Abstract
Many new parasitic infections have emerged in Korea, with >35 new species appearing since the 1980s. Among them, Capillaria species are unique for contributing to morbidity in many countries as well as in Korea. Since the first reported case of a 41-year-old male patient diagnosed with intestinal capillariasis in 1991, a total of six cases have been reported thus far. In this case report, we present another imported case of intestinal capillariasis in Korea, in which a 42-year-old male patient presented with intractable diarrhea and weight loss. The diagnosis was confirmed by biopsy of the ileum. The pathognomonic radiographic presentation of a ribbon-like appearance in a small bowel series was crucial in raising an early suspicion of capillariasis and in deciding to perform diagnostic biopsy.
Keywords: Capillaria; Capillaria philippinensis; Intestine, small; Colonoscopy; Albendazole
INTRODUCTION
Parasitic diseases in Korea have remarkably decreased in prevalence since the 1980s, partly owing to the introduction of several national health care programs.1 However, many new parasitic infections have hence emerged, and >35 parasitic species have emerged and re-emerged since 1980.1
Intestinal capillariasis is caused by Capillaria philippinensis and was first reported in 1968 as an autopsy case in the Philippines.2 Other Asian countries have reported sporadic cases since then, followed by Middle Eastern countries and even South America. The first Korean case of intestinal capillariasis was reported in 1993 in a 41-year-old male patient.3 Thereafter, several more cases have been diagnosed in Korea owing to increased awareness and vigilance in detection efforts.3-7 Among them were three indigenous cases, in which no history of travelling abroad were noted, and three imported cases, in which a history of travel to endemic areas was established.3-7
In this case report, we present another imported case of intestinal capillariasis in Korea that was confirmed only through an endoscopic biopsy of the ileum in a 42-year-old male patient who had intractable diarrhea and weight loss. The pathognomonic radiographic findings of a small bowel series was crucial in raising the suspicion of intestinal capillariasis, eventually leading to the successful diagnosis through endoscopic biopsy. The patient was successfully treated after a course of albendazole.
CASE REPORT
In June 2004, a 42-year-old male patient was admitted to our hospital with a nearly 2-year history of intractable diarrhea. He had been residing in the Philippines for 9 years before his visit. He was a fisherman, and he enjoyed eating raw fish. He experienced watery diarrhea several times daily during the last 2 years, with no significant impact on his daily life. However, the diarrhea unexpectedly worsened approximately 2 months before presentation, resulting in a weight loss of 10 kg. He was thus admitted to a hospital in the Philippines, but no improvement was observed. He subsequently returned to Korea for evaluation and treatment several days before admission to our hospital.
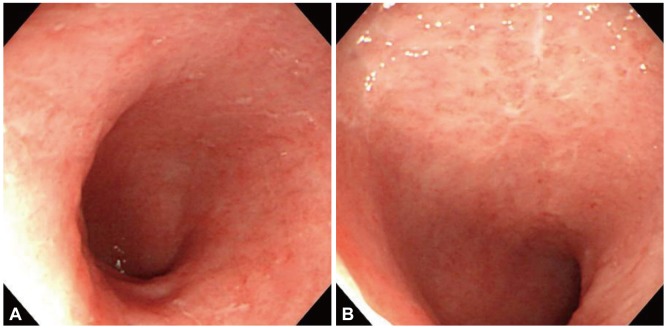
On presentation, he complained of symptoms including severe diarrhea, weight loss, and abdominal pain. Physical examination revealed stable vital signs with normal blood pressure and heart rate. Routine laboratory tests revealed leukocytosis with a white blood cell count of 16,550/mm3 but without eosinophilia, hyponatremia (sodium level, 128.5 mmol/L), hypokalemia (potassium level, 3.11 mmol/L), and hypoalbuminemia (albumin level, 1.2 g/dL). Further laboratory studies and colonoscopy were performed to rule out any medical conditions leading to chronic diarrhea. Results of the stool examination for parasites, acquired immune deficiency syndrome test, and antineutrophil cytoplasmic antibody test were negative. Thyroid function test showed a free thyroxine level of 1.27 ng/dL, a triiodothyronine level of 80.01 ng/dL, and a thyroid-stimulating hormone level of 3.94 µIU/mL, all within the reference range. Colonoscopy revealed no significant abnormal findings. Abdominopelvic computed tomography (AP CT) showed diffuse wall thickening of the