Abstract
Although therapeutic community (TC) treatment is a promising intervention for substance use disorders, a primary obstacle to successful treatment is premature attrition. Because of their prevalence within substance use treatment facilities, personality disorder (PD) diagnoses have been examined as predictors of treatment completion. Prior research on TC outcomes has focused almost exclusively on antisocial personality disorder (ASPD), and the results have been mixed. The current study extends previous research by examining the impact of the 10 Axis II PDs on early (first 30 day) attrition as well as overall time to dropout in a 9-month residential TC. Survival analyses indicated that borderline was the only PD negatively related to overall program retention. In contrast, ASPD, as well as histrionic PD, were related to very early attrition but not to overall program retention. Early assessment and identification of at-risk individuals may improve treatment retention and outcome for TC treatment.
Keywords: survival, antisocial, borderline, histrionic, SNAP
Introduction
Therapeutic community (TC) treatment is a potentially effective psychosocial intervention for reducing substance use, criminality, unemployment, and other psychosocial problems experienced by addicted individuals1. Several large-scale studies2–4 have found significant and sustained improvements following successful completion of a TC typically after 6–12 months of residential treatment5. These multi-site studies indicate that the most stable predictor of positive treatment outcomes is retention in the treatment3–9. Unfortunately, it is common in intensive residential TCs for as many as 50% of residents to drop out within the first month and another 25–40% or more to drop out during subsequent months, often leaving as few as 10% of admissions who receive a moderately to maximally effective dose of this treatment modality10. Identification of factors associated with very early attrition and poor longer term retention is important to help recognize individuals who may be at high risk for poor outcomes and for whom additional intervention might be necessary.
We evaluated the impact of the 10 Axis II personality disorders (PDs) on very early attrition (within first 30 days) as well as overall time to dropout during a 9-month treatment program. PDs are the most common form of co-occurring psychiatric disorder found in TCs11–15 and the severe and persistent cognitive, emotional, interpersonal, and behavioral problems characterizing these disorders contribute to poor outcomes in substance abuse treatment as well as a variety of psychiatric disorders16. Median prevalence rates of Axis II disorders are especially high (70–80%) among drug dependent persons treated in inpatient or residential settings17. A systematic review of the literature18 found that PDs, particularly antisocial (ASPD) and borderline (BPD), were consistently associated with risks for early drop out from all types of substance abuse treatment. Other studies19–23 have also documented poor outcomes for PDs in general, including their negative association with treatment completion in a large sample of homeless military veterans in a residential rehabilitation facility24 and among a sample of 307 Norwegian drug abusers25.
TCs were specifically designed to address the attitude, behavioral, criminogenic, and personality problems that characterize severe addiction and ASPD. As such, ASPD might be expected to have no appreciable impact on retention in an effectively run TC. However, studies evaluating retention among ASPD in TCs have been mixed. Goldstein et al.26 compared patients who met full criteria for ASPD (i.e., adult criteria and evidence of conduct disorder in childhood) versus those who only displayed adult antisocial behavior. They found that the ASPD diagnosed group had poorer retention for the longer (i.e., 180 day) treatment program, but that the groups did not differ for the 90 day program. In contrast, Haller et al.27 (1997) reported that ASPD was positively related to treatment retention in a sample of pregnant women. Messina and colleagues found that ASPD, diagnosed with either self-report inventory28 or semi-structured interview29 was unrelated to several outcome measures, including the completion of the 12 month TC. Most recently, Daughters et al.30 reported that, while ASPD status did not predict retention on its own, the interaction of ASPD and court-mandated status did predict early attrition in a sample of 236 male TC patients. Considering these mixed findings for ASPD, continued study of its impact on TC retention would be helpful in supplementing and potentially clarifying the existing literature.
Although a TC’s highly structured, hierarchical social milieu, emphasizing positive and negative consequences, may be well suited to ASPD, such an intensive and confrontive peer pressure environment may not be an effective approach for PDs characterized by significant cognitive (e.g., paranoid), emotional (e.g., borderline), or interpersonal (e.g., avoidant) vulnerability or rigidity. We are aware of only a few other studies that have evaluated PDs other than ASPD in relation to TC retention. Karterud et al.31 evaluated 97 patients in a Norwegian day hospital TC and divided the patients into four diagnostic groups: borderline, schizotypal, “other” PD, and no PD. Borderline and schizotypal groups had greater rates of attrition than did the other PD or no PD groups. Fals-Stewart32 also examined the MCMI-II 33 PD scales and found that schizoid and schizotypal scales were negatively related to length of stay within a TC, while histrionic and narcissistic scales were positively related.
The current study attempted to address several gaps in the literature by conducting a more thorough evaluation of the relation between all 10 PDs and two measures of retention (i.e., early attrition, defined as premature dropout within the first 30 days, and overall time to dropout from the 9-month treatment program). We chose these two frames because of their clinical relevance and because they corresponded to time frames chosen in prior research. We also addressed the limitations of previous research31 which relied on unstructured clinical diagnoses, did not test all PDs, used a general index of retention (percent dropped out), and a lower intensity non-residential TC milieu. Although previous studies have been mixed, we predicted that ASPD would not be related to either very early attrition or overall time to dropout. However, we predicted that borderline PD and several Cluster A (paranoid, schizoid, schizotypal) and Cluster C (avoidant, obsessive-compulsive) PDs characterized by severe cognitive, emotional, and interpersonal vulnerabilities would be related to reduced retention.
