to support our third research hypothesis, it is important to note that changing the default choice, going from an Opt-in to an Opt-out system, is able to generate approximately 80% of the gains achievable when altering the allocation rule. Therefore, although it is not a one-to-one equivalent the gains are significant enough that policy makers may wish to consider changing just the default option versus the allocation rule if changing the default option is a more palatable public policy.
Investigating our third research hypothesis illustrated that sizable gains are achievable by changing either the allocation rule or the default choice, with the allocation rule outperforming the default choice by a small margin. Our fourth research hypothesis investigates whether or not using either of these changes in isolation yields the same result as combining them and utilizing an Opt-out with Priority program. Figure 2 clearly illustrates that Opt-out with Priority treatment outperforms both the Opt-out treatment and the Priority treatment separately, as it generated the highest donation rate of all the treatments. This does not support our fourth research hypothesis, as it is clear that combining both changes exceeds either of them individual. Over all the rounds the average donation rate was 70.8% for the Opt-out with Priority treatment, compared with 48.8% and 61.3% observed under the Opt-out and Priority treatments respectively. This is also true when comparing the results from rounds 1–15 and rounds 16–30. Over the first 15 rounds, the Opt-out with Priority treatment had an average donation rate of 73.2%, while the Opt-out treatment was 53.8% and the Priority treatment was 59.6%. Over the last 15 rounds, the Opt-out with Priority treatment had an average donation rate of 68.4% while the Opt-out treatment was 43.9% and the Priority treatment was 63.0%. The results from the probit regressions in Table 4 are also consistent with this observation. The coefficient on Opt-out with Priority in regression (1) is positive and highly statistically significant, representing that subjects are about 45% more likely to donate in the Opt-out with Priority treatment than in the Control treatment. Using estimates from regression (1), we find that Opt-out with Priority also performs better than either Opt-out (p<0.01) or Priority (p<0.01) treatments separately.21
As mentioned earlier, our experiment is fundamentally different from Kessler and Roth’s (2012) experiment as it investigates the separable and combined effects of changing the allocation rule as well as the default option and it contextualizes the decision environment. Our fifth and final research hypothesis investigates whether or not the abstract and contextual framing generates the same donor registration rates. Our experimental results indicate that the contextual framing leads to a larger donor registration rate than a neutral framing. Evidence of this can be seen in Figure 2, where the neutral framing donation rates are on average lower than those observed in the contextual framing treatment. However, the differences are not as clear over rounds 1–15 as they are over rounds 16–30.
The probit regressions clarify this treatment effect. The significant negative coefficient on Neutral in regression Model 1 indicates that subjects are about 10% less likely to register as a donor in the neutral-framed treatment than in the organ-framed treatment across all 30 rounds. When controlling for other covariates in the experiment, Models 2 through 5, this percentage decreases to around 5%. Therefore, using a neutral framing, as was conducted by Kessler and Roth (2012), will generate a lower rate of donor registration.22
Robustness of Results
Table 4 also reports results from probit regressions with controls for order effects, information from the previous round and demographic controls. Results are qualitatively the same when we add additional controls. Regression (2) includes a control variable Second Treatment and its interactions with the treatment variables. Coefficient on Second Treatment and its interaction terms suggest there is not a restart effect after the break between round 15 and 16.
Regression (3) controls for the effect of earnings in the previous round on donor registration. The significant positive coefficient on Earnings Last Round suggests earnings in the previous round have a positive impact on the donation decision. Although subjects played multiple rounds in the experiment, only one round was randomly selected for payment at the end of each session. Subjects’ donation decisions should not be affected by their previous earnings. However, subjects could get information about others’ donation decision through receiving a B organ when needed in a previous period of the experiment. We further included variables Received an Organ Last round and Benefit of Organ Received Last Round in regression (4). The significant positive coefficient on Received an Organ Last Round shows that subjects are 7% more likely to donate if they received a B organ in the previous round. Since receiving a B organ leads to additional earnings, especially earnings after receiving a B organ in the previous round, this may affect the likelihood of donation. The coefficient on Benefit of Organ Received Last Round is positive and significant at 10% level. This indicates that the longer one remains active after receiving a donated organ (resulting in higher earnings that round), the greater the probability they will be a subsequent donor. Regression (5) controls for demographic information of the subjects. We did not find any behavioral difference across either gender, ethnicity, or real-life organ donation status. Among our selected subjects, males, whites or real-life organ donor are just as likely to donate as their counterparts.
