Abstract
Objective
To enumerate global health training activities in U.S. obstetrics and gynecology residency programs, and to examine the worldwide distribution of programmatic activity relative to the maternal and perinatal disease burden.
Methods
Using a systematic, Web-based protocol, we searched for global health training opportunities at all U.S. obstetrics and gynecology residency programs. Country-level data on disability-adjusted life years due to maternal and perinatal conditions were obtained from the Global Burden of Disease study. We calculated Spearman’s rank correlation coefficients to estimate the cross-country association between programmatic activity and disease burden.
Results
Of the 243 accredited U.S. obstetrics and gynecology residency programs, we identified 41 (17%) with one of several possible predefined categories of programmatic activity. Thirty-three residency programs offered their residents opportunities to participate in one or more elective-based rotations, eight offered extended field-based training, and 18 offered research activities. A total of 128 programmatic activities were dispersed across 64 different countries. At the country level, the number of programmatic activities had a statistically significant association with the total disease burden due to maternal (Spearman’s ρ=0.37; 95% confidence interval [CI], 0.14-0.57) and perinatal conditions (ρ=0.34; 95% CI, 0.10-0.54) but not gynecologic cancers (ρ=−0.24; 95% CI, −0.46 to 0.01).
Conclusions
There are few global health training opportunities for U.S. obstetrics and gynecology residents. These activities are disproportionately distributed among countries with greater burdens of disease.
INTRODUCTION
Global health training is increasing in prominence in U.S. pre-medical education [1] and both undergraduate [2] and graduate [3, 4] medical education. The availability of global health training opportunities has been shown to affect medical students’ selections in the U.S. National Resident Matching Program [5-8] and their subsequent decisions to seek employment in underserved communities or pursue graduate education in public health [9, 10]. While residency programs have, in general, responded to this increased demand by expanding global health training opportunities for residents as a whole [11], the extent to which such expansions have occurred specifically in the field of obstetrics and gynecology is unclear.
Global health training in obstetrics and gynecology residency programs is of substantive public health concern, as maternal conditions are a leading cause of death among women of reproductive age worldwide [12]. Moreover, cesarean sections are among the most common surgical procedures performed in low-resource settings [13, 14], and the rates of obstetrical complications in low-resource countries exceed those in other parts of the world [15]. A major bottleneck to improving surgical care in general is the lack of adequately trained providers [16-18]. Overall, in many low-resource countries, access to essential obstetrical and gynecological services remains limited [19].
In July 2012, the Executive Board of the American College of Obstetricians and Gynecologists issued a Statement of Policy supporting women’s health and rights globally. However, to date, the literature has only contained case studies of global health training programs for obstetrics and gynecology residents at specific institutions (e.g., the Global Health Residency Track in the Department of Obstetrics, Gynecology, and Reproductive Sciences at Mount Sinai School of Medicine [20]). The magnitude and distribution of global health training in obstetrics and gynecology have not been systematically assessed. We undertook this study to quantify the extent of global health training in U.S. obstetrics and gynecology residency programs. A secondary aim was to compare, at the country level, the distribution of programmatic activity with the maternal and perinatal disease burden.
METHODS
Characterizing global health-related programmatic activities
We implemented a standardized search protocol to systematically identify and characterize global health-related programmatic activities in U.S. obstetrics and gynecology residency programs. First, we identified all U.S. obstetrics and gynecology residency programs (numeric program code 220) accredited by the Accreditation Council for Graduate Medical Education (ACGME) for the academic year 2010-2011. Using this nationwide sampling frame, one of the study authors (VBK) and two research assistants examined the official residency program web site, if available, and search results from systematic Google queries. We chose to use a web-based search instead of direct surveys of program directors or residents, because anonymous surveys of global health training activities have often yielded little response from prospective participants (either program directors or residents), and previously published journal articles have been based on data from surveys with response rates as low as 25 percent [8, 21-23]. The Google queries were conducted January-June 2011 and, using the “Find pages with all these words” function, searched for the following: [ACGME-listed program name] global health obstetrics gynecology residency. The first page of 20 search results, as well as any linked web pages with the keywords “enrichment,” “global health,” “health inequity,” “international health,” “research,” “rural,” or “vulnerable populations,” were scanned for relevant data. Data linking the ACGME-accredited residency program to global or international health-related programmatic activities were abstracted from any of these web pages. A program was coded as not having any global health training if neither the official residency program web site nor the Google queries uncovered any relevant data.
