Abstract
Surprisingly little is known about how or if knowledge of one’s HIV status influences the desire to have children in sub-Saharan Africa. This paper takes advantage of a unique situation in rural Malawi where no one knew their HIV status prior to testing being introduced as part of an ongoing panel study. Using a sample of men and women (n = 1,380) who were interviewed in 2001 and 2006, we examine how HIV positive and negative test results impact respondents’ desires to continue childbearing. We then consider how prior perceptions of one’s status influence this effect. Respondents who received a positive test result reduced their childbearing desires. When self-assessed likelihood of infection was considered, however, only those who were surprised by their test result altered their fertility preferences, a finding which held true for both positive and negative results. The implications of the results and potential applications to other HIV/AIDS research are discussed.
Keywords: HIV/AIDS, Fertility, Malawi, HIV testing, Longitudinal study
Introduction
The relationship between HIV and fertility will be a key determinant of the future demographic, epidemiologic and social makeup of sub-Saharan Africa. Despite the scholarly attention paid to the epidemic, however, surprisingly little is known about how HIV/AIDS affects pregnancy, fertility, and reproductive goals in the region (Casterline 2002). In this paper, we take advantage of a unique situation in rural Malawi where no one knew their HIV status prior to participating in an ongoing longitudinal study that introduced HIV testing and counseling. We ask how knowledge of one’s HIV status influences the desire to continue having children and whether prior perceptions about infection alter this relationship.
HIV infection is known to affect the biological capacity for children, particularly during the latter stages, as increases in viral load are associated with decreases in fecundity (Desgrees-du-Lou et al. 1999; Ross et al. 2004; Zaba and Gregson 1998; Lewis et al. 2004; Nguyen et al. 2006). Far less is known about how HIV infection affects the way sub-Saharan Africans think and make decisions about fertility in contexts where childbearing remains a rite of passage for both men and women. We see two reasons for this research gap. First, early in the epidemic, when the societal consequences were less severe, there was probably little deliberate attempt to limit pregnancies in response to HIV infection, particularly in rural areas (Casterline 2002; Setel 1995). Second, until recently, few people in sub-Saharan Africa had access to HIV testing, so few knew their HIV status to be able to make childbearing decisions based on a known infection. Over the past decade both of these circumstances have changed: the consequences of the AIDS pandemic have worsened and more directly affect rural communities (Heuveline 2004; Gregson et al. 2007) and HIV testing is increasingly available, allowing people information about their HIV status before the signs and symptoms appear (WHO/UNAIDS/UNICEF 2008).
Existing research on the relationship between HIV and fertility desires has produced contradictory and inconclusive findings. A series of qualitative studies among women and men unaware of their HIV status (Rutenberg et al. 2000; Baylies 2000; Grieser et al. 2001) found that most respondents did not have strong feelings about the relationship between HIV and childbearing unless the hypothetical infected individuals they were asked about already had symptoms, at which point the general consensus was that they should not have more children. Other qualitative studies among women and men who knew they were HIV positive found that the desire for children persisted despite knowledge of one’s infection (Cooper et al. 2007; Aka-Dago-Akribi et al. 1999).
While informative, such qualitative data are inadequate for assessing latent changes in preferences or gauging the impact of HIV status on fertility desires. Few larger studies have examined the relationship between HIV status and fertility desires in the region making it difficult to untangle the biological and intentional components of fertility change. Quantitative analyses examining HIV and contraceptive use have largely failed to find differential contraceptive or condom use following HIV testing (Temmerman et al. 1990; Lutalo et al. 2000; Allen et al. 1993). More recently, a study by Hoffman et al. (2008) examined changes in pregnancy intentions following an HIV positive test result among urban Malawian women recruited from hospital clinics. They found that HIV positive women had reduced fertility desires over the year of the study. However, by only examining women who were HIV positive, the study had no reference category with which to compare those who learned they were infected. This is a particularly serious limitation in a clinic setting where women received counseling on family planning and HIV as part of the study.
