Summary
Impressive results in patient care and cost reduction have increased the demand for systems-engineering methodologies in large health care systems. This Report from the Field describes the feasibility of applying systems-engineering techniques at a community health center currently lacking the dedicated expertise and resources to perform these activities.
Keywords: Systems engineering, workflow, implementation, evidence-based interventions
Community health centers (CHCs) are vanguard providers of primary care for vulnerable populations.1-4 Located in areas where care is needed but scarce, CHCs improve access to care for Americans regardless of their insurance status or ability to pay.5,6 With passage of health care reform, an estimated 32 million Americans will become newly insured and CHCs, the primary care safety net, will become a critical element of health care expansion through a primary care portal.5
Primary care practices are key to the dissemination of prevention and early detection interventions.7,8 However, ample literature describes the challenges posed by time constraints to implement changes in these settings.9-20 The volume of work associated with primary care delivery in the United States has increased to a greater extent than visit duration.19,21-25 Initiatives to transform primary care have therefore emphasized the need for a team approach to delivering care.26
As medical care becomes more complex at every stage—diagnosis, treatment, and follow-up—experts underscore that effective health care requires a delivery system that is fully coordinated and interconnected.27 A joint report by the Institute of Medicine and the National Academy of Engineering recommended the widespread application of systems-engineering approaches to deliver health care that is effective, efficient, patient-centered, and equitable.28
Systems engineering focuses on the coordination, synchronization, and integration of complex systems of personnel, information, materials, and financial resources.29,30 To determine how complex systems can be improved, engineers apply analytic methods to understand how such systems operate and where changes can be made. Systems-engineering techniques can help to ensure that the increasing volume of work encompassed by primary care, especially in resource-constrained CHCs, is performed efficiently and effectively. Impressive results in patient care and cost reduction achieved through improved efficiencies at several hospitals have increased demand for these methodologies in large health care systems.31
Value-stream mapping is one of several systems-engineering tools that can be used to define, plan, analyze, and implement significant process changes32 in hospitals and primary care settings. A value stream is the set of all actions required to take a particular good, service, or combination of the two from concept to a finished product in the hands of the customer.33,34 A value-stream map depicts the flow of work;35 the major steps in the process; the activities that take place in each step; and the time elements of the flow.36
Value-stream mapping facilitates the visualization and understanding of actual workflow, describing in detail how a facility should operate in order to improve flow and ensure the completion of tasks without delays.33,34,36,37 In manufacturing, flow and value are defined in relation to the processing of products, so that value is added whenever a product advances toward completion. In health care, the definition of value depends on the objective to be achieved (e.g., decrease in patient waiting time, increase in the number of patients seen).38 Identifying the entire value stream for a process exposes waste, so that time and resources can be invested in steps that add value to the overall process.33
Although conceptual frameworks emphasize the importance of compatibility between an intervention and its target setting,39,40 limited guidance is available to determine how an intervention can strategically fit within a health care system. Systems-engineering techniques provide what-if scenarios, including the likely consequences of various alternative courses of action, to determine optimal scenarios for patient care. Such analyses, which are relatively new to health care, can predict the impact of a proposed change on workflow and patient flow.41
In this report we summarize a feasibility study that applied systems-engineering methodologies, specifically value-stream mapping, to examine the implementation of an evidence-based intervention (EBI) in a clinic. A search of Pubmed and Web of Science yielded no studies that applied value-stream mapping in primary care clinics. We found one qualitative study that observed workflow at six safety-net clinics.42
description of Project
In 2010, our partner CHC provided comprehensive primary care to 15,016 predominantly limited-English proficient patients by staff who spoke 17 different languages and dialects, at two urban clinics.43
We previously developed an EBI to promote colorectal cancer screening among Chinese immigrants, the largest ethnic population at the CHC, through culturally and linguistically appropriate education materials and a trilingual health educator.44 This EBI was selected as a Research Tested Intervention Program for Cancer Control P.L.A.N.E.T., a Web site maintained by the National Cancer Institute and the Substance Abuse and Mental Health Services Administration.45
In a follow-up study, we investigated the adaptation of this EBI for Vietnamese immigrants, the second largest patient population at the CHC. Core elements of the adapted EBI included 1) translated educational materials for a different patient population with overlapping cultural and health beliefs, 2) delivery of these materials through a different channel—i.e., medical assistants (MAs), who are members of the primary care team with broader reach to clinic patients, and 3) presentations on colorectal cancer for the MAs.