5. Conclusion
A fundamental limitation to the success of transplantation-based medical treatments is the supply of organs. Although there have been sizeable gains in the development of immunosuppressant drugs that have increased the pool of potential candidates for a donated organ, there still exists an ever widening gap between the number of organ donors and the number of patients on the waiting list. Recently, the transplantation community has made sizable gains in the utilization of donated organs (Howard et al., 2007; Shafer et al., 2008), but future changes in public policy may be required to increase the rate of organ donation within the United States in order to save more lives.
In order to inform public policy, a large amount of research is needed to improve the mechanisms and institutions surrounding organ donation. During the most recent Advisory Committee on Organ Transplantation (ACOT)23 meeting the committee discussed the difficulties of conducting donor-based research. “For clinical research, the areas that come up include IRB approval, how protocols get disseminated, getting consent, etc. How can the field move forward given the complexities? The obstacles to research and innovation in brain-dead deceased donors, include scientific, ethnical, logistical, and regulatory obstacles (Gerber 2013).” Laboratory experiments may offer one additional avenue of scientific research in which many of these complexities are relaxed. While not medical in nature, the laboratory experiments may offer an invigorating glimpse at fundamental changes in the current organ allocation policy. These experiments may prove insightful when designing new medical control trials or in formulating public policy.
Drawing from the experiences in other countries, changes in public policy can arise from either changing the allocation rule to provide priority for those who are registered donors or from changing the default choice from a standard opt-in to an opt-out system. Furthermore, as is the case in Singapore, it is possible to combine both changes in the allocation rule and default choice. The results from our experiment provide the first rigorous investigation of changing both the allocation rules and default choice separately as well as jointly.
Our results are consistent with those previously observed in Kessler and Roth (2012), in that changing the allocation rule to a priority rule system yields a sizable increase in the organ donation rate. We further extend this finding to illustrate that the priority rule generates a larger marginal gain than altering the default choice from an opt-in to an opt-out public policy. In addition, we find that combining both an opt-out and priority rule policy will provide the largest gains in the organ donation rate and that gains are substantially different from the individual effect of each public policy change. We further find evidence that the context of the experiment used to investigate the organ donation decision does matter with a contextualized decision environment yielding an increase in organ donation rates of around 5%.
An important public policy finding that our results illustrate is that approximately 80% of the gains observed under a priority allocation rule are achievable by switching from an opt-in to an opt-out public policy. This is extremely important from a public policy perspective as the costs, both pecuniary and psychological, associated these two possible changes may be substantially different. A change in the allocation rule redefines the rules of whom is to receive priority for an organ which post-transplantation may invoke concepts of fairness and equality as enforcement of this rule may still rely on the deceased donors next-of-kin being amenable to their deceased’s donation preferences. On the other hand, an opt-out policy redefines the rule of who owns a deceased’s individuals organs from the next-of-kin to the government. The choice of which option is more appropriate is subject to the policy maker’s discretion and the constituents that they represent.
Highlights.
We design a laboratory experiment to measure the relative effectiveness of potential policy changes that target increasing donor registration.
We focus on two policy proposals: the opt-out system and the priority rule.
Both the opt-out system and the priority rule have a positive impact on donor registration.
The priority rule outperforms the opt-out system, while the opt-out system generates approximately 80% of the gain achieved under the priority rule.
The combination of the opt-out system and the priority rule generates the highest registration rate.
Acknowledgments
Author wishes to acknowledge funding support provided by NSF (BCS-0908679) and NIH (NIA-1RC4AG039071-01).