One reason why the relationship between HIV status and fertility desires remains unclear may be the widespread assumption that people are unaware of their HIV status before they are tested for HIV. In the absence of HIV testing—and even where testing is available but under-utilized—people living in a generalized epidemic are not unaware of their HIV risk. Individually and within social networks they speculate about their HIV status based on symptomology and knowledge of their own, and their partners’ sexual behavior (Zaba and Gregson 1998; Smith and Watkins 2005; Bignami-Van Assche et al. 2007). While people do not have perfect knowledge of their HIV status, they do have opinions about their own likelihood of infection (Bignami-Van Assche et al. 2007; Anglewicz and Kohler 2009). For example, in the 2004 wave of the Malawi Diffusion and Ideational Change Project, the data used in the present study, fewer than 13% of respondents answered that they did not know their likelihood of infection. The vast majority were able to assess their own chance of infection and indicate that they had no, low, medium, or high likelihood (Fig. 1). Respondents were more likely to think they were HIV positive when they were really negative than that they were HIV negative when they were really positive. Thirty-four percent of women and 24% of men thought they had some likelihood of infection in 2004, which was more than four times the percent that were actually infected when they got tested the following week. While clearly imperfect, such self-assessments are not random: respondents who reported that they had a high likelihood of infection were almost twice as likely to be infected as those who reported no likelihood. Nonetheless, 88% of respondents (not shown) who thought it was highly likely they were HIV positive were uninfected at the time.
Fig. 1.
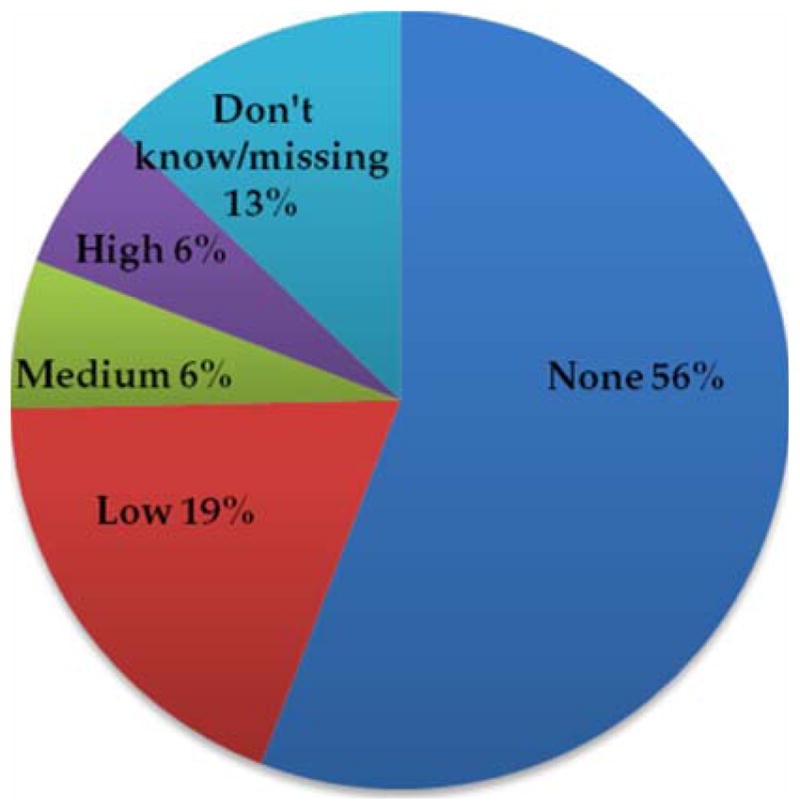
Perceived likelihood of infection, MDICP 2004
Two studies have examined the relationship between HIV/AIDS perceptions and fertility. In rural Malawi, Noel-Miller (2003) found a small reduction in actual fertility between two survey waves for women who were very worried they might become infected. In Zimbabwe, Moyo and Mbizvo (2004) found a reduced but insignificant desire for subsequent pregnancy among women who perceived their risk of infection to be high. No study, of which we are aware, has considered the impact of an HIV negative test result on fertility preferences despite the fact that most people test negative and many will be surprised by that result.
In the present study, we set up a quasi-experimental design using panel data from rural Malawi to examine how HIV testing influences fertility preferences. Unlike previous studies, we consider change over time, the separate impact of a positive and negative test result, and the influence that prior perception of one’s status may have in mediating the effect of testing on preferences.
Methods
The Malawi Diffusion and Ideational Change Project (MDICP)1 is an ongoing longitudinal data collection project in rural Malawi designed to examine the role of social interactions in contraceptive decision making and the diffusion of knowledge about HIV and AIDS. The MDICP began in 1998 with a sample of 1,500 ever-married women and their husbands, using a cluster sampling strategy from 145 randomly selected villages in three rural districts of Malawi. The methods have been described in detail elsewhere (Watkins et al. 2003).