Method
Participants
We recruited adult and adolescent patients from a long-term residential TC treatment program for substance abuse located in an urban area in the Northeastern United States. For inclusion, patients had to be either adolescents (15–18 years; n = 49) or adults (19–65 years; n = 77) and have a lifetime DSM-IV substance abuse or dependence diagnosisA. Seven additional patients provided informed consent, but were excluded based on inability to read or understand the consent or assessment forms based on the Slosson Oral Reading Test34. Patients with current suicidal or homicidal plans, severe medical illness, schizophrenia, or bipolar disorder were not eligible for admission to the residential program. Interested individuals provided consent and received the baseline packet of self-report materials from a research assistant. Participants received a $50 store gift card for completing the baseline assessment, $10 for month 1–5 assessments, $60 for the month 6 and $70 for month 9 assessments. This study was approved by the Institutional Review Board at the authors’ institution.
Materials
Personality disorders were assessed using the Schedule for Nonadaptive and Adaptive Personality (SNAP) 35. The SNAP is a self-report inventory that includes 375 items rated as true or false. It provides an assessment of three broad temperaments (i.e., positive affect, negative affect, and disinhibition) as well as 12 maladaptive trait scales that assess aspects of personality pathology (e.g., mistrust, aggression, and impulsivity). The SNAP also provides an assessment of the DSM-III-R36 personality disorders, using some items that overlap with those included in the trait scales. These PD scales can be scored dimensionally (i.e., summing the items) or can produce categorical variables for each diagnostic criterion that can then be counted to determine whether the individual reaches the diagnostic threshold. Scores on the SNAP PD scales obtained stability coefficients over a nine-month interval ranging from .59 (schizotypal) to .84 (antisocial), with a median of .75 in a non-clinical sample37. SNAP PD scale scores have demonstrated validity when compared to semi-structured interview measures with a median convergent correlation of .5535. In addition, SNAP PD scores correlate strongly with scores from other self-report PD instruments with a median convergent value of .62 across the 10 PDs38. In addition, portions of the Structured Clinical Interview for DSM-IV (SCID) were administered for descriptive purposes.
Procedures
TC residents were approached about their interest in participating in research within one week of program admission. Eligible and interested residents provided informed consent and completed a baseline assessment which included the SNAP and then monthly and follow-up assessments during their participation in a randomized clinical trial of two active psychotherapies. All participants were admitted to the TC with a minimal length of stay of 9 months and typically by referral through the criminal justice or child protection systems. APT Residential Services Division embraces most of the core elements that have defined a TC39. The program involves a highly organized, staff-guided, self-help positive peer pressure process focused especially on changing attitudes, perceptions and behaviors associated with drug use and criminality. Peers influence peers to promote learning and assimilation of social norms and skills. There are strict, explicit, behavioral norms with contingencies to promote self-control and responsibility. The first 30 days of treatment are spent in a semi-segregated “orientation group program” in which the rules and responsibilities are learned and residents are supported through their accommodation to this new milieu. The next 6 or more months are spent in the main TC program and then followed by 6 or more months in a higher status resident coordinator role or employment in the community during a re-entry phase.
Although community meetings and psychoeducational groups are important tools, peer encounter and other therapy groups are considered the core techniques aimed at change. These groups are meant to heighten each individual’s awareness of specific attitudes or behavioral patterns that negatively affect the community and need to be changed for the individual to recover. All of these groups focus on changing cognitive, behavioral, and emotional processes that severely impede affiliation with the community and thus prevent socialization and maturation. In addition, there are an array of professional support services in place (group counseling, case management, medical care, psychiatric services, educational and vocational programming). Job or school functions are arranged in a hierarchy according to seniority and individual productivity such that progress leads to higher levels of management/coordination as well as additional privileges. This social organization reflects fundamental elements of the rehabilitative approach: self-help, trust in the community, responsible performance, honesty, hard work, tough love, and earned successes. These are conceptualized as necessary for long-term recovery from addiction.
Data Analyses
Although the primary result of interest was the impact of PDs on 9-month TC program retention, attrition in the very early phase of treatment is a significant clinical problem for all addiction treatment modalities. Therefore, we also chose to evaluate 30 day attrition because the first month (orientation phase) is a critical phase of adjustment to a TC where separate programming is provided and because this is the shortest duration used as an outcome variable in previous TC research. We first conducted univariate analyses using chi-square to evaluate early drop-out and Kaplan-Meier survival analyses to evaluate days retained in treatment. For these univariate analyses, each diagnostic group was compared to the group without a PD diagnosis. In order to evaluate which predictors showed the strongest relationship we then conducted multivariate analyses by entering all diagnoses simultaneously. Binary logistic regression was used for early dropout and Cox regression survival analyses for treatment retention. Finally, because the field of PD research appears to be moving toward dimensional approaches for DSM-540, we repeated the multivariate analyses using dimensional PD scores. For these analyses, the raw item scores for each SNAP scale were summed to create variables referred to as PD severity scores. Again, early dropout was evaluated using binary logistic regression and Cox regression was used for overall retention.
