Abstract
Background
Mitral regurgitation (MR) is the second most common valvular heart disease after aortic stenosis. Without intervention, prognosis is poor in patients with severe symptomatic MR. While surgical repair is recommended for many patients with severe degenerative MR (DMR), as many as 49% of patients do not qualify as they are at high surgical risk. Furthermore, surgical correction for functional MR (FMR) is controversial with suboptimal outcomes and significant perioperative mortality. The percutaneous MitraClip implantation can be seen as a viable option in high surgical risk patients. The purpose of this meta-analysis is to compare the safety, clinical efficacy, and survival outcomes of MitraClip implantation with surgical correction of severe MR.
Methods
Six electronic databases were searched for original published studies from January 2000 to August 2013. Two reviewers independently appraised studies, using a standard form, and extracted data on methodology, quality criteria, and outcome measures. All data were extracted and tabulated from the relevant articles’ texts, tables, and figures and checked by another reviewer.
Results
Overall 435 publications were identified. After applying selection criteria and removing serial publications with accumulating number of patients or increased length of follow-up, four publications with the most complete dataset were included for quality appraisal and data extraction. There was one randomized controlled trial (RCT) and three prospective observational studies. At baseline, patients in the MitraClip group were significantly older (P=0.01), had significantly lower LVEF (P=0.03) and significantly higher EuroSCORE (P<0.0001). The number of patients with post-procedure residual MR severity >2 was significantly higher in the MitraClip group compared to the surgical group (17.2% vs. 0.4%; P<0.0001). 30-day mortality was not statistically significant (1.7% vs. 3.5%; P=0.54), nor were neurological events (0.85% vs. 1.74%; P=0.43), reoperations for failed MV procedures (2% vs. 1%; P=0.56), NYHA Class III/IV (5.7% vs. 11.3; P=0.42) and mortality at 12 months (7.4% vs. 7.3%; P=0.66).
Conclusions
Despite a higher risk profile in the MitraClip patients compared to surgical intervention, the clinical outcomes were similar although surgery was more effective in reducing MR in the early post procedure period. We conclude the non-inferiority of the MitraClip as a treatment option for severe, symptomatic MR in comparison to conventional valvular surgery.
Keywords: Mitral valve repair, mitral valve annuloplasty, edge-to-edge technique, MitraClip, mitral clip
Introduction
Mitral regurgitation (MR) is the second most common valvular heart disease after aortic stenosis. The natural history of severe MR without surgical intervention is poor, leading to worsening left ventricular (LV) failure, pulmonary hypertension, atrial fibrillation and death (1). Surgical repair is recommended for severe degenerative MR (DMR) with better perioperative mortality, preservation of postoperative LV function, and long-term survival compared to valve replacement. If performed before the onset of limiting symptoms or LV dysfunction, surgical repair can restore normal life expectancy and quality of life (2,3). However, some patients do not qualify for surgery as advanced age or other comorbidities place them at high surgical risk (4).
In contrast, functional MR (FMR) is due to LV remodelling processes causing papillary muscle dislocation and leaflet tethering rather than primary anatomical alterations. Surgical correction for FMR is controversial, with no consistent outcomes for patients in terms of survival and quality of life and reports of suboptimal outcomes and significant perioperative mortality (4).
As many as 49% of patients with MR and in need of repair or replacement are considered at high-risk for surgical intervention, and are therefore not amenable to surgery. Such patients may be relegated to medical management which alleviates symptoms but does not alter the progression of the disease (5). Various percutaneous techniques have been developed to treat MR with less invasive approaches to minimize surgical trauma. Currently, the device with the widest clinical use is the MitraClip system (Abbot Vascular, Abbot Park, Illinois).
The MitraClip is a percutaneous method of repair of the mitral valve that mimics the surgical edge-to-edge Alfieri technique through mechanical coaptation of the mitral leaflets whilst minimizing surgical trauma (Figure 1). Percutaneous repair is via femoral venous and transeptal access to the left atrium. A clip is inserted through the mitral orifice into the left ventricle to grasp the leaflet edges and enable vertical coaptation (6).
Figure 1.