Data for the present study come from three waves of the MDICP: 2001, 2004, and 2006. A series of core questions were asked in each wave using a structured questionnaire. Questions on fertility preferences were included in 2001 and 2006 but, unfortunately, were not included in the 2004 questionnaire. During the 2004 wave, nurses offered respondents HIV testing in their homes using ORASURE (OraSure Technologies, Inc., Bethlehem, Pennsylvania) saliva tests (positive results were confirmed through Western Blot). Tents were set up at randomly selected locations 4–6 weeks after testing so that respondents could receive test results, counseling, and treatment for curable sexually transmitted infections. Ninety-one percent of respondents contacted agreed to be tested and 70% of those tested returned for their test results (Thornton et al. 2005). Figure 2 presents a timeline of the MDICP surveys and HIV testing that took place between 2001 and 2006.
Fig. 2.
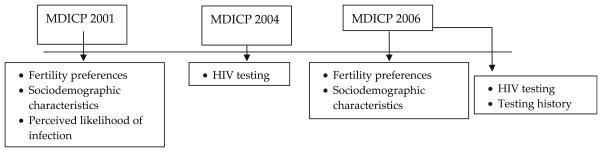
Timeline of MDICP components used in quasi-experimental design
The desire to continue childbearing, the dependent variable, was captured using the question: “(After the child you are expecting is born), would you like to have a(nother) child or would you like to stop having children?” Fertility preferences as measured with this question are good predictors of future fertility and considered the least biased of standard preference measures (Bongaarts 1990; Thomson et al. 1990; Pritchett 1994). The variable was dichotomized such that “0” signified that the respondent did not want to have another child and “1” that the respondent wanted to continue childbearing.
Respondents are assumed to have not received an HIV test result before 2004—a reasonable assumption given that HIV testing was not available in rural Malawi until 2005 when voluntary counseling and testing centers were gradually rolled out in regional hospitals. Respondents are considered to have received an HIV positive test result between 2001 and 2006 if they either (1) tested positive for HIV and received their results in 2004 with MDICP or (2) tested positive for HIV in 2004, did not receive their results from MDICP but indicated in a 2006 questionnaire that they had tested elsewhere and received their results between 2004 and 2006. Respondents are considered to have received an HIV negative test result between 2001 and 2006 if they either (1) tested negative for HIV and received their results in 2004 with MDICP or (2) tested negative for HIV in 2004, did not receive their results from MDICP but indicated in a 2006 testing history that they had tested elsewhere and received their results between 2004 and 2006 and did not seroconvert between 2004 and 2006 (i.e., tested negative in 2006). The comparison group includes all other respondents who were interviewed in both 2001 and 2006 but did not receive their HIV test results in 2004 and for whom we cannot confirm that they received their results elsewhere between 2004 and 2006. This includes respondents who tested positive or negative but did not collect their results between 2004 and 2006 and respondents who had never been tested. On average, bias from this varied control group should minimize rather than exaggerate any effect size.
The final analytic sample consists of 1,380 respondents, 758 women and 622 men, who met the age criteria (<40 for women in 2001), and provided classifiable responses (i.e., not missing or “don’t know”) on the dependent variable in both years.
Treatment Context
Between 2005 and 2006, rural district hospitals in Malawi began offering antiretroviral therapy (ART) free of charge to HIV positive adults with advanced infections (WHO stages 3 and 4) on a limited basis (Libamba et al. 2006; Ministry of Health and Population 2007). Despite impressive scaling up of ART services, regular access to ART remains impracticable for most infected rural residents given current resource and infrastructure constraints. There remains a possibility that the prospect of future access to ART may have influenced respondents. However, few MDICP respondents reported knowing someone on ART in 2006, and qualitative interviews by the author (Yeatman 2008) suggest that ART did not have a major influence on respondents at the time of the study.
Ethical Considerations
Written informed consent was obtained from all participants for each survey wave and for HIV testing. The MDICP was approved by the University of Pennsylvania’s Institutional Review Board and the Malawi College of Medicine’s Institutional Review Board.
Statistical Analysis
Difference in differences analyses (Meyer 1995; Abadie 2005) are used to assess the impact that receiving an HIV positive or negative test result has on the desire to continue childbearing. The models compare those with who received a positive or negative test result to a control group over the time period when testing took place. The models subtract the differences between the two groups before and after testing to estimate the causal effect of receiving a certain HIV test result on fertility desires. The approach is performed using logistic regression to adjust for time invariant and time varying observable characteristics.
In the second section of the analyses, the sample is divided into those who stated in 2001, when fertility preferences were first measured, that they had some likelihood of infection and those who stated that they had none.2 This division allows for an assessment of how perceived HIV status prior to testing alters the relationship between testing and changes in fertility preferences.
All models adjust for age, education, living children, marital status, site, and sex. Age, number of living children, and marital status are allowed to vary with time while the other control variables remain constant. Models additionally adjust for clustering to minimize autocorrelation from multiple responses from each individual. Data analyses were performed using Stata 9.0 (Stata Corp, College Station, Texas).