Appendix A: Experimental Parameters
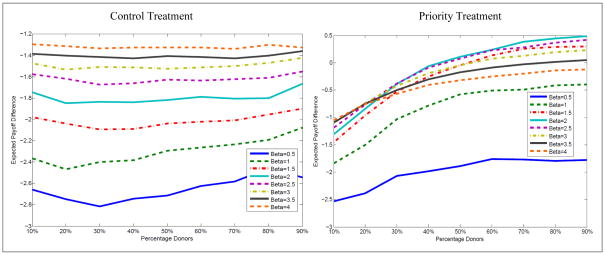
Given the complexity of the decision environment we elected to simulate the decision environment to inform our parameterization of the experiment. The most critical parameter in our experiment is the probability of organ failure. There are two types of organ failure in our experiment. Subjects with an A organ failure potentially provide transplantable organs for subjects with a B organ failure. The ratio of the probability of B organ failure to the probability of A organ failure should be high enough to keep the scarcity of transplantable organs high, but it also cannot be too high because it will cancel out the incentive to donate in the Priority treatment. Figure A.1 shows the expected payoff difference between donors and non-donors for different parameter values in both the Control treatment and the Priority treatment (based on 100,000 simulations of donation rate from 0% to 100% for each set of parameters). The parameter values vary the ratio of the probability of B organ failure to the probability of A organ failure (Beta in Figure A.1).
Figure A.1.
Simulations payoff difference between being a donor and a non-donor for both the Control treatment (left panel) and Priority the treatment (right panel) while varying the percentage of donors (x-axis) as well as the ratio of the A organ failure to B organ failure (Beta).
In Figure A.1, the teal blue line represents the expected payoff difference with the parameters actually used in the experiment (Beta=2), consistent with those used by Kessler and Roth (2012). In the Control treatment, being a donor is more costly that being a non-donor, which would predict no donation in the game. Non-zero donation in the Control treatment would be the expression of altruistic motivation. In the Priority treatment, the payoff difference is increasing with the donation rate. It is worth noting that once Beta exceeds two the payoff difference start to fall off again and the benefits of being a donor are reduced. The reason for these results is an increase in Beta generates an overwhelming gap between organ demand and supply. Due to the high odds of having a B organ failure and the insufficient organ supply, the probability of dying while waiting for a B organ increases even for donors who have priority on the waiting list. The incentive to donate provided by priority rule is canceled out, since having priority on the waiting list does not generate benefit any more.
Appendix B: Experimental Instructions for the Control Treatment
INSTRUCTIONS (Treatment IN)
Now that the experiment has begun, we ask that you do not talk. If you have a question after you finish reading the instructions, please raise your hand and the experimenter will approach you and answer your question in private. In today’s experiment, you are going to make decisions about hypothetical organ donation. None of the choices you make in the experiment today will affect your real life.
Show-up Fee
You have already earned U.S. $10 for arriving to the experiment on time.
Experiment
There are multiple rounds in the experiment today. In each round, you are assigned a virtual life. A virtual life comprises of one A organ and two B organs. Each round consists of a finite number of periods in which you can earn money.
In each period of any round, you have a 10% probability of A organ failure and a 20% probability of B organ failure (both B organs fail together). You will never experience both types of organ failure at the same time. Whenever your A organ fails, you will cease to participate in that round. Whenever your B organs fail, you will be placed on a waiting list to receive one B organ donated from others. You may remain on the waiting list for up to 5 periods. If you do not receive a B organ within the 5 periods, you will cease to participate in that round.
Waiting List
If your B organ fails, you will be placed on a waiting list to receive one B organ donated by others in the order of your rank on the list. The rank is determined by the length of time that one has been waiting on the list. Those who have been waiting longer are ranked higher. Ranks of those who have the same waiting time are randomly determined. For example, if there are two persons on the waiting list. Person 1 has been waiting for 4 periods and person 2 has been waiting for 3 periods. According to the rule, person 1 ranks higher than person 2 on the list. If there were an active B organ donated, it would go to person 1 before person 2.
Earnings of Each Round
You will earn $3 in each period that you have an active A organ and at least one active B organ. However, you will not earn any money in any period that you are on the waiting list or you are no longer actively participating in the round.
Organ Donation Decision and Cost
At the beginning of each round, you begin by not being an organ donor. You will be asked to declare whether you want to change your status and become an organ donor in that round. Being an organ donor may potentially save two subjects who are in need of B organ and increase their earnings in that round. If you want to change your status, you must register yourself by checking the box on your screen; otherwise, you can leave the box empty. Please note that the organ donor registration (checking the box) will cost you $0.75. This registration cost will be charged whether or not you actually become a donor.
