Abstract
In both social science and medicine, research on reproduction generally focuses on women. In this article, we examine how men’s reproductive contributions are understood. We develop an analytic framework that brings together Cynthia Daniels’ conceptualization of reproductive masculinity (2006) with a staged view of reproduction, where the stages include the period before conception, conception, gestation, and birth. Drawing on data from two medical sites that are oriented to the period before pregnancy (preconception health care and sperm banks), we examine how gendered knowledge about reproduction produces different reproductive equations in different stages of the reproductive process. We conclude with a new research agenda that emerges from rethinking the role of men and masculinity in reproduction.
Keywords: gender, reproduction, men, masculinity, preconception care, sperm banks
Most research on reproduction is about women. Whether the studies are conducted by social scientists or clinicians, whether they rely on qualitative methods or quantitative methods, the focus is on women’s experiences and women’s bodies. For example, sociologists and anthropologists have written extensively about women’s experiences of pregnancy, prenatal screening, abortion, and birth (e.g., Ginsburg and Rapp 1995; Jordan 1983; Luker 1984; Rothman 1986), but have published just a handful of studies on men’s experiences in these realms (e.g., Inhorn et al. 2009). To many people, the focus on women makes sense, as it is within their bodies that conception, gestation, and birth occur. However, the lack of attention to men in research on reproduction leaves open many important questions, including how men’s reproductive contributions are understood.
As one way of answering these questions, Cynthia Daniels has developed the concept of “reproductive masculinity,” which consists of the following interrelated assumptions: that men are secondary to biological reproduction, that they are less vulnerable to reproductive harm than women, that they are virile, and that they are relatively distant from the health problems of the children they father (Daniels 2006, 6–7). In this article, we seek to build on this framework by examining whether these assumptions hold in all reproductive situations or whether there is variation in how men’s contributions to reproduction are perceived. Specifically, we find it useful to examine the tenets of reproductive masculinity within each stage of the reproductive process, from the period before conception, to conception, gestation, and birth. This makes it possible to ask, for example, whether the view of men as secondary to biological reproduction is associated more with pregnancy and birth than it is with conception.
Recognizing the cultural power of medicine and science to define bodies and bodily processes (Clarke et al. 2010), we focus our analysis on two medicalized sites. The first is a new public health initiative touting the importance of “preconception health,” which encourages people to prepare their bodies for reproduction before pregnancy occurs. The second is the sperm bank, where men are screened on the basis of health and virility before being paid to produce reproductive material. In contrast to sites where the focus is on pregnancy or birth, both of these sites are oriented to the period before and during conception, which opens up the possibility of more attention to men’s reproductive contributions. Through interviews, observations, and content analyses, we find that clinicians’ ideas about reproductive masculinity differ depending on the stage in reproduction, leading them to produce varying “reproductive equations” for calculating men’s contributions. We conclude by discussing the implications of our results, and we generate a new research agenda that emerges from rethinking the role of men and masculinity in reproduction.
GENDERED KNOWLEDGE AND REPRODUCTION
Medical knowledge has long served as a powerful resource for justifying cultural gender norms, a trend that was only magnified with the rising social significance of scientific and biological knowledge in recent centuries (Rosenberg and Smith-Rosenberg 1997 [1976]). Scientific and medical claims about women and men are shaped by normative expectations about their proper roles in society, as well as ideals of femininity and masculinity (Ehrenreich and English 2005 [1978]; Laqueur 1990). Moreover, medical knowledge is not only gendered, it is also gendering (Lorber 1993): It shapes definitions of the “standard” human (Epstein 2007), how clinicians research and treat disease (e.g., Kempner 2006), and the development of pharmaceuticals and medical technologies (Blum and Stracuzzi 2004; Mamo and Fishman 2001), such as contraception (Campo-Engelstein 2011; Oudshoorn 2003).
At the same time, women have received more attention than men in social scientific studies of medicine, in part because of concerns that they were more often victims of medical interventions (Riessman 1983; Riska 2003). While there has been some analysis of medicalized masculinities (e.g., Rosenfeld and Faircloth 2006), research on “gender” still tends to focus on women, both in medicine in general and in reproduction in particular. This simultaneous attention to women and inattention to men are both produced by and contributors to gendered knowledge about reproduction.
Indeed, Inhorn and colleagues have called for a reconception of men in reproduction, one that does not leave them out of the “reproductive equation” (Inhorn et al. 2009, 3). Yet, the dearth of research provides little guidance for how to do this. In essence, we found two kinds of studies. The first group focuses on men’s experiences of reproduction, including conception (Higgins, Hirsch, and Trussell 2008), contraception (Gutmann 2007), their partner’s pregnancies (Locock and Alexander 2006; K. Reed 2009), birth (Leavitt 2009; R. Reed 2005), and infertility (Becker 2000). The second group focuses on biomedical approaches to sperm, including how it has been scrutinized by scientists in the twentieth century (Clarke 1998; Moore 2007), how it is affected by exposure to toxins (Daniels 2006), how it is portrayed in medical textbooks (Martin 1991), and how it is packaged and sold for use in assisted reproduction (Almeling 2011). Within and between these two strands of literature, there are many questions about the relationship between individual experiences and medical knowledge, a topic to which we return in the discussion. Our analytic focus, though, is squarely on the medical profession: In what ways does gendered knowledge about reproduction shape how clinicians think about men’s reproductive contributions?
To construct a conceptual framework for this analysis, we bring together Daniels’ discussion of “reproductive masculinity” (2006, 6–7) with a staged view of reproduction, where the stages include the period before conception, conception, gestation, and birth. Whereas Daniels traces the social history of each element of reproductive masculinity, we examine whether and how the four elements vary in different stages of the reproductive process.1 First, are men consistently seen as secondary to biological reproduction, even in the period before and during conception? Second, is there more concern about men’s vulnerability to reproductive harm in earlier stages of the reproductive process? Third, are clinicians uniform in perceiving men as virile? Fourth, to what extent are men perceived as distant from the health problems of their children, and does the distance increase in later stages of reproduction? Specifying stages within the reproductive process opens up the conceptual possibility that there may be variation in how men’s part in the reproductive equation is calculated.