We categorized global health programs into four non-mutually exclusive categories of programmatic activity. “Electives” were defined as clinical or educational activities of less than six weeks’ duration. Engagements lasting six weeks or more, with or without designated didactic study in global health, were categorized as “extended field training.” Any activities involving human subjects research (i.e., interaction with living persons and/or the use of identifiable private information) were categorized as “research,” regardless of duration. If a particular global health-related programmatic activity did not fit one of these three categories or could not be characterized (e.g., due to lack of information), it was listed as “other.” We summated the total count of programmatic activities across residency programs and across countries. For example, an obstetrics and gynecology residency program that offered electives in six countries, research in one country, and extended field training in one country was coded as offering a total of eight programmatic activities. Programs with longitudinal curricula and established ties to partner institutions were then described in more detail.
This study did not involve human subjects research and received an exempt determination from the Partners Human Research Committee.
Statistical analysis
We sought to estimate the cross-country association between programmatic activity and disease burden. To measure disease burden, we abstracted data on disability-adjusted life years (DALYs) due to maternal and perinatal conditions and gynecologic cancers for each country with any programmatic activity from the Global Burden of Disease study [24]. For this analysis we adopted the same general categorizations used in the Global Burden of Disease study: “maternal conditions” included maternal hemorrhage, maternal sepsis, hypertensive disorders of pregnancy, obstructed labor, and abortion; “perinatal conditions” included prematurity and low birth weight, birth asphyxia and birth trauma, and neonatal infections and other conditions; and “gynecologic cancers” included cervical, uterine, and ovarian cancer. We calculated Spearman’s rank correlation coefficients and their 95% confidence intervals to estimate the association between programmatic activity and disease burden. Scatterplots were used to display this information graphically. For graphical visualization, in order to determine whether the best fit to the line was linear, quadratic, or cubic, we fitted ordinary least squares regression models to the data, using Huber-White standard errors to ensure that the estimates were robust to distributional assumptions. The dependent variable was specified as the number of programs, and the explanatory variable specified as the burden of disease per 100,000 DALYs. We sequentially added quadratic or cubic terms to the regression models, assessed their incremental contributions to the models using Wald-type F-tests, and selected a quadratic or cubic fit line based on these findings. All statistical analyses were conducted using the Stata/MP software package (version 12.0, StataCorp LP, College Station, Tex.).
RESULTS
From among the 243 ACGME-accredited obstetrics and gynecology residency programs in the U.S., we identified 41 (17%) residency programs that provided details of their global health training opportunities online. These programs offered a total of 69 global health-related programmatic activities. Electives were by far the most prevalent type of programmatic activity, offered by 33 programs. Another 18 residency programs offered research opportunities, while only eight offered extended field-based training. Ten residency programs offered global health-related programmatic activities that did not fall into one of the three categories or could not otherwise be classified. Selected programs’ global health activities are described in more detail in Table 1.
Table 1.
Global Health Programmatic Activities in U.S. Obstetrics and Gynecology Residency Programs with Established Partner Sites
| Program Name | Description |
|---|---|
| Beth Israel Deaconess Medical Center Program |
The integrated Global and Community Health program provides a longitudinal curriculum, mentorship, and networking for obstetrics and gynecology residents. They may engage in global health activities at department-specific partner sites or at institution-wide partner sites. Residents have 5 weeks of dedicated elective time in each of PGY2 and 3. Departmental funding is available to support either clinical or research activities, with the exact amounts determined on an individual basis. |
| Brown University (Women and Infants Hospital of Rhode Island) Program |