Results
One-hundred and twenty-six participants completed the baseline assessment and 17 (14%) dropped out before 30 days, and 81 of these participants (64%) did not complete the 9-month programB. Table 1 provides descriptive statistics on demographic variables as well as selected Axis I and Axis II PD diagnoses for the entire sample.
Table 1.
Descriptive Statistics for Overall Sample on Demographic Variables, SCID Axis I Diagnoses, and SNAP Personality Disorder Diagnoses
| Variable |
|---|
| Gender (%male) |
| Race |
| Caucasian (%) |
| African-American (%) |
| Hispanic (%) |
| other (%) |
| Age (M [SD]) |
| Adult (%) |
| Lifetime Substance Diagnosis |
| Alcohol (%) |
| Stimulant (%) |
| Opioid (%) |
| Cannabis (%) |
| other (%) |
| Lifetime Axis I Diagnosis |
| Major Depression (%) |
| Social Phobia (%) |
| PTSD (%) |
| Personality Disorder |
| Paranoid (%) |
| Schizoid (%) |
| Schizotypal (%) |
| Antisocial (%) |
| Borderline (%) |
| Histrionic (%) |
| Narcissistic (%) |
| Avoidant (%) |
| Dependent (%) |
| Obsessive-Compulsive (%) |
Notes: SCID = Structured Clinical Interview for DSM-IV- Axis I 48; PTSD = Post-Traumatic Stress Disorder. SNAP = Schedule for Nonadptive and Adaptive Personality.
Univariate Analyses
We first examined the impact of any PD diagnosis, by comparing those meeting criteria for one or more PDs (n = 75) to those without any PD diagnosis (n = 51) on both early attrition and overall time to dropout. Five times as many patients with a PD diagnosis dropped out within the first 30 days compared to those without a PD diagnosis (see Table 2). Over the entire treatment, patients with any PD diagnosis completed significantly fewer days in treatment than those without a PD diagnosis. Chi-square results indicated that antisocial, histrionic, and paranoid PD diagnoses were significantly related to early attrition. However, when considering overall number of days in treatment, Kaplan-Meier analyses suggested that borderline, paranoid, and avoidant diagnoses were significantly predictive of shorter duration over the entire 9 months of treatment.
Table 2.
Univariate Analyses for SNAP PD Diagnoses on Early Attrition and Overall Time to Dropout
| Diagnostic Group | Early Attrition (< 30 days) | Overall Time to Dropout (270 days) | |||||
|---|---|---|---|---|---|---|---|
| % Attrited | χ2 | p | Mean | 95% CI | log-rank χ2 | p | |
|
|
|
|
|||||
| Paranoid (26) | 19% | 4.88 | .04 | 127.1 | 88.2 – 165.9 | 4.27 | .04 |
| Schizoid (9) | 22% | 4.12 | .10 | 141.8 | 67.9 – 215.7 | 1.17 | .28 |
| Schizotypal (17) | 0% | .69 | 1.00 | 149.3 | 104.5 – 194.1 | 1.25 | .26 |
| Antisocial (39) | 26% | 9.02 | .00 | 133.5 | 100.0 – 167.1 | 3.25 | .07 |
| Borderline (32) | 13% | 2.16 | .20 | 114.0 | 83.4 – 144.7 | 11.06 | .00 |
| Histrionic (31) | 26% | 8.62 | .01 | 141.1 | 103.9 – 175.7 | 3.07 | .08 |
| Narcissistic (13) | 15% | 2.32 | .18 | 126.2 | 72.3 – 180.0 | 2.71 | .10 |
| Avoidant (29) | 14% | 2.60 | .18 | 134.4 | 98.0 – 170.9 | 4.57 | .03 |
| Dependent (17) | 18% | 3.53 | .10 | 136.9 | 88.2 – 185.6 | 1.94 | .16 |
| OCPD (4) | 25% | 3.20 | .21 | 202.8 | 102.2 – 303.3 | .04 | .85 |
| Any PD (75) | 20% | 6.72 | .02 | 135.3 | 112.3 – 158.3 | 6.09 | .01 |
| No PD (51) | 4% | - | - | 191.2 | 165.8 – 216.5 | - | - |
Notes: Early dropout present chi-square analyses using Fisher’s exact test (two-sided). Treatment completion analyses present results from Kaplan-Meier survival analysis with data right-censored at 270 days. Each diagnostic group was compared to the group without any PD diagnoses, provided on the lowest row. SNAP = Schedule for Non-Adaptive and Adaptive Personality (Clark, 1993); PD = Personality Disorder; Mean = the mean number of days in treatment; CI = Confidence Interval. Numbers in parentheses indicate the number of patients who met criteria for the PD. OCPD = Obsessive-Compulsive Personality Disorder. PD = personality disorder. Values in boldface type indicate significance at p < .05.