If you choose to be a donor and your A organ fails, your active B organs will be donated to those in need of a B organ in the order of their rank on the waiting list. Please note that the realized donation will cost you $2.25. This donation cost will only be charged if donation actually takes place. The organs you donated cannot be re-donated by recipients.
Final Payoff
Your payoff in each round is equal to your earnings in that round minus your costs of donation. There are multiple rounds in the experiment; however, only ONE round will be randomly selected for payment at the end of the experiment. Thus, you should make your decision in each round independently of your choice in other rounds. If in this selected round your earnings cannot cover your cost of donation, the extra cost will be charged from your show-up fee.
Appendix C: Experimental Instructions for the Opt-out Treatment
INSTRUCTIONS (Treatment ON)
Now that the experiment has begun, we ask that you do not talk. If you have a question after you finish reading the instructions, please raise your hand and the experimenter will approach you and answer your question in private. In today’s experiment, you are going to make decisions about hypothetical organ donation. None of the choices you make in the experiment today will affect your real life.
Show-up Fee
You have already earned U.S. $10 for arriving to the experiment on time.
Experiment
There are multiple rounds in the experiment today. In each round, you are assigned a virtual life. A virtual life comprises of one A organ and two B organs. Each round consists of a finite number of periods in which you can earn money.
In each period of any round, you have a 10% probability of A organ failure and a 20% probability of B organ failure (both B organs fail together). You will never experience both types of organ failure at the same time. Whenever your A organ fails, you will cease to participate in that round. Whenever your B organs fail, you will be placed on a waiting list to receive one B organ donated from others. You may remain on the waiting list for up to 5 periods. If you do not receive a B organ within the 5 periods, you will cease to participate in that round.
Waiting List
If your B organ fails, you will be placed on a waiting list to receive one B organ donated by others in the order of your rank on the list. The rank is determined by the length of time that one has been waiting on the list. Those who have been waiting longer are ranked higher. Ranks of those who have the same waiting time are randomly determined. For example, if there are two persons on the waiting list. Person 1 has been waiting for 4 periods and person 2 has been waiting for 3 periods. According to the rule, person 1 ranks higher than person 2 on the list. If there were an active B organ donated, it would go to person 1 before person 2.
Earnings of Each Round
You will earn $3 in each period that you have an active A organ and at least one active B organ. However, you will not earn any money in any period that you are on the waiting list or you are no longer actively participating in the round.
Organ Donation Decision and Cost
At the beginning of each round, you begin by being an organ donor. You will be asked to declare whether you want to change your status and become a non-donor in that round. Being an organ donor may potentially save two subjects who are in need of B organ and increase their earnings in that round. However, if you want to change your status, you must withdraw yourself by checking the box on your screen; otherwise, you can leave the box empty. Please note that the decision to withdrawal from being an organ donor (checking the box) will cost you $0.75.
If you keep your status as an organ donor and your A organ fails, your active B organs will be donated to those in need of a B organ in the order of their rank on the waiting list. Please note that the realized donation will cost you $2.25. This donation cost will only be charged if donation actually takes place. The organs you donated cannot be re-donated by recipients.
Final Payoff
Your payoff in each round is equal to your earnings in that round minus your costs of donation. There are multiple rounds in the experiment; however, only ONE round will be randomly selected for payment at the end of the experiment. Thus, you should make your decision in each round independently of your choice in other rounds. If in this selected round your earnings cannot cover your cost of donation, the extra cost will be charged from your show-up fee.
Appendix D: Experimental Instructions for the Priority Treatment
INSTRUCTIONS (Treatment IP)
Now that the experiment has begun, we ask that you do not talk. If you have a question after you finish reading the instructions, please raise your hand and the experimenter will approach you and answer your question in private. In today’s experiment, you are going to make decisions about hypothetical organ donation. None of the choices you make in the experiment today will affect your real life.
Show-up Fee
You have already earned U.S. $10 for arriving to the experiment on time.
Experiment
There are multiple rounds in the experiment today. In each round, you are assigned a virtual life. A virtual life comprises of one A organ and two B organs. Each round consists of a finite number of periods in which you can earn money.
In each period of any round, you have a 10% probability of A organ failure and a 20% probability of B organ failure (both B organs fail together). You will never experience both types of organ failure at the same time. Whenever your A organ fails, you will cease to participate in that round. Whenever your B organs fail, you will be placed on a waiting list to receive one B organ donated from others. You may remain on the waiting list for up to 5 periods. If you do not receive a B organ within the 5 periods, you will cease to participate in that round.