Moreover, expanding the analytic framework of reproduction to include the period before conception (and focusing our data collection at sites where this is the time period of interest) creates at least the theoretical possibility that men’s contributions to reproduction will be considered alongside women’s. Whereas conception (usually2), gestation (always), and birth (always) occur within female bodies, the period before conception is one in which family health history and current health behaviors matter for women and men alike. This could produce a reproductive equation in which women and men are perceived as making equal contributions to conception, either in terms of the number of cells (one egg + one sperm), the amount of genetic material (23 chromosomes + 23 chromosomes), the health of the body producing those cells, or the status of that body’s family history. However, it is possible that the strong association between women’s bodies and reproduction overwhelms all consideration of men’s reproductive contributions, even during the period of time before conception.
In sum, rather than approaching reproduction qua reproduction writ large, we look to particular stages to assess how clinicians figure men’s role in the reproductive equation. We do so in sites where we expect there to be some discussion of men’s contributions to conception, gestation, and birth. This allows us to specify when and how notions of reproductive masculinity contribute to varying reproductive equations, and it offers insights about how clinicians are both responding to and creating gendered medical knowledge about reproduction.
SITE SELECTION, METHODS, AND DATA
There are few places in the social world where men’s reproduction takes center stage. The sperm bank is one, and a recent public health initiative devoted to preconception care also offers at least the possibility that men’s reproductive contributions will be considered alongside women’s. Although these two sites were originally chosen for other projects (Almeling 2011; Waggoner 2013), we found that comparing them offers a number of distinct opportunities for examining how clinicians figure men’s role in reproduction. First, we provide a brief description of each site before elaborating on the analytical leverage we gain through the comparison.
Preconception Health
Despite decades of concerted policy efforts to improve infant health in the United States, rates of adverse birth outcomes remained stubbornly high through the 1980s. Deeming the model of prenatal care insufficient because the interventions came too late, maternal and child health experts turned to a new initiative: preconception care. Beginning in 2004, the Centers for Disease Control and Prevention (CDC) convened experts from various disciplines to construct this new framework for treating women’s and men’s bodies prior to pregnancy (see Casper and Moore 2009; Johnson et al. 2006), formally launching the “Preconception Health and Health Care Initiative” (PCHHC). The basic idea is to locate, modify, and treat negative health behaviors before a pregnancy occurs. Clinicians screen women and men for disease, urge them to attain a healthy weight, and counsel them to eliminate behaviors, such as smoking, that might adversely affect conception or fetal development. This shift in focus from prenatal interventions to the period prior to conception has resulted in a recommendation that is generally directed at women to treat pregnancy as if it lasts 12 months (see Waggoner 2013).
Sperm Banks
Sperm donation programs have been operating in the United States since the early 1900s. Serving heterosexual couples contending with infertility and, more recently, lesbian couples and single women, sperm banks profess to offer “high-quality” sperm samples that will help clients have healthy children.3 To this end, men applying to become donors are subjected to medical, genetic, and social assessments. Fewer than 10 percent of applicants make it through the months-long screening process, and those who do must commit to weekly donations for one year. Moreover, every visit to the sperm bank must be preceded by 48 hours of abstinence to ensure a high sperm count. In addition to monitoring their sexual activities, sperm donors are counseled to eat healthy foods, avoid stress, and reduce alcohol consumption, all of which can affect sperm count. And sperm donors pay attention to this advice, because if their sperm count falls below bank standards, they are not paid for that day’s deposit (see Almeling 2011).
The Comparison
Both sites are oriented to the period prior to pregnancy, which creates a space for men’s reproductive contributions to be considered. However, the sites differ in that clinicians working on preconception health are actively constructing the tenets of a new model of care, while clinicians working in sperm banks are putting those tenets into practice. To be clear, there is no direct conversation between these two sites, and sperm bank staff do not use the language of “preconception care” in detailing their protocols for screening and monitoring donors. However, that is exactly what sperm banks are doing as they test men for disease and encourage them to engage in healthy behaviors. In this sense, sperm banks are in the day-to-day business of men’s preconception health care. In comparing these two sites, then, we are able to see how clinicians define men’s role in reproduction (or ignore it) at the level of both knowledge and practice.
While it is the case that most men will never step foot in a sperm bank, and the preconception health framework is still gaining prominence, the clinicians who work in these spaces were trained within the same system of medical education as clinicians who do not work in these specialized sites. As such, we take their words to represent something broader about how biomedical and scientific discourses position men in the realm of reproduction. In the following analysis, we take care in pointing to some of the specificities of these sites (such as the visibility of sperm count in sperm banks), but it is worth noting that the recommendations issued by the PCHHC Initiative are ostensibly aimed at all people of reproductive age. Given that these are among the few sites in which one would expect to find explicit accounts of men’s role in reproduction, we examine those accounts in order to shed light on the relationship between gender, medical knowledge, and clinical practice.
Data And Analysis
As part of a larger project on the emergence of the preconception care paradigm, Waggoner conducted interviews in 2010–2011 with 57 experts drawn from the select panel and expert working groups within the CDC’s PCHHC Initiative. Interviewees include prominent scientists (epidemiologists, behavioral scientists, and geneticists), clinicians (obstetricians, pediatricians, family practitioners, and nurses), and public health and policy experts. In addition, using the MEDLINE database, Waggoner conducted a content analysis of the preconception research literature published between 1980 and 2010.
As part of a larger project on sperm and egg donation, Almeling interviewed the founders of commercial sperm donation programs in the United States, nationally prominent clinicians and researchers who specialize in assisted reproduction, and staffers from four sperm banks. The banks were chosen to reflect diversity in terms of size, longevity, geography, and tax status, and they include two of the oldest and largest commercial sperm banks, the only nonprofit sperm bank in the country, and a small sperm bank located in the obstetrics and gynecology division of a major research university. All interviews were conducted between 2002 and 2006.