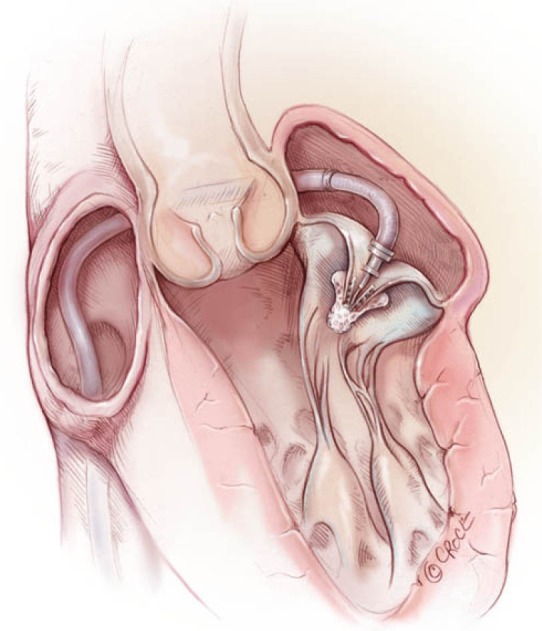
A MitraClip implantation.
The EVEREST II study is the only randomized controlled trial (RCT) with published data comparing percutaneous MitraClip implantation to conventional surgery. At four years follow-up, patients treated with the MitraClip more frequently required surgery to treat residual MR compared to the surgical group, although no differences were observed after one year of follow up. The authors of this study concluded that there were no differences in the prevalence of moderate-severe and severe MR or mortality at four years (7). A systematic review performed by our group of twelve studies found that the MitraClip can be implanted with reproducible safety and feasibility profile in high risk surgical patients with severe MR (8).
Based on the current evidence, surgery remains the standard treatment for MR in eligible patients. However percutaneous repair is associated with similar mortality and symptomatic improvement and is a potential alternative for up to half of all MR patients who are denied surgery. The aim of this meta-analysis is to compare the safety, clinical efficacy, and survival outcomes of MitraClip implantation versus surgical correction of severe MR.
Methods
Literature search
A meta-analysis on percutaneous edge-to-edge mitral valve repair with the MitraClip system versus surgical intervention in patients with severe organic and/or FMR was performed. Six electronic databases including MEDLINE, EMBASE, PubMed, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Database of Abstracts of Reviews of Effectiveness were searched for original published studies from January 2000 to August 2013. To achieve the maximum sensitivity of the search strategy and identify all studies, we used appropriate free text and thesaurus terms: ‘‘percutaneous’’ OR ‘‘transcutaneous’’ OR ‘‘transcatheter’’ OR “catheter-based” OR “endovascular” OR ‘‘trans-septal’’ AND ‘‘mitral valve repair’’ OR “edge-to-edge technique” OR “Alfieri’s technique” OR “double-orifice technique” OR “MitraClip” OR “mitral clip”. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. Expert academic cardiologists (U.D. and L.K.) and surgeons (O.A., P.G.B and T.D.Y.) were asked whether they knew of any unpublished data and formed the expert advisory panel. The quality of studies was assessed using assessment criteria recommended by the National Health Service Centre for Reviews and Dissemination (University of York, Heslington, United Kingdom) (9).
Selection criteria
Studies eligible for this meta-analysis included surgical candidates as well as high-risk surgical patients with significant degenerative and/or FMR who have undergone percutaneous mitral valve edge-to-edge repair using the MitraClip device. Experimental or observational studies were included in the present review. Case reports, series with less than ten patients, abstracts, editorials, and expert opinions were excluded. When centers had published duplicate trials with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for qualitative appraisal and data extraction. All studies selected were human trials and in the English language. Preoperative study variables included left ventricular ejection fraction (LVEF), European System for Cardiac Operative Risk Evaluation (EuroSCORE) and age. Postoperative study variables included early MR ≤2+ and acute procedural success. The guidelines of the Meta-Analysis of Observational Studies in Epidemiology group were followed (10).
Data extraction
Two reviewers (B.W and M.R.) independently appraised studies from January 2000 to August 2013, using a standard form, and extracted data on methodology, quality criteria, and outcome measures. All data were extracted and tabulated from the relevant articles’ texts, tables, and figures and checked by an additional reviewer (S.M.). Discrepancies between the reviewers were resolved by discussion and consensus with the senior investigator (T.D.Y.).