small bowel with mesenteric lymph node enlargement. This was followed by a small bowel series to verify the presence of the lesion found in AP CT. A plain radiograph of the small bowel revealed straightening of the lumen, known as a ribbon-like appearance in the ileum, without abnormal disturbance of passage (Fig. 1). Although the folds of the jejunum were relatively spared, those and the villi of the ileum were obliterated, along with the luminal straightening. A second colonoscopy session was planned for the purpose of biopsy to detect mucosal lesions in the ileum that may be indicative of the cause of the diarrhea (Fig. 2). Although the second colonoscopy also failed to identify any striking anomaly in the mucosae of the terminal ileum and colon, endoscopic biopsy at the distal ileum was performed because of the suspicion of several diseases limited to the small intestine; this revealed chronic inflammation with mucosal atrophy, eosinophilic infiltration, and the presence of parasitic worms in the mucosa, consistent with intestinal capillariasis (Fig. 3). The diagnosis of intestinal capillariasis was confirmed, and the patient received 400 mg of albendazole daily for the next 4 weeks. At the end of 4 weeks, all of his symptoms abated, and he showed an increase in body weight from 48 to 58 kg. While stool examination, probably the simplest method of evaluating parasitic infestation, was performed as part of the initial examination, neither the larvae nor the ova of the parasite were observed. Thus, after the confirmation of C. philippinensis infection through a pathologic study, stool examination was repeated once before albendazole treatment and three times after medication to further validate the finding. Nevertheless, the result of stool examination was negative in all five occasions.
Fig. 1.
Abdominal radiograph. Small bowel series performed with barium illustrates marked luminal narrowing and effacement of folds producing a ribbon-like appearance of the ileum. However, even the involved ileum does not show demonstrable luminal narrowing or passage disturbance, and the folds are well preserved in the jejunum.
Fig. 2.
(A, B) Endoscopic images of the distal ileum. Scattered erosive mucosal lesions with loss of villi and several shallow erosions with whitish exudates were observed.
Fig. 3.
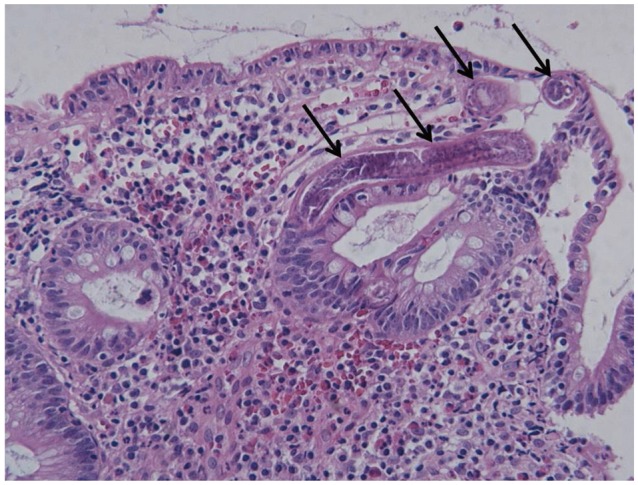
Photomicrograph of the biopsy specimen from the distal ileum (H&E stain, ×200). Biopsy specimens of the ileum show atrophic changes of the intestinal villi, infiltration of plasma cells and eosinophils, and several sections of worms invading the mucosa (arrows).
DISCUSSION
Although Capillaria species had primarily been associated with fowl, C. philippinensis infections in humans have been consistently reported in other Asian countries as well as in South America since the 1964 human infestation case in the Philippines.8-14 A notable feature of this infection is that the larvae may reproduce in a shortened autoinfection cycle, which could lead to high parasitic loads.15 Because of these autoinfections, C. philippinensis infection can easily progress to intestinal capillariasis without appropriate treatment. In humans, C. philippinensis can be acquired through eating raw or insufficiently cooked infected fish. Freshwater fishes and fisheating birds are deemed natural hosts of C. philippinensis.15
Most known cases have occurred in the Philippines and Thailand. Sporadic cases, however, have been reported from many other Asian countries.10-13 The existence of C. philippinensis in Korea was not proven until the cases reported in the 1990s; however, several studies had suggested that C. philippinensis may have been transported from the Philippines or other Asian countries to Korea by migrating birds.3,16
Cases reported in the Philippines and Thailand suggested that men tend to be more easily infected than women. In the six cases reported in Korea to date, all of the patients were men. The mean age of the six patients was 44.5 years; the patient in this present case was also a 42-year-old man.3-7 Further details on the characteristics of the patient are provided in Table 1.3-7
Table 1.