Medical-assistant responsibilities included measuring and recording patient vital signs; facilitating in-clinic laboratory testing; and providing coordination, information, and instructions, as needed, during and after patient interactions with medical providers.
To explore the appeal of a more systematic approach to understanding the efficient integration of new MA tasks, we sought the expertise of the Chair of the University of Washington’s Industrial and Systems Engineering Department (RS), and then engaged in discussions with the CHC leadership to explore a feasibility study. We successfully obtained approval to add the feasibility study to our follow-up study, first from the CHC’s Research Review Committee and subsequently from the Institutional Review Board of the University of Washington. With the available resources, we then conducted value-stream mapping of MAs, providers, and patients in order to encompass patient-centered perspectives.
time and motion studies
After training, four University of Washington engineering students conducted time and motion studies to capture the current state of MA and provider workflows, and patient flow. No observations were conducted in exam rooms, and specific details of work at the MA stations and providers’ desks were not recorded since this was a feasibility study using limited resources and it was imperative to minimize disruptions in clinic services while simultaneously adhering to privacy standards required by federal law (the Health Insurance Portability and Accountability Act).
Time and motion study is a well-established technique used to evaluate the efficiency of work processes.46,47 Originally applied to increase productivity in manufacturing, this technique systematically analyzes workflows through first-hand observation and timing.47 Workflows in health care, like manufacturing tasks, tend to have a repetitive pattern, making time and motion studies a highly applicable tool.