Multivariate Analyses
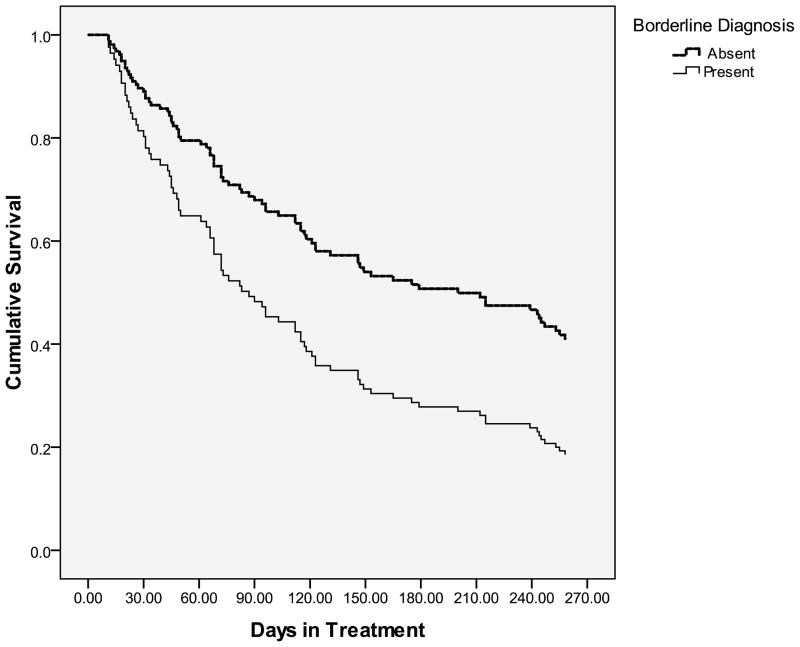
Seeking to better understand the unique contribution of each individual PD, we then entered the ten PDs simultaneously into a binary logistic regression predicting the dichotomous variable of attrition within the first 30 days. Schizotypal diagnosis was excluded from the early attrition analyses because all 17 individuals meeting criteria for schizotypal remained in treatment at 30 days, providing no variability in the outcome. As with the univariate analyses, ASPD and histrionic were significantly predictive of early attrition. However, in contrast to the univariate findings, the impact of a paranoid diagnosis was non-significant when all the diagnoses were considered simultaneously (see Table 3). Multivariate analyses of days until dropout indicated that BPD was the only diagnosis that evidenced a significantly shorter stay over the 9-month treatment. Figure 1 presents the cumulative survival for those with and without a BPD diagnosis.
Table 3.
Multivariate Analyses of SNAP PD diagnoses on early attrition and overall time to dropout
| Early Dropout (< 30 days) | Overall Time to Dropout (270 days) | |||||
|---|---|---|---|---|---|---|
| Wald χ2 | OR | 95% CI | Wald χ2 | HR | 95% CI | |
|
|
|
|||||
| Paranoid | 2.23 | 3.49 | .68 – 17.96 | .38 | 1.26 | .61 – 2.62 |
| Schizoid | 1.97 | 5.26 | .52 – 53.44 | .10 | 1.16 | .45 – 3.02 |
| Schizotypal | .00 | 1.36 | .58 | .23 – 1.45 | ||
| Antisocial | 5.53 | 5.16 | 1.31 – 20.22 | .04 | 1.06 | .60 – 1.88 |
| Borderline | 1.44 | .35 | .06 – 1.93 | 4.47 | 1.89 | 1.05 – 3.40 |
| Histrionic | 5.35 | 5.14 | 1.28 – 20.57 | .08 | 1.09 | .60 – 1.97 |
| Narcissistic | .91 | .28 | .02 – 3.76 | .23 | .79 | .29 – 2.11 |
| Avoidant | .78 | 2.14 | .39 – 11.67 | 1.31 | 1.45 | .77 – 2.72 |
| Dependent | .07 | .80 | .14 – 4.50 | .03 | .94 | .42 – 2.07 |
| OCPD | .52 | 3.57 | .11 – 112.93 | .62 | .56 | .13 – 2.39 |
Notes: Early attrition analyses present binary logistic regressions on presence of drop-out at 30 days. Overall time to dropout analyses present Cox regression analyses for attrition over 9-months. SNAP = Schedule for Nonadaptive and Adaptive Personality35. PD = Personality disorder. OR = Odds ratio; HR = Hazard ratio; 95% CI = 95% Confidence Interval. OCPD = obsessive-compulsive PD. Values in boldface type indicate significance at p < .05. * Schizotypal was excluded from early attrition analysis due to lack of variability in the outcome measure.
Figure 1. Cox Regression Survival Analysis for Borderline Personality Disorder Diagnosis.
Notes: n = 126; BPD = borderline personality disorder; Data right-censored at 270 days
Dimensional Scores
Finally, in order to determine whether dimensional representations of these constructs would show comparable findings, we repeated the multivariate analyses using continuous measures of the PD constructs. A binary logistic regression on the early attrition variable showed that histrionic severity was significantly predictive of early attrition (Wald χ2 = 5.0, OR = 1.58, 95% CI = 1.06 – 2.36), while antisocial severity trended but was not significant (Wald χ2 = 3.1, p = .08; OR = 1.20, 95% CI = .98 – 1.47). Consistent with the categorical results above, a Cox proportional hazards regression indicated that borderline severity significantly predicted shorter treatment lengths, Wald χ2 = 4.40, p < .05; H.R. = 1.21, 95% CI = 1.00 – 1.45.