Obstetrics and gynecology residents receive a $1,000 stipend to help defray research expenses, but other travel and basic living expenses are borne by individual residents. They may also apply, along with residents in the other clinical programs, for scholarships up to $3,500 from the Interdisciplinary Framework in Global Health, a program of Brown University’s Global Health Initiative. There are 2 weeks of dedicative elective time in PGY2 and 6.5 weeks in PGY3. |
| Brigham and Women’s Hospital (BWH) /Massachusetts General Hospital (MGH) Program |
Travel funding is supported by a private donation to the program. Obstetrics and gynecology residents are eligible, along with other BWH and/or MGH residents, to apply for other internal travel grants that are awarded on a competitive basis, including the $2,000 Global and Humanitarian Health Center of Expertise Travel Grant and the $2,000 MGH Center for Global Health Travel Award. Residents have 5 weeks of dedicated elective time in PGY3. |
| Case Western Reserve University/University Hospitals Case Medical Center Program |
The Women and Newborns -- Didactic, Outreach, Opportunities and Research (WONDOOR) Program provides a 30-month longitudinal curriculum, mentorship, and networking for residents. There are 5-6 weeks of dedicated elective time in each of PGY3 and 4. |
| Emory University Program | The Emory Global Health Residency Scholars Program provides a longitudinal curriculum, mentorship, and networking for Emory residents in internal medicine, obstetrics and gynecology, pathology, pediatrics, radiology, and surgery. Obstetrics and gynecology residents have 4 weeks of dedicated elective time in PGY4. The department has established a Gynecology-Obstetrics Global Health Rotation Fund to support resident participation in global health activities. |
| Indiana University (IU) School of Medicine Program |
The IU Interdepartmental Residency Track in Global Health provides a longitudinal curriculum, mentorship, and networking for IU residents in family medicine, internal medicine, medicine/pediatrics, obstetrics and gynecology, pediatrics, and general surgery. Obstetrics and gynecology residents have 4-5 weeks of dedicated elective time during PGY2 to conduct a needs assessment, followed by 8-10 weeks of dedicated elective time during either PGY3 or 4. Departmental funding is available. |
| Kaiser Permanente Medical Group |
The Kaiser Permanente (KP) Global Health Program provides residents in the 3 Northern California Residency Programs with funding for global health activities. Obstetrics and gynecology residents in the KP-Oakland Program have 4 weeks of dedicated time in each of the postgraduate years (PGY) 3 and 4. KP- San Francisco provides 8 weeks of dedicated time in PGY2 and 4 weeks in PGY3, while KP-Santa Clara provides 8 weeks of dedicated time in PGY3. |
| Mayo Clinic Program | Residents from all three sites (Arizona, Florida, and Minnesota) in the Mayo School of Graduate Medical Education are eligible to apply to join the Mayo International Health Program. Financial stipends of up to $2,500 are given to help defray travel and basic living expenses. Obstetrics and gynecology residents have 1 block of dedicated elective time in PGY3. |
| Michigan State University (MSU) Program |
The Global Reproductive Health Training Program provides bilateral exchange between obstetrics and gynecology residents at the MSU College of Human Medicine-affiliated training programs (Grand Rapids Medical Education Partners, Hurley Medical Center, and Sparrow Hospital) and at the University of Costa Rica. All expenses are borne by the participating resident. Contingent on approval, residents from the MSU affiliated programs spend 4 weeks at the partner site. |
| Mount Sinai School of Medicine Program |
Although obstetrics and gynecology residents cannot participate in the Mount Sinai Global Health Residency Track (which is open to residents in emergency medicine, internal medicine, pediatrics, and psychiatry), the Department of Obstetrics, Gynecology, and Reproductive Sciences offers its own global health resident track. The program provides a preparatory curriculum in global women’s health and financial stipend of $1,500 to help defray travel and basic living expenses. Residents have 6-8 weeks of dedicated elective time in PGY3. |
| New York University (NYU) School of Medicine Program |
The NYU Division of Global Women’s Health provides a formal curriculum for residents planning to engage in global health activities. Departmental funding is available to cover the costs of travel. Residents have 4 weeks of dedicated elective time in PGY3 and 4. |
| University of California at San Francisco (UCSF) Program |
Formerly resident-driven with program director approval, proposed electives now require an on-site faculty mentor and a formal agreement with the host institution. There are 4 weeks of dedicated elective time in each of PGY2 and 4. Funding for travel and lodging is provided for the PGY3 rotation in Uganda. Residents are encouraged to apply to join the UCSF Global Health Sciences (GHS) Clinical Scholars Program, which provides a longitudinal curriculum, mentorship, and networking for residents across the UCSF clinical training programs. To help defray travel and research costs, GHS Clinical Scholars can apply for grants of up to $3,000 that are awarded on the basis of a competitive internal review by the Eustace-Kwan Family Foundation. |