We observed a total of 44 MA cycles, 40 provider cycles, and 31 patients. A cycle is defined as one complete process flow.37 For example, a MA cycle begins when he/she leaves the MA station to pick up a patient in the clinic waiting area, and it concludes when the MA returns to the MA station in preparation to pick up the next patient. Observation of at least 30 cycles ensures stable estimates of the mean and standard deviation of the time spent at each step. Using stopwatches and data collection forms, the students spent 59.25 hours conducting observations over the course of 22 separate days, from February 22 to May 7, 2010. Distances between locations were recorded separately and assumed to be related to the time spent walking between them.
Value-stream mapping
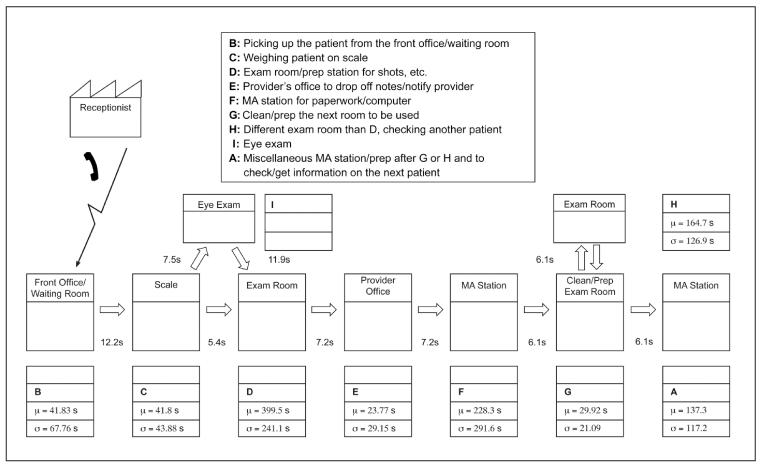
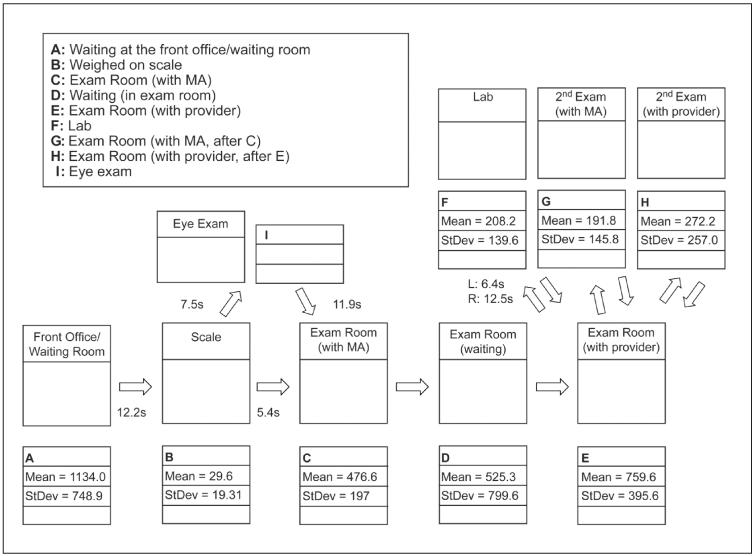
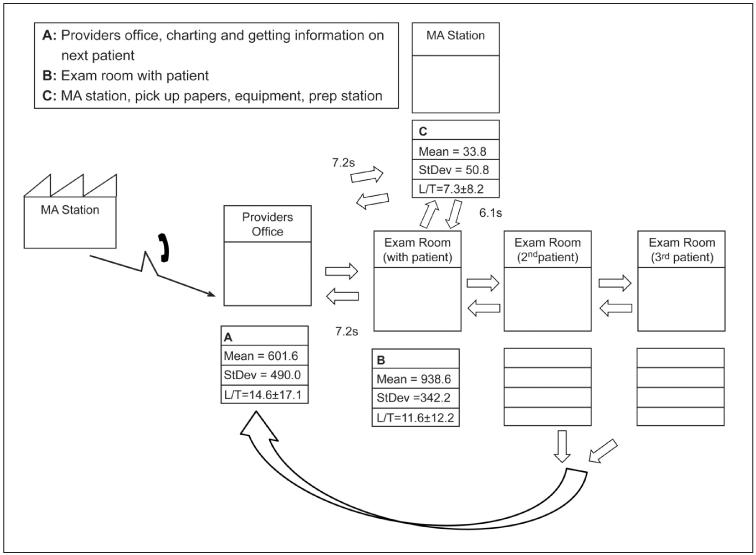
Using the time and motion study data, we developed value-stream maps for the MAs, providers, and patients (Figures 1-3). Presenting the data in this way made it easier to recognize the overall movement patterns of these individuals throughout the clinic. Each value-stream map documents key steps in the workflow and their associated location, and identifies general activities by assigning alphabetic characters in sequential order to each step. Each map also details the mean duration in seconds of each step (μ) and the standard deviation (σ). Arrows indicate the direction of the flow, and the numbers adjacent to each arrow represent the average walking time in seconds from starting point to destination.
Figure 1.
Current state value-stream map of medical assistants’ activities.
Figure 3.
Current state value-stream map of patients’ activities.
Within a given value-stream map, steps with the greatest variability and duration present opportunities for improvement, and are generally ideal places to introduce change. In accordance with this technique, we met with the MAs to elicit their feedback on the initial draft of the value-stream map. They noted that our value-stream map omitted less frequent workflow steps, such as vision exams and the use of extra exam rooms to accommodate providers who see more than one patient at a time. Since our observations did not include these additional steps, Figure 1 incorporates the MAs’ feedback but does not report times for these activities.