Discussion
Although TCs are a promising treatment modality for severe addiction, criminality, unemployment, and other psychosocial problems, research has indicated that premature attrition is negatively associated with these long-term outcomes3. The existing literature has provided mixed findings with respect to ASPD and little information about the impact of other PDs on retention. In contrast with some other research26 our findings replicate those of Messina and colleagues28–29 who also reported that ASPD was unrelated to TC retention. Globally, the results of the current study are consistent with previous findings in demonstrating that the presence of any PD is associated with worse retention in a TC24–25. However, the effect appears to be more specific both in terms of specific diagnoses and treatment intervals. The current study suggests that when considered in isolation, individuals with baseline diagnoses of BPD, avoidant, and paranoid PDs had significantly fewer days in treatment, compared to individuals without a PD diagnosis. However, when all ten diagnoses were considered simultaneously only BPD remained significant, suggesting that it is most related to shorter duration, over the course of a 9-month treatment. Additionally, individuals with ASPD, histrionic, and paranoid PD diagnoses were significantly more likely than those without any diagnosis to drop out within the first 30 days of treatment. Nonetheless, multivariate analyses (in which all diagnoses were entered at once) indicated that only the findings for ASPD and histrionic remained significant. It is perhaps interesting that, although BPD was the diagnosis with the shortest overall treatment duration, it was not significantly related to early attrition in the first 30 days.
These findings indicate that individuals with high emotional reactivity (which characterizes BPD) are not prone to retention problems during the orientation phase of TC treatment when they are receiving highly structured psychoeducational group and individual meetings focused on adaptation to the program milieu. During these first 30 days, residents are also relatively segregated from the broader program population and stressors of peer confrontation and behavioral consequences. Our results suggest that BPD residents experience retention problems the longer that they are exposed to the more intensive environment of the regular TC program which can be characterized by affectively-charged and interpersonally confrontive interactions with peers and staff. This type of demanding TC milieu contrasts with existing empirically supported treatments for BPD such as dialectical behavior therapy41 which focuses explicitly on balancing change with empathic acceptance and validation of the individual. Research suggests that this type of treatment can increase retention and treatment outcomes for emotionally dysregulated and vulnerable patients42–43. Symptoms associated with BPD might not substantially interfere with the initial orientation to the TC model, but might interfere with the longer-term effective utilization of the TC’s core treatment processes.
In this sense, the findings for BPD were almost completely opposite those for ASPD and histrionic as those PDs were both related to early attrition, but not to overall time spent in the TC. In contrast to BPD, the traits associated with ASPD, such as assertiveness, competitiveness, and tough-skinned independence, might lead to difficulty accepting the rules and regulations of the well-controlled environment. However, once the initial orientation period is over, those same traits might equip the individual for success within (or at least tolerance for) the confrontive TC atmosphere. The present findings for ASPD at the two time points might also explain its inconsistent relationship with TC completion in previous studies. The definition of treatment completion has varied greatly, from as few as 30 days30 to as long as 12 months28. This wide range of intervals across studies as well as the fact that ASPD might present greater risks early in treatment suggests that, in addition to programmatic differences across TCs, the previous research might have been capturing temporal variation.
The finding that histrionic PD is also associated with attrition within the first 30 days of treatment is somewhat more difficult to understand. Only one other study has examined the relationship between histrionic PD and TC completion and it suggested that histrionic scores were positively related to overall length of treatment32. Nonetheless, that study used a version of the MCMI33 that researchers have suggested may assess only qualitative, and perhaps even adaptive, aspects of histrionic PD44. Histrionic is defined primarily by the need to be the center of attention and represented by traits such as exhibitionism. It is possible that such individuals also may not respond well to the early phases of TC orientation when they are segregated from the population and less able to engage the wider attention of all residents and staff. Nonetheless, the fact that the current study is the first to report that histrionic PD might be related to early TC attrition should be interpreted cautiously until it can be further tested in additional studies.
While the most robust findings were for BPD (in terms of overall treatment duration) and for ASPD and histrionic (in terms of attrition within the first 30 days), there were also other PDs that evidenced an increased risk for attrition. Notably, individuals diagnosed with paranoid PD completed fewer total days in treatment and were more likely to drop out within the first 30 days than individuals without a PD diagnosis. In both cases, the findings for paranoid PD were not significant when considered simultaneously with the other PD diagnoses. This perhaps suggests that the effect of paranoid might be accounted for by its comorbidity with other disorders, rather than its unique variance. Similarly, individuals with an avoidant PD diagnosis spent significantly fewer days in treatment than individuals without any PD diagnoses, but this effect was also not significant when considered in multivariate analyses. At a minimum these findings suggest that future studies of premature dropout should also consider paranoid and avoidant PD.
Finally, it is important to note that the present findings were not specific to diagnostic status defined categorically (i.e., presence vs. absence of the diagnosis) as analyses of dimensional scorings also obtained comparable results. This is particularly important as it appears increasingly likely that DSM-5 will incorporate a dimensional understanding of personality pathology. Within the currently available proposal40 it appears that ASPD and BPD will continue to be included (although histrionic might be excluded) but will be rated along a continuum rather than categorically. If this model is indeed adopted, the dimensional results presented in the current study might be most relevant to future researchers and clinicians.