Characteristics of the Patients Diagnosed with Intestinal Capillariasis in Korea
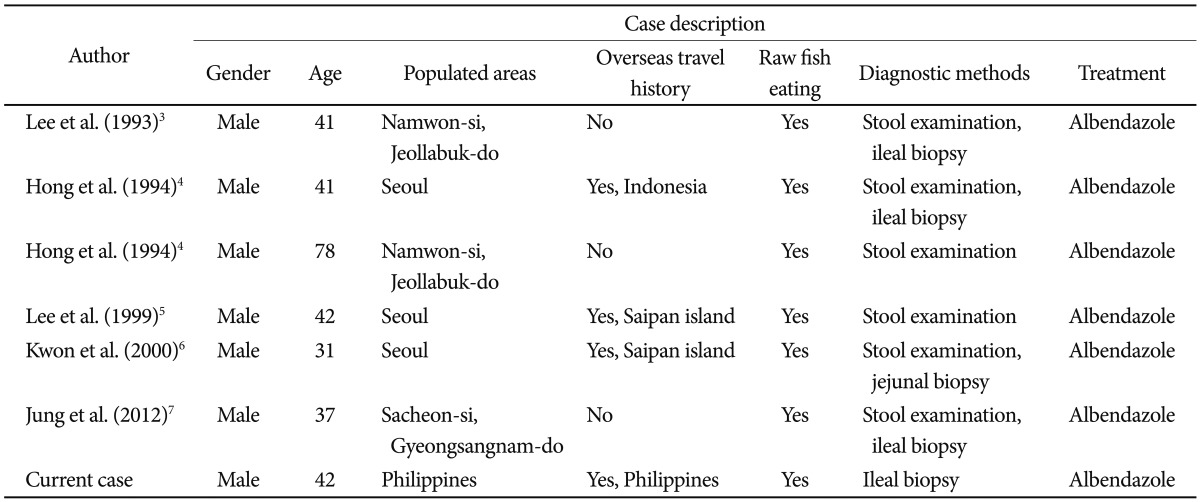
The diagnosis of intestinal capillariasis is based on the detection of ova, larvae, and/or adult worms in the feces. However, it is difficult to identify larvae or eggs as belonging to C. philippinensis because of their similarity in appearance to other parasites and the nonconstant shedding in the feces.12,15,17 These characteristics have often made intestinal capillariasis difficult to diagnose on the basis of stool examination, arguably the simplest diagnostic tool. More than 10-stool examinations were performed before diagnosis in one case reported in China, and, as in the present report, the parasite's ova or larvae may not be isolated after five repetitions of stool examination.13
Although the diagnosis may also be obtained from endoscopic biopsy, the lesion is difficult to access with an endoscope because infestation by C. philippinensis occurs mostly in the jejunum. Nevertheless, stool examination or jejunal biopsy often allows diagnosis of intestinal capillariasis. However, several case studies have reported on its diagnosis through ileal biopsies, as was the case in the present study, when either surgical resection was not performed or when an endoscopic approach proved difficult.18 In the case presented here, unlike in previously reported cases in Korea, larvae or ova were never conclusively detected in five stool examinations before and after albendazole administration. However, a small bowel series performed to verify the small bowel lesion found on CT demonstrated the pathognomonic ribbon-like appearance in the ileum, providing a sufficient level of suspicion to perform endoscopic biopsy from the distal ileum despite the lack of an obvious mucosal lesion. It should be noted that while the parasite causing intestinal capillariasis is known to be present mainly in the jejunum, the small bowel series performed in the present case revealed a lesion localized to the ileum rather than to the jejunum. However, based on the clinical course of the patient, it is thought likely that the already elevated parasitic load has allowed for the involvement of the intestinal tract other than the jejunum, and that the ileum, with its relatively smaller and thinner circular folds and villi, soon showed luminal straightening, resulting in the characteristic ribbon-like appearance.