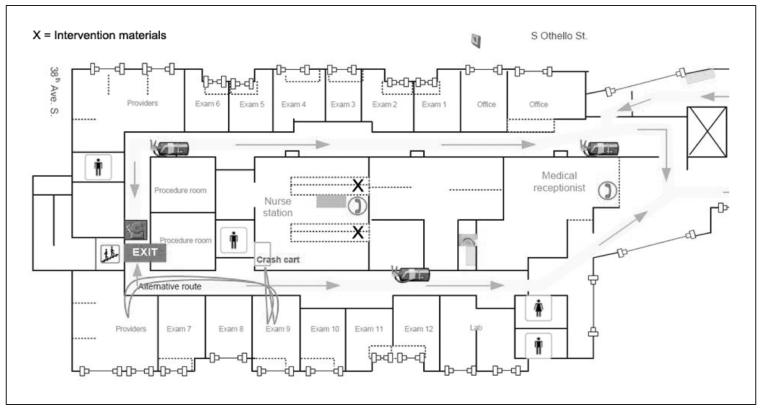
Spaghetti diagrams
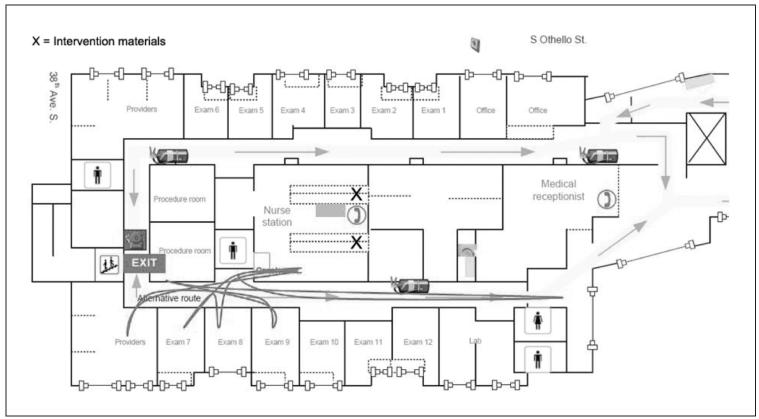
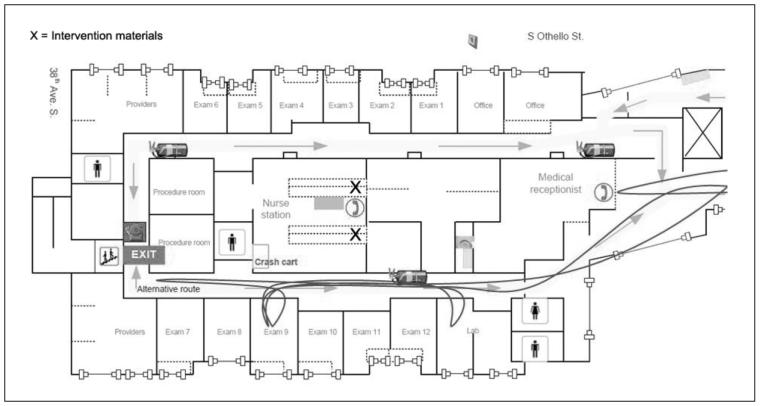
Spaghetti diagrams visually represent the movement of a person or product through a physical space.36 They depict walking patterns and can 1) identify where time is wasted by traveling between locations of essential checkpoints in the flow; 2) reveal unnoticed workarounds; and 3) identify opportunities for layout improvements, such as the movement of equipment and supplies, to reflect better the ways in which people move and work.36
Using the time and motion study data and value-stream maps we generated spaghetti diagrams of the movements of MAs, providers, and patients. Figures 4-6 present the respective spaghetti diagrams for each group, observed in a top-down layout of the clinic.
Figure 4.
Spaghetti diagram of medical assistants’ activities.
Figure 6.
