Abstract
Background
Individuals living in primary care health professional shortage areas (PC-HPSA) often have difficulty obtaining medical care; however, no previous studies have examined association of PC-HPSA residence with prevalence of CVD risk factors.
Methods and Results
To examine this question, the authors used data from the Multi-Ethnic Study of Atherosclerosis baseline exam (2000–2002). Outcomes included the prevalence of diabetes, hypertension, hyperlipidemia, smoking and obesity as well as the awareness and control of diabetes, hypertension, and hyperlipidemia. Multivariable Poisson models were used to examine the independent association of PC-HPSA residence with each outcome. Models were sequentially adjusted for demographics, acculturation, socioeconomic status, access to health care and neighborhood socioeconomic status. Similar to the national average, 16.7% of MESA participants lived in a PC-HPSA. In unadjusted analyses, prevalence rates of diabetes (14.8% vs 11.0%), hypertension (48.2% vs 43.1%), obesity (35.7% vs 31.1%) and smoking (15.5% vs 12.1%) were significantly higher among residents of PC-HPSAs. There were no significant differences in the awareness or control of diabetes, hypertension, or hyperlipidemia. After adjustment, residence in a PC-HPSA was not independently associated with CVD risk factor prevalence, awareness or control.
Conclusions
This study suggests that increased prevalence of CVD risk factors in PC-HPSAs are explained by the demographic and socioeconomic characteristics of their residents. Future interventions aimed at increasing the number of primary care physicians may not improve cardiovascular risk without first addressing other factors underlying healthcare disparities.
Keywords: epidemiology, prevention, risk factors
Over 65 million Americans, one-fifth of the entire US population, live in a primary care health professional shortage area (PC-HPSA).1 These shortage areas are designated by the Health Resources and Services Administration as areas of unusually low primary care physician availability and/or high unmet population needs for primary care.1 Residents of primary care health professional shortage areas have less access to medical services including lack of a usual source of care, inability to get healthcare when needed and less outpatient care, especially preventative care.2–3 In addition, middle-aged and older individuals living in PC-HPSA’s report being in poorer general health as compared to non-residents.2, 4 A nationwide study of Medicare beneficiaries found that residence in a primary care shortage area was associated with a 70% higher rate of preventable hospitalizations.5
Most prior research on health professional shortage areas has focused on differences in general health status and overall healthcare utilization. 2, 4 Little is known about the potential impact of primary care physician shortages on prevalence of cardiovascular risk factors and what factors may mediate this association. In this study we examined the cross-sectional association between residence in a primary care shortage area and cardiovascular risk factor prevalence, awareness and control among participants of the Multiethnic Study of Atherosclerosis (MESA) study. Specifically, our aim was to examine whether demographic and socioeconomic characteristics mediate the association between residence in a primary care shortage area and the prevalence, awareness and control of cardiovascular risk factors. By understanding the impact of primary care availability on cardiovascular risk factors, we can identify and target community-level interventions to those in the greatest need.
METHODS
Individual-level data
The Multi-Ethnic Study of Atherosclerosis (MESA) is a multicenter, prospective cohort study of individuals aged 45–84 years. Begun in 2000–2002, it was designed to investigate the prevalence, correlates, and progression of subclinical cardiovascular disease. Further details on the study design have been published previously.6 The study enrolled 6,814 African American, Chinese, Hispanic, and non-Hispanic white men and women, recruited from 6 communities across the US: Forsyth County, North Carolina; northern Manhattan and the Bronx, New York; Baltimore City and Baltimore County, Maryland; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles, California. Individuals were excluded if they had known prior clinical cardiovascular disease, any prior cardiovascular procedure, weighed >300 pounds (135 kg), were pregnant, or had an impediment to long-term participation. The MESA protocol was approved by the institutional review boards of all collaborating institutions and the National Heart, Lung, and Blood Institute (Bethesda, Maryland).
The present study included all MESA participants who participated in the ancillary MESA Neighborhood Study and had geocoded information available at baseline. Individuals whose did not consent to the ancillary MESA neighborhood study (n=623) or whose address could not be reliably linked to the census tract (n=167) were excluded from this study.