For the purposes of this analysis, each author selected a subset of interviews to code. From the PCHHC data set, we coded any interview in which the respondent mentioned men (n = 29) and the few research articles that discussed men in a substantive way. From the sperm donation data set, we coded interviews with respondents who met two criteria: They worked with donors in a sperm bank or infertility practice, and they had some form of medical or scientific training, which ranged from lab technicians to PhDs and MDs (n = 16). All interviews were recorded and transcribed in full.
Initially, each author searched her own transcripts for instances in which respondents discussed men’s contributions to reproduction. Then, we both reviewed all of the selected excerpts and developed two main codes: (1) men’s contributions to conception and (2) men’s contributions to fetal development and gestation. As we analyzed the combined data, it became clear that men’s reproductive contributions are discussed in dramatically different ways—from incredibly significant to virtually unknown—depending on the stage in the reproductive process.
REPRODUCTIVE EQUATIONS
While sperm bank staffers are squarely focused on men’s bodies and men’s behavior, the scientists and clinicians working to promote preconception care generally focus their attention on women’s bodies and women’s behavior. Yet, about half of the preconception health interviewees made some reference to men. The statements were often vague, as when a behavioral scientist, an obstetrician, and a nurse all used the same language to say that “men are part of the equation.”
What follows is a conceptual mapping of just how it is that men’s “part” in the reproductive equation is figured, both by those who create such knowledge and those who put it into practice. First, we demonstrate that clinicians understand men’s reproductive contributions as incredibly important when it comes to conception, but that men are of declining significance in subsequent stages of reproduction. Such variation stands in sharp contrast to Daniels’ suggestion that men are generally considered secondary to biological reproduction. However, it is consistent with a truly ancient and yet persistent idea of men as providing the creative spark of life with their “seed” while women provide the nurturing “soil” (Delaney 1986), a formulation that positions men’s role in conception as significant and their role in gestation as insignificant.
Second, we examine the generalized sense among our respondents that much about men’s part in the reproductive equation remains unknown. This finding concurs with Daniels’ argument that assumptions about men as less vulnerable to reproductive harm and relatively distant from the health problems of their offspring have stifled research on men’s contributions to reproduction. Drawing on interviews with those who work in sites where such information is crucial and yet remains elusive allows us to provide additional insights about how gendered knowledge or, in this case, non-knowledge, is produced and enacted.
Men’s Role in Conception = Significant
When it comes to conception, men are often portrayed as constituting the primary component of the reproductive equation because they are understood as the active agent in establishing a pregnancy. This belief is evident in a comment from the founder of one of the first commercial sperm banks, who described infertile men as “individuals who frankly had bad sperm, and that’s why they weren’t getting people pregnant.” In another example, a lab technician at a sperm bank mentioned to a donor, “There’s a woman that says that she’s become pregnant with your samples.” Such views stem from ancient Greek ideas about the role of men in creating life (Delaney 1986) and are reflected today in colloquialisms like “He got her pregnant” or, more crudely, “He knocked her up.” In effect, sperm is understood as the entity that produces a pregnancy, not eggs (Martin 1991), and this positions men as incredibly significant in the earliest stages of reproduction, before and during conception.
In sperm banks, the focus on male seed is due in part to its visibility. Indeed, sperm is on display in a way that is not at all the case when people reproduce using old-fashioned methods. Sperm count is one of the primary criterion on which prospective donors are assessed, and once they are accepted into the program, men must produce “samples” on a regular basis. Lab technicians evaluate those samples to assess sperm count and morphology, as well as the volume of seminal fluid. In the words of an embryologist at an academic medical center, sperm donors are “highly selected.”
[They should have] high sperm counts, good motility, vigorous moving sperm, and you would like to have a known fertility status on the donor.4 Now we’re adding sperm morphology, because morphology and function are very tightly connected with sperm. Everything is kind of put together for one purpose: transporting DNA.
While it may be the case that men are generally assumed to be virile, there are certainly spaces in which that assumption does not hold. Sperm banks are one such site, where men and their sperm are subject to a variety of tests to ascertain virility.
Like sperm bank staffers, preconception care advocates point to the impact of men’s behavior on the quality and quantity of sperm, which can affect both the chances of conception and the health of the resulting offspring. They cite evidence for how men’s use of alcohol and drugs, as well as their exposure to toxins and even advancing age, can damage DNA and lead to birth defects (de Weerd and Steegers 2002; Frey et al. 2008). Frey and colleagues suggest that “improving men’s preconception health can result in improved pregnancy outcomes by enhancing men’s biologic and genetic contributions to the pregnancy conception” (Frey et al. 2008, S389). Such arguments point to an intriguing discrepancy in how the elements of reproductive masculinity operate at this early stage: While men often receive credit for establishing a pregnancy, they are not assigned much responsibility for fetal health (see also Rapp 1999, 88). As a result, preconception care researchers have to work to create a conceptual link between men’s behavior around the time of conception and pregnancy outcomes.
In sperm banks, though, the effects of men’s behavior are visible on a daily basis. As one donor manager explained, “After a while, we get to know what their [sperm] counts are normally like, and whenever they go down, I’m immediately asking them, ‘Have you been sick? Are you under a lot of stress? Have you been sleeping alright?’” A lab technician at another sperm bank specifically mentioned the effects of alcohol and cigarette smoking:
I can tell if they’ve gone out and partied the night before. If they have increased alcohol consumption, or cigarettes are another big one, they create round cells, and it’s like immature cells or white cells in their specimen. One of the doctors I spoke to in California said [she’s] noticed [it] with marijuana smokers too.
Since sperm counts must be high enough for samples to be accepted, ensuring that men engage in healthful behaviors is necessary for ensuring the financial stability of the bank.