Spaghetti diagram of patients’ activities.
meeting with ChC clinical leadership team
Previously, CHC clinical leaders expressed interest in a comprehensive portrayal of clinic activities. At a meeting to present the value-stream maps and spaghetti diagrams, the leaders reiterated their preference for a more comprehensive value-stream mapping with additional staff (e.g., nurses and interpreters) and all areas of the clinic. They also expressed great interest in developing the CHC’s capacity to apply value-stream mapping in conjunction with Kaizen workshops. Kaizen is a Japanese word often translated as “continuous improvement,” and Kaizen events typically follow a three-step process: observation and careful documentation of the current state using a process or value-stream map; value analysis and process redesign towards a future state with input from frontline employees; and implementation of the ideal future state.48
Currently, our partner CHC lacks the dedicated expertise and resources needed to conduct value-stream mapping or Kaizen workshops at their clinics. Given the CHC’s interest in acquiring the expertise needed for these activities, we collaborated on another research proposal to investigate the application of systems-engineering techniques by CHC staff, with training from systems engineers, to integrate our EBI into clinic services.
Conclusion
According to the literature, systems-engineering techniques have been available predominantly in hospitals and large health care systems that have the resources to pay for the necessary expertise.31,49-56 Like larger health care systems,31,57 CHCs and the patients they serve are likely to benefit from the application of systems-engineering techniques to deliver care. In order for CHCs to serve a larger segment of the U.S. population, or to expand beyond their current programs, it is imperative that the implementation of new programs not interfere with essential processes of medical care delivery.
Our feasibility study adapted approaches from traditional applications in manufacturing. In contrast to manufacturing settings, the application of these techniques in health care may face unique challenges, including the imperative to maintain confidentiality of patient health information, limited availability of space in certain clinical settings, and disruptions in patient care.
To identify appropriate value-adding operations at a clinic, comprehensive value-stream mapping must incorporate more detailed staff activities, include additional clinic staff, and encompass all areas of the clinic. We also recommend obtaining informed consent from patients, clinic staff, and providers prior to scheduled medical visits to minimize disruptions in patient care.
Research on the efficacy and effectiveness of systems-engineering methods is necessary not only to augment the quality improvement literature but, more crucially, to guide busy CHC clinics in their mission of satisfying the complex health care needs of underserved populations.
Figure 2.
Current state value-stream map of providers’ activities.
Figure 5.
Spaghetti diagram of providers’ activities.
acknowledgments
We would like to thank: 1) International Community Health Services, the Executive Team, the Management Team, and all the staff who contributed to this collaborative research; 2) our Systems Engineer colleagues, Jennifer Einberg, Sae Chung, Brittany Kohler, Zandra Mamaril, and Matthew Perez.
This work was supported by grant R01 CA 124397 from the National Cancer Institute. The National Cancer Institute played no role in the design of the work or the interpretation or presentation of it made here.
Footnotes
Conflict of interest. None of the authors have any past or present commercial associations that might pose a conflict of interest. None of the authors have any financial disclosures to make, and all authors declare that they have no competing interests of any kind.