Waiting List
If your B organ fails, you will be placed on a waiting list to receive one B organ donated by others in the order of your rank on the list. The rank is determined by two criteria: first one’s donation decision, and second the length of time that one has been waiting on the list. If you are an organ donor, you will be given priority in ranking on the waiting list. Donors are ranked higher than the non-donors. Individuals with the same donation decision will be ranked according to the length of time they have been waiting. Those waiting longer are ranked higher. The ranks of those who have the same waiting time are randomly determined. For example, if there are two persons on the waiting list. Person 1 is an unregistered donor who has been waiting for 4 periods and person 2 is a registered donor who has been waiting for 3 periods. Person 2 will rank higher than person 1. If there were an active B organ donated, it would go to person 2 before person 1.
To reiterate, if you are not a donor, you will be ranked behind donors on the waiting list.
Earnings of Each Round
You will earn $3 in each period that you have an active A organ and at least one active B organ. However, you will not earn any money in any period that you are on the waiting list or you are no longer actively participating in the round.
Organ Donation Decision and Cost
At the beginning of each round, you begin by not being an organ donor. You will be asked to declare whether you want to change your status and become an organ donor in that round. Being an organ donor may potentially save two subjects who are in need of B organ and increase their earnings in that round. If you want to change your status, you must register yourself by checking the box on your screen; otherwise, you can leave the box empty. Please note that the organ donor registration (checking the box) will cost you $0.75. This registration cost will be charged whether or not you actually become a donor.
If you choose to be a donor and your A organ fails, your active B organs will be donated to those in need of a B organ in the order of their rank on the waiting list. Please note that the realized donation will cost you $2.25. This donation cost will only be charged if donation actually takes place. The organs you donated cannot be re-donated by recipients.
Final Payoff
Your payoff in each round is equal to your earnings in that round minus your costs of donation. There are multiple rounds in the experiment; however, only ONE round will be randomly selected for payment at the end of the experiment. Thus, you should make your decision in each round independently of your choice in other rounds. If in this selected round your earnings cannot cover your cost of donation, the extra cost will be charged from your show-up fee.
Appendix E: Experimental Instructions for the Opt-out with Priority Treatment
INSTRUCTIONS (Treatment OP)
Now that the experiment has begun, we ask that you do not talk. If you have a question after you finish reading the instructions, please raise your hand and the experimenter will approach you and answer your question in private. In today’s experiment, you are going to make decisions about hypothetical organ donation. None of the choices you make in the experiment today will affect your real life.
Show-up Fee
You have already earned U.S. $10 for arriving to the experiment on time.
Experiment
There are multiple rounds in the experiment today. In each round, you are assigned a virtual life. A virtual life comprises of one A organ and two B organs. Each round consists of a finite number of periods in which you can earn money.
In each period of any round, you have a 10% probability of A organ failure and a 20% probability of B organ failure (both B organs fail together). You will never experience both types of organ failure at the same time. Whenever your A organ fails, you will cease to participate in that round. Whenever your B organs fail, you will be placed on a waiting list to receive one B organ donated from others. You may remain on the waiting list for up to 5 periods. If you do not receive a B organ within the 5 periods, you will cease to participate in that round.
Waiting List
If your B organ fails, you will be placed on a waiting list to receive one B organ donated by others in the order of your rank on the list. The rank is determined by two criteria: first one’s donation decision, and second the length of time that one has been waiting on the list. If you are an organ donor, you will be given priority in ranking on the waiting list. Donors are ranked higher than the non-donors. Individuals with the same donation decision will be ranked according to the length of time they have been waiting. Those waiting longer are ranked higher. The ranks of those who have the same waiting time are randomly determined. For example, if there are two persons on the waiting list. Person 1 is an unregistered donor who has been waiting for 4 periods and person 2 is a registered donor who has been waiting for 3 periods. Person 2 will rank higher than person 1. If there were an active B organ donated, it would go to person 2 before person 1.
To reiterate, if you are not a donor, you will be ranked behind donors on the waiting list.