In both preconception care and sperm banks, then, there is no sense in which men are considered invulnerable to reproductive harm. Indeed, as one nurse in a university’s donation program noted, “Sperm is very sensitive to lots of internal and external issues.” Thus, at this early stage in the reproductive process, men’s part in the reproductive equation is calculated as incredibly significant, both in terms of their role in establishing a pregnancy and in contributing to fetal health outcomes.
50/50
The idea that sperm is the active agent in establishing a pregnancy coexists with the idea that men and women contribute equally to reproduction. As one obstetrician involved in preconception care noted, “[Men] are part of the equation, 50 percent of the equation to be exact.” Figuring the reproductive equation as 50/50 occurred most often in the context of discussing genetic contributions to the embryo. Depending on whether respondents worked in a context where the focus is usually on the woman, as in preconception care, or usually on the man, as in sperm banks, they took care to note that “half” of the genes would come from the other sex. An epidemiologist who does research on preconception care noted that “half of the biologic predisposition comes from the father of the fetus.” A genetic counselor at a sperm bank often felt the need to remind recipients that “of course the child’s going to have half of the woman’s genes.”
More than just referencing genes, those working in both sites underscored the “equal importance” of men’s and women’s family health history. The goal is to identify “red flags,” medical conditions or predispositions that could negatively affect fetal development or contribute to health problems in children. A geneticist involved in preconception care explained that “in terms of family history, men are equally important” but that “sometimes that gets left out of the discussion.” This is just one effect of the disproportionate focus on women in the realm of preconception care, and it is not at all the case in sperm banks, where the evaluation of men’s health history is a crucial part of the extensive screening process. Men applying to be donors provide not only their own medical history but their parents’ and grandparents’, while also submitting to genetic tests. The end result, according to a commercial sperm bank founder, is sperm that is “a medical product. It’s well-characterized material intended for use with counseling by a physician just like a prescription drug.”
Nevertheless, there are still occasions in which women who have conceived with donated sperm report concerns about their pregnancies or children. As a result, sperm banks have developed detailed organizational procedures for handling what they call “donor offspring problems” and “adverse outcome reports.” Here, a genetic counselor at one of the largest sperm banks in the country describes this component of her job:
If something comes up once the patient’s pregnant, and people are starting to be concerned as to the health of the fetus, or the child is born with a problem at birth, or a child develops problems along the way, then [my department] handles that. Now, sometimes it’s not really an adverse outcome because it turns out to be okay, but in the moment that we’re contacted: “What is this? Have we seen this in other offspring or pregnancies? This isn’t in my family. Did the donor not tell us?” Most of the time, it’s not donor related, and many times it’s not even related to the mother. Patients call up with things like, “My child has allergies,” “My child is not walking yet,” or “My child’s head looks a little big,” or it can be something very serious—childhood cancers, fetuses developing abnormally in the uterus. In a couple of cases, the disorder is not in either parent. It’s a new mutation in the child, and it’s kind of just bad luck.
Sperm bank staffers take for granted the importance of men’s contributions to the health of offspring. In fact, this is the basis for business in a sperm bank, and ensuring the “quality” of the “product,” as one clinical director put it, is a foremost concern.
Whereas Daniels contends that men are generally perceived as secondary to biological reproduction, we find that when it comes to genetics and family history, women and men are assigned equal parts in the reproductive equation. Such calculations also stand in contrast to traditional notions of men providing the seed and women providing the soil, which position each sex as significant or insignificant in conception and gestation. When clinicians shift their attention from these sorts of embodied processes to thinking about genetics, they engage in less hierarchical reproductive calculations, privileging neither the contributions of women nor men.
Men’s Role in Pregnancy = Insignificant
While men’s reproductive contributions are seen as very significant when it comes to conception and equal to women’s when it comes to genetics, their role in pregnancy is understood as negligible. Among those working in preconception care, there was little discussion of men in this stage of the reproductive process. When it was mentioned, that role was primarily defined in terms of “how they could be supportive” of the pregnant woman, as one public health expert put it. As part of being able to offer such support, men are encouraged to create “reproductive health plans” and to “deliberately decid[e] before a conception if and when one would like to become a father” (Moos 2010, 564). Indeed, one epidemiologist expressed a desire to “stop putting it all on women”:
I want us to start talking to men and boys. “When do you want to get somebody pregnant? What do you want for your future? How are you going to support your partner when she does get pregnant?” I just feel like everything, a lot of things, especially with pregnancy or even family planning, is always put on the women. I think we really, really, really need to shift that conversation [and] understand that pregnancy happens in a partnership.
Even as she mentions the significance of men in conception (“getting somebody pregnant”), this researcher, like many who work in preconception care, understands a reproductive “partnership” primarily as a social relationship, one in which the man is a potential source of support before and during pregnancy.
However, that social relationship can also have biological effects on a pregnancy, as when men engage in behaviors that can negatively affect a developing fetus. As one public health expert put it, “Men who drink, men who use drugs, men who smoke all pose risks to a healthy pregnancy.” In this sense, men can have a direct impact on gestational outcomes, which counters the traditional view that because pregnancy happens in women’s bodies, men’s role is purely “social” at this stage in the reproductive process.
Yet, even among those who acknowledge that men do make some contribution to gestational outcomes, either in terms of sperm quality, behavior, or social support, there is a persistent emphasis on women and the “uterine environment.” For example, an obstetrician working in preconception care explains:
There’s some data to suggest that men [who] work around heavy organic solvents may slightly increase [their] risk of having children with birth defects. But a lot of the data indicate that it’s really the intrauterine environment that’s the most important thing. So although there are a few situations in which the male partner’s health becomes an issue, there are not many. I mean, obviously for genetic diseases, the father’s history is important. The age of the father is important, because if he’s over 40, [there is an] increased risk of certain kinds of genetic problems, [also] fathers taking certain kinds of medications. But ultimately, 98 percent of the evidence suggests it’s [the] intrauterine environment that’s the most important thing.
