Abstract
Objective
Traumatic joint injury can initiate early cartilage degeneration in the presence of elevated inflammatory cytokines (e.g., TNF-α and IL-6). The positive/negative effects of post-injury dynamic loading on cartilage degradation and repair in vivo is not well-understood. This study examined the effects of dynamic strain on immature bovine cartilage in vitro challenged with TNF-α + IL-6 and its soluble receptor (sIL-6R) with/without initial mechanical injury.
Methods
Groups of mechanically injured or non-injured explants were cultured in TNF-α + IL-6/sIL-6R for 8 days. Intermittent dynamic compression was applied concurrently at 10%, 20%, or 30% strain amplitude. Outcome measures included sGAG loss (DMMB), aggrecan biosynthesis (35S-incorporation), aggrecanase activity (Western blot), chondrocyte viability (fluorescence staining) and apoptosis (nuclear blebbing via light microscopy), and gene expression (qPCR).
Results
In bovine explants, cytokine-alone and injury-plus-cytokine treatments markedly increased sGAG loss and aggrecanase activity, and induced chondrocyte apoptosis. These effects were abolished by moderate 10% and 20% strains. However, 30% strain-amplitude greatly increased apoptosis and had no inhibitory effect on aggrecanase activity. TNF+IL-6/sIL-6R downregulated matrix gene expression and upregulated expression of inflammatory genes, effects that were rescued by moderate dynamic strains but not by 30% strain.
Conclusions
Moderate dynamic compression inhibits the pro-catabolic response of cartilage to mechanical injury and cytokine challenge, but there is a threshold strain-amplitude above which loading becomes detrimental to cartilage. Our findings support the concept of appropriate loading for post-injury rehabilitation.
Keywords: Dynamic Compression, Cartilage, Injury, Cytokines, Apoptosis, Rehabilitation post-injury
INTRODUCTION
Joint injuries such as the anterior cruciate ligament (ACL) tear are a major risk factor for osteoarthritis (OA) later in life. The initial joint trauma can be a single disruption of the ligament, or accompanied by damage to cartilage, meniscus, synovium, and subchondral bone. Post-injury evaluation of the synovial fluid from ACL-deficient patients has revealed inflammation-associated biochemical changes including increased levels of pro-inflammatory cytokines (e.g., TNF-α, IL-1, and IL-6) as well as matrix protein degradation products generated by matrix metalloproteinases (MMPs) and ADAMTS aggrecanases (A Disintegrin And Metalloproteinase with Thrombospondin Motifs)[1–4]. This inflammatory response, which can be prolonged after the initial injury, is believed to act in conjunction with abnormal mechanical loading to accelerate cartilage degeneration that eventually leads to OA. Indeed, studies comparing OA patients with or without prior joint injury provided strong evidence that ACL tears can significantly increase the risk for early OA[5–7].
In vivo, articular cartilage is subjected to a complex combination of shear, compressive, and tensile stress under normal loading conditions. After joint injury, in addition to the inflammatory response, trauma-induced joint instability also alters the contact mechanics between articular surfaces[8]. In particular, Van de Velde[9, 10] used dual fluoroscopic and MR imaging techniques to quantify tibiofemoral joint kinematics in both normal and ACL-deficient human patients. Their results showed that cartilage contact deformation increased significantly to ~20–30% in the ACL-deficient knee from ~15–20% in the contralateral healthy knee during lunge motion with 0–30° flexion[10]; while surgical reconstruction restored some of the in vivo contact biomechanics, the increased cartilage deformation was not ameliorated[11]. These studies raise the question of whether post-injury joint loading can cause additional damage to cartilage, and whether there exists a range of motion within which rehabilitative loading can be beneficial in maintaining cartilage structure and function.
Over the last two decades, in vitro injury models have been developed to facilitate understanding of cartilage mechanical injury on the onset and progression of OA[12–14]. Consistently, injurious loading has been shown to result in loss of proteoglycans[15], tissue swelling[14], collagen network damage[12], and reduced tissue stiffness[13]. In addition, significantly increased chondrocyte apoptosis was observed[16, 17], especially in the superficial zone[18], and the degree of cell damage was age-dependent[19]. Matrix biosynthesis by remaining live cells was also suppressed by injury[13]. Furthermore, injury potentiates proteoglycan catabolism induced by exogenous cytokines TNF-α and IL-6[20], which were introduced to simulate the inflammatory environment seen in vivo after joint injury. These studies have furthered our understanding of the immediate effects of mechanical injury; however, the interplay between cytokines and post-injury mechanical signals is less understood.
Dynamic compression can induce anabolic responses in normal cartilage which promote matrix biosynthesis with a strong dependence on compression frequency, amplitude, and loading duty cycle[21–24]. The spatial profiles of cell-mediated matrix biosynthesis have been correlated with compression-induced interstitial fluid flow[25–27], and the mechano-transduction pathways involve MAPK activation, intracellular calcium and cyclic AMP[28, 29]. Additionally, dynamic compression can mitigate the catabolic responses of chondrocytes to cytokines in tissue-engineered cultures[30]. However, little is known about the effects of follow-on dynamic compression after injury/cytokine- challenge in intact cartilage.
In the present study, we implemented a previously-characterized in vitro injury model involving cytokines TNF-α and IL-6/sIL-6R with or without initial mechanical injury, and investigated the effects of intermittent unconfined dynamic compression (10%–30% strain amplitude) on immature bovine cartilage. We hypothesized that (1) dynamic compression can maintain anabolic effects in an inflammatory environment by rescuing matrix biosynthesis suppressed by cytokines[31]; (2) dynamic compression has an additional anti-catabolic role in reducing cytokine-mediated cartilage degradation; (3) there is a range of strain amplitudes within which dynamic compression is beneficial, while overload strain amplitudes above a threshold can be deleterious.
MATERIALS AND METHODS
Bovine articular cartilage harvest and culture
Articular cartilage disks were harvested from the femoropatellar grooves of 1–2-week-old calves, obtained on the day of slaughter (Research ‘87, Boylston, MA). A total of 19 joints from 15 different animals were used. Full-thickness cartilage cylinders were cored using a 3-mm dermal punch, and the top 1-mm disk containing intact superficial zone was harvested with a blade. Disks were incubated in serum-free medium (low-glucose Dulbecco’s Modified Eagle’s Medium [DMEM; 1g/L]) supplemented with 1% insulin–transferrin–selenium (ITS, 10 g/ml, 5.5 g/ml, and 5 g/ml, respectively, Sigma, St. Louis, MO), 10 mM HEPES buffer, 0.1 mM nonessential amino acids, 0.4 mM proline, 20 g/ml ascorbic acid, 100 units/ml penicillin G, 100 g/ml streptomycin, and 0.25 g/ml amphotericin B for 2–3 days (5% CO2; 37°C). Disks for each test were match for anatomic location on the joint surface, and the thickness variation for those receiving dynamic compression was limited to <5%.