Statistical analysis
Meta-analyses were performed using either odds ratios (OR) or weighted mean differences (WMD). A random effects model was used as it accounts for potential clinical diversity and methodological variation between studies where selection criteria and risk profiles of patients differed (11). I2 statistics were used to estimate the variation across studies due to heterogeneity rather than chance. I2 values greater than 50% were considered high and the possible clinical and methodological reasons for this were explored qualitatively (12). Statistical significance was considered at P<0.05. All P values were 2-sided. Data were analysed using Review Manager Version 5.2.4 (The Cochrane Collaboration, Oxford, England).
Results
Quantity of studies
A total of 435 references were identified through searching of six electronic databases. Initial evaluation identified 210 potentially relevant articles. Manual search of the reference lists identified two additional publications of interest. After the inclusion criteria were applied to these 111 articles, eight articles remained for assessment. A second manual search of the reference lists of these eight articles did not yield any new relevant studies. From the eight articles, studies that reported duplicate data from the same centers were identified and only those with the most complete data set were selected. Four studies remained for inclusion in this meta-analysis. Baseline characteristics are summarized in Table 1. Outcomes following MitraClip procedure or surgery are summarized in Tables 2,3.
Table 1. Patient characteristics at baseline.
| Study | Number of patients |
Surgical MV Repairs% | Age, years |
Male % |
Logistic EuroSCORE, % |
Mitral valve pathology % |
MR Grade ≥3 |
Previous cardiac surgery |
LVEF % |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | |||||||||
| FMR | DMR | FMR | DMR | |||||||||||||||||||||
| Feldman (6) | 184 | 95 | 86 | 67.3±12.8 | 65.7±12.9 | 63 | 66 | – | – | 27 | 73 | 27 | 73 | 96 | 93 | 21* | 19* | 60.0±10.1 | 60.6±11.0 | |||||
| Conradi (13) | 95 | 76 | 100 | 72.4±8.1 | 64.5±11.4 | 64 | 45 | 33.7±18.7 | 10.1±8.7 | 86† | 14^ | 96† | 4^ | 100 | 99 | 46 | 11 | 36.2±12.5 | 42.1±16.2 | |||||
| Paranskaya (14) | 24 | 26 | 100 | 80±5 | 63±12 | 42 | 65 | 12.3±3.7 | 3.9±3.7 | 33 | 67¶ | 27 | 73¶ | 100 | 100 | 8 | 0 | 57.9±6.9 | 58.8±8.2 | |||||
| Taramasso (15) | 52 | 91 | 100 | 68.4±9.2 | 64.9±9.8 | 83 | 77 | 21.9±4.8 | 10.2±7.4 | 100 | 0 | 100 | 0 | – | – | 23 | 10 | 27.7±10 | 38.6±11.3 | |||||
| Weighted mean | NA | NA | 95 | 69.7±11.4 | 64.9±11.5 | 65 | 64 | 27.1±16 | 9.3±7.9 | 54 | 34 | 56 | 32 | 98 | 96 | 27 | 12 | 48.8±17.1 | 48.6±16.0 | |||||
*, previous CABG only; †, functional derived from dilated+ischaemic; ^, “other/unknown” presumed to represent degenerative pathology; ¶, value reported is degenerative/combined; NA, not applicable.
Table 2. Procedural outcomes following MitraClip intervention or surgery.
| Study | 30-day mortality % |
Acute procedural success % |
Major adverse events (30 days) % |
Urgent or emergent surgery % |
Reoperation for failed MV repair or replacement % |
Neurological event % |
Transfusion of ≥2 units % |
Acute kidney injury % |
Length of hospital stay, days |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | |
| Feldman (6) | 1.1 | 2.1 | – | – | 15 | 48% | 2 | 4 | 0 | 1 | 1 | 2 | 13 | 45 | 0.6 | 0 | – | – |
| Conradi (13) | 4.2 | 2.6 | 96 | 99 | – | – | – | – | 3 | – | 1 | 0 | – | – | – | – | 13.4±12.4 | 9.2±3.8 |
| Paranskaya (14) | 0 | 0 | 92 | 100 | 33 | 42 | 4 | 0 | 8 | 4 | 0 | 4 | 4 | 8 | 4 | 8 | 8.6±6.5 | 10.6±1.7 |
| Taramasso (15) | 0* | 6.6* | 98 | – | – | – | – | – | 2 | – | 0 | 2 | – | – | 31 | 31 | 5 (4-9)† | 11 (7-19)† |
| Weighted mean | 1.7 | 3.5 | 96 | 99 | 17 | 47 | 2.2 | 3.1 | 1.6 | 1.6 | 0.8 | 1.7 | 12 | 37 | 7 | 14 | NA | NA |
*, values used are for in-hospital mortality; †, median (IQR); NA, not applicable.