Results
Table 1 presents descriptive characteristics of the sample in 2001 and 2006 by whether they received an HIV positive test result, an HIV negative test result, or no test result between the two time periods. The three groups are broadly similar. Differences that do exist are adjusted for in regression analysis.
Table 1.
Descriptive statistics by test results, MDICP 2001 and 2006
| Positive test resulta
|
Negative test resulta
|
Did not receive result
|
||||
|---|---|---|---|---|---|---|
| 2001 | 2006 | 2001 | 2006 | 2001 | 2006 | |
| Want a(nother) child (%) | 63.8 | 20.7* | 53.6+ | 31.8 | 58.5 | 34.0 |
| Some likelihoods of infection (%) | 32.8 | n/a | 29.0 | n/a | 30.0 | n/a |
| Age (years) | 32.6 | 37.6 | 34.7 | 39.7 | 34.7 | 39.7 |
| Living chlidren | 2.7* | 3.6** | 4.0+ | 5.0 | 3.8 | 4.9 |
| Married (%) | 94.8 | 81.0** | 97.4** | 96.1+ | 93.6 | 93.9 |
| Compl primary education (%) | 29.3 | 26.1 | 28.9 | |||
| Southern site (%) | 36.2 | 30.9 | 30.0 | |||
| Central site (%) | 37.9 | 34.6 | 37.8 | |||
| Northern site(%) | 25.9 | 34.5 | 32.2 | |||
| Male (%) | 27.6** | 44.5 | 48.6 | |||
| N (response) | 58 | 58 | 896 | 896 | 426 | 426 |
Note: Significantly different from “did not receive result” at
P < 0.10;
P <0.05;
P <0.01
Received a positive or negative test result between 2004 and 2006. 2001 period refers to before testing
The analytic sample tends toward the latter stages of reproduction because the original MDICP sample was drawn from a random population of ever-married women and their husbands in 1998. HIV prevalence for this rural longitudinal sample is relatively low—only 6% of women and 3% of men received an HIV positive test result.3
Table 2 presents the exponentiated results of difference in differences logistic regression models predicting the desire to have children. Model 1 combines the entire sample adjusting for sex and sociodemographic characteristics. The first row, “Positive test result”, refers to pre-testing differences in fertility preferences between those who subsequently received a positive test result and those who did not receive their test result. Across all models there are no significant differences prior to HIV testing. The second row captures changes in fertility preferences between 2001 and 2006. Fertility desires are highly age dependent, and this is reflected in the models. The impact of a positive test result on subsequent fertility preferences is captured through the interaction (“Positive×change in fertility preferences”) of receiving a positive test result and the post-testing period of data collection. In the combined model, people who learned they were HIV positive had less than half the odds (OR = 0.40) of wanting to continue childbearing as they would have been expected to have without their test result.
Table 2.
Odds ratios predicting desire for a(nother) child after an HIV positive test result by prior speculation, MDICP 2001–2006
| Model 1 combined | Model 2 no likelihood | Model 3 some likelihood | |
|---|---|---|---|
| Positive test resultsa | 0.89 | 1.31 | 0.48 |
| Change in fertility preferences 2001–2006 | 0.60** | 0.73+ | 0.37** |
| Positive × change in fertility preferences | 0.40* | 0.23** | 1.12 |
| Male | 2.57** | 2.49** | 2.58* |
| < 25 years | 2.86** | 3.43** | 2.23 |
| 25–29 | 1.29 | 1.03 | 2.18 |
| 30–34(ref) | 1.00 | 1.00 | 1.00 |
| 35–39 | 0.51** | 0.53* | 0.41+ |
| 40–44 | 0.32** | 0.30** | 0.39* |
| 45–50 | 0.35** | 0.30** | 0.45* |
| 50+ | 0.09** | 0.07** | 0.14* |
| Compl primary education | 0.54** | 0.54* | 0.52+ |
| Living chlidren | 0.68** | 0.69** | 0.63** |
| Married | 1.25 | 0.78 | 2.54+ |
| Southern site (ref) | 1.00 | 1.00 | 1.00 |
| Central site | 0.67 | 0.71 | 0.47+ |
| Northern site | 1.47 | 1.41 | 1.40 |
| Pseudo R^2 | 0.29 | 0.29 | 0.32 |
| N (respondents) | 484 | 337 | 147 |
Note: Significantly different from comparison category at
P < 0.10;
P < 0.05;
P < 0.01
Reference category is no result
Models 2 and 3 divide the sample into those who perceived they had no likelihood of infection in 2001 and those who perceived they had some likelihood of infection, respectively. The impact of receiving a positive test result on the desire to bear more children was particularly strong for those who thought they had no likelihood of infection in 2001 (OR = 0.23) and not statistically significant for those who had thought they might be infected. The strength of these conclusions is limited by the sample size, but differ significantly at the P < 0.10 level4 and suggest an interaction between perceived likelihood and actual infection.