Injurious compression and exogenous cytokines
After equilibration, groups of cartilage disks were injuriously compressed in a custom-designed, incubator-housed loading apparatus (Figure 1A)[32]. As described previously[33], each bovine disk was placed in a polysulfone chamber and subjected to radially unconfined compression to 50% final strain at a strain rate of 100%/s, followed by immediate release at the same rate (Figure 1B). After injury, disks were immediately placed in treatment medium in the presence or absence of rhTNF-α (25 ng/ml), rhIL-6 (50 ng/ml), and sIL-6R (250 ng/ml) (R&D Systems, Minneapolis, MN). Previous studies showed that this combination of cytokines caused significantly greater sulfated glycosaminoglycan (sGAG) loss than either cytokine alone[20, 34].
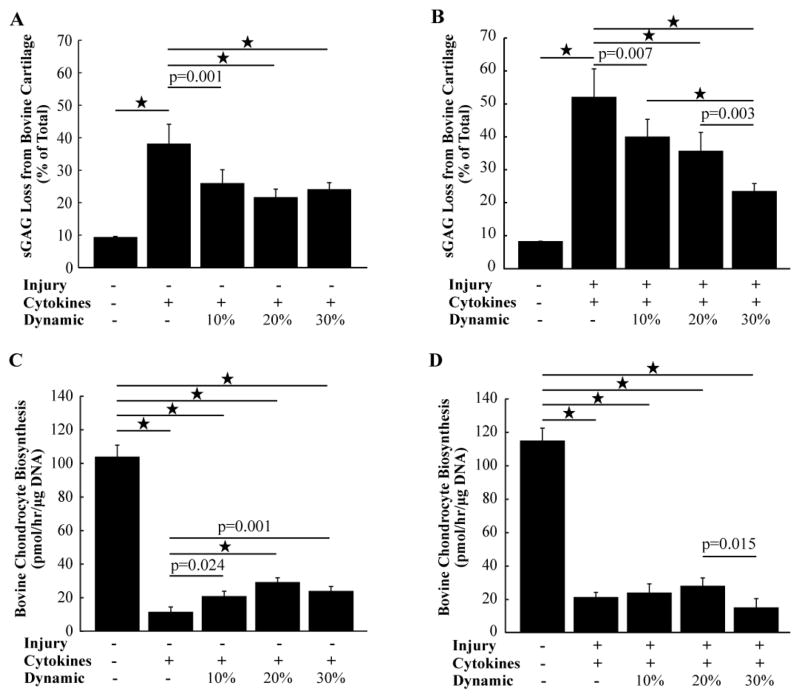
Figure 1.
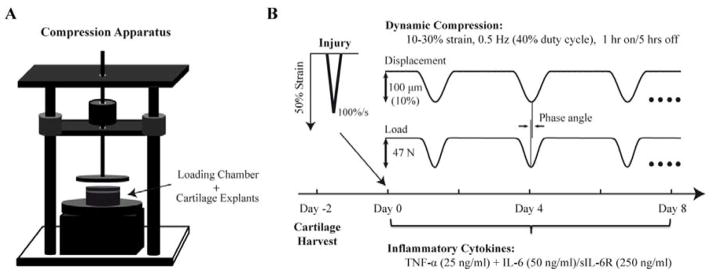
A, Schematic of custom-designed, incubator-housed loading apparatus [32] used to perform injurious and dynamic compression. B, Experimental design: Injurious compression was applied to cartilage explants on Day 0, followed by immediate incubation in TNF-α + IL-6/sIL-6R. Intermittent dynamic compression started on Day 0 (10%, 20% or 30% applied strain amplitude) and continued up through Day 8. Representative waveforms shown for a 10% dynamic strain amplitude applied to a group of 12 disks within the loading chamber, and the corresponding measured total compressive load.
Dynamic compression
On Day 0 (Figure 1B), one disk was placed (with superficial surface facing upward) in each well of a 12-well polysulfone loading chamber, with 0.3 ml treatment medium. The chamber was then inserted into the loading apparatus (Figure 1A). Disks were statically compressed to 10% strain to ensure contact, and unconfined dynamic compression was then superimposed using a displacement-controlled haversine waveform (0.5 Hz, 40% duty cycle) continuously for 1 hour, followed by 5 hours rest with the applied static and dynamic load removed. This [1-hour load]—[5-hour-rest] cycle was repeated 4 times per day (Figure 1B). Dynamic compression at three different strain amplitudes (10%, 20%, and 30%) was applied to 3 different groups of 12 bovine explants simultaneously using three identical loading instruments. Medium was changed every 2 days.
sGAG biosynthesis and biochemical analysis
On Day 6, culture medium was supplemented with 5 μCi/ml [35S]-sulfate (Perkin-Elmer, Norwalk, CT). After 48-hour radiolabeling, disks were washed 4 times over 80 min with cold PBS to completely remove the free label. Each disk was measured to determine its wet weight and then was digested with proteinase K (Roche, Indianapolis, MN) overnight. The sGAG content in the medium and digested explants was quantified using the dimethylmethylene blue assay[35]. The amount of radiolabel in each digested sample and the medium standard [35S]-sulfate were measured using a liquid scintillation counter[21]. Radiolabel concentration was calculated from the standard and then was normalized to DNA (measured via Hoechst 33258 dye-binding)[36].
Histologic analysis
After 4 days of treatments, disks (N = 4 from each group) were fixed in 4% paraformaldehyde overnight at 4°C. Next day, disks were cut in half and one of the halves was embedded in paraffin. Serial cross-sections (3 mm-long × 1 mm-wide × 5 μm-thick) were microtomed, immobilized on glass slides, and stained with Mayer’s hematoxylin. To quantify cell apoptosis, 1–2 slices from each cross-section were evaluated by light microscopy with a 40x objective. To exclude artifacts of cutting-induced cell death at specimen edges, only cells 100 μm inward from the cut-edges were examined (the superficial-most cells were examined). Nine optical fields (each 0.2 mm × 0.2 mm) were examined for each slice, distributed evenly between left, central, and right positions of the superficial, middle, and deep zones of the tissue. Chondrocytes with condensed and blebbed nuclei were counted as apoptotic cells based on previously published methods and analyses[19], and the rest were counted as normal cells (30–70 total cells/field).