Although its nonconstant shedding in stool and the similarity to other parasites in terms of morphology make C. philippinensis difficult to diagnose by stool examinations, stool examination is still the least invasive diagnostic method of intestinal capillariasis. However, as shown in the present case, stool examination alone is often insufficient to diagnose intestinal capillariasis. Given the increase in overseas travel to Southeast Asia by Koreans, the relevant indigenous cases, and the dire clinical consequences including death, aggressive efforts to screen and diagnose intestinal capillariasis in patients with intractable diarrhea and weight loss warrant serious consideration.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Chai JY. Emerging parasitic diseases in Korea. J Korean Med Assoc. 2007;50:946–958. [Google Scholar]
- 2.Chitwood MB, Valesquez C, Salazar NG. Capillaria philippinensis sp. n. (Nematoda: Trichinellida), from the intestine of man in the Philippines. J Parasitol. 1968;54:368–371. [PubMed] [Google Scholar]
- 3.Lee SH, Hong ST, Chai JY, et al. A case of intestinal capillariasis in the Republic of Korea. Am J Trop Med Hyg. 1993;48:542–546. doi: 10.4269/ajtmh.1993.48.542. [DOI] [PubMed] [Google Scholar]
- 4.Hong ST, Kim YT, Choe G, et al. Two cases of intestinal capillariasis in Korea. Korean J Parasitol. 1994;32:43–48. doi: 10.3347/kjp.1994.32.1.43. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Rhee PL, Lee JH, et al. A case of intestinal capillariasis: fourth case report in Korea. Korean J Gastroenterol. 1999;34:542–546. [Google Scholar]
- 6.Kwon Y, Jung HY, Ha HK, Lee I. An imported case of intestinal capillariasis presenting as protein-losing enteropathy. Korean J Pathol. 2000;34:235–238. [Google Scholar]
- 7.Jung WT, Kim HJ, Min HJ, et al. An indigenous case of intestinal capillariasis with protein-losing enteropathy in Korea. Korean J Parasitol. 2012;50:333–337. doi: 10.3347/kjp.2012.50.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bickford AA, Gaafar SM. Multiple capillariasis in game-farm pheasants. Avian Dis. 1966;10:428–437. [PubMed] [Google Scholar]
- 9.Jortner BS, Helmboldt CF, Pirozok RP. Small intestinal histopathology of spontaneous capillariasis in the domestic fowl. Avian Dis. 1967;11:154–169. [PubMed] [Google Scholar]
- 10.Hwang KP. Human intestinal capillariasis (Capillaria philippinensis) in Taiwan. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1998;39:82–85. [PubMed] [Google Scholar]
- 11.Ahmed L, el-Dib NA, el-Boraey Y, Ibrahim M. Capillaria philippinensis: an emerging parasite causing severe diarrhoea in Egypt. J Egypt Soc Parasitol. 1999;29:483–493. [PubMed] [Google Scholar]
- 12.Saichua P, Nithikathkul C, Kaewpitoon N. Human intestinal capillariasis in Thailand. World J Gastroenterol. 2008;14:506–510. doi: 10.3748/wjg.14.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fan Z, Huang Y, Qian S, et al. Serious diarrhea with weight loss caused by Capillaria philippinensis acquired in China: a case report. BMC Res Notes. 2012;5:554. doi: 10.1186/1756-0500-5-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dronda F, Chaves F, Sanz A, Lopez-Velez R. Human intestinal capillariasis in an area of nonendemicity: case report and review. Clin Infect Dis. 1993;17:909–912. doi: 10.1093/clinids/17.5.909. [DOI] [PubMed] [Google Scholar]
- 15.Cross JH. Intestinal capillariasis. Clin Microbiol Rev. 1992;5:120–129. doi: 10.1128/cmr.5.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cross JH, Basaca-Sevilla V. Intestinal capillariasis. Prog Clin Parasitol. 1989;1:105–119. [PubMed] [Google Scholar]
- 17.Bair MJ, Hwang KP, Wang TE, et al. Clinical features of human intestinal capillariasis in Taiwan. World J Gastroenterol. 2004;10:2391–2393. doi: 10.3748/wjg.v10.i16.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu LH, Lin MR, Choi WM, et al. Human intestinal capillariasis (Capillaria philippinensis) in Taiwan. Am J Trop Med Hyg. 2006;74:810–813. [PubMed] [Google Scholar]