Table 3 presents the exponentiated logistic regression results for receiving an HIV negative test result. Model 1 finds that testing negative has little impact on childbearing desires (“Negative x change in fertility preferences”)—respondents who tested negative had a slight but insignificant increased desire to continue childbearing than would have been expected without receiving their results. When the sample is divided by prior perceptions, however, the picture once again changes. Respondents who were surprised to test negative because they thought it likely they were HIV positive increased their desire to have children relative to the control group (people who did not get their status and reported some likelihood of infection) after testing. They have more than twice the odds of wanting more children than they would have had if they had not received the negative test result. In contrast, among respondents who reported no likelihood of infection in 2001, a negative test result had little impact on fertility desires. These two results differed significantly, a finding confirmed through subgroup analysis (z-score = 2.45, P < 0.01).
Table 3.
Odds ratios predicting desire for a(nother) child after an HIV negative test result by prior speculation, MDICP 2001–2006
| Model 1 combined | Model 2 no likelihood | Model 3 some likelihood | |
|---|---|---|---|
| Negtive test resultsa | 0.83 | 0.87 | 0.72 |
| Change in fertility preferences 2001–2006 | 0.61** | 0.72+ | 0.40** |
| Negative × change in fertility preferences | 1.18 | 0.88 | 2.35* |
| Male | 2.41** | 2.42** | 2.73** |
| < 25 years | 3.67** | 4.78** | 2.13+ |
| 25–29 | 1.53** | 1.61** | 1.34 |
| 30–34(ref) | 1.00 | 1.00 | 1.00 |
| 35–39 | 0.61** | 0.60** | 0.56** |
| 40–44 | 0.35** | 0.39** | 0.25** |
| 45–50 | 0.30** | 0.30** | 0.25** |
| 50+ | 0.14** | 0.14** | 0.11** |
| Compl primary education | 0.78+ | 0.82 | 0.68 |
| Living chlidren | 0.72** | 0.72** | 0.72** |
| Married | 1.61+ | 1.17 | 2.85* |
| Southern site (ref) | 1.00 | 1.00 | 1.00 |
| Central site | 0.54** | 0.53** | 0.62+ |
| Northern site | 1.13 | 1.02 | 1.44 |
| Pseudo R^2 | 0.23 | 0.25 | 0.22 |
| N (respondents) | 1322 | 934 | 388 |
Note: Significantly different from comparison category at
P < 0.10;
P < 0.05;
P < 0.01
Reference category is no result
Limitations
The present study goes beyond previous work on the relationship between HIV status and fertility desires by incorporating pre- and post-testing preferences and accounting for secular changes over time. Nonetheless, there are limitations to these analyses that deserve to be addressed. First, the MDICP sample used does not reflect the normal reproductive age distribution of rural Malawi. The original MDICP sample began as a sample of ever-married women and their husbands in rural Malawi in 1998. Thus, at time of interview in 2001 and 2006, the respondents are older and tend towards the end rather than the beginning of their reproductive lives. This limitation does not affect internal validity but will limit the generalizability of findings to the rural Malawian population as we are unable to draw conclusions about how HIV testing affects the fertility desires of the young or those just getting married for the first time.
Second, the time gap between 2001 and 2006 is a long period in the reproductive lives of the respondents. Because fertility preferences were not included in the 2004 MDICP survey, 2001 is used as the pre-testing period. There are, however, external influences that may have affected fertility preferences during this period. We minimize this limitation by adjusting for three of the main influences on fertility desires over the 5 years: age, children, and marital status. The direction of bias introduced by such a long gap will most likely be to reduce the effect of positive or negative test results because of statistical noise that increases with the length of the time period. The consistency of the findings despite this sizeable gap is reassuring.
Discussion
This study found that rural Malawians adjust their fertility preferences in response to information about their HIV status. Although some had speculated early on that HIV would increase childbearing desires (Gregson 1994; Temmerman et al. 1994; Ntozi and Kirunga 1998), there is no evidence for such an effect in rural Malawi. Among this older and ever-married sample, respondents reduced their desire to have more children after testing HIV positive. This finding should not mask considerable heterogeneity as 20% of women and 13% of men still wanted to have children despite receiving a HIV positive test result.