| University of Michigan Program |
Global health activities for all University of Michigan residents are facilitated through the Global Research, Education, and Collaboration in Health (REACH) office. The department of obstetrics and gynecology subsidizes travel, expenses, and research projects at established partner sites. Residents have 8 weeks of dedicated elective time in PGY3. |
| University of North Carolina (UNC) Hospitals Program |
Global health activities for all UNC residents are coordinated through the UNC Office of International Activities (OIA). To help defray travel and/or research costs, UNC residents from all clinical specialties can apply for grants of up to $2,000 that are awarded on a biannual funding cycle through the OIA. Additional funding to help defray the costs of travel, insurance, and basic living expenses is available through the Dr. Charles A. Sanders/Project HOPE International Residency Scholarship Program For North Carolina Medical Residents, which is open to all UNC residents (as well as residents at the other three North Carolina medical schools) on a competitive basis. Obstetrics and gynecology residents have the option of 4 weeks of dedicated elective time in each of PGY3 and 4. |
| University of Pennsylvania Program |
The Botswana-UPenn Partnership provides up to $2,500 to defray travel and housing costs for 2 obstetrics and gynecology residents per year. Residents have 4 weeks of dedicated elective time in PGY3. |
| University of Pittsburgh Medical Center Medical Education Program |
The Global Health Program in Reproductive Sciences provides a longitudinal curriculum, mentorship, and networking for obstetrics and gynecology residents. The costs of travel, vaccinations, and anti-malarial medications are covered. Residents can also participate in the work of Basic Health International, a non- profit organization focused on global cervical cancer screening. There is one block of dedicated elective time in PGY3. |
| University of Washington (UW) Program |
The UW Women’s Health International Program provides a longitudinal curriculum, mentorship, and networking for obstetrics and gynecology residents. Participating residents are also encouraged to apply for the UW Integrated Residency Global Health Leadership Course. Residents have 4 weeks of dedicated elective time in PGY3. |
PGY2, postgraduate year 2; PGY3, postgraduate year 3; PGY4, postgraduate year 4.
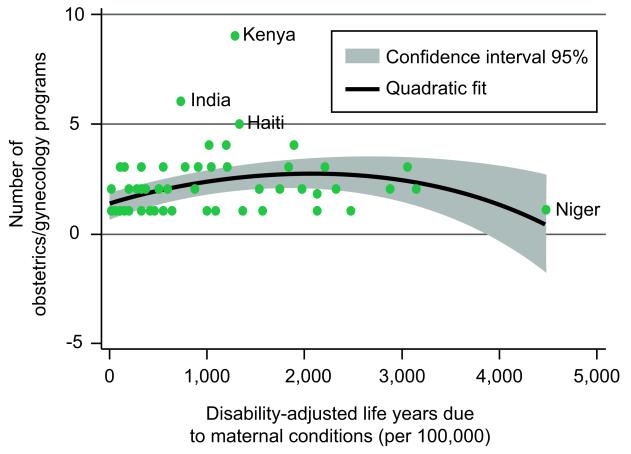
There were a total of 128 sites of programmatic activity dispersed across 64 different countries, indicating that residency programs typically offered a given activity at multiple sites. The density of programmatic activity had a statistically significant association with the country-level burden of disease due to maternal conditions (Spearman’s ρ=0.37; 95% confidence interval [CI], 0.14-0.57) (Figure 1) and perinatal conditions (ρ=0.34; 95% CI, 0.10-0.54). The regression analyses suggested a quadratic fit modeled the data best, with the intensity of programmatic activity increasing with disease burden at the lower end of the scale and then decreasing with disease burden at the upper end of the scale. The cross-country association between programmatic activity and gynecologic cancers was negative but not statistically significant (ρ=−0.24; 95% CI, −0.46 to 0.01). When we examined the correlations for the different types of gynecologic cancers separately, we observed a negative and statistically significant association between programmatic activity and uterine (ρ=−0.48; 95% CI, −0.65 to −0.27) and ovarian (ρ=−0.26; 95% CI, −0.48 to −0.01) cancers but a null association with cervical cancers (ρ=−0.02; 95% CI, −0.27 to 0.23).
Figure 1.
Association between country-level programmatic activity and disease burden due to maternal conditions
DISCUSSION
In this systematic enumeration of global health training across all U.S. obstetrics and gynecology residency programs, we identified only 41 residency programs that described their global health-related training opportunities online. The cross-country associations between the intensity of programmatic activity and maternal and perinatal disease burden were statistically significant but relatively small in magnitude, suggesting that training opportunities appear to be distributed according to the global burden of maternal and perinatal conditions. Our findings have substantive implications for U.S. graduate obstetrics and gynecology education, both in terms of quantifying the relatively low rates of global health training and identifying the potential for improved programming in the future.