Table 3. Echocardiographic, functional and survival outcomes.
| Study | Early grade MR ≤2+ % |
NYHA functional class III/IV % |
Survival % |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
12 m |
6 m |
12 m |
|||||||||||
| MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | MitraClip | Surgical | |||||
| Feldman (6) | 77 | 100 | 51 | 47 | 2 | 13 | NR | NR | 94 | 94 | ||||
| Conradi (13) | 85 | 99 | 98 | 88 | NR | NR | 93 | 95 | NR | NR | ||||
| Paranskaya (14) | 100 | 100 | 88 | 96 | 4 | 8 | NR | NR | 92 | 100 | ||||
| Taramasso (15) | 90 | 100 | 85 | 67 | 15 | 11 | NR | NR | 88* | 89* | ||||
| Weighted mean | 83 | 99.7 | 71 | 69 | 5 | 12 | NA | NA | 93 | 93 | ||||
*, 12 months actuarial survival given only, not Kaplan-Meier; †, median (IQR); NA, not applicable.
Quality of evidence
Only one multi-institutional RCT comparing MitraClip versus surgical therapy was identified (6). The remaining three studies appraised were prospective observational studies (13-15). All studies were from specialized tertiary referral centres. With the exception of one study that had 178 MitraClip patients and 80 surgical patients (6), all other studies included had fewer than 100 patients in each treatment group (range 24-178, MitraClip; range 26-91, surgical). One study consisted of a cohort of patients that only had FMR (15) and the remaining studies consisted of patients with FMR and DMR (6,13,14). All studies explicitly stated a priori inclusion criteria. Two studies had a median follow-up of 12 months (6,14) while one study had a median follow-up of 6 months (13). One study had a follow up of 8.5 months and 18 months in the MitraClip and surgical group respectively (15).
Demographics and operative characteristics
Age was significantly higher in the MitraClip group compared to the surgical group (WMD, 7.22; 95% CI: 1.75 to 12.70; P=0.010). LVEF was significantly lower in the MitraClip group (WMD, –2.74; 95% CI: –5.27 to –0.22; P=0.03). EuroSCORE was reported in three studies and found to be significantly higher in the MitraClip group (WMD, 14.25; 95% CI: 7.72 to 20.79; P<0.0001).
All other reported baseline characteristics were not statistically different between the studied groups. The number of patients with MR severity of grade 3 or 4 was similar in both MitraClip and surgical groups (98% vs. 96%; OR, 1.88; 95% CI: 0.70-5.10; P=0.21; I2=0%). Frequency of functional mitral valve pathology was similar in the MitraClip and surgical groups (46% vs. 54%; OR, 0.77; 95% CI: 0.34-1.72; P=0.77; I2=50%). Previous cardiac surgery was comparable between the MitraClip and surgical group (27% vs. 12%, OR, 2.93; 95% CI: 1.02-8.45; P=0.05; I2=77%).
Residual MR
The number of patients with post-procedure residual MR severity >2 on echocardiography was significantly higher in the MitraClip group compared to the surgical group (17.2% vs. 0.4%; OR, 20.72; 95% CI: 4.91-87.44; P<0.0001, I2=0%) (Figure 2).
Figure 2.
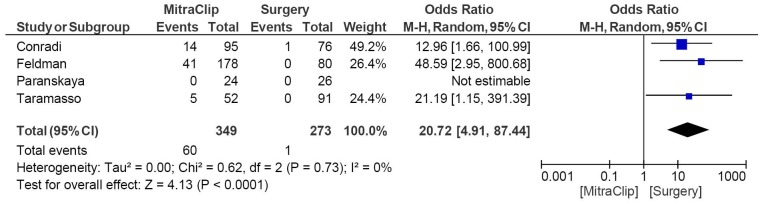
Forest plot of the odds ratio (OR) of early residual MR severity >2 after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Mortality and morbidity
Although the trend suggested 30-day mortality was lower in the MitraClip compared to the surgical groups, the result was not statistically significant (1.7% vs. 3.5%; OR, 0.66; 95% CI: 0.17-2.52; P=0.54; I2=19%) (Figure 3). Neurological events reported were comparable between MitraClip and surgical group (0.85% vs. 1.74%; OR, 0.58; 95% CI: 0.15-2.23; P=0.43; I2=0%) (Figure 4). Reporting of acute procedural success showed no significant difference between the MitraClip and surgical group (95% vs. 99%; OR, 0.25; 95% CI: 0.04-1.50; P=0.13; I2=0%), although this was only reported in two studies. Reoperations for failed MV procedures were also not significantly different (2% vs. 1%; OR, 1.80; 95% CI: 0.02-12.92; P=0.56; I2=32%) (Figure 5).