The study also highlights the importance of individuals’ perceptions about their own HIV status in mediating the impact of HIV testing. When prior perceptions were considered, the effect of an HIV test result on childbearing desires was limited to tests that disconfirmed self-diagnoses. For example, when respondents suspected they were HIV negative, an HIV negative test result had little impact on their childbearing desires as it only confirmed what was already believed. On the other hand, when respondents believed they might be infected but later tested negative, the negative test result influenced their childbearing desires because it contrasted with expectations. The results suggest that self-assessments of HIV status are meaningful and used to inform decisions in rural Malawi.
This finding has potential implications for other HIV/AIDS research. For example, evidence for HIV testing and counseling altering sexual risk behavior in sub-Saharan Africa has been contradictory and largely disappointing for policymakers (Yeatman 2007; Shelton 2008). However, no study, to our knowledge, has yet considered the role of prior perceptions in moderating the influence of HIV testing on behavioral outcomes. Most studies assume ignorance to one’s status prior to testing which, as shown here, is a flawed assumption. The present research, if extrapolated from childbearing to sexual behavior, allows for the possibility that HIV testing and counseling may affect sexual risk behavior, but only in those cases where results counter perception.
The past 5 years have seen dramatic shifts in access to, and use of, free HIV testing across sub-Saharan Africa—and the next five will no doubt see shifts that are just as substantial. There are millions of men and women of childbearing age in the region who are unaware of their HIV infection. This study’s findings suggest that testing may lead to a reduction in childbearing preferences for these individuals. The corollary, however, is that in many communities there exists a larger population who suspect they are HIV positive but are in fact uninfected. When this population learns they are HIV negative in contrast to their expectations, the desire to have children—which had been suppressed by their perceived infection—may be reinvigorated. Given these countervailing forces, an expansion in HIV testing in the current medical environment may ultimately lead to a net increase in fertility desires. If acted upon, such changes could translate to increases in fertility, which would be further exacerbated by the higher fecundity of those who are uninfected.
Acknowledgments
Data collection and the author’s time were supported by funding from NIH (5 T32HD007081, R01 HD/MH41713, R01 HD373-276, R01 HD044228) and NSF (SES-0623543). This paper is a version of a paper presented at the Union for African Population Studies 5th Annual Meeting in Arusha, Tanzania, December 2007. Susan Watkins and Joe Potter provided helpful comments on an earlier draft.
Footnotes
Malawi Diffusion and Ideational Change Project (PIs Susan Watkins, Hans-Peter Kohler and Jere Behrman). Detailed descriptions of the MDICP sample selection, data collection and data quality are provided in a 2003 Special Collection of the online journal Demographic Research that is devoted to the MDICP and on the project website: http://www.malawi.pop.upenn.edu/.
This group includes those who said they “do not know”. This is a difficult group to categorize. While their actual HIV prevalence was similar to those who thought they had a high likelihood of infection, what is relevant here is what they thought of their risk. The analyses were run with this group in both categories, as well as dropped entirely. The results did not change substantially; the method chosen was considered to be a conservative approach.
HIV prevalence for the entire 2004 MDICP sample was 6.7%–5.7% of men and 7.6% of women (though they did not all receive their test result). The longitudinal sample has lower HIV prevalence because of disproportionate attrition among HIV positive individuals—HIV positive individuals in 2004 were more likely to have died and more likely to not be found in 2006. The potential bias introduced is not believed to substantially affect the results because there is no clear theoretical reason why mortality would be higher among infected persons who were more or less likely to change their fertility preferences. In fact, the findings are most relevant to those with lower mortality—the least ill—whose fertility preferences are of greater demographic and epidemiologic relevance.