Even after listing four specific factors associated with men’s bodies and behaviors (exposure to chemicals, family history, age, and medication use), this clinician underscores the connection between women’s bodies and reproductive outcomes. That she bases this assessment on “98 percent” of the evidence demonstrates how the paucity of knowledge about men shapes reproductive equations in such a way that reinforces traditional understandings of men as seed and women as soil.
Unknown
The dearth of research about men’s contributions to reproduction renders much about their part in the reproductive equation unknown. As Daniels notes, cultural norms of masculinity have “skewed” scientific investigations of sperm and left unasked innumerable questions about the role of men in the reproductive process (2006). Even in sites where such information is crucial, such as preconception care and sperm banks, we find that the mutually reinforcing processes of inattention and lack of research contribute to ongoing ignorance and uncertainty, both at the levels of knowledge and practice.
Among the scientists and clinicians actively involved in designing the framework for preconception health care, the overwhelming focus is on preparing women’s bodies for reproduction, one result of which is a profound inattention to men. For example, an epidemiologist noted that “there is a men’s component to preconception care that’s not women’s health. We have to remind ourselves that men are generally involved in reproduction.” Likewise, a national leader in reproductive medicine explained that, simply, “people think of the man as not as important in reproduction as the woman.”
Such inattention to men’s reproductive contributions, evidenced by the need to “remind” oneself that they are “generally involved” in reproduction, translates into an absence of clinical research on how men matter. The same epidemiologist explained that the “majority” of articles on preconception care do not discuss men at all, or mention them only briefly. Indeed, in an introduction to a comprehensive supplemental issue of the American Journal of Obstetrics & Gynecology (AJOG) on preconception health, the authors discussed 84 different risk factors and components of preconception care (Jack et al. 2008). Rather than including men in categories such as alcohol or illicit drug use, they are assigned to a catch-all category at the end labeled “men.”
Even as preconception health advocates point to the lack of research on exactly how men matter, they do make occasional references to the importance of including men in this kind of care. For example, one public health specialist explained that preconception health is important because of “what we know about the health impacts of the things that women and potentially men do prior to becoming pregnant.” These depictions of men’s potential to matter in reproductive outcomes reveal that even when experts include men in these discussions, they still evince little working knowledge of exactly how they matter. As a result, the inattention to men’s role in reproduction is reinforced by a lack of data about their contributions and vice versa.
While preconception health researchers sometimes express frustration about the unknowns of men’s reproductive contributions, those working in sperm banks navigate them on a daily basis, doing their best to avoid even potential risks. Indeed, because sperm banks are often in the position of operating under conditions of uncertainty about what exactly constitutes a medical risk, they have created medical advisory boards. The donor manager for a large commercial sperm bank explains:
We operate entirely by standard operating procedure that outlines what medical criteria will make a donor not eligible. Those criteria are partly set forth by regulatory standards. But some things aren’t addressed. We have a medical advisory board that decides, for example, how many heart attacks, or just what in a family history would make it so the guy is considered high risk, like one or two incidences of this type of cancer. So we have a medical advisory board that helps us set criteria for screening donors based on family background.
As in this case, sometimes the lack of knowledge stems from the still–evolving science of calculating disease risks on the basis of genetics or family history, a form of uncertainty that affects the analysis of both women’s and men’s contributions to the health of future generations.
In other cases, though, the uncertainty can be traced more directly to a lack of knowledge about how men’s health status affects the chances of conception, as well as fetal health and development. For example, this same donor manager described the medical advisory board’s response to concerns following the Persian Gulf War in 1991:
When the Desert Storm thing came out, when people were coming back, oh, there’s no known disease, they call it Desert Storm Syndrome. People were starting to freak out. “Is my baby going to be orange because I bought a donor?” So the medical board got together and made the decision we don’t want any donor that’s been in the Middle East. So that is on the medical history questionnaire.
Indeed, in sperm banks, decisions about how to evaluate prospective donors are often made with an eye toward how recipients will respond. This nexus of uncertainty and marketing is articulated by a lab technician who also serves as the donor manager in a non-profit sperm bank:
[The donor screener] looks at the history of the donor, any patterns that might be easily visible that might show genetic problems or also any patterns that might be flags for recipients. For example, if there’s a lot of alcoholism, that person’s probably not going to sell, because someone choosing a donor is going to want someone that doesn’t have this very repetitive problem.
While it is certainly the case that most women will not be in the position of choosing among many potential sperm donors, this unique site throws into stark relief the lack of detailed information about the exact nature of men’s contributions to reproductive outcomes.
DISCUSSION AND CONCLUSION
Scientists and clinicians working in reproductive medicine are operating under the aegis of varying reproductive equations, which leads them to figure men’s contributions to conception as significant, their contributions to genetics as equal to women’s, and their contributions to gestation as insignificant. At the same time, both preconception care advocates and sperm bank staff admit to having little concrete data on which to base their assessments. As a result, evidence of men’s fluctuating significance throughout the reproductive process, together with the profound lack of scientific knowledge in this realm, suggests that calculations about men’s part in the reproductive equation are determined not only by biology but by the social context in which they are being generated.
An important part of the social context is provided by norms of reproductive masculinity, a concept to which we add nuance by finding variation in how its constituent elements are mobilized in different reproductive stages and in different reproductive sites. In the initial stages of reproduction, men are assigned a primary role, while in later stages they are assigned a secondary role. This view of men’s contributions is rooted in ancient Greek portrayals of conception and gestation that have contemporary resonance (Almeling 2011; Delaney 1986). Shifting definitions of men’s role, from conception to gestation and birth, provide different ways of calculating the reproductive equation. Fundamentally, reproductive masculinity is about how men’s contributions to reproduction are understood, and thus it is crucial to specify when, where, and why there is variation in such calculations.