Relative to the fields of internal medicine [25] and pediatrics [8, 21], we found fewer U.S. obstetrics and gynecology residency programs with global health training opportunities. The Residency Review Committee (RRC) for Obstetrics and Gynecology currently permits international experiences to count towards graduation and does not specifically exclude cases obtained during these experiences from counting towards ACGME requirements. Given these favorable allowances in obstetrics and gynecology, the greater prevalence of global health training opportunities in other fields may be due to the intensive service requirements of obstetrics and gynecology residency programs, which are also smaller in class size compared to other specialties. Call-free time is rare. For example, unless a resident has elective time dedicated for an overseas elective in which she or he is not a member of the overnight call pool, any clinical duties missed must be covered by other residents in the program. Similar considerations have been described as hampering the expansion of global health training opportunities in U.S. graduate surgical education [22, 26], despite active resident interest [27, 28].
Among the programs we identified as having established relationships with international partner institutions, none provided funding for trainees from partner institutions to access learning opportunities in the U.S. This disparity is consistent with the review of general surgery global health residency programs by Jayaraman et al. [22], in which few programs offered faculty or residents from partner institutions to travel to the U.S. These asymmetries are likely driven not only by funding constraints (e.g., the extent to which U.S. institutions are willing or able to provide funding for trainees from partner institutions to access learning opportunities in the U.S.) but also by regulatory constraints (e.g., licensure requirements that limit the extent to which foreign medical graduates’ are permitted to engage in clinical work in the U.S.). Different programs have adopted different models to address these issues. The Michigan State University Program hosts residents from its partner sites in Costa Rica, but all costs are borne solely by participating residents -- suggesting important limitations in the extent to which a similar model could be implemented with partner institutions in sub-Saharan African countries where the per capita gross domestic product is typically lower by an order of magnitude. The University of Toronto Department of Obstetrics and Gynecology -- excluded from this review, along with other residency programs not based in the U.S. -- hosts trainees from Moi University, Kenya as part of the Academic Model Providing Access to Healthcare (AMPATH) consortium led by Indiana University. Moving forward, we believe the continued gaps in the learning experiences of trainees from the U.S. vs. those from partner institutions should be addressed in the development of new obstetrics and gynecology global health residency programs.
The relative lack of global health training among U.S. obstetrics and gynecology residency programs that we identified in our study suggests lost opportunities from multiple vantage points [27, 29]. U.S. residents lose critical opportunities to increase their mastery of ACGME core competencies in a different setting. The disparities in resources across various global settings offers U.S. residents the opportunity to broaden and deepen their mastery of core competencies (patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice) in their graduate surgical education, as has been described first-hand [30]. As the variety and volume of diseases vary worldwide, so does the availability of technology and thus the need for residents trained in highly technology-driven settings to rely on their basic clinical and leadership skills to obtain information and communicate effectively. The perspectives of other stakeholders are relevant as well. Faculty members lose opportunities to engage in collaborative research and/or sharing of educational resources. U.S. institutions lose ground in recruiting trainees who are attracted by opportunities for cross-cultural interactions and career development [5-8]. Underserved regions of the U.S. lose access to new physicians whose decisions to choose generalist- or public service-oriented careers or to practice in underserved communities could have been favorably influenced by global health-related experiences during their training [5, 9, 10]. Finally, international partner institutions lose opportunities to provide learning experiences -- not only locally but also at institutions in the U.S. that are widely perceived to be among the most prestigious centers of higher education worldwide -- that engage the minds of their best and the brightest and that potentially help to mitigate some of the adverse effects of “brain drain” to other countries [31]. A renewed focus on innovative mechanisms to expand the scope and reach of obstetrics and gynecology global health residency programs is an important area for future educational and operational research.
Our analysis found a statistically significant cross-country association between the intensity of programmatic activity and the burden of maternal and perinatal conditions. However, we observed a negative but non-statistically significant association for gynecologic cancers, a trend that appeared to be driven principally by negative associations between programmatic activity and the burden of uterine and ovarian cancers. These inconsistent findings are likely due to several factors. First, in our experience, myriad factors influence program placement in low-resource settings, including the availability of funding, identification of partner institutions, or both, and these may bear little to no relation to the country-level burden of disease for any particular condition. Second, the greater infrastructure required to provide effective care for gynecologic malignancies compared to benign obstetrics and gynecology (such as the more involved surgeries and the need for radiotherapy, chemotherapy, and supportive care for medically complex patients -- potentially addressable through emerging care delivery models [32]) may pose a barrier to involvement by U.S. trainees on a short-term, skill-limited basis. Third, we could not rule out unobserved confounding. For example, low-resource countries are known to have a lower burden of ovarian and uterine cancers [33]. If programmatic activities are primarily being directed to low-resource countries (i.e., irrespective of their burden of ovarian and uterine cancer), this could produce the associational patterns observed here. Overall, however, the data suggest a trend of U.S. obstetrics and gynecology residents obtaining their global health training experiences in countries with greater disease burdens. To ensure that such momentum continues, residency leadership bodies such as the Council on Resident Education in Obstetrics and Gynecology could convene strategic meetings to share best practices and logistical models, as has been proposed for the Association of Program Directors in Surgery [23]. Priority-setting exercises, similar to those that have been conducted to guide investments in global health research [34-36], could also provide concrete guidance about the placement of new global health training activities. And finally, program evaluations similar to those that have been completed for other disciplines [4, 37] should be planned, perhaps employing the ACGME core competencies as an outline for identifying measurable outcomes.