Tested using subgroup analysis (Altman and Bland 2003)
References
- Abadie A. Semiparametric difference-in-differences estimators. Review of Economic Studies. 2005;72:1–19. doi: 10.1111/0034-6527.00321. [DOI] [Google Scholar]
- Aka-Dago-Akribi H, Desgrees du Lou A, Msellati P, Dossou R, Welffens-Ekra C. Issues surrounding reproductive choice for women living with HIV in Abidjan, Cote d’Ivoire. Reproductive Health Matters. 1999;7:20–29. doi: 10.1016/S0968-8080(99)90108-8. [DOI] [Google Scholar]
- Allen S, Serufilira A, Gruber V, Kegeles S, Vandeperre P, Carael M, et al. Pregnancy and contraception use among urban Rwandan women after HIV testing and counselling. American Journal of Public Health. 1993;83:705–710. doi: 10.2105/AJPH.83.5.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman DG, Bland JM. Interaction revisited: The difference between two estimates. (Statistics notes) British Medical Journal. 2003;326(1):219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglewicz P, Kohler HP. Overestimating HIV Infection: The construction and accuracy of subjective probabilities of HIV infection in rural Malawi. Demographic Research. 2009;20:65–96. doi: 10.4054/DemRes.2009.20.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylies C. The impact of HIV on family size preference in Zambia. Reproductive Health Matters. 2000;8:77–86. doi: 10.1016/S0968-8080(00)90008-9. [DOI] [PubMed] [Google Scholar]
- Bignami-Van Assche S, Chao LW, Anglewicz P, Chilongozi D, Bula A. The validity of self-reported likelihood of HIV infection among the general population in rural Malawi. Sexually Transmitted Infections. 2007;83:35–40. doi: 10.1136/sti.2006.020545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongaarts J. The measurement of wanted fertility. Population and Development Review. 1990;16:487–506. doi: 10.2307/1972833. [DOI] [Google Scholar]
- Casterline JB. HIV/AIDS and fertility in sub-Saharan Africa: A review of the recent literature. New York: United Nations; 2002. [Google Scholar]
- Cooper D, Harries J, Myer L, Orner P, Bracken H. “Life is still going on”: Reproductive intentions among HIV-positive women and men in South Africa. Social Science and Medicine. 2007;65:274–283. doi: 10.1016/j.socscimed.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Desgrees-du-Lou A, Msellati P, Yao A, Noba V, Viho I, Ramon R, et al. Impaired fertility in HIV-1-infected pregnant women: A clinic-based survey in Abidjan, Cote d’Ivoire, 1997. AIDS (London, England) 1999;13:517–521. doi: 10.1097/00002030-199903110-00011. [DOI] [PubMed] [Google Scholar]
- Gregson S. Will HIV become a major determinant of fertility in sub-Saharan Africa. The Journal of Development Studies. 1994;30:650–679. doi: 10.1080/00220389408422331. [DOI] [Google Scholar]
- Gregson S, Mushati P, Nyamukapa C. Adult mortality and erosion of household viability in AIDS-afflicted towns, estates, and villages in eastern Zimbabwe. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007;44:188–195. doi: 10.1097/01.qai.0000247230.68246.13. [DOI] [PubMed] [Google Scholar]
- Grieser M, Gittelsohn J, Shankar AV, Koppenhaver T, Legrand TK, Marindo R, et al. Reproductive decision making and the HIV/AIDS epidemic in Zimbabwe. Journal of Southern African Studies. 2001;27:225–243. doi: 10.1080/03057070120049949. [DOI] [Google Scholar]
- Heuveline P. Impact of the HIV epidemic on population and household structure: the dynamics and evidence to date. AIDS (London, England) 2004;18:S45–S53. doi: 10.1097/00002030-200406002-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman IF, Martinson FEA, Powers KA, Chilongozi DA, Msiska ED, Kachipapa EI, et al. The year-long effect of HIV-positive test results on pregnancy intentions, contraceptive use, and pregnancy incidence among Malawian women. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2008;47:477–483. doi: 10.1097/QAI.0b013e318165dc52. [DOI] [PubMed] [Google Scholar]
- Lewis JJC, Ronsmans C, Ezeh A, Gregson S. The population impact of HIV on fertility in sub-Saharan Africa. AIDS (London, England) 2004;18:S35–S43. doi: 10.1097/00002030-200406002-00005. [DOI] [PubMed] [Google Scholar]
- Libamba E, Makombe S, Mhango E, de AscurraTeck, Limbambala O, Schouten EJ, et al. Supervision, monitoring and evaluation of nationwide scale-up of antiretroviral therapy in Malawi. Bulletin of the World Health Organization. 2006;84:320–326. doi: 10.2471/blt.05.023952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutalo T, Kidugavu M, Wawer MJ, Serwadda D, Zabin LS, Gray RH. Trends and determinants of contraceptive use in Rakai District, Uganda, 1995–98. Studies in Family Planning. 2000;31:217–227. doi: 10.1111/j.1728-4465.2000.00217.x. [DOI] [PubMed] [Google Scholar]