Clinical Implications
A primary implication of the current study is the importance of thorough personality assessment at the outset of treatment within a TC. Specifically, identification of those traits and behaviors characteristic of BPD and ASPD, as well as perhaps histrionic, paranoid, and avoidant PDs, is essential as they predicted different retention challenges. The current results suggest that ASPD should be identified quickly and that specific interventions be targeted toward these individuals to assist in their engagement and orientation to the TC atmosphere. The findings suggest that the risk for attrition for these individuals is greatest at the beginning of treatment and that the personality traits associated with ASPD might have a negligible (or even protective) effect once they integrate into the TC. Individuals with high standing on BPD, on the other hand, appear to be at no greater risk for very early attrition in programs that do not require immediate immersion into the treatment milieu. Nonetheless, the fact that BPD predicted attrition prior to program completion, suggests that a TC might not be the optimal choice of treatment for these individuals. Perhaps this initial early period (i.e., first 30 days) can be utilized by identifying the individuals least likely to benefit from the TC and make programmatic adjustments or external referral to promote better treatment retention and outcome.
Limitations
The current study provides data on the impact of PDs on TC retention at two different time points, but is not without limitations. While self-reports of PDs are the most common method of assessment within the research literature, semi-structured interviews are considered to be the most valid method45. In addition, the version of the SNAP employed in the current study assesses the DSM-III-R categories. Although the differences between the PD scales on the SNAP34 and the SNAP-246 are relatively minor (typically only a few items were changed), the use of DSM-IV scales would be preferable. Finally, the initial sample size was larger than some previous examinations (e.g., 97 patients31 and 65 patients25) but was also smaller than others (e.g., 275 patients28). Nonetheless, the low prevalence of some PDs within this sample perhaps reduced the ability to detect their impact on retention. This factor, combined with the gender imbalance typical of most TCs, prevented our evaluation of the effects of gender on retention for all PDs. Future studies that examine potential gender interactions would be particularly important for BPD and ASPD given the gender differences in these diagnoses47.
Conclusions
This was the first study to evaluate the categorical and dimensional representation of all 10 PDs in relation to two treatment retention milestones. Our results suggest that previously inconsistent findings for ASPD might be attributable to the length of the treatment interval used to define “completion.” Finally, the current study also indicated that BPD negatively relates to long-term retention suggesting that other treatment modalities or approaches for emotionally dysregulated individuals might be preferable.
Acknowledgments
Writing of this manuscript was supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs. Research was supported by NIDA grant DA14967 to S.A. Ball.
Footnotes
Before combining results from the adolescent and adults, we carefully examined them for potential differences. Beyond age, t-tests and chi-square analyses did not indicate significant differences for racial or gender makeup. Significant differences were noted for lifetime substance diagnoses, with adults more likely to qualify for alcohol, opioid, and stimulant diagnoses while adolescents were more likely to be diagnosed with cannabis dependence. No differences were detected for lifetime rates of major depressive disorder or social phobia, but adults were more likely to have a diagnosis of post-traumatic stress disorder. Most importantly, chi-square analyses also did not detect significant differences in the diagnostic rate for any of the 10 PDs, which were the variables of interest in the current study. While diagnosis of PDs within DSM-IV (APA, 2000) is restricted to individuals over the age of 18, there is increasing evidence for the continuity of maladaptive personality functioning across this arbitrary threshold49–50. Additionally, the DSM-5 Personality and Personality Disorders Workgroup proposal40 does not include an age requirement.
Although 270 days represented completion of the formal treatment, some patients remained in treatment for more than a year.