Figure 3.

Forest plot of the odds ratio (OR) of 30-day mortality after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Figure 4.
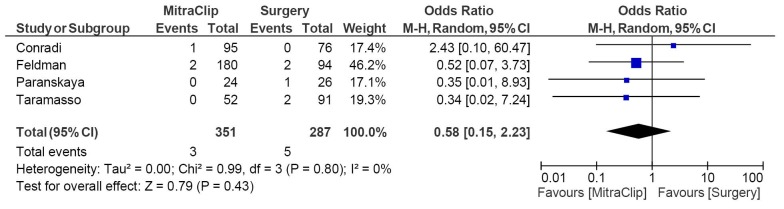
Forest plot of the odds ratio (OR) of neurological events after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Figure 5.
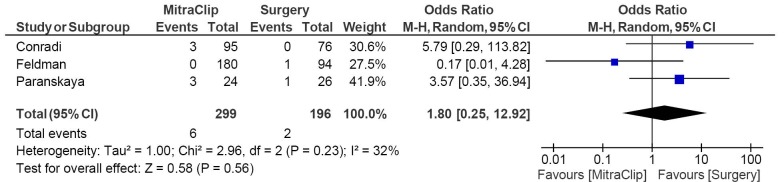
Forest plot of the odds ratio (OR) of reoperation after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Functional and survival outcomes
NYHA Class III/IV at baseline showed no significant difference between the MitraClip and surgical group (71% vs. 69%; OR, 1.77; 95% CI: 0.73-4.28; P=0.20). NYHA Class III/IV reported was also comparable at 12 months between the MitraClip and surgical group (5.7% vs. 11.3%; OR, 0.51; 95% CI: 0.10-2.58; P=0.42; I2=71%) (Figure 6). Mortality at 12 months was not significantly different between the MitraClip and surgical group (7.4% vs. 7.3%; OR, 1.18; 95% CI: 0.56-2.48; P=0.66; I2=0%) (Figure 7).
Figure 6.
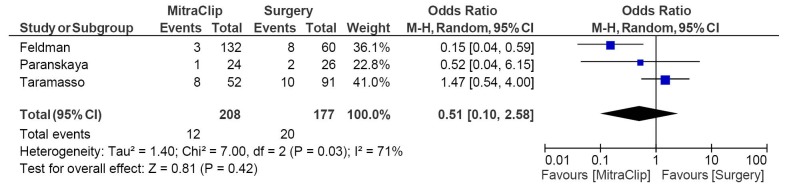
Forest plot of the odds ratio (OR) of NYHA Class III/IV at 12 months after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Figure 7.
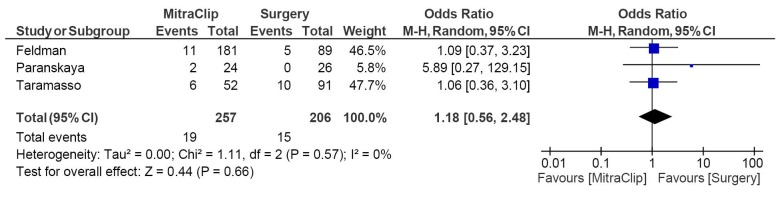
Forest plot of the odds ratio (OR) of survival at 12 months after MitraClip procedure or surgery in patients with severe MR. The estimate of the OR of each trial corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). On each line, the number of events as a fraction of the total number randomized is shown for both treatment groups. For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. M-H, Mantel-Haenszel.