Reproductive equations are powerful not only in the making of clinical practice but in the production of medical knowledge. In evaluating why there is still so little research about how men and their sperm matter for reproductive outcomes (Daniels 2006), we point to the widespread and stubborn belief among our respondents in the overriding significance of women’s role in reproduction. As one nurse involved with the CDC’s PCHHC Initiative put it, “We can’t get around it; it’s not the man having the baby.” That this is true even among those who focus on the period before conception, which ostensibly offers an opening for thinking in more egalitarian ways, suggests the intransigence of gendered ways of figuring reproductive equations. The end result is deeply gendered knowledge about reproduction that simultaneously leaves open social and clinical questions about men while reinforcing women’s part of the equation through research and medical practice.
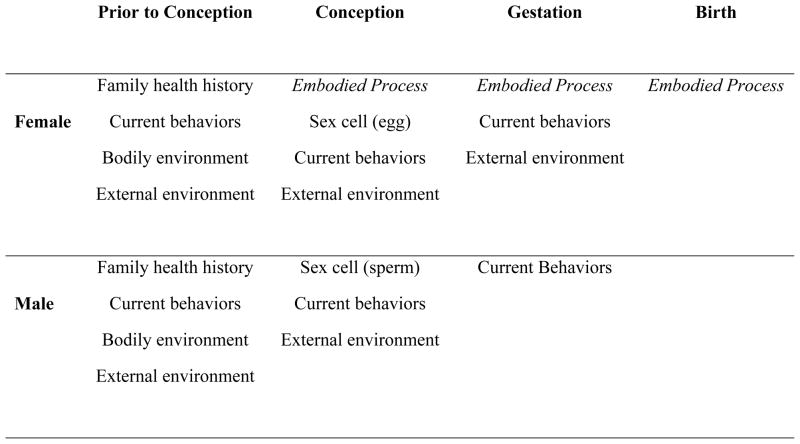
To counter the overwhelming focus on women in both the social scientific and medical literature on reproduction, we propose the following schematic as a way of thinking about women’s and men’s reproductive contributions (see Figure 1). Whereas most scholarship on reproduction focuses on biological difference, we suggest that it would be analytically productive to examine points of similarity, while also continuing to pay attention to difference. To that end, we outline the contributions that women and men make at each stage of the process. Representing reproduction in this way makes it possible to see similarities between women’s and men’s role in the period prior to conception and during conception, while it also takes into account the increasing significance of female bodies in subsequent stages of gestation and birth. Yet, it is important to note that men still matter, even when it comes to pregnancy.
Figure 1. Women’s and Men’s Reproductive Contributions by Stage.
Note: Since we are interested in biological similarities and differences, we have represented the two partners as female and male, but the chart could be adapted for single parents, same-sex couples, and those who use reproductive technologies such as egg/sperm donation or surrogacy.
Using this diagram and reflecting on our findings, we suggest a number of new research questions that emerge, particularly in terms of how gendered knowledge about reproductive contributions is produced and put into practice. In terms of the persistent inattention to men by those who create knowledge, focusing on reproduction as a biological and social process that unfolds in a series of stages may make it possible to disrupt the close association of reproduction with women’s bodies and generate new questions about men’s part in the reproductive equation. Whereas non-knowledge can result from controversy (Kempner, Merz, and Bosk 2011), it is more likely in this case that such questions have simply not been thinkable because of cultural constructs around gender and reproduction (cf. Oudshoorn 2003).
To ensure that men’s reproductive contributions do not remain an unknown quantity, we need more research on how men and their sperm actually matter for reproductive outcomes. Calling attention to the ways in which men factor into the equation at various junctures provides support for the small but growing literature on how men matter, both directly, as with paternal age, and indirectly, through behaviors such as alcohol abuse and domestic violence (Armstrong 2003; Kong et al. 2012). To be sure, researchers in the last century had already begun to examine how toxins affect sperm (Clarke 1998; Moore 2007), but there are still many open questions, including the extent to which such exposure impacts the likelihood of conception and gestational development (Moos 2010). Moreover, there is some cultural momentum for these kinds of questions. Recent headlines in The New York Times, such as “Men, Who Needs Them?” and “Why Fathers Really Matter,” showcase not only the growing attention to this issue but also the need for future studies to employ a framework of reproductive equations to sort through seeming incongruities in how men matter.
Thinking in new ways about how reproductive equations are constituted also raises new questions about men’s experiences with reproduction. Rayna Rapp has noted the contrast between Greek beliefs about the importance of sperm and the widespread assumption that women are responsible for “fetal quality and health” (Rapp 1999, 86). She argues that this assigns men “a proprietary interest, but not a practical responsibility, in a pregnancy’s outcome” (Rapp 1999, 88). Yet, scholars who interview men find they do feel some sense of reproductive responsibility (Locock and Alexander 2006; K. Reed 2009). In a study of prenatal testing, Reed finds that “men’s interests in the impact of their genes on the health of the fetus became more pronounced when they were offered screening themselves” (K. Reed 2009, 354), which provides additional support for Inhorn and Wentzell’s (2011) call to examine how medical technology shapes men’s embodiment. Contraception, too, is an arena with the potential for men to fully participate in reproductive behavior (Campo-Engelstein 2011; Terry and Braun 2011).
At the individual level, we need to know more about how men think about conception and gestation (and birth and fatherhood as well). To what extent do they associate their masculinity with their virility? How do they think about their role in reproductive outcomes? In terms of health care, what kinds of advice, if any, do men receive about preparing their bodies for reproduction? Advocates for the preconception health framework tout the motto “Every woman, every time” in referring to the importance of talking with women of reproductive age during every clinical encounter about whether they intend to become pregnant (Waggoner 2013). By way of contrast, in an article about preconception care for men, Frey and colleagues conclude that to ask “busy clinicians” to adhere to what would be the corollary of “Every man, every visit” is not “feasible” (Frey et al. 2008, S393).