References
- 1.De Leon G. Therapeutic communities. In: Galanter M, Kleber H, editors. The American Psychiatric Publishing Textbook of Substance Abuse Treatment. 3. Washington, DC: American Psychiatric Publishing; 2004. pp. 485–501. [Google Scholar]
- 2.Simpson DD, Sells SB. Effectiveness of treatment for drug abuse: An overview of the DARP research program. Adv Alcohol Subst Abuse. 2002;2:7–29. [Google Scholar]
- 3.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychol Addict Behav. 1997;11:294–307. [Google Scholar]
- 4.Hubbard RL, Marsden ME, Rachal JV, Harwood HJ, Cavanaugh ER, Ginzburg HM. Drug abuse treatment: A national study of effectiveness. Chapel Hill, NC: University of North Carolina Press; 1989. [Google Scholar]
- 5.Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Psychol Addict Behav. 1997;11:261–278. [Google Scholar]
- 6.Anglin MD, Hser YI. Treatment of drug abuse. In: Tonry M, Morris, editors. Drugs and crime: Crime and justice: A review of research. Chicago, IL: University of Chicago Press; 1991. [Google Scholar]
- 7.Condelli WS, Hubbard RL. Relationship between time spent in treatment and client outcomes from therapeutic communities. J Subst Abuse Treat. 1994;11:25–33. doi: 10.1016/0740-5472(94)90061-2. [DOI] [PubMed] [Google Scholar]
- 8.De Leon G. Treatment Research Monograph Series. DHHS Publication no (ADM) 85-1286. Rockville, MD: National Institute on Drug Abuse; 1994. The therapeutic community: Study of effectiveness. [Google Scholar]
- 9.Sacks S, Banks S, McKendrick K, Sacks JY. Modified therapeutic community for co-occurring disorders: A summary of four studies. J Subst Abuse Treat. 2008;34:112–122. doi: 10.1016/j.jsat.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Condelli WS. Domains of variables for understanding and improving retention in therapeutic communities. Int J Addict. 1994;29:593–607. doi: 10.3109/10826089409047402. [DOI] [PubMed] [Google Scholar]
- 11.De Leon G, Skodol A, Rosenthal MS. Phoenix House: Changes in psychopathological signs of resident drug addicts. Arch Gen Psychiatry. 1973;28:131–135. doi: 10.1001/archpsyc.1973.01750310103017. [DOI] [PubMed] [Google Scholar]
- 12.De Leon G. Psychopathology and substance abuse: What is being learned from research in therapeutic communities. J Psychoactive Drugs. 1989;21:177–188. doi: 10.1080/02791072.1989.10472158. [DOI] [PubMed] [Google Scholar]
- 13.Jainhill NG, De Leon G, Pinkham L. Psychiatric diagnoses among substance abusers in the therapeutic community. J Psychoactive Drugs. 1986;8:209–213. doi: 10.1080/02791072.1986.10472349. [DOI] [PubMed] [Google Scholar]
- 14.Sacks S, De Leon G, Balisteri E, Liberty HJ, McKendrick K, Sacks J, Staines G, Yagelka J. Modified therapeutic community for homeless mentally ill chemical abusers. J Subst Abuse Treat. 1999;15:545–554. doi: 10.1016/s0740-5472(97)00314-0. [DOI] [PubMed] [Google Scholar]
- 15.Sacks JG, Levy NM. Objective personality changes in residents of a therapeutic community. Am J Psychiatry. 1979;136:796–799. doi: 10.1176/ajp.136.6.796. [DOI] [PubMed] [Google Scholar]
- 16.Ansell EB, Grilo CM. Personality disorders. In: Hersen M, Turner SM, Beidel, editors. Adult psychopathology and diagnosis. Hoboken, NJ: Wiley; 2007. [Google Scholar]
- 17.Verheul R, Ball S, van den Brink W. Substance abuse and personality disorders. In: Kranzler HR, Rounsaville BJ, editors. Dual Diagnosis and Treatment: Substance Abuse and Comorbid Medical and Psychiatric Disorders. New York: Marcel Dekker; 1998. [Google Scholar]
- 18.Meier PS, Barrowclough C. Mental health problems: Are they or are they not a risk factor for dropout from drug treatment? A systematic review of the evidence. Drugs: Education, Policy, and Prevention. 2009;16:7–38. [Google Scholar]
- 19.DeJong C, van den Brink W, Harteveld FM, van der Wielen GM. Personality disorders in alcoholics and drug addicts. Compr Psychiatry. 1993;34:87–94. doi: 10.1016/0010-440x(93)90052-6. [DOI] [PubMed] [Google Scholar]
- 20.Kosten TA, Kosten TR, Rounsaville BJ. Personality disorders in opiate addicts show prognostic specificity. J Subst Abuse Treat. 1989;6:163–168. doi: 10.1016/0740-5472(89)90003-2. [DOI] [PubMed] [Google Scholar]
- 21.Nace EP, Davis CW. Treatment outcome in substance abusing patients with a personality disorder. Am J Addict. 1993;2:26–33. [Google Scholar]
- 22.Rounsaville BJ, Kosten TR, Weissman MM, Kleber HD. A 2.5 year follow-up of short-term interpersonal psychotherapy in methadone maintained opiate addicts. Compr Psychiatry. 1986;27:201–210. doi: 10.1016/0010-440x(86)90041-6. [DOI] [PubMed] [Google Scholar]
- 23.Thomas VH, Melchert TP, Banken JA. Substance dependence and personality disorders: Comorbidity and treatment outcome in an inpatient treatment population. J Stud Alcohol. 1999;60:271–277. doi: 10.15288/jsa.1999.60.271. [DOI] [PubMed] [Google Scholar]
- 24.Justus AN, Burling TA, Weingardt KR. Client predictors of treatment retention and completion in a program for homeless veterans. Subst Use Misuse. 2002;41:751–762. doi: 10.1080/10826080500411353. [DOI] [PubMed] [Google Scholar]
- 25.Ravndal E, Vaglum P, Lauritzen G. Completion of long-term inpatient treatment of drug abusers: A prospective study from 13 different units. Eur Addict Res. 2005;11:180–185. doi: 10.1159/000086399. [DOI] [PubMed] [Google Scholar]