Cell viability
To further study the effect of dynamic compression on chondrocyte viability, tested bovine and human disks were cut into 100–200 μm-thick slices (3 mm-long × 1 mm-wide cross-sections from superficial surface to 1-mm deep). Fluorescein diacetate (FDA; 4 μg/ml in PBS) was used to stain viable cells green while propidium iodide (PI; 40 μg/ml in PBS) (both from Sigma) stained non-viable cells red. Two slices from each explant were stained for 2–3 minutes in the dark and then washed with PBS. Two separate images were taken for each slice using a Nikon fluorescence microscope with a 4x objective.
Gene expression analyses
Bovine cartilage explants from 4 different animals (6 disks per condition per animal) were treated for 48 hours and stored in −80°C after flash-freezing. On the extraction day, the 6 disks from each condition were pooled, pulverized, and lysed in TRIzol reagent (Invitrogen, Carlsbad, CA) with a homogenizer, as previously described in detail [28, 37]. The extract was then separated using phase-gel tubes (Eppendorf, Hamburg, Germany), and the supernatant was purified following the Qiagen RNeasy mini kit protocol (Qiagen, Chatsworth, CA). Reverse transcription was performed with equal amounts of RNA from each condition using the AmpliTaq-Gold Reverse Transcription kit (Applied Biosystems, Foster City, CA). Primer pairs used were previously reported [28, 37] except for the newly designed primer: NF-κB (p65 unit; forward 5′-CGGGTGAATCGGAACTCTGG-3′, reverse 5′-TCGATGTCCTCTTTCTGCACC-3′). Real-time qPCR was performed via 384-well plate format using the Applied Biosystems 7700HT instrument with SYBR Green Master Mix (Applied Biosystems) and analyzed as described in detail previously[28, 37]. Gene expression levels were normalized to the housekeeping gene 18S, as previous studies with this system have demonstrated the utility of this reference gene [28, 37].
Aggrecan degradation by western analysis
Explants were diced and extracted in 4M Guanidine for 48 hours at 4°C. The extracted aggrecan was precipitated overnight at −20°C in 100% ethanol with 5 mM sodium acetate, and then deglycosylated using chondroitinase ABC, keratanase II, and endo-β-galactosidases (all from Seikagaku America, Rockville, MD). Equal amounts of sGAG were loaded on a 4–12% Bis-Tris gradient gel (Invitrogen), and proteins were separated by electrophoresis. Western blot analysis was performed using the monoclonal antibody anti-NITEGE (kindly provided by Dr. Carl Flannery), which is specific to aggrecanase-generated NITEGE neoepitope (Glu373-Ala374)[38].
Statistical analysis
To analyze the effects of dynamic compression on sGAG loss and biosynthesis in bovine explants, a linear mixed effects model was used with animal as a random factor, followed by Tukey’s post hoc comparison. Bovine chondrocyte apoptosis data from histological images were analyzed using three-way analysis of variance (ANOVA), followed by Tukey’s post hoc comparison. Bovine chondrocyte gene expression was log-transformed and analyzed by the linear mixed effect model with animal as a random factor, followed by Bonferroni’s test for pair-wise comparisons. Human explant studies were all evaluated using two-way ANOVA with Tukey’s post hoc comparison. Statistical analysis was performed using Systat 12 software (Richmond, CA).
RESULTS
Effects of dynamic compression on sGAG loss, sGAG biosynthesis, and aggrecanase activity in cytokine-treated bovine explants with or without injury
In the absence of initial injury, cytokine treatment alone induced significantly higher sGAG loss to the medium compared to untreated controls during an 8-day experiment (38.1 ± 6.1% vs. 9.3 ± 0.4%, mean ± 95% confidence interval, p < 0.0001, n = 18 from 3 different animals) (Figure 2A). The addition of 10% dynamic strain significantly reduced sGAG loss to 25.9 ± 4.2% (p = 0.0001 vs. cytokines alone), and there was a further reduction to 21.6 ± 2.6% when 20% dynamic strain was applied. 30% dynamic strain also caused a decrease in sGAG loss similar to the more moderate 10% and 20% strain.
Figure 2.
A&B, Cumulative sGAG loss from bovine cartilage to the medium in response to 8-day treatments without or with initial mechanical injury. C&D, Bovine chondrocyte biosynthesis measured during day 6–8 as 35S-sulfate incorporation rate for the same cartilage disks as in A&B, respectively. Values are mean ±95% confidence interval; A&C: N = 3 animals (6 disks/animal); B&D: N = 4 animals (4–6 disks/animal); * = P < 0.001.
In the presence of injury, the initial injurious compression produced peak stresses of 18.5 ± 0.4 MPa (n = 96 disks from 4 different animals). Without dynamic compression, the combined injury plus 8-day-cytokine treatment induced 51.4 ± 8.8% sGAG loss (Figure 2B) which was significantly greater than the 7.8 ± 0.2% sGAG loss from untreated controls (p < 0.0001), consistent with previous findings[20]. Similar to the case without initial injury, the addition of moderate dynamic compression at 10% and 20% strain amplitude reduced this 51.4 ± 8.8% sGAG loss to 39.4 ± 5.5% (p = 0.007) and 35.1 ± 5.9% (p < 0.0001), respectively (Figure 2A). In contrast to Figure 2A, however, the largest inhibitory effect of dynamic compression was at 30% strain amplitude (22.9 ± 2.5%), which was a significant decrease even from the 20% strain amplitude (p = 0.003).
35S-sulfate incorporation during the last 2 days of culture was used to assess sGAG biosynthesis. Compared to controls (103.1 ± 7.4 pmoles/hour/μg DNA), cytokine treatment alone significantly reduced biosynthesis (p < 0.0001, Figure 2C). There was a significant increase in biosynthesis (rescuing effect) with increased dynamic strain up to 20%; 30% dynamic strain also showed a significantly higher biosynthesis rate than cytokines alone (p = 0.0012). Similarly, in the presence of initial injury, injury-plus-cytokine treatment significantly reduced biosynthesis compared to untreated controls (p < 0.0001, Figure 2D). Addition of 10% and 20% dynamic compressive strains did not alter this result (p = 0.946 and p = 0.434, respectively); however, 30% dynamic strain caused a further decrease in biosynthesis rate compared to 20% strain amplitude (p = 0.015).