Interpretation of our data is subject to several important limitations. First, the Internet-based search protocol may have had low sensitivity for identifying obstetrics and gynecology residency programs with global health training. For example, some residency training programs may offer global health training either formally or informally without describing such activity on their programs’ web sites [23]. Many faculty members in departments of obstetrics and gynecology are engaged in global health research or clinical care activities and invite residents to participate without establishing longitudinal curricula or formal programs. Alternatively, the information contained on the programs’ web sites could simply be out of date. While a nationwide survey of residency program directors could potentially have yielded a more in-depth and current characterization of global health-related programmatic activities, previous surveys of program directors [21-23] and residents [8] have been characterized by relatively low response rates and, therefore, unpredictable biases. Second, our review excluded several institution-wide global health programs that do not provide opportunities for obstetrics and gynecology residents. These include, for example, the Yale/Stanford Johnson and Johnson Global Health Scholars Program and the Mount Sinai Global Health Residency Track, which enroll residents from several different specialties but do not enroll obstetrics and gynecology residents. Third, our review did not account for institutions offering fellowship-level training in global health [38], as well as residency programs offered by institutions in other high-income countries. As a result, our review therefore explicitly excluded programs such as the Duke Global Health Residency/Fellowship Pathway and the AMPATH Reproductive Health program led by the University of Toronto.
This study represents a unique assessment of the scope of global health-related programmatic activities available to U.S. obstetrics and gynecology residents. We found that there are relatively few global health training opportunities but that these appear to be distributed according to the global burden of maternal and perinatal conditions. Given the limitations we described, as well as the fact that global health-related programmatic activity in U.S. obstetrical and gynecological education is rapidly evolving, the field has an opportunity to further deepen its involvement and leadership in this area. Carefully planned program evaluations and priority setting exercises will help to ensure that global health programs in U.S. graduate obstetrics and gynecology education achieve their goals of increasing women’s access to health care and reducing the burden of disease due to maternal and perinatal conditions worldwide.
ACKNOWLEDGMENTS
The authors thank Brian A. Bergmark, Regan W. Bergmark, and Chaturia Rouse for research assistance. There are relatively few global health training opportunities for U.S. obstetrics and gynecology residents, with differential program placement in countries with higher burdens of disease.
Supported by the Mark and Lisa Schwartz Foundation; the Klingenstein Family Foundation; and the Harvard University Center for AIDS Research, through U.S. National Institutes of Health (NIH) P30AI060354. The authors also acknowledge salary support from NIH K23MH096620 (ACT), NIH R01AI058736 (RPW), and NIH K24MH087227 (DRB).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hill DR, Ainsworth RM, Partap U. Teaching global public health in the undergraduate liberal arts: a survey of 50 colleges. Am J Trop Med Hyg. 2012 Jul;87:11–5. doi: 10.4269/ajtmh.2012.11-0571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heck JE, Wedemeyer D. International health education in US medical schools: trends in curriculum focus, student interest, and funding sources. Family Med. 1995;27:636–40. [PubMed] [Google Scholar]