Surgical intervention of the mitral valve differed in procedural parameters according to valve approach (median sternotomy or minimally invasive techniques), access to valve (direct left atria or trans-septal), method of repair (annuloplasty or Alfieri technique), type of annuloplasty (complete, rigid or semi-rigid), and leaflet/chordae modifications (resection, repair or annuloplastly alone). Surgical repair, as opposed to replacement, was the surgical method of choice in all studies except by Feldman et al. which reported 69 mitral valve repairs and 11 mitral valve replacements.
Publication bias
Publication bias was not assessed as there were inadequate numbers of included trials to properly assess a funnel plot or more advanced regression-based assessments.
Discussion
The current meta-analysis is an attempt to collate available information on the outcome experience of percutaneous repair versus conventional surgery of the MV in the setting of MR. All of the studies included in the analysis used the MitraClip method of percutaneous repair.
Although surgical mitral valve repair represents the gold standard for treating severe MR in symptomatic patients with LVEF >30% and left ventricular end systolic dimension (LVESD) <55 mm (16), it is associated with perioperative mortality and considerable rates of recurrent MR (17,18). Mortality rates are even higher for patients at high surgical risk (5.4% vs. 3.1%) (19). An alternate treatment modality developed for MR is the MitraClip, a transcatheter mitral valve repair system inspired by the Alfieri technique. The Alfieri edge-to-edge technique for repair of the mitral valve first performed in 1991 (20) has demonstrated durable results for as long as 12 years after surgical repair without annuloplasty (21,22). EVEREST I, a feasibility study for the MitraClip system, demonstrated low rates of morbidity and mortality and a composite primary efficacy end point (freedom from MR >2+, surgery or death at 12 months) of 66% (95% CI: 55-75%) (23). EVEREST II is the only RCT to have compared percutaneous MitraClip implantation to conventional surgery. The MitraClip was associated with similar mortality and symptomatic improvement but a higher rate of MR requiring repeat procedures, and less improvement in LV dimensions than surgery. Although the MitraClip was associated with a higher rate of residual MR at one year, there was no difference in later occurrence of MR or mitral valve intervention between 1- and 4-year follow-up. Unlike surgical intervention, the MitraClip device does not address mitral annulus enlargement problems associated with FMR, and thus explains the higher rate of residual MR at one year leading to repeat surgeries. Freedom from death, surgery, or grade 3+ or 4+ MR at four years was 39.8% versus 53.4% in the MitraClip and surgical groups respectively (P=0.070) while surgery for mitral valve dysfunction in the MitraClip group was 24.8% versus 5.5% in the surgical group (P<0.001) (7).
This meta-analysis has demonstrated a higher overall risk profile in percutaneous patients. Patients in the MitraClip group were older, had a higher EuroSCORE and a lower LVEF at baseline. Such differences must be considered when investigating clinical endpoints of the different treatment modalities. Despite surgery being more effective than the MitraClip at reducing early MR to a grade of ≤2, the clinical benefits were observed to be similar. It is possible that the difference in early MR reduction may represent early experience of a novel treatment. Indeed in the EVEREST II trial, 5% of patients had single leaflet device attachment whereas this rate in practice is now closer to 1% (24). Furthermore, a second device is now more frequently implanted (7). Comparable mortality, morbidity, reoperation rates, frequency of NYHA Functional Class III/IV and 12 months survival in this meta-analysis suggest the non-inferiority of the MitraClip, particularly considering the bias of baseline characteristics.
Many patients at high risk do not undergo surgery because of perceived excessive morbidity and mortality. Indeed, some reports suggest that up to 49% of patients with severe symptomatic MR are denied surgery (25,26). The non-inferiority of the MitraClip reaffirms its role in providing an alternative treatment modality for patients ineligible for surgery. There is insufficient evidence to indicate that patients suitable for surgical mitral valve repair should be candidates for the MitraClip.
Limitations
No subgroup meta-analysis of MV pathology could be conducted due to a lack of reporting. Only Feldman et al. provided a subgroup comparison between the MitraClip group and the surgery group in the subgroups FMR and DMR. The differences in rates of the primary efficacy end point (freedom from death, surgery and grade 3+ or 4+ MR) were smaller among FMR (P=0.02) and favoured surgery in DMR patients (6). The role of MitraClip in DMR is currently limited to high risk patients whilst in isolated FMR, MitraClip and surgery have the same recommendation level in recent guidelines. Given the fact that these two etiologies of MR are quite distinct, with FMR not being a primary valve disease but rather a product of LV dysfunction resulting in tethering and reducing closing forces, the MitraClip may play a bigger role in future guidelines regarding the treatment of isolated FMR. The COAPT and RESHAPE-HF trials are randomized studies comparing MitraClip versus optimal medical therapy alone in high-surgical risk patients with clinically significant FMR. The results of these trials will provide more insight into the value of MitraClip in treating FMR (27).