Earnings of Each Round
You will earn $3 in each period that you have an active A organ and at least one active B organ. However, you will not earn any money in any period that you are on the waiting list or you are no longer actively participating in the round.
Organ Donation Decision and Cost
At the beginning of each round, you begin by being an organ donor. You will be asked to declare whether you want to change your status and become a non-donor in that round. Being an organ donor may potentially save two subjects who are in need of B organ and increase their earnings in that round. However, if you want to change your status, you must withdraw yourself by checking the box on your screen; otherwise, you can leave the box empty. Please note that the decision to withdrawal from being an organ donor (checking the box) will cost you $0.75.
If you keep your status as an organ donor and your A organ fails, your active B organs will be donated to those in need of a B organ in the order of their rank on the waiting list. Please note that the realized donation will cost you $2.25. This donation cost will only be charged if donation actually takes place. The organs you donated cannot be re-donated by recipients.
Final Payoff
Your payoff in each round is equal to your earnings in that round minus your costs of donation. There are multiple rounds in the experiment; however, only ONE round will be randomly selected for payment at the end of the experiment. Thus, you should make your decision in each round independently of your choice in other rounds. If in this selected round your earnings cannot cover your cost of donation, the extra cost will be charged from your show-up fee.
Appendix F: Experimental Instructions for the Neutral Treatment
INSTRUCTIONS (Treatment NF)
Now that the experiment has begun, we ask that you do not talk. If you have a question after we finish reading the instructions, please raise your hand and the experimenter will approach you and answer your question in private.
Show-up Fee
You have already earned U.S. $10 for arriving to the experiment on time.
Experiment
There are multiple rounds in the experiment today. At the beginning of each round, you will be assigned with three tokens: one A token and two B tokens. Each round of the experiment consists of a finite number of periods in which you can potentially earn more money.
In each period of any round, it is possible that you will lose your tokens. There is a 10% probability of losing an A token and 20% probability of losing both B tokens (both B tokens will be lost the same time). You will not lose both types of tokens at the same time. Whenever you lose an A token in a round, you will cease to participate in that round. Whenever you lose both B tokens in a round, you will be placed on a waiting list to receive a B token donated by others. You may remain on the waiting list for up to 5 periods. If you do not receive one B token within the 5 periods, you will cease to participate in that round.
Waiting List
If you lose your B tokens, you will be placed on a waiting list to receive one donated by others in the order of your rank on the list. The rank is determined by the length of time that one has been waiting on the list, and the ones who have been waiting longer are ranked higher. The ranks of those who have the same waiting time are randomly determined. For example, if there are two persons on the waiting list. Person 1 has been waiting for 4 periods and person 2 has been waiting for 3 periods. According to the rule, person 1 ranks higher than person 2 on the list. Whenever there is an available B token, it will go to person 1 before person 2.
Earnings of Each Round
You will earn $3 in each period in which you have one A token and at least one B token. Please note that you will not earn any money in a period in which you are on the waiting list or you are no longer actively participating in the round (i.e., do not have at least one active B token).
Donation Decision and Cost
At the beginning of each round, you will be asked to declare whether you want to donate your B tokens after you lost your A token. Donating may potentially increase other’s earnings in that round. If you want to donate your B tokens, you must register yourself as a donor by checking the box on your screen; otherwise, you can leave the box empty. Please note that the decision to register as a donor (checking the box) will cost you $0.75.
If you choose to be a donor and you lose your A token, your B tokens will be donated to those who are on the waiting list in the order of their rank. Please note that the realized donation will cost you $2.25. This donation cost will only be charged if a donation actually takes place. The tokens you donated cannot be re-donated by recipients.
Final Payoff
Your payoff in a round is equal to your earnings in that round minus your costs of donation. There are multiple rounds in the experiment; however, only ONE round will be randomly selected for payment at the end of the experiment. Thus, you should make your decision in each round independently of your choice in other rounds. If in this selected round your earnings cannot cover your cost of donation, the extra cost will be charged from your show-up fee.
Footnotes
It is worth noting that the reported deaths while on the waiting list per 1,000 patient years at risk has decreased from 104.6 in 2000 to 84.5 in 2009 (SRTR 2012). This is primarily due the advancements in care for these patients and not a function of increased transplantation.