The same authors, however, caution against assuming that “all reproductive responsibility (and biologic risk) is held by women” (Frey et al. 2008, S389). We concur, and point to the potential policy implications that would result from taking seriously the role of men in reproduction. For example, insurance companies may be more likely to cover visits in which men’s health is evaluated prior to conception in an effort to reduce birth defects. Already, the Affordable Care Act stipulates that women with private insurance are no longer required to pay a copayment for a preconception health appointment, but excluding men from such coverage continues to obscure their role in reproduction. Paying attention to how reproductive equations influence policy can suggest new and different avenues for improving public health.
Finally, it is important to investigate other causes of variation in how reproductive equations are figured. Our analysis has centered on gendered knowledge and practice in preconception care and sperm banks, which are sites of intentional reproduction. In contrast, about half of the pregnancies in the United States each year are not planned (Finer and Henshaw 2006). To what extent are individual experiences, health care practices, and medical knowledge shaped by the intentionality of the pregnancy? Moreover, given the strong presumption of heterosexuality in reproductive medicine, how are reproductive equations figured when there are different numbers and kinds of parents involved, including single mothers and lesbian and gay couples, not to mention all of the other combinations now possible with reproductive technologies? From a historical perspective, what explains variation in how reproductive equations have been figured in different times and different places?
Our study has critically engaged the meaning, both theoretically and practically, of men’s reproductive contributions in spaces oriented to the period before pregnancy. By examining the nuances of how women and men are positioned within reproductive equations, we offer a lens through which to document, understand, and problematize the ways in which gender and bodies matter for the medical and symbolic construction of responsibility for reproductive outcomes.
Acknowledgments
Both authors received funding from the National Science Foundation (Almeling grant #0602871 and Waggoner grant #1029087), and Miranda Waggoner also received support from the National Institutes of Health (T32 HD007163). We thank Elizabeth Mitchell Armstrong, Joya Misra, Jeff Ostergren, and the anonymous reviewers for comments.
Biographies
Rene Almeling is an assistant professor of sociology at Yale University. She is the author of Sex Cells: The Medical Market for Eggs and Sperm (University of California Press, 2011), and her current research projects include genetic testing, in vitro fertilization, and the history of medical specialization.
Miranda Waggoner is a postdoctoral research fellow with the Office of Population Research at Princeton University. Her work focuses on the social and ethical dimensions of new developments in science, technology, and medicine. Her research on preconception care also appears in the Journal of Health Politics, Policy and Law.
Footnotes
At two points, Daniels does mention fertilization and pregnancy as key moments in the reproductive process (2006, 30, 161), but she does not systematically compare the elements of reproductive masculinity in these two stages.
An exception occurs with in vitro fertilization, which involves placing eggs and sperm in a petri dish.
However, this goal is not always realized, as media reports have revealed cases in which donors have passed on diseases to multiple offspring.
“Known fertility status” refers to whether the man’s sperm has ever produced a pregnancy, either through the donation program or in his own relationships.
Contributor Information
RENE ALMELING, Yale University, USA.
MIRANDA R. WAGGONER, Princeton University, USA
References
- Almeling Rene. Sex cells: The medical market for eggs and sperm. Berkeley: University of California Press; 2011. [Google Scholar]
- Armstrong Elizabeth M. Conceiving risk, bearing responsibility: Fetal alcohol syndrome and the diagnosis of moral disorder. Baltimore: Johns Hopkins University Press; 2003. [Google Scholar]
- Becker Gay. The elusive embryo: How women and men approach new reproductive technologies. Berkeley: University of California Press; 2000. [Google Scholar]
- Blum Linda, Stracuzzi Nena F. Gender in the Prozac nation: Popular discourse and productive bodies. Gender & Society. 2004;18:269–86. [Google Scholar]
- Campo-Engelstein Lisa. No more larking around! Why we need male LARCs. The Hastings Center Report. 2011;41:22–26. doi: 10.1002/j.1552-146x.2011.tb00137.x. [DOI] [PubMed] [Google Scholar]
- Casper Monica J, Moore Lisa Jean. Calculated losses: Taking the measure of infant mortality. In: Casper Monica J, Moore Lisa Jean., editors. Missing bodies: The politics of visibility. New York: New York University Press; 2009. [Google Scholar]
- Clarke Adele E. Disciplining reproduction: Modernity, American life sciences, and “the problems of sex”. Berkeley: University of California Press; 1998. [Google Scholar]
- Clarke Adele E, Mamo Laura, Fosket Jennifer Ruth, Fishman Jennifer R, Shim Janet K., editors. Biomedicalization: Technoscience, health, and illness in the US. Durham, NC: Duke University Press; 2010. [Google Scholar]
- Daniels Cynthia R. Exposing men: The science and politics of male reproduction. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- de Weerd Sabina, Steegers Eric AP. The past and present practices and continuing controversies of preconception care. Community Genetics. 2002;5:50–60. doi: 10.1159/000064631. [DOI] [PubMed] [Google Scholar]
- Delaney Carol. The meaning of paternity and the virgin birth debate. Man. 1986;21:494–513. [Google Scholar]
- Ehrenreich Barbara, English Deirdre. 2005 For her own good: Two centuries of the experts’ advice to women. New York: Anchor; 1978. [Google Scholar]
- Epstein Steven. Inclusion: The politics of difference in medical research. Chicago: University of Chicago Press; 2007. [Google Scholar]