Again, only Feldman et al. provided an age subgroup comparison between the MitraClip group and the surgery group. It is known that more than 10% of patients aged 75 years and older that require hospitalization have significant MR (28). Yet, advanced age constitutes a major risk factor for surgery. In this study, there was a significantly smaller between-group difference of the primary end point among patients aged 70 years and older, as compared to those under 70 years of age which had outcomes favouring surgery (6). More comparisons of MitraClip versus surgery between the elderly and non-elderly are needed in future studies to confirm the role of MitraClip in patients with advanced age.
A limitation to this present meta-analysis is the lack of consistent reporting between studies. In one study, primary efficacy endpoint was defined as procedural success by placement of an annuloplasty ring or MitraClip(s) with acute reduction of MR to ≤2 (13). A similar definition of procedural success was given by Paranskaya et al., although with the additional requirement of freedom from new onset of significant mitral stenosis. However, procedural success was not defined nor reported for both treatment modalities in the other two studies. Similarly, the need for subsequent surgery was not consistently reported with some studies reporting urgent or emergent reoperations, while others reported surgery for valvular dysfunction with varying timeframes. Furthermore, useful mid-term echocardiographic findings and clinical outcomes were not consistently reported.
Another limitation to this present meta-analysis is the inclusion of only one RCT owing to the scarcity of publications comparing percutaneous mitral valve intervention with conventional surgical treatment. A MitraClip cohort with a greater comorbid profile may increase the propensity for a higher rate of adverse outcomes.
The ACCESS-EU study was designed to provide further evidence of the safety and effectiveness of the MitraClip system in a real-world setting through a snapshot of the current practice in Europe. The one-year findings have recently been published showing that patients in the real-world undergoing the MitraClip therapy are high-risk, elderly and mainly affected by FMR. This represents a significant shift from the population originally studied in the EVEREST II RCT trial. Interestingly, clinical outcomes from surgical intervention was not superior compared to the MitraClip in these groups (elderly and FMR) in the exploratory intention-to-treat analysis of the EVEREST II trial. This is reaffirmed by the results of the ACCESS-EU study which found that the MitraClip in high risk patients with FMR was safe with low rates of hospital mortality and adverse events. Meaningful clinical improvement was observed, with objective improvement of quality of life and functional status reported (29).
In view of our findings, we conclude the non-inferiority of the MitraClip as a treatment for severe, symptomatic MR, in comparison to conventional valvular surgery. Despite a higher risk profile in the MitraClip patients, the clinical outcomes were comparable although surgery was more effective in reducing MR in the early post procedure period. In light of the apparent clinical benefits of the MitraClip in a real world patient population with significant comorbidities and high surgical risk, as well as the need for a safer solution in such patient populations, this meta-analysis supports the indication for MitraClip therapy in high risk-patients. Further randomised controlled trials with more consistent reporting of outcomes and longer follow-up periods will better evaluate the clinical benefits of the MitraClip system.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Iung B, Baron G, Tornos P, et al. Valvular heart disease in the community: a European experience. Curr Probl Cardiol 2007;32:609-61 [DOI] [PubMed] [Google Scholar]
- 2.Yun KL, Miller DC. Mitral valve repair versus replacement. Cardiol Clin 1991;9:315-27 [PubMed] [Google Scholar]
- 3.Olson LJ, Subramanian R, Ackermann DM, et al. Surgical pathology of the mitral valve: a study of 712 cases spanning 21 years. Mayo Clin Proc 1987;62:22-34 [DOI] [PubMed] [Google Scholar]
- 4.Taramasso M, Buzzatti N, La Canna G, et al. Interventional vs. surgical mitral valve therapy. Herz 2013;38:460-6 [DOI] [PubMed] [Google Scholar]
- 5.Carabello BA. The current therapy for mitral regurgitation. J Am Coll Cardiol 2008;52:319-26 [DOI] [PubMed] [Google Scholar]
- 6.Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406 [DOI] [PubMed] [Google Scholar]
- 7.Mauri L, Foster E, Glower DD, et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013;62:317-28 [DOI] [PubMed] [Google Scholar]
- 8.Munkholm-Larsen S, Wan B, Tian DH, et al. A systematic review on the safety and efficacy of percutaneous edge-to-edge mitral valve repair with the MitraClip system for high surgical risk candidates. Heart. 2013 doi: 10.1136/heartjnl-2013-304049. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Khan KS, ter Riet G, Glanville J, et al. eds. Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for those Carrying Out or Commissioning Reviews (CRD Report Number 4) (2nd edition). York (UK): NHS Centre for Reviews and Dissemination, University of York, 2001.