Based on the 2012 National Donor Designation Report Card by the Donate Life America at http://donatelife.net/wp-content/uploads/2012/06/DLA-Report-Card-2012-350781.pdf
While a live donor can give a kidney, or a portion of the liver, lung, intestine, or pancreas, it is essentially impossible for live donation of solid organs such as the heart, pancreas, and intestinal organs.
This policy was announced in June 1998: http://archive.hhs.gov/news/press/1998pres/980617.html
The Organ Donation Breakthrough Collaborative began in 2003 at the request of HHS Secretary Tommy G. Thompson.
Healy indicates the possibility of donating is affected by the network ties to recipients, educational attainment, and income. However, these effects vary across countries. For example, the network ties to recipient have a strongly positive effect in Germany. However, the network effects are very weak in British.
A zero HLA mismatch with a particular donor will automatically move a patient up the waiting queue.
The final decision to utilize an organ is made by the transplant surgeon. However, changes in the allocation mechanism will alter the distribution of organ offers.
The new organ allocation policy was first suggested to the Israel National Transplant Council (INTC) in 2006. It was put into effect in January 2010. The new policy can be found as the Organ Transplant Law 5768-2008, Israeli Book of Laws (English translation provided by the Israeli Ministry of Justice).
Details of the HOTA can be found http://statutes.agc.gov.sg/aol/search/display/view.w3p;page=0;query=DocId%3Adb05e985-f8a0-4d61-a906-9fd39f3b5ac9%20Depth%3A0%20ValidTime%3A02%2F01%2F2011%20TransactionTime%3A31%2F07%2F2005%20Status%3Ainforce;rec=0#legis
Kessler and Roth (2012) have the design of one A units with two B units, where A represents brain and B represents kidney. We keep the consistent design so that the results of our experiment are comparable.
These parameters are identical to those have been used by Kessler and Roth (2012). We also conducted additional sensitivity analyses, discussed in Appendix A, specific to our design to ensure they are appropriate.
The assumption here is that a subject can function normally with one B organ donated by another subject. This is consistent with kidney transplantation practice.
The true costs associated with organ donation cannot be measured. Here we impose these costs merely to model the incentives involved in organ donation. Since the costs vary as the default choice changes, we divide the costs into two parts, the cost of overriding the default and the cost of donation.
A copy of the experiment instructions for each of the five treatments can be obtained from the corresponding author.
The ordering of subjects on the waiting list implicitly assumes that all the subjects are homogeneous with regard to their patient-specific characteristics that might impact their status in the queue in the real world. This is a necessary abstraction so that we can focus on the treatment effects within our experiment.
The experiment was conducted using the experimental software z-Tree 3.3.6 (Fishbacher 2007).
The results are qualitatively the same when we cluster at the session level.
A series Wilcoxon rank-sum tests were also conducted comparing the Control and Opt-out treatments. The test statistics were −14.988, −11.493 and −9.713 for the pooled data, first 15 rounds and last 15 rounds of the experiment, which further support our first research hypothesis.
A series of Wilcoxon rank-sum tests further confirm the treatment effects. The test statistics are −22.309, −13.895, and −17.680 when comparing the Control treatment with the Priority treatment for all the rounds, rounds 1–15 and rounds 16–30 respectively. The test statistics comparing the Opt-out with the Opt-out with priority treatment are −11.656, −7.402 and −9.102 when comparing the total rounds, rounds 1–15 and rounds 16–30 respectively.
A series of Wilcoxon rank-sum tests were also conducted and all of them concluded that the Opt-out with Priority treatment generated the statistically significant and higher donation rates than all the other treatments. The results from these tests can be obtained from the corresponding author.
A series of Wilcoxon rank-sum tests were conducted as well comparing the donation rates between the Control and Neutral treatments. The test statistics were 5.376, 2.362 and 5.431 for all rounds, the first 15 and the last 15 rounds respectively. This further supports the parametric regression results.
The Advisory Committee on Organ Transplant was established to assist the Health and Human Services Secretary in enhancing organ donation, ensuring that the system of organ transplantation is grounded in the best available medical science, assuring an effective and equitable system, and increasing public confidence.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Danyang Li, Email: prcdlx@gmail.com.
Zackary Hawley, Email: z.hawley@tcu.edu.
Kurt Schnier, Email: kschnier@gsu.edu.