- 3.Kerry VB, Ndung’u T, Walensky RP, Lee PT, Kayanja VF, Bangsberg DR. Managing the demand for global health education. PLoS Med. 2011 Nov;8:e1001118. doi: 10.1371/journal.pmed.1001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai AC, Ordóñez AE, Reus VI, Mathews CA. Eleven-year outcomes from an integrated residency program to train research psychiatrists. Acad Med. 2013;88:983–8. doi: 10.1097/ACM.0b013e318294f95d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta AR, Wells CK, Horwitz RI, Bia FJ, Barry M. The International Health Program: the fifteen-year experience with Yale University’s Internal Medicine Residency Program. Am J Trop Med Hyg. 1999 Dec;61:1019–23. doi: 10.4269/ajtmh.1999.61.1019. [DOI] [PubMed] [Google Scholar]
- 6.Dey CC, Grabowski JG, Gebreyes K, Hsu E, VanRooyen MJ. Influence of international emergency medicine opportunities on residency program selection. Acad Emerg Med. 2002 Jul;9:679–83. doi: 10.1111/j.1553-2712.2002.tb02145.x. [DOI] [PubMed] [Google Scholar]
- 7.Bazemore AW, Henein M, Goldenhar LM, Szaflarski M, Lindsell CJ, Diller P. The effect of offering international health training opportunities on family medicine residency recruiting. Family Med. 2007;39:255–60. [PubMed] [Google Scholar]
- 8.Anspacher M, Frintner MP, Denno D, Pak-Gorstein S, Olness K, Spector J, et al. Global health education for pediatric residents: a national survey. Pediatrics. 2011 Oct;128:e959–65. doi: 10.1542/peds.2011-0129. [DOI] [PubMed] [Google Scholar]
- 9.Thompson MJ, Huntington MK, Hunt DD, Pinsky LE, Brodie JJ. Educational effects of international health electives on U.S. and Canadian medical students and residents: a literature review. Acad Med. 2003 Mar;78:342–7. doi: 10.1097/00001888-200303000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Jeffrey J, Dumont RA, Kim GY, Kuo T. Effects of international health electives on medical student learning and career choice: results of a systematic literature review. Fam Med. 2011 Jan;43:21–8. [PubMed] [Google Scholar]
- 11.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med. 2009 Mar;84:320–5. doi: 10.1097/ACM.0b013e3181970a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013 Dec 15;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ivers LC, Garfein ES, Augustin J, Raymonville M, Yang AT, Sugarbaker DS, et al. Increasing access to surgical services for the poor in rural Haiti: surgery as a public good for public health. World J Surg. 2008 Apr 32;:537–42. doi: 10.1007/s00268-008-9527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taira BR, Kelly McQueen KA, Burkle FM., Jr. Burden of surgical disease: does the literature reflect the scope of the international crisis? World J Surg. 2009 May 33;:893–8. doi: 10.1007/s00268-009-9981-x. [DOI] [PubMed] [Google Scholar]
- 15.Debas HT, Gosselin R, McCord C, Thind A. Surgery. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease control priorities in developing countries. 2nd edition. Oxford University Press and The International Bank for Reconstruction and Development; New York and Washington, D.C.: 2006. pp. 1245–60. [PubMed] [Google Scholar]
- 16.Kingham TP, Kamara TB, Cherian MN, Gosselin RA, Simkins M, Meissner C, et al. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg. 2009 Feb;144:122–7. doi: 10.1001/archsurg.2008.540. discussion 8. [DOI] [PubMed] [Google Scholar]
- 17.Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H, et al. Assessment of capacity for surgery, obstetrics and anaesthesia in 17 Ghanaian hospitals using a WHO assessment tool. Trop Med Int Health. 2010 Sep;15:1109–15. doi: 10.1111/j.1365-3156.2010.02589.x. [DOI] [PubMed] [Google Scholar]
- 18.Linden AF, Sekidde FS, Galukande M, Knowlton LM, Chackungal S, McQueen KA. Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J Surg. 2012 May;36:1056–65. doi: 10.1007/s00268-012-1482-7. [DOI] [PubMed] [Google Scholar]
- 19.Grimes CE, Law RS, Borgstein ES, Mkandawire NC, Lavy CB. Systematic review of met and unmet need of surgical disease in rural sub-Saharan Africa. World J Surg. 2012 Jan;36:8–23. doi: 10.1007/s00268-011-1330-1. [DOI] [PubMed] [Google Scholar]
- 20.Shirazian T, Ascher-Walsh C, Brodman M. Global women’s healthcare in obstetrics and gynecology: a model for resident programs. Contemp Obstet Gynecol. 2012;57:48–51. [Google Scholar]
- 21.Nelson BD, Lee AC, Newby PK, Chamberlin MR, Huang CC. Global health training in pediatric residency programs. Pediatrics. 2008 Jul;122:28–33. doi: 10.1542/peds.2007-2178. [DOI] [PubMed] [Google Scholar]