- 10.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12 [DOI] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N.Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88 [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conradi L, Treede H, Rudolph V, et al. Surgical or percutaneous mitral valve repair for secondary mitral regurgitation: comparison of patient characteristics and clinical outcomes. Eur J Cardiothorac Surg 2013;44:490-6; discussion 496 [DOI] [PubMed] [Google Scholar]
- 14.Paranskaya L, D’Ancona G, Bozdag-Turan I, et al. Percutaneous vs surgical repair of mitral valve regurgitation: single institution early and midterm outcomes. Can J Cardiol 2013;29:452-9 [DOI] [PubMed] [Google Scholar]
- 15.Taramasso M, Denti P, Buzzatti N, et al. Mitraclip therapy and surgical mitral repair in patients with moderate to severe left ventricular failure causing functional mitral regurgitation: a single-centre experience. Eur J Cardiothorac Surg 2012;42:920-6 [DOI] [PubMed] [Google Scholar]
- 16.Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007;28:230-68 [DOI] [PubMed] [Google Scholar]
- 17.Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation 1995;91:1022-8 [DOI] [PubMed] [Google Scholar]
- 18.Ciarka A, Braun J, Delgado V, et al. Predictors of mitral regurgitation recurrence in patients with heart failure undergoing mitral valve annuloplasty. Am J Cardiol 2010;106:395-401 [DOI] [PubMed] [Google Scholar]
- 19.Haan CK, Cabral CI, Conetta DA, et al. Selecting patients with mitral regurgitation and left ventricular dysfunction for isolated mitral valve surgery. Ann Thorac Surg 2004;78:820-5 [DOI] [PubMed] [Google Scholar]
- 20.Alfieri O, Maisano F, De Bonis M, et al. The double-orifice technique in mitral valve repair: a simple solution for complex problems. J Thorac Cardiovasc Surg 2001;122:674-81 [DOI] [PubMed] [Google Scholar]
- 21.Maisano F, Viganò G, Blasio A, et al. Surgical isolated edge-to-edge mitral valve repair without annuloplasty: clinical proof of the principle for an endovascular approach. EuroIntervention 2006;2:181-6 [PubMed] [Google Scholar]
- 22.Maisano F, Caldarola A, Blasio A, et al. Midterm results of edge-to-edge mitral valve repair without annuloplasty. J Thorac Cardiovasc Surg 2003;126:1987-97 [DOI] [PubMed] [Google Scholar]
- 23.Feldman T, Kar S, Rinaldi M, et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial Everest (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol 2009;54:686-94 [DOI] [PubMed] [Google Scholar]
- 24.Kar S, Rinaldi M, Lim S, et al. EVEREST II REALISM: A continued access study to evaluate the safety and effectiveness of the MitraClip device: Demographics and Procedural Outcomes. Society for Cardiovascular Angiography and Interventions (SCAI) 2011 Scientific Sessions, 2011. [Google Scholar]
- 25.Rogers JH, Franzen O. Percutaneous edge-to-edge MitraClip therapy in the management of mitral regurgitation. Eur Heart J 2011;32:2350-7 [DOI] [PubMed] [Google Scholar]
- 26.Mirabel M, Iung B, Baron G, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J 2007;28:1358-65 [DOI] [PubMed] [Google Scholar]
- 27.Schurer RA, Douglas YL, van der Werf HW, et al. Use of the MitraClip in high-risk patients with severe heart failure: are we ready to identify the right candidate? Eur J Heart Fail 2013;15:715-6 [DOI] [PubMed] [Google Scholar]
- 28.Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231-43 [DOI] [PubMed] [Google Scholar]
- 29.Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol 2013;62:1052-61 [DOI] [PubMed] [Google Scholar]