- 26.Goldstein RB, Powers SI, McCusker J, Lewis BF, Bigelow C, Mundt KA. Antisocial behavioral syndromes among residential drug abuse treatment clients. Drug Alcohol Depend. 1998;49:201–216. doi: 10.1016/s0376-8716(98)00014-3. [DOI] [PubMed] [Google Scholar]
- 27.Haller DL, Knisley JS, Elswick RK, Dawson KS, Schnoll SH. Perinatal substance abusers: Factors influencing treatment retention. J Subst Abuse Treat. 1997;14:513–519. doi: 10.1016/s0740-5472(97)00119-0. [DOI] [PubMed] [Google Scholar]
- 28.Messina N, Wish ED, Hoffman JA, Nemes S. Antisocial personality disorder and TC treatment outcomes. Am J Drug Alcohol Abuse. 2002;28:197–212. doi: 10.1081/ada-120002970. [DOI] [PubMed] [Google Scholar]
- 29.Messina NP, Wish ED, Nemes S. Therapeutic community treatment for substance abusers with antisocial personality disorder. J Subst Abuse Treat. 1999;17:121–128. doi: 10.1016/s0740-5472(98)00066-x. [DOI] [PubMed] [Google Scholar]
- 30.Daughters SB, Stipleman BA, Sargeant MN, Schuster R, Bornolova MA, Lejuez CW. The interactive effects of antisocial personality disorder and court-mandated status on substance abuse treatment dropout. J Subst Abuse Treat. 2008;34:157–164. doi: 10.1016/j.jsat.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karterud S, Vaglum S, Friis S, Irion ZT, Johns S, Vaglum P. Day hospital therapeutic community treatment for patients with personality disorders: An empirical evaluation of the containment function. J Nerv Ment Dis. 1992;180:238–243. doi: 10.1097/00005053-199204000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Fals-Stewart W. Personality characteristics of substance abusers: An MCMI cluster typology of recreational drug users treated in a therapeutic community and its relationship to length of stay and outcome. J Pers Assess. 1992;59:515–527. doi: 10.1207/s15327752jpa5903_7. [DOI] [PubMed] [Google Scholar]
- 33.Millon T, Millon C, Davis R. Millon Clinical Multiaxial Inventory: MCMI-III. Upper Saddle River, NJ: Pearson Assessments; 1996. [Google Scholar]
- 34.Slosson R, Nicholson C. Slosson oral reading test (rev ed) East Aurora, NY: Slosson Educational Publications; 1990. SORT-R3. [Google Scholar]
- 35.Clark LA. Manual for the Schedule for Nonadaptive and Adaptive Personality. Minneapolis, MN: University of Minnesota Press; 1993. [Google Scholar]
- 36.American Psychiatric Association. Diagnostic and statistical manual of mental disorders Revised. 3. Washington, DC: American Psychiatric Association; 1987. revised. [Google Scholar]
- 37.Melley AH, Oltmanns TF, Turkheimer E. The Schedule for Nonadaptive and Adaptive Personality (SNAP): Temporal stability and predictive validity of the diagnostic scales. Assessment. 2002;9:181–187. doi: 10.1177/10791102009002009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Widiger TA, Boyd S. Assessing personality disorders. In: Butcher JN, editor. Oxford handbook of personality assessment. 3. New York: Oxford University Press; 2009. pp. 336–363. [Google Scholar]
- 39.De Leon G. Therapeutic communities: Is there an essential model. In: De Leon G, editor. Community as method: Therapeutic communities for special populations and special settings. Westport, CT: Praeger; 1997. [Google Scholar]
- 40.DSM-5 Personality Disorders Workgroup. [Accessed Jul 12, 2010.];Reformulation of personality disorders in DSM-5. http://www.dsm5.org/ProposedRevisions/Pages/PersonalityandPersonalityDisorders.aspx.
- 41.Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical Behavior Therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- 42.Bornalova MA, Daughters SB. How does Dialectical Behavior Therapy facilitate treatment retention among individuals with comorbid borderline personality disorder and substance use disorders. Clin Psychol Rev. 2007;27:923–943. doi: 10.1016/j.cpr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 43.Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 44.Craig RJ. Overview and current status of the Millon Clinical Multiaxial Inventory. J Pers Assess. 1999;72:390–406. doi: 10.1207/S15327752JPA7302_7. [DOI] [PubMed] [Google Scholar]
- 45.McDermut W, Zimmerman M. Assessment instruments and standardized evaluation. In: Bender D, Oldham J, Skodol A, editors. The American Psychiatric Publishing textbook of personality disorders. Washington, DC: American Psychiatric Publishing; 2005. pp. 89–101. [Google Scholar]
- 46.Clark LA, Simms LJ, Wu KD, Casillas . Manual for the Schedule for Nonadaptive and Adaptive Personality (SNAP-2) Minneapolis, MN: University of Minnesota Press; In press. [Google Scholar]
- 47.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 48.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) Washington, D.C: American Psychiatric Press; 1996. [Google Scholar]
- 49.De Clercq B, De Fruyt F, Widiger TA. Integrating a developmental perspective in dimensional models of personality disorders. Clin Psychol Rev. 2009;29:154–162. doi: 10.1016/j.cpr.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 50.Shiner RL. A developmental perspective on personality disorders: Lessons from research on normal personality development in childhood and adolescence. J Pers Disord. 2005;19:202–210. doi: 10.1521/pedi.19.2.202.62630. [DOI] [PubMed] [Google Scholar]