Notes
- 1.Lefkowitz B. The health center story: forty years of commitment. Journal of ambulatory care management. 2005 Oct-Dec;28(4):295–303. doi: 10.1097/00004479-200510000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Proser M. Deserving the spotlight: health centers provide high-quality and cost-effective care. Journal of Ambulatory Care Management. 2005 Oct-Dec;28(4):321–30. doi: 10.1097/00004479-200510000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care. 2010 Aug;48(8):668–75. doi: 10.1097/MLR.0b013e3181e3585c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Association of Community Health Centers . The need. National Association of Community Health Centers; Bethesda, MD: 2010. [Google Scholar]
- 5.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care—the growing importance of the community health center. New England Journal Of Medicine. 2010 Jun 3;362(22):2047–50. doi: 10.1056/NEJMp1003729. [DOI] [PubMed] [Google Scholar]
- 6.National Association of Community Health Centers . Official web site. National Association of Community Health Centers; Bethesda, MD: 2010. [Google Scholar]
- 7.Kerner JF, Guirguis-Blake J, Hennessy KD, et al. Translating research into improved outcomes in comprehensive cancer control. Cancer Causes Control. 2005 Oct;16(Suppl 1):27–40. doi: 10.1007/s10552-005-0488-y. [DOI] [PubMed] [Google Scholar]
- 8.Klabunde CN, Lanier D, Meissner HI, et al. Improving colorectal cancer screening through research in primary care settings. Med Care. 2008 Sep;46(9 Suppl 1):S1–4. doi: 10.1097/MLR.0b013e3181805e2a. [DOI] [PubMed] [Google Scholar]
- 9.Ka’ano’i ME, Braun KL, Gotay CC. Primary care physicians’ knowledge, attitudes and practices related to cancer screening and cancer prevention clinical trials. Pac Health Dialog. 2004 Sep;11(2):160–5. [PubMed] [Google Scholar]
- 10.Meredith LS, Mendel P, Pearson M, et al. Implementation and maintenance of quality improvement for treating depression in primary care. Psychiatr Serv. 2006 Jan;57(1):48–55. doi: 10.1176/appi.ps.57.1.48. [DOI] [PubMed] [Google Scholar]
- 11.Graham IM, Stewart M, Hertog MG. Factors impeding the implementation of cardiovascular prevention guidelines: findings from a survey conducted by the European Society of Cardiology. Eur J Cardiovasc Prev Rehabil. 2006 Oct;13(5):839–45. doi: 10.1097/01.hjr.0000219112.02544.24. [DOI] [PubMed] [Google Scholar]
- 12.Miller PM, Stockdell R, Nemeth L, et al. Initial steps taken by nine primary care practices to implement alcohol screening guidelines with hypertensive patients: the AA-TRIP project. Subst Abus. 2006 Jun;27(1-2):61–70. doi: 10.1300/J465v27n01_08. [DOI] [PubMed] [Google Scholar]
- 13.MacGregor K, Handley M, Wong S, et al. Behavior-change action plans in primary care: a feasibility study of clinicians. J Am Board Fam Med. 2006 May-Jun;19(3):215–23. doi: 10.3122/jabfm.19.3.215. [DOI] [PubMed] [Google Scholar]
- 14.Mattocks K, Lalime K, Tate JP, et al. The state of physician office-based health information technology in Connecticut: current use, barriers and future plans. Conn Med. 2007 Jan;71(1):27–31. [PubMed] [Google Scholar]
- 15.Helfrich CD, Weiner BJ, McKinney MM, et al. Determinants of implementation effectiveness: adapting a framework for complex innovations. Med Care Res Rev. 2007 Jun;64(3):279–303. doi: 10.1177/1077558707299887. [DOI] [PubMed] [Google Scholar]
- 16.Wolfson D, Bernabeo E, Leas B, et al. Quality improvement in small office settings: an examination of successful practices. BMC Fam Pract. 2009 Feb 9;10:14. doi: 10.1186/1471-2296-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolford SJ, Clark SJ, Ahmed S, et al. Feasibility and acceptability of a 1-page tool to help physicians assess and discuss obesity with parents of preschoolers. Clin Pediatr (Phila) 2009 Nov;48(9):954–9. doi: 10.1177/0009922809338060. [DOI] [PubMed] [Google Scholar]