Effects of dynamic compression on aggrecan cleavage
Aggrecan core protein neoepitope NITEGE373-A374 generated by aggrecanases (ADAMTS-4/5) was assessed on Days 2, 4, and 8 after treatments. No detectable NITEGE fragments were found in any conditions on Day 2 or Day 4 (data not shown), consistent with a previous study[39]. However, by Day 8, NITEGE-positive fragments were detected following cytokines treatment alone (Figure 3A) and injury-plus-cytokine treatment (Figure 3B). In the absence of injury, 10% and 20% dynamic strain strongly reduced NITEGE bands. However, 30% dynamic strain showed increased signal compared to the moderate dynamic strain (Figure 3A). This effect was even more obvious when initial injury was present (Figure 3B): while the abundance of NITEGE neoepitopes was markedly reduced by 10% dynamic strain amplitude and essentially abolished by 20%, NITEGE was unaffected by 30% strain. This experiment was repeated using two additional animals with similar results (data not shown).
Figure 3.
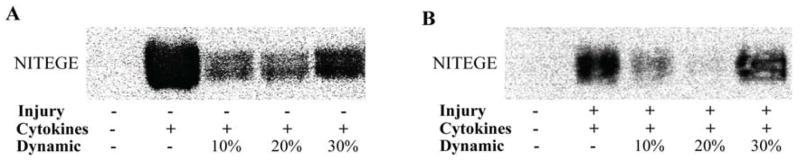
Western analysis of aggrecan fragments using the antibody to the aggrecanase-generated neoepitope, NITEGE, with aggrecan extracted from the bovine explants 8 days after treatments without (A) or with (B) initial mechanical injury.
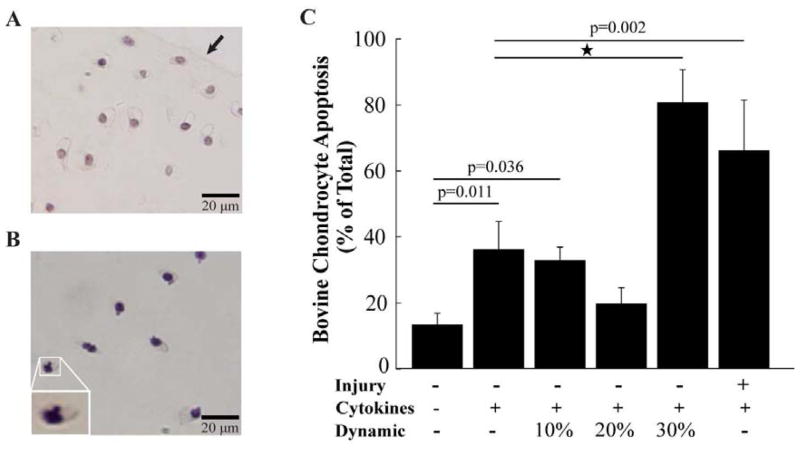
Effects of dynamic compression on cytokine-induced apoptosis in bovine cartilage
Since mechanical injury is known to induce chondrocyte apoptosis [19], we hypothesized that high-magnitude dynamic compression can act in a similar manner and induce cell apoptosis. In order to test this hypothesis and to parse out the individual effects of dynamic compression versus injury, chondrocyte apoptosis was first assessed 4 days after treatment in the presence of cytokines but without initial injury; injury-plus-cytokine treatment then served as a positive control. Compared to normal cells (Figure 4A), apoptotic chondrocytes exhibited condensed cytoplasm and chromatin, as well as nuclear blebbing (Figure 4B). Treatment with cytokines alone significantly increased cell apoptosis compared to untreated controls (p = 0.011, Figure 4C), consistent with the consensus that TNF-α signals through apoptotic pathways[40]. Interestingly, 20% dynamic strain reduced apoptosis to levels not different than controls (p = 0.879). But at 30% strain amplitude, apoptosis dramatically increased (p < 0.0001 compared to cytokines-alone), reaching levels not different from treatment by injurious compression plus cytokines (p = 0.232), which is significant from cytokines-alone treatment (p = 0.002).
Figure 4.
Bovine chondrocyte apoptosis within the explants in response to 4-day treatments. A, Representative image (40X objective) of histological sections from untreated control disks using hematoxylin staining for the nucleus. The superficial-most surface is visualized in the upper right corner (arrow). B, Histological section from explant treated with the combination of cytokines (TNF-α + IL-6/sIL-6R) plus intermittent 30% dynamic strain amplitude. Image (40X objective) was taken from middle zone cartilage: apoptotic cells displayed nuclear blebbing, a morphological marker of apoptosis [19]. Insert: Higher magnification of nuclear blebbing. C, Percentage of chondrocytes in histological sections that underwent apoptosis, quantified as the ratio of cells showing nuclear blebbing to total cell count; n = 4 disks per condition (see Methods). Values are mean ± 95% confidence interval; * = P < 0.001.
Chondrocyte viability in bovine cartilage
To examine whether the presence of initial injury can alter the effects of dynamic compression on chondrocyte viability shown in Figure 4, cell viability in the explants after 2, 4, and 8 days treatments was further assessed via live-dead fluorescence. Representative images (Figure 5) showed minimal cell death in control samples over 8 days. In contrast, injury-plus-cytokines caused marked cell death throughout tissue cross-sections, especially in the superficial zone (cell death in the radial periphery was caused by cutting-induced damage). Qualitatively, dynamic compression at 10% or 20% strain amplitude had little or no additional effect, consistent with the absence of additional apoptosis (Figure 4C). However, addition of 30% dynamic strain to injury-plus-cytokines (Figure 5, right most column) resulted in a further marked loss of cell viability by Day 4, and more so by Day 8. This is also consistent with Figure 4C, where 30% dynamic strain + cytokines treatment in the absence of injury already showed a dramatic increase in cell apoptosis, similar to the injury-plus-cytokine treatment.
Figure 5.