- Finer Lawrence B, Henshaw Stanley K. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Frey Keith A, Navarro Shannon M, Kotelchuck Milton, Lu Michael C. The clinical content of preconception care: Preconception care for men. American Journal of Obstetrics & Gynecology. 2008;199:S389–S395. doi: 10.1016/j.ajog.2008.10.024. [DOI] [PubMed] [Google Scholar]
- Ginsburg Faye D, Rapp Rayna., editors. Conceiving the new world order: The global politics of reproduction. Berkeley: University of California Press; 1995. [Google Scholar]
- Gutmann Matthew. Fixing men: Sex, birth control, and AIDS in Mexico. Berkeley: University of California Press; 2007. [Google Scholar]
- Higgins Jenny A, Hirsch Jennifer S, Trussell James. Pleasure, prophylaxis and procreation: A qualitative analysis of intermittent contraceptive use and unintended pregnancy. Perspectives on Sexual and Reproductive Health. 2008;40:130–37. doi: 10.1363/4013008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inhorn Marcia C, Tjornhoj-Thomsen T, Goldberg H, la Cour Mosegaard M., editors. Reconceiving the second sex: Men, masculinity, and reproduction. New York: Berghahn Books; 2009. [Google Scholar]
- Inhorn Marcia C, Wentzell Emily A. Embodying emergent masculinities: Men engaging with reproductive and sexual health technologies in the Middle East and Mexico. American Ethnologist. 2011;38:801–15. [Google Scholar]
- Jack Brian W, Atrash Hani, Coonrod Dean V, Moos Merry-K, O’Donnell Julie, Johnson Kay. The clinical content of preconception care: An overview and preparation of this supplement. American Journal of Obstetrics & Gynecology. 2008;199:S266–79. doi: 10.1016/j.ajog.2008.07.067. [DOI] [PubMed] [Google Scholar]
- Johnson Kay, Posner Samuel F, Biermann Janis, Cordero José F, Atrash Hani K, Parker Christopher S, Boulet Sheree, Curtis Michele G. Recommendations to improve preconception health and health care—United States: A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. Morbidity and Mortality Weekly Report. 2006;55(RR06):1–23. [PubMed] [Google Scholar]
- Jordan Brigitte. Birth in four cultures. Montreal: Eden Press; 1983. [Google Scholar]
- Kempner Joanna. Uncovering the man in medicine: Lessons learned from a case study of cluster headache. Gender & Society. 2006;20:632–56. [Google Scholar]
- Kempner Joanna, Merz Jon F, Bosk Charles L. Forbidden knowledge: Public controversy and the production of non-knowledge. Sociological Forum. 2011;26:475–500. [Google Scholar]
- Kong Augustine, Frigge Michael L, Masson Gisli, Besenbacher Soren, Sulem Patrick, Magnusson Gisli, Gudjonsson Sigurjohn A, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012;488:471–75. doi: 10.1038/nature11396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laqueur Thomas. Making sex: Body and gender from the Greeks to Freud. Cambridge, MA: Harvard University Press; 1990. [Google Scholar]
- Leavitt Judith Walzer. Make room for daddy: The journey from waiting room to birthing room. Chapel Hill: University of North Carolina Press; 2009. [Google Scholar]
- Locock Louise, Alexander Jo. “Just a bystander”? Men’s place in the process of fetal screening and diagnosis. Social Science & Medicine. 2006;62:1349–59. doi: 10.1016/j.socscimed.2005.08.011. [DOI] [PubMed] [Google Scholar]
- Lorber Judith. Believing is seeing: Biology as ideology. Gender & Society. 1993;7:568–81. [Google Scholar]
- Luker Kristen. Abortion and the politics of motherhood. Berkeley: University of California Press; 1984. [Google Scholar]
- Mamo Laura, Fishman Jennifer R. Potency in all the right places: Viagra as a technology of the gendered body. Body & Society. 2001;7:13–35. [Google Scholar]
- Martin Emily. The egg and the sperm: How science has constructed a romance based on stereotypical male-female roles. Signs. 1991;16:485–501. [Google Scholar]
- Moore Lisa Jean. Sperm counts: Overcome by man’s most precious fluid. New York: New York University Press; 2007. [Google Scholar]
- Moos Merry-K. From concept to practice: Reflections on the preconception health agenda. Journal of Women’s Health. 2010;19:561–67. doi: 10.1089/jwh.2009.1411. [DOI] [PubMed] [Google Scholar]
- Oudshoorn Nelly. The male pill: A biography of a technology in the making. Durham, NC: Duke University Press; 2003. [Google Scholar]
- Rapp Rayna. Testing women, testing the fetus: The social impact of amniocentesis in America. New York: Routledge; 1999. [Google Scholar]
- Reed Kate. “It’s them faulty genes again”: Women, men and the gendered nature of genetic responsibility in prenatal blood screening. Sociology of Health & Illness. 2009;31:343–59. doi: 10.1111/j.1467-9566.2008.01134.x. [DOI] [PubMed] [Google Scholar]
- Reed Richard. Birthing fathers: The transformation of men in American rites of birth. New Brunswick, NJ: Rutgers University Press; 2005. [Google Scholar]
- Riessman Catherine Kohler. Women and medicalization: A new perspective. Social Policy. 1983;14:3–18. [PubMed] [Google Scholar]
- Riska Elianne. Gendering the medicalization thesis. In: Segal Marcia Texler, Demos Vasilikie, Kronenfeld Jennie Jacobs., editors. Gender perspectives on health and medicine: Key themes, advances in gender research. Vol. 7. Waltham, MA: Elsevier; 2003. [Google Scholar]
- Rosenberg Charles E, Smith-Rosenberg Carroll. 1997 The female animal: Medical and biological views of women. In: Rosenberg Charles E., editor. No other gods: On science and American social thought. Baltimore: Johns Hopkins University Press; 1976. [Google Scholar]
- Rosenfeld Dana, Faircloth Christopher A. Medicalized masculinities. Philadelphia, PA: Temple University Press; 2006. [Google Scholar]
- Rothman Barbara Katz. The tentative pregnancy: Prenatal diagnosis and the future of motherhood. New York: Viking; 1986. [Google Scholar]
- Terry Gareth, Braun Virginia. “It’s kind of me taking responsibility for these things”: Men, vasectomy and “contraceptive economies”. Feminism & Psychology. 2011;21:477–95. [Google Scholar]
- Waggoner Miranda R. Motherhood preconceived: The emergence of the preconception health and health care initiative. Journal of Health Politics, Policy and Law. 2013;38:345–71. doi: 10.1215/03616878-1966333. [DOI] [PMC free article] [PubMed] [Google Scholar]