- 18.Lemay CA, Beagan BM, Ferguson WJ, et al. Lessons learned from a collaborative to improve care for patients with diabetes in 17 community health centers, Massachusetts, 2006. Prev Chronic Dis. 2010 Jul;7(4):A83. [PMC free article] [PubMed] [Google Scholar]
- 19.Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008 Dec;23(12):2058–65. doi: 10.1007/s11606-008-0805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.To T, McLimont S, Wang C, et al. How much do health care providers value a community-based asthma care program? A survey to collect their opinions on the utilities of and barriers to its uptake. BMC Health Serv Res. 2009 May;11:9–77. doi: 10.1186/1472-6963-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doerr E, Galpin K, Jones-Taylor C, et al. Between-visit workload in primary care. J Gen Intern Med. 2010 Dec;25(12):1289–92. doi: 10.1007/s11606-010-1470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baron RJ. What’s keeping us so busy in primary care? a snapshot from one practice. New England Journal of Medicine. 2010 Apr 29;362(17):1632–6. doi: 10.1056/NEJMon0910793. [DOI] [PubMed] [Google Scholar]
- 23.Farber J, Siu A, Bloom P. How much time do physicians spend providing care outside of office visits? Ann Intern Med. 2007 Nov 20;147(10):693–8. doi: 10.7326/0003-4819-147-10-200711200-00005. [DOI] [PubMed] [Google Scholar]
- 24.Gottschalk A, Flocke SA. Time spent in face-to-face patient care and work outside the examination room. Ann Fam Med. 2005 Nov-Dec;3(6):488–93. doi: 10.1370/afm.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen MA, Hollenberg JP, Michelen W, et al. Patient care outside of office visits: a primary care physician time study. J Gen Intern Med. 2011 Jan;26(1):58–63. doi: 10.1007/s11606-010-1494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stange KC, Miller WL, Nutting PA, et al. Context for understanding the National Demonstration Project and the patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):S2-8–S92. doi: 10.1370/afm.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.James BC. Learning opportunities for health care. In: Grossmann C, Goolsby WA, Olsen LA, et al., editors. Engineering a learning healthcare system: a look at the future: workshop summary. The National Academies Press; Washington, DC: 2011. [Google Scholar]
- 28.Reid PP, Compton WD, Grossman J, et al. Building a better delivery system: a new engineering/health care partnership. National Academy Press; Washington, DC: 2005. [PubMed] [Google Scholar]
- 29.Kossiakoff A, Sweet W. Systems engineering principles and practice. Wiley; New York, NY: 2003. [Google Scholar]
- 30.Kopach-Konrad R, Lawley M, Criswell M, et al. Applying systems engineering principles in improving health care delivery. J Gen Intern Med. 2007 Dec;22(Suppl 3):431–7. doi: 10.1007/s11606-007-0292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weed J. Factory efficiency comes to the hospital. The New York Times; New York, NY: Jul 9, 2010. [Google Scholar]
- 32.McJoynt TA, Hirzallah MA, Satele DV, et al. Building a protocol expressway: the case of Mayo Clinic Cancer Center. J Clin Oncol. 2009 Aug 10;27(23):3855–60. doi: 10.1200/JCO.2008.21.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Womack JP, Jones DT. Lean thinking. Free Press; New York, NY: 2003. [Google Scholar]
- 34.Nelson-Peterson DL, Leppa CJ. Creating an environment for caring using lean principles of the Virginia Mason Production System. Journal of Nursing Administration. 2007 Jun;37(6):287–94. doi: 10.1097/01.NNA.0000277717.34134.a9. [DOI] [PubMed] [Google Scholar]
- 35.Jimmerson C. Value-stream mapping for healthcare made easy. Productivity Press; New York, NY: 2009. [Google Scholar]
- 36.Graban M. Lean hospitals: improving quality, patient safety, and employee satisfaction. Productivity Press; New York, NY: 2008. [Google Scholar]