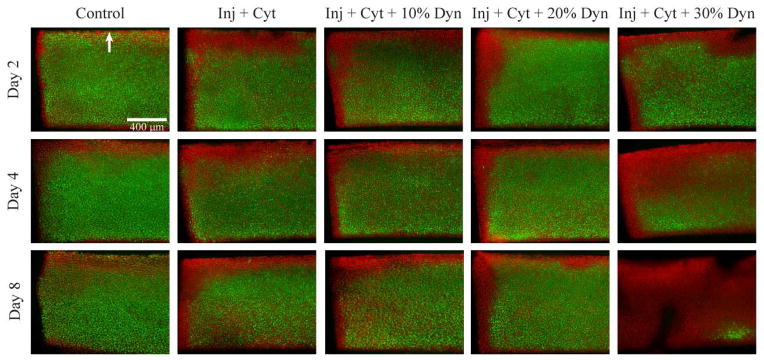
Fluorescently stained bovine explants after treatments for 2, 4, and 8 days. A single injurious compression was applied on Day 0, followed by culture in exogenous cytokines. Intermittent dynamic compression (10%, 20%, or 30% strain amplitude) was applied and continued throughout the entire 2–8 day culture period (Figure 1B). Cartilage disks were stained immediately upon termination of culture with fluorescein diacetate (FDA, green) for viable cells and propidium iodide (PI, red) for non-viable cells. Images were taken with a 4X objective. The superficial-most surface is at the top of each image (arrow), while a cut at the middle/deep zone is at the bottom. The left edge of each disk was created when a dermal punch was used to harvest the cartilage disks, each having dimensions 3 mm diameter by 1 mm thick. Inj: injurious compression; Cyt: cytokines TNF-α + IL-6/sIL-6R; Dyn: dynamic compression. Bar = 400 μm.
Bovine chondrocyte gene expression
To elucidate the mechanism of action of dynamic compression, qPCR was used to examine gene expression after 48-hour treatments in the absence of injury. Aggrecan gene expression was markedly suppressed by cytokines-alone (p < 0.0001, Figure 6), consistent with previous findings[34]. Dynamic compression partially rescued this decrease regardless of the strain amplitude (p < 0.0001 for all 3 strains). Collagen II expression showed a similar overall response, except that 30% dynamic strain did not rescue the cytokine-induced decrease in collagen II expression (p = 0.21). Cytokine treatment markedly upregulated expression of ADAMTS-4 and -5 compared to controls (p < 0.0001 for both). While dynamic compression had no effect on ADAMTS-4 expression (p > 0.1), 30% dynamic strain amplitude increased ADAMTS-5 expression by more than two fold (p = 0.012) compared to cytokine treatment alone. Cytokine treatment increased IL-6 mRNA levels (p < 0.0001) but dynamic compression reduced this response to control levels (p = 0.001 for 10% and p < 0.0001 for both 20% and 30% amplitude). Dynamic strain also significantly countered the increase in NF-κB expression caused by cytokines alone (p = 0.027 for 10%, p = 0.02 for 20%, and p = 0.002 for 30%). While cytokine-plus-dynamic compression at 10% or 20% strain increased COX-2 expression by 3–4 fold compared to cytokines-alone (p = 0.01 and p = 0.002, respectively), 30% strain caused a further increase to >40 fold compared to cytokines alone (p < 0.0001). Cytokines increased iNOS mRNA levels by more than 200 fold (p < 0.0001), but 30% strain significantly suppressed this increase in expression (p = 0.001).
Figure 6.
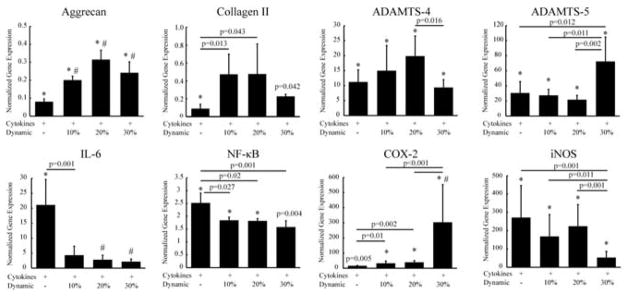
The effects of dynamic compression on bovine chondrocyte gene expression after 48 hours of treatment with exogenous cytokines. For each condition, 6 cartilage disks from the same animal were pooled for mRNA extraction; n = 4 animals. Gene expression levels were normalized to that of the 18S gene and then normalized to the no-cytokine, no-compression control condition which had an expression level = 1. Data are presented as mean ± 95% confidence interval, * = P < 0.001 compared with untreated control; # = P < 0.001 compared with cytokines-alone treatment.
DISCUSSION
Using in vitro models of joint injury, we demonstrated that moderate, intermittent dynamic compression (i.e., 10%–20% strain amplitude) has significant anti-catabolic effects on cartilage homeostasis. Moderate dynamic compression of bovine cartilage rescued cell apoptosis caused by cytokine challenge and upregulated cytokine-suppressed matrix gene expression. In contrast, high compression amplitude (30%) caused severe loss of cell viability and increased matrix degradation, and decreased matrix gene expression and biosynthesis. Consistent with these results, Torzilli[41] reported that load-controlled confined cyclic compression (0.5 Hz) with 0.5 MPa (but not 0.2) peak stress counteracted IL-1α-induced sGAG loss in mature bovine explants. While their loading configuration was different than that of Fig. 1B, their reported inhibitory effect of cyclic loading on sGAG loss is consistent with that demonstrated here for moderate dynamic compression in immature bovine, which sustained a comparable peak stress of 0.55 ± 0.20 MPa at 10% strain amplitude (mean ± 95% CI, 4 animals).
Interestingly, high (30%) dynamic strain resulted in the greatest inhibition of sGAG loss compared to moderate strains in immature cartilage, especially in the presence of injury (Figure 2A&B). However, high dynamic strain caused significant apoptosis (Figure 4C, as high as injurious compression), and loss of cell viability (Figure 5). Such nonviable cells cannot respond to catabolic cytokines and upregulate aggrecanases that cause sGAG loss. Consistent with this interpretation, 30% dynamic strain also suppressed chondrocyte biosynthesis (Figure 2C&D). In contrast, 20% strain inhibited apoptosis (Figure 4C), further suggesting that moderate dynamic compression may transduce anti-apoptotic signals, though the mechano-transduction pathways remain to be elucidated. In addition, the increased abundance in NITEGE neoepitope at 30% strain (Figure 3) indicated elevated aggrecanase activity in the tissue, again contrary to the anti-catabolic effects of moderate dynamic compression. Together, these results lead to our hypothesis that high-magnitude dynamic compression is pro-inflammatory, and the suppression of sGAG loss by 30% strain resulted from load-induced reduction in cell viability, resulting in a slower rate of live-cell-dependent matrix degradation mediated by cytokines.