- 22.Jayaraman SP, Ayzengart AL, Goetz LH, Ozgediz D, Farmer DL. Global health in general surgery residency: a national survey. J Am Coll Surg. 2009 Mar;208:426–33. doi: 10.1016/j.jamcollsurg.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell KB, Tarpley MJ, Tarpley JL, Casey KM. Elective global surgery rotations for residents: a call for cooperation and consortium. World J Surg. 2011 Dec;35:2617–24. doi: 10.1007/s00268-011-1311-4. [DOI] [PubMed] [Google Scholar]
- 24.Mathers C, Boerma JT, Fat DM. The global burden of disease: 2004 update. World Health Organization; Geneva: 2008. [Google Scholar]
- 25.Kolars JC, Halvorsen AJ, McDonald FS. Internal medicine residency directors perspectives on global health experiences. Am J Med. 2011 Sep;124:881–5. doi: 10.1016/j.amjmed.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Klaristenfeld DD, Chupp M, Cioffi WG, White RE. An international volunteer program for general surgery residents at Brown Medical School: the Tenwek Hospital Africa experience. J Am Coll Surg. 2008 Jul;207:125–8. doi: 10.1016/j.jamcollsurg.2008.01.025. [DOI] [PubMed] [Google Scholar]
- 27.Ozgediz D, Roayaie K, Debas H, Schecter W, Farmer D. Surgery in developing countries: essential training in residency. Arch Surg. 2005 Aug;140:795–800. doi: 10.1001/archsurg.140.8.795. [DOI] [PubMed] [Google Scholar]
- 28.Powell AC, Casey K, Liewehr DJ, Hayanga A, James TA, Cherr GS. Results of a national survey of surgical resident interest in international experience, electives, and volunteerism. J Am Coll Surg. 2009 Feb;208:304–12. doi: 10.1016/j.jamcollsurg.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 29.Ozgediz D, Wang J, Jayaraman S, Ayzengart A, Jamshidi R, Lipnick M, et al. Surgical training and global health: initial results of a 5-year partnership with a surgical training program in a low-income country. Arch Surg. 2008 Sep;143:860–5. doi: 10.1001/archsurg.143.9.860. discussion 5. [DOI] [PubMed] [Google Scholar]
- 30.Schecter WP, Farmer D. Surgery and global health: a mandate for training, research, and service--a faculty perspective from the UCSF. Bull Am Coll Surg. 2006 May;91:36–8. [PubMed] [Google Scholar]
- 31.Klufio CA, Kwawukume EY, Danso KA, Sciarra JJ, Johnson T. Ghana postgraduate obstetrics/gynecology collaborative residency training program: success story and model for Africa. Am J Obstet Gynecol. 2003 Sep;189:692–6. doi: 10.1067/s0002-9378(03)00882-2. [DOI] [PubMed] [Google Scholar]
- 32.Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet. 2010 Oct 2;376:1186–93. doi: 10.1016/S0140-6736(10)61152-X. [DOI] [PubMed] [Google Scholar]
- 33.Soerjomataram I, Lortet-Tieulent J, Parkin DM, Ferlay J, Mathers C, Forman D, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012 Nov 24;380:1840–50. doi: 10.1016/S0140-6736(12)60919-2. [DOI] [PubMed] [Google Scholar]
- 34.Rudan I, Gibson JL, Ameratunga S, El Arifeen S, Bhutta ZA, Black M, et al. Setting priorities in global child health research investments: guidelines for implementation of CHNRI method. Croat Med J. 2008 Dec;49:720–33. doi: 10.3325/cmj.2008.49.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rudan I, Chopra M, Kapiriri L, Gibson J, Ann Lansang M, Carneiro I, et al. Setting priorities in global child health research investments: universal challenges and conceptual framework. Croat Med J. 2008 Jun;49:307–17. doi: 10.3325/cmj.2008.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tomlinson M, Rudan I, Saxena S, Swartz L, Tsai AC, Patel V. Setting priorities for global mental health research. Bull World Health Organ. 2009 Jun;87:438–46. doi: 10.2471/BLT.08.054353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gourevitch MN, Jay MR, Goldfrank LR, Mendelsohn AL, Dreyer BP, Foltin GL, et al. Training physician investigators in medicine and public health research. Am J Public Health. 2012 Jul;102:e39–45. doi: 10.2105/AJPH.2011.300486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goodman A, Clark RM, Bradford LS. Caring for women with gynecologic cancers around the world: the need for global health training in gynecologic oncology fellowship programs. Am J Clin Oncol. 2012 Dec;35:511–3. doi: 10.1097/COC.0b013e318271b18a. [DOI] [PubMed] [Google Scholar]