- Meyer BD. Quasi-experiments natural in economics. Journal of Business & Economic Statistics. 1995;13:151–161. doi: 10.2307/1392369. [DOI] [Google Scholar]
- Ministry of Health and Population. ART in the public sector in Malawi, results up to 31st December 2006. HIV/AIDS Unit. Lilongwe, Malawi: Department of Clinical Services; 2007. [Google Scholar]
- Moyo W, Mbizvo MT. Desire for a future pregnancy among women in Zimbabwe in relation to their self-perceived risk of HIV infection, child mortality, and spontaneous abortion. AIDS and Behavior. 2004;8:9–15. doi: 10.1023/b:aibe.0000017521.26426.9d. [DOI] [PubMed] [Google Scholar]
- Nguyen RHN, Gange SJ, Wabwire-Mangen F, Sewankambo NK, Serwadda D, Wawer MJ, et al. Reduced fertility among HIV-infected women associated with viral load in Rakai district, Uganda. International Journal of STD and AIDS. 2006;17:842–846. doi: 10.1258/095646206779307586. [DOI] [PubMed] [Google Scholar]
- Noel-Miller C. Concern regarding the HIV/AIDS epidemic and individual childbearing evidence from rural Malawi. Demographic Research Special Collection. 2003;1:319–348. [Google Scholar]
- Ntozi JP, Kirunga CT. Family planning and HIV/AIDS in sub-Saharan Africa: Challenges and strategies. African Journal of Reproductive Health. 1998;2:44–56. [Google Scholar]
- Pritchett LH. Desired fertility and the impact of population policies. Population and Development Review. 1994;20:1–55. doi: 10.2307/2137629. [DOI] [Google Scholar]
- Ross A, Van derPaal L, Lubega R, Mayanja BN, Shafer LA, Whitworth J. HIV-1 disease progression and fertility: The incidence of recognized pregnancy and pregnancy outcome in Uganda. AIDS (London, England) 2004;18:799–804. doi: 10.1097/00002030-200403260-00012. [DOI] [PubMed] [Google Scholar]
- Rutenberg N, Biddlecom AE, Kaona FAD. Reproductive decision-making in the context of HIV and AIDS: A qualitative study in Ndola, Zambia. International Family Planning Perspectives. 2000;26:124–130. doi: 10.2307/2648301. [DOI] [Google Scholar]
- Setel P. The effect of HIV and AIDS on fertility in East and Central Africa. Health Transition Review. 1995;5:179–189. [PubMed] [Google Scholar]
- Shelton J. Counseling and testing for HIV prevention. Lancet. 2008;372:273–275. doi: 10.1016/S0140-6736(08)61091-0. [DOI] [PubMed] [Google Scholar]
- Smith KP, Watkins SC. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Social Science and Medicine. 2005;60:649–660. doi: 10.1016/j.socscimed.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Temmerman M, Chomba EN, Piot P. HIV-1 and reproductive health in Africa. International Journal of Gynaecology and Obstetrics: the Official Organ of the International Federation of Gynaecology and Obstetrics. 1994;44:107–112. doi: 10.1016/0020-7292(94)90062-0. [DOI] [PubMed] [Google Scholar]
- Temmerman M, Moses S, Kiragu D, Fusallah S, Wamola LA, Piot P. Impact of single session post-partum counseling of HIV infected women on their subsequent reproductive behavior. AIDS Care. 1990;2:247–252. doi: 10.1080/09540129008257737. [DOI] [PubMed] [Google Scholar]
- Thomson E, McDonald E, Bumpass LL. Fertility desires and fertility–hers, his, and theirs. Demography. 1990;27:579–588. doi: 10.2307/2061571. [DOI] [PubMed] [Google Scholar]
- Thornton R, Bula A, Chavula K, Bignami-Van Assche S, Watkins SC. Reactions to voluntary counselling and testing in rural Malawi. Malawi diffusion and ideational change project. 2005 Working paper, on-line at malawi.pop.upenn.edu.
- Watkins SC, Zulu EM, Kohler HP, Behrman JR. Introduction to social interactions and HIV/AIDS in rural Africa. Demographic Research. 2003;S1:1–30. doi: 10.4054/DemRes.2003.S1.1. [DOI] [Google Scholar]
- WHO/UNAIDS/UNICEF. Progress report, June 2008. Geneva: World Health Organization; 2008. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. [Google Scholar]
- Yeatman SE. Ethical and public health considerations in HIV counseling and testing: What do we know and what should that mean for policy? Studies in Family Planning. 2007;38(4):271–278. doi: 10.1111/j.1728-4465.2007.00139.x. [DOI] [PubMed] [Google Scholar]
- Yeatman SE. PhD Dissertation. University of Texas; Austin: 2008. Childbearing in an AIDS epidemic. [Google Scholar]
- Zaba B, Gregson S. Measuring the impact of HIV on fertility in Africa. AIDS (London, England) 1998;12:S41–S50. doi: 10.1097/00002030-199807000-00001. [DOI] [PubMed] [Google Scholar]