Preliminary studies have been performed using adult human cartilage to extend the findings from bovine experiments. 30% dynamic strain increased sGAG loss compared to 10% strain, and lower NITEGE abundance was seen at 30% strain compared to 20%(Data not shown). Moderate dynamic at 10% appeared to exert beneficial effects, rather than 20% in immature bovine cartilage. These differences are likely age-related, associated with differences in matrix composition and distribution[42], matrix maturity[19], mechanical properties[43], and cell density[44, 45]. The immature bovine tissue is more vulnerable[46], especially the soft superficial zone, which receives the most local strain during compression[46], likely causing more cell damage at higher strain amplitudes than in human cartilage. Ongoing studies focus on adult human cartilage as additional tissue becomes available. Although immature bovine cartilage may not completely capture the behavior of normal adult cartilage, it is useful to note that chondrocytes in adult osteoarthritic cartilage also have higher metabolic and biosynthetic activity than normal adult cartilage. And importantly, chondral lesions have been reported to be the most common injury to immature human knees (more prevalent than ACL or meniscal injuries)[47].
Certain mechanisms by which dynamic compression may regulate cytokine-induced cartilage degradation and biosynthesis were revealed at the gene transcription level. Consistent with previous reports that moderate dynamic compression is an anabolic stimulus for cartilage matrix biosynthesis[21], we observed that 10% and 20% strain amplitude significantly upregulated aggrecan and type II collagen mRNA levels even in the presence of cytokines. This suggests that the anabolic nature of moderate dynamic compression is preserved in an inflammatory environment. Although moderate dynamic compression did not significantly suppress cytokine-induced upregulation of ADAMTS-4 and -5 genes, western analyses showed strong reduction in aggrecanase activity (Figure 3). These differences between signals at the gene and protein levels may be due to (1) the time-dependence of gene activation, which we evaluated only at the 48-hour time point, and/or (2) the effects of dynamic compression on post-transcriptional processes such as aggrecanase activation by proprotein convertases[48]. Therefore, further studies should examine the effects of dynamic compression at the protein level associated with post-transcriptional regulation of protease activation.
Inflammatory genes cyclo-oxygenase (COX-2) and inducible nitric oxide synthase (iNOS) were activated by cytokines at 48-hour; however, moderate dynamic compression had no inhibitory effects on either gene. Consistent with these results, Chowdhury[30] showed significant inhibition of IL-1β-induced COX-2 and iNOS expression by 15% dynamic compression (1 Hz) at 6 and 12 hours but not 48 hours using chondrocyte-seeded agarose gels, further emphasizing the time-dependence of gene transcription of mechanical signals. Dynamic compression of bovine explants suppressed cytokine-induced upregulation of IL-6 and NF-κB transcription (Figure 6). Interestingly, Agarwal[49] reported a magnitude-dependent mechanism through which cyclic tensile strain transduced signals via the NF-κB pathway in isolated chondrocytes. Lastly, 30% strain significantly increased ADAMTS-5 and COX-2 expression and had no stimulatory effect on type II collagen expression, further strengthening our hypothesis that high-magnitude dynamic compression is pro-inflammatory.
In the present study, we demonstrated the anti-catabolic effects of moderate dynamic compression on injury/TNF + IL-6/sIL-6R-challenged immature bovine and adult human cartilage. Importantly, we discovered that there exists a threshold strain amplitude above which dynamic compression becomes detrimental to cell viability as well as upregulation of inflammatory genes and aggrecanase activity in the remaining viable cells. Together, these results provide evidence to support the concept that appropriate loading-rehabilitation post-joint injury can be beneficial at the cell level, but above threshold dynamic loading may further contribute to loss of cell and tissue function. Further studies exploring the effects of frequency and loading type (e.g., continuous vs. intermittent) are suggested to optimize the beneficial effects of dynamic loading.
Acknowledgments
This work has been supported by NIH Grants AR060331 and AR045779, and NIH Biomechanics Training Grant Fellowship (YL). The funding sources had no involvement in the design, collection, analysis and interpretation of data, nor in the writing and submission of this manuscript.
Footnotes
CONFLICTS OF INTEREST
All authors have no financial interests or personal relationships with other people or organizations that could potentially and inappropriately influence the conduct or reporting of this work.