- 37.Rother M, Shook J. Learning to see: value-stream mapping to add value and eliminate muda. Lean Enterprise Institute Inc.; Cambridge, MA: 2009. [Google Scholar]
- 38.Aherne J, Whelton J, editors. Applying lean in healthcare: a collection of international case studies. Productivity Press; New York, NY: 2010. [Google Scholar]
- 39.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science; London, England: 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanchard BS, Fabrycky WJ. Systems engineering and analysis. 5th ed. Upper Saddle River, NJ; Prentice Hall: 2010. [Google Scholar]
- 42.Fish A, George S, Terrien E, et al. Workflow concerns and workarounds of readers in an urban safety net teleretinal screening study. AMIA; Hollywood, CA: 2011. [PMC free article] [PubMed] [Google Scholar]
- 43.International Community Health Services . Annual report. International Community Health Services; Seattle, WA: 2010. [Google Scholar]
- 44.Tu SP, Taylor V, Yasui Y, et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. 2006 Sep 1;107(5):959–66. doi: 10.1002/cncr.22091. [DOI] [PubMed] [Google Scholar]
- 45.National Cancer Institute . Colorectal cancer screening in Chinese Americans Project. National Cancer Institute; Washington, DC: 2011. [Google Scholar]
- 46.Freivalds A, Niebel B. Niebel’s methods, standards, and work design. 12th ed. McGraw Hill; New York, NY: 2008. [Google Scholar]
- 47.Cady R, Finkelstein S, Lindgren B, et al. Exploring the translational impact of a home telemonitoring intervention using time-motion study. Telemed J E Health. 2010 Jun;16(5):576–84. doi: 10.1089/tmj.2009.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dickson EW, Anguelov Z, Vetterick D, et al. Use of lean in the emergency department: a case series of 4 hospitals. Ann Emerg Med. 2009 Oct;54(4):504–10. doi: 10.1016/j.annemergmed.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 49.Deckard GJ, Borkowski N, Diaz D, et al. Improving timeliness and efficiency in the referral process for safety net providers: application of the Lean Six Sigma methodology. Journal of Ambulatory Care Management. 2010 Apr-Jun;33(2):124–30. doi: 10.1097/JAC.0b013e3181d91670. [DOI] [PubMed] [Google Scholar]
- 50.Zai AH, Grant RW, Estey G, et al. Lessons from implementing a combined workflow-informatics system for diabetes management. J Am Med Inform Assoc. 2008 Jul-Aug;15(4):524–33. doi: 10.1197/jamia.M2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007 Feb;16(1):2–3. doi: 10.1136/qshc.2006.022046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hassell LA, Glass CF, Yip C, et al. The combined positive impact of lean methodology and Ventana Symphony autostainer on histology lab workflow. BMC Clin Pathol. 2010 Feb 8;10:2. doi: 10.1186/1472-6890-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Raab SS, Andrew-Jaja C, Grzybicki DM, et al. Dissemination of lean methods to improve Pap testing quality and patient safety. J Low Genit Tract Dis. 2008 Apr;12(2):103–10. doi: 10.1097/LGT.0b013e31815ae9a1. [DOI] [PubMed] [Google Scholar]
- 54.Malhotra S, Jordan D, Shortliffe E, et al. Workflow modeling in critical care: piecing together your own puzzle. J Biomed Inform. 2007 Apr;40(2):81–92. doi: 10.1016/j.jbi.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 55.Aboumatar HJ, Winner L, Davis R, et al. Applying Lean Sigma solutions to mistake-proof the chemotherapy preparation process. Joint Commission Journal on Quality and Patient Safety. 2010 Feb;36(2):79–86. doi: 10.1016/s1553-7250(10)36014-4. [DOI] [PubMed] [Google Scholar]
- 56.Harmelink S. Performance improvement using methodology: case study. Radiol Manage. 2008 Sep-Oct;30(5):62–5. [PubMed] [Google Scholar]
- 57.Magill MK, Day J, Mervis A, et al. Improving colonoscopy referral rates through computer-supported, primary care practice redesign. J Healthc Qual. 2009 Jul-Aug;31(4):43–52. doi: 10.1111/j.1945-1474.2009.00037.x. quiz 52-43. [DOI] [PubMed] [Google Scholar]