References
- Abbink K, Hennig-Schmidt H. Neutral versus loaded instructions in a bribery experiment. Experimental Economics. 2006;9 (2):103–121. [Google Scholar]
- Bonnie RJ, Wright S, Dineen KK. Legal authority to preserve organs in cases of uncontrolled cardiac death: Preserving family choice. Journal of Law, Medicine and Ethics. 2008;36 (4):741–751. doi: 10.1111/j.1748-720X.2008.00333.x. [DOI] [PubMed] [Google Scholar]
- Breyer F, Kliemt H. The shortage of human organs: Causes, consequences and remedies. Analyse & Kritik. 2007;29:188–205. [Google Scholar]
- Cason TN, Raymond L. Framing effects in an emissions trading experiment with voluntary compliance. In: Isaac RM, Norton DA, editors. Experiments on Energy, the Environment, and Sustainability. Emerald Group Publishing Limited; Bingley: 2011. pp. 77–114. [Google Scholar]
- Donate Life America. National donor designation report card 2012. Richmond, VA: 2012. [Google Scholar]
- Fischbacher U. z-Tree: Zurich toolbox for ready-made economic experiments. Experimental Economics. 2007;10 (2):171–178. [Google Scholar]
- Gäbel H. Donor and non-donor registries in Europe. Stockholm, Sweden: on behalf of the committee of experts on the organizational aspects of co-operation in organ transplantation of the council of Europe; 2002. [Google Scholar]
- Gerber D. Comment made during the U.S. Department of Health and Human Services Advisory Committee on Organ Transplantation (ACOT) Meeting on March 7, 2013. [last accessed July 28, 2013];Minutes from the conference call available online. 2013 http://www.organdonor.gov/legislation/acotmarch2013notes.html.
- Howard DH, Siminoff LA, McBride V, Lin M. Does quality improvement work? Evaluation of the organ donation breakthrough collaborative. Health Service Research. 2007;42 (6):2294–2323. doi: 10.1111/j.1475-6773.2007.00732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy K. Last best gifts: Altruism and the market for human blood and organs. University of Chicago Press; Chicago and London: 2006. [Google Scholar]
- Johnson EJ, Bellman S, Lohse GL. Defaults, framing and privacy: Why opting in-opting out. Marketing Letters. 2002;13 (1):5–15. [Google Scholar]
- Johnson EJ, Goldstein DG. Do defaults save lives? Science. 2003;302:1338–1339. doi: 10.1126/science.1091721. [DOI] [PubMed] [Google Scholar]
- Johnson EJ, Goldstein DG. Defaults and donation decisions. Transplantation. 2004;78 (12):1713–1716. doi: 10.1097/01.tp.0000149788.10382.b2. [DOI] [PubMed] [Google Scholar]
- Johnson EJ, Hershey J, Meszaro J, Kunreuther H. Framing, probability distortions, and insurance decisions. Journal of Risk and Uncertainty. 1993;7 (1):35–51. [Google Scholar]
- Kessler JB, Roth AE. Organ allocation policy and the decision to donate. American Economic Review. 2012;102 (5):2048–2082. doi: 10.1257/aer.102.5.2018. [DOI] [PubMed] [Google Scholar]
- Lavee J, Ashkenazi T, Gurman G, Steinberg D. A new law for allocation of donor organs in Israel. The Lancer. 2010;375 (9720):1131–1133. doi: 10.1016/S0140-6736(09)61795-5. [DOI] [PubMed] [Google Scholar]
- Madrian BC, Shea DF. The power of suggestion: Inertia in 401(k) participation and savings behavior. Quarterly Journal of Economics. 2001;116 (4):1149–1187. [Google Scholar]
- Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR) OPTN/SRTR 2010 annual data report. Rockville, MD: 2011. [Google Scholar]
- Samuelson W, Zeckhauser R. Status quo bias in decision making. Journal of Risk and Uncertainty. 1988;1 (1):7–59. [Google Scholar]
- Shafer TJ, Wagner D, Chessare J, et al. US organ donation breakthrough collaborative increases organ donation. Critical Care Nursing Quarterly. 2008;31 (3):190–210. doi: 10.1097/01.CNQ.0000325044.78904.9b. [DOI] [PubMed] [Google Scholar]