AUTHOR CONTRIBUTIONS
YL contributed to the conception and design of the study, including collection, analysis, and interpretation of data, drafting and revising of the manuscript. EHF contributed to the design of the study and data interpretation. WY and HH contributed to the collection of experimental data. SC contributed to obtaining and interpretation of data on human tissue. AJG contributed to the conception and design of the study, including obtaining of funding, interpretation of data, and drafting and critical revision of the article for intellectual content. All authors approved the final version of the article. First and last authors take responsibility for the integrity of the work as a whole, from inception to finished article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, et al. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 2.Higuchi H, Shirakura K, Kimura M, Terauchi M, Shinozaki T, Watanabe H, et al. Changes in biochemical parameters after anterior cruciate ligament injury. Int Orthop. 2006;30:43–47. doi: 10.1007/s00264-005-0023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elsaid KA, Fleming BC, Oksendahl HL, Machan JT, Fadale PD, Hulstyn MJ, et al. Decreased lubricin concentrations and markers of joint inflammation in the synovial fluid of patients with anterior cruciate ligament injury. Arthritis Rheum. 2008;58:1707–1715. doi: 10.1002/art.23495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catterall JB, Stabler TV, Flannery CR, Kraus VB. Changes in serum and synovial fluid biomarkers after acute injury (NCT00332254) Arthritis Res Ther. 2010;12:R229. doi: 10.1186/ar3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill CL, Seo GS, Gale D, Totterman S, Gale ME, Felson DT. Cruciate ligament integrity in osteoarthritis of the knee. Arthritis Rheum. 2005;52:794–799. doi: 10.1002/art.20943. [DOI] [PubMed] [Google Scholar]
- 6.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 7.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38:293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Van de Velde SK, Gill TJ, Li G. Evaluation of kinematics of anterior cruciate ligament-deficient knees with use of advanced imaging techniques, three-dimensional modeling techniques, and robotics. J Bone Joint Surg Am. 2009;91 (Suppl 1):108–114. doi: 10.2106/JBJS.H.01382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van de Velde SK, Bingham JT, Hosseini A, Kozanek M, DeFrate LE, Gill TJ, et al. Increased tibiofemoral cartilage contact deformation in patients with anterior cruciate ligament deficiency. Arthritis Rheum. 2009;60:3693–3702. doi: 10.1002/art.24965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosseini A, Van de Velde S, Gill TJ, Li G. Tibiofemoral cartilage contact biomechanics in patients after reconstruction of a ruptured anterior cruciate ligament. J Orthop Res. 2012;30:1781–1788. doi: 10.1002/jor.22122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen CT, Burton-Wurster N, Lust G, Bank RA, Tekoppele JM. Compositional and metabolic changes in damaged cartilage are peak-stress, stress-rate, and loading-duration dependent. J Orthop Res. 1999;17:870–879. doi: 10.1002/jor.1100170612. [DOI] [PubMed] [Google Scholar]
- 13.Kurz B, Jin M, Patwari P, Cheng DM, Lark MW, Grodzinsky AJ. Biosynthetic response and mechanical properties of articular cartilage after injurious compression. J Orthop Res. 2001;19:1140–1146. doi: 10.1016/S0736-0266(01)00033-X. [DOI] [PubMed] [Google Scholar]
- 14.Torzilli PA, Grigiene R, Borrelli J, Jr, Helfet DL. Effect of impact load on articular cartilage: cell metabolism and viability, and matrix water content. J Biomech Eng. 1999;121:433–441. doi: 10.1115/1.2835070. [DOI] [PubMed] [Google Scholar]
- 15.Ewers BJ, Dvoracek-Driksna D, Orth MW, Haut RC. The extent of matrix damage and chondrocyte death in mechanically traumatized articular cartilage explants depends on rate of loading. J Orthop Res. 2001;19:779–784. doi: 10.1016/S0736-0266(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 16.Loening AM, James IE, Levenston ME, Badger AM, Frank EH, Kurz B, et al. Injurious mechanical compression of bovine articular cartilage induces chondrocyte apoptosis. Arch Biochem Biophys. 2000;381:205–212. doi: 10.1006/abbi.2000.1988. [DOI] [PubMed] [Google Scholar]
- 17.D’Lima DD, Hashimoto S, Chen PC, Colwell CW, Jr, Lotz MK. Human chondrocyte apoptosis in response to mechanical injury. Osteoarthritis Cartilage. 2001;9:712–719. doi: 10.1053/joca.2001.0468. [DOI] [PubMed] [Google Scholar]
- 18.Chen CT, Burton-Wurster N, Borden C, Hueffer K, Bloom SE, Lust G. Chondrocyte necrosis and apoptosis in impact damaged articular cartilage. J Orthop Res. 2001;19:703–711. doi: 10.1016/S0736-0266(00)00066-8. [DOI] [PubMed] [Google Scholar]
- 19.Kurz B, Lemke A, Kehn M, Domm C, Patwari P, Frank EH, et al. Influence of tissue maturation and antioxidants on the apoptotic response of articular cartilage after injurious compression. Arthritis Rheum. 2004;50:123–130. doi: 10.1002/art.11438. [DOI] [PubMed] [Google Scholar]
- 20.Sui Y, Lee JH, DiMicco MA, Vanderploeg EJ, Blake SM, Hung HH, et al. Mechanical injury potentiates proteoglycan catabolism induced by interleukin-6 with soluble interleukin-6 receptor and tumor necrosis factor alpha in immature bovine and adult human articular cartilage. Arthritis Rheum. 2009;60:2985–2996. doi: 10.1002/art.24857. [DOI] [PubMed] [Google Scholar]
- 21.Sah RL, Kim YJ, Doong JY, Grodzinsky AJ, Plaas AH, Sandy JD. Biosynthetic response of cartilage explants to dynamic compression. J Orthop Res. 1989;7:619–636. doi: 10.1002/jor.1100070502. [DOI] [PubMed] [Google Scholar]
- 22.Ackermann B, Steinmeyer J. Collagen biosynthesis of mechanically loaded articular cartilage explants. Osteoarthritis Cartilage. 2005;13:906–914. doi: 10.1016/j.joca.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Kim YJ, Sah RL, Grodzinsky AJ, Plaas AH, Sandy JD. Mechanical regulation of cartilage biosynthetic behavior: physical stimuli. Arch Biochem Biophys. 1994;311:1–12. doi: 10.1006/abbi.1994.1201. [DOI] [PubMed] [Google Scholar]
- 24.Kisiday JD, Jin M, DiMicco MA, Kurz B, Grodzinsky AJ. Effects of dynamic compressive loading on chondrocyte biosynthesis in self-assembling peptide scaffolds. J Biomech. 2004;37:595–604. doi: 10.1016/j.jbiomech.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Quinn TM, Grodzinsky AJ, Buschmann MD, Kim YJ, Hunziker EB. Mechanical compression alters proteoglycan deposition and matrix deformation around individual cells in cartilage explants. J Cell Sci. 1998;111 (Pt 5):573–583. doi: 10.1242/jcs.111.5.573. [DOI] [PubMed] [Google Scholar]
- 26.Buschmann MD, Kim YJ, Wong M, Frank E, Hunziker EB, Grodzinsky AJ. Stimulation of aggrecan synthesis in cartilage explants by cyclic loading is localized to regions of high interstitial fluid flow. Arch Biochem Biophys. 1999;366:1–7. doi: 10.1006/abbi.1999.1197. [DOI] [PubMed] [Google Scholar]
- 27.Soulhat J, Buschmann MD, Shirazi-Adl A. A fibril-network-reinforced biphasic model of cartilage in unconfined compression. J Biomech Eng. 1999;121:340–347. doi: 10.1115/1.2798330. [DOI] [PubMed] [Google Scholar]
- 28.Fitzgerald JB, Jin M, Dean D, Wood DJ, Zheng MH, Grodzinsky AJ. Mechanical compression of cartilage explants induces multiple time-dependent gene expression patterns and involves intracellular calcium and cyclic AMP. J Biol Chem. 2004;279:19502–19511. doi: 10.1074/jbc.M400437200. [DOI] [PubMed] [Google Scholar]
- 29.Fitzgerald JB, Jin M, Chai DH, Siparsky P, Fanning P, Grodzinsky AJ. Shear- and compression-induced chondrocyte transcription requires MAPK activation in cartilage explants. J Biol Chem. 2008;283:6735–6743. doi: 10.1074/jbc.M708670200. [DOI] [PubMed] [Google Scholar]
- 30.Chowdhury TT, Arghandawi S, Brand J, Akanji OO, Bader DL, Salter DM, et al. Dynamic compression counteracts IL-1beta induced inducible nitric oxide synthase and cyclo-oxygenase-2 expression in chondrocyte/agarose constructs. Arthritis Res Ther. 2008;10:R35. doi: 10.1186/ar2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilbrink B, Nietfeld JJ, den Otter W, van Roy JL, Bijlsma JW, Huber-Bruning O. Role of TNF alpha, in relation to IL-1 and IL-6 in the proteoglycan turnover of human articular cartilage. Br J Rheumatol. 1991;30:265–271. doi: 10.1093/rheumatology/30.4.265. [DOI] [PubMed] [Google Scholar]
- 32.Frank EH, Jin M, Loening AM, Levenston ME, Grodzinsky AJ. A versatile shear and compression apparatus for mechanical stimulation of tissue culture explants. J Biomech. 2000;33:1523–1527. doi: 10.1016/s0021-9290(00)00100-7. [DOI] [PubMed] [Google Scholar]
- 33.Patwari P, Cook MN, DiMicco MA, Blake SM, James IE, Kumar S, et al. Proteoglycan degradation after injurious compression of bovine and human articular cartilage in vitro: interaction with exogenous cytokines. Arthritis Rheum. 2003;48:1292–1301. doi: 10.1002/art.10892. [DOI] [PubMed] [Google Scholar]
- 34.Lu YC, Evans CH, Grodzinsky AJ. Effects of short-term glucocorticoid treatment on changes in cartilage matrix degradation and chondrocyte gene expression induced by mechanical injury and inflammatory cytokines. Arthritis Res Ther. 2011;13:R142. doi: 10.1186/ar3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farndale RW, Buttle DJ, Barrett AJ. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta. 1986;883:173–177. doi: 10.1016/0304-4165(86)90306-5. [DOI] [PubMed] [Google Scholar]
- 36.Kim YJ, Sah RL, Doong JY, Grodzinsky AJ. Fluorometric assay of DNA in cartilage explants using Hoechst 33258. Anal Biochem. 1988;174:168–176. doi: 10.1016/0003-2697(88)90532-5. [DOI] [PubMed] [Google Scholar]
- 37.Wheeler CA, Jafarzadeh SR, Rocke DM, Grodzinsky AJ. IGF-1 does not moderate the time-dependent transcriptional patterns of key homeostatic genes induced by sustained compression of bovine cartilage. Osteoarthritis Cartilage. 2009;17:944–952. doi: 10.1016/j.joca.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sandy JD, Neame PJ, Boynton RE, Flannery CR. Catabolism of aggrecan in cartilage explants. Identification of a major cleavage site within the interglobular domain. J Biol Chem. 1991;266:8683–8685. [PubMed] [Google Scholar]
- 39.Patwari P, Gao G, Lee JH, Grodzinsky AJ, Sandy JD. Analysis of ADAMTS4 and MT4-MMP indicates that both are involved in aggrecanolysis in interleukin-1-treated bovine cartilage. Osteoarthritis Cartilage. 2005;13:269–277. doi: 10.1016/j.joca.2004.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carames B, Lopez-Armada MJ, Cillero-Pastor B, Lires-Dean M, Vaamonde C, Galdo F, et al. Differential effects of tumor necrosis factor-alpha and interleukin-1beta on cell death in human articular chondrocytes. Osteoarthritis Cartilage. 2008;16:715–722. doi: 10.1016/j.joca.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 41.Torzilli PA, Bhargava M, Park S, Chen CT. Mechanical load inhibits IL-1 induced matrix degradation in articular cartilage. Osteoarthritis Cartilage. 2010;18:97–105. doi: 10.1016/j.joca.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stockwell RA, Scott JE. Distribution of acid glycosaminoglycans in human articular cartilage. Nature. 1967;215:1376–1378. doi: 10.1038/2151376a0. [DOI] [PubMed] [Google Scholar]
- 43.Demarteau O, Pillet L, Inaebnit A, Borens O, Quinn TM. Biomechanical characterization and in vitro mechanical injury of elderly human femoral head cartilage: comparison to adult bovine humeral head cartilage. Osteoarthritis Cartilage. 2006;14:589–596. doi: 10.1016/j.joca.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 44.Jadin KD, Wong BL, Bae WC, Li KW, Williamson AK, Schumacher BL, et al. Depth-varying density and organization of chondrocytes in immature and mature bovine articular cartilage assessed by 3d imaging and analysis. J Histochem Cytochem. 2005;53:1109–1119. doi: 10.1369/jhc.4A6511.2005. [DOI] [PubMed] [Google Scholar]
- 45.Gilmore RS, Palfrey AJ. Chondrocyte distribution in the articular cartilage of human femoral condyles. J Anat. 1988;157:23–31. [PMC free article] [PubMed] [Google Scholar]
- 46.Rolauffs B, Muehleman C, Li J, Kurz B, Kuettner KE, Frank E, et al. Vulnerability of the superficial zone of immature articular cartilage to compressive injury. Arthritis Rheum. 2010;62:3016–3027. doi: 10.1002/art.27610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oeppen RS, Connolly SA, Bencardino JT, Jaramillo D. Acute injury of the articular cartilage and subchondral bone: a common but unrecognized lesion in the immature knee. AJR Am J Roentgenol. 2004;182:111–117. doi: 10.2214/ajr.182.1.1820111. [DOI] [PubMed] [Google Scholar]
- 48.Tortorella MD, Arner EC, Hills R, Gormley J, Fok K, Pegg L, et al. ADAMTS-4 (aggrecanase-1): N-terminal activation mechanisms. Arch Biochem Biophys. 2005;444:34–44. doi: 10.1016/j.abb.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 49.Agarwal S, Deschner J, Long P, Verma A, Hofman C, Evans CH, et al. Role of NF-kappaB transcription factors in antiinflammatory and proinflammatory actions of mechanical signals. Arthritis Rheum. 2004;50:3541–3548. doi: 10.1002/art.20601. [DOI] [PMC free article] [PubMed] [Google Scholar]