The outcome variables examined in this study include the baseline prevalence of diabetes, hypertension, hyperlipidemia, obesity and smoking, the awareness of having diabetes, hypertension, or hyperlipidemia, and control of hypertension and hyperlipidemia among people with these risk factors. Total, low-density, and high-density lipoprotein cholesterol, and plasma glucose were measured from blood samples obtained after a 12-hour fast. Seated, resting blood pressure was measured 3 times; the mean of the last 2 blood pressure measurements was used.6
Hypertension prevalence and control were defined according the JNC VII criteria.7 Prevalent hypertension was defined as systolic blood pressure ≥ 140 mm/Hg or diastolic blood pressure ≥ 90 mm/Hg or self reported use of any anti-hypertensive medication. Individuals were considered to be aware of their hypertension if they self-reported a diagnosis of hypertension or were being treated with antihypertensive medications. Among hypertensive individuals, hypertension was considered under control if their systolic blood pressure was less than 140 mm/Hg and diastolic blood pressure less than 90 mm/Hg or SBP less than 130 mm/Hg and DBP less than 80 for individuals with diabetes.
Hyperlipidemia was defined as LDL cholesterol concentration ≥ 160 mg/dL according to the ATP III guidelines or self-reported use of lipid-lowering medication.8 Individuals were considered to be aware of their hyperlipidemia if they self-reported a diagnosis of hypertension or were being treated with lipid-lowering medications. Among individuals with hyperlipidemia, controlled hyperlipidemia was defined as having an LDL cholesterol concentration less than ATP III goals based on CHD risk classification: 0–1 risk factor - < 160 mg/dL; 2+ risk factors and 10-year CHD risk ≤20% - <130 mg/dL; CHD, CHD Risk Equivalent or 10-yr CHD risk >20% - <100 mg/dL.
Diabetes was defined according the American Diabetes Association 2010 Guidelines as fasting glucose of ≥ 126 mg/dL or self-reported use of any anti-diabetic medications.9 Individuals were considered to be aware of their diabetes if they self-reported a diagnosis of diabetes or were being treated with anti-diabetic medications. BMI was categorized as normal weight( <25.0), overweight (25.0–29.9), and obese (≥ 30) in accordance with definitions from the World Health Organization10 and the National Heart, Lung and Blood Institute11 Smoking status was categorized as never smoker, ex-smoker (smoked > 1 year ago) and current smoker according to self-report. Individuals who reported either being diagnosed by their physician or using appropriate medications were considered aware of the risk factor. In addition, we also examined the cumulative number of prevalent risk factors.
Additional participant covariates included study site and patient demographics such as age, gender, race/ethnicity, education level (categorized as less than high school; high school graduate; some college; college graduate; graduate school), marital status, country of birth (US, Puerto Rico, Other), language primarily spoken at home (English, other), employment, residential status (rent, own home, pay mortgage, other), gross family income (dichotomized as <$40,000 and ≥$40,000; $40,000 is approximately the cohort’s mean income), resided length of residence at current location (years), and family history of a heart attack. In addition, participants’ access to care as determined by their insurance status (categorized as HMO/Private Insurance; Medicaid; Medicare; Military/VA; Other; No Health Insurance) and usual source of care (categorized as Doctor’s Office or Clinic; Hospital or Emergency Room; Other) were examined. All covariates were assessed by questionnaire.
Area-level data
The primary exposure in this study was residence in a primary care health professional shortage area. Primary care health professional shortage areas are defined by the U.S Department of Health and Human Services, Health Resources and Services Administration as geographic areas, including counties or clusters of census tracts in metropolitan areas, which are rational areas for the delivery of primary medical care services and either have a population to full-time-equivalent primary care physician ratio of at least 3,500:1, or a population to full-time equivalent primary care physician ratio of less than 3,500:1 but greater than 3,000:1 and unusually high needs for primary care services or insufficient capacity of existing primary care providers.1 In addition, primary medical professionals in contiguous areas must be over-utilized, excessively distant, or inaccessible to the population under consideration.1 Additional details of the Primary Care Shortage Area Definition can be found in the Online Data Supplement, Expanded Methods. Participants were linked to data on PC-HPSA from the Health Resources and Services Administration based on their census tract of residence creating a binary indicator for each participant identifying whether they lived in a PC-HPSA or not.
In order to take into account the neighborhood environment five neighborhood scores were derived using factor analysis from 2000 census variables at the census tract level and were included as covariates. These five scores reflect neighborhood: 1) Poverty (% vacant housing, % no telephone, % no vehicle, % unemployed, median household income, % poverty); 2) Education/Occupation (% at least a bachelors degree, % non-managerial occupation, % households with interest/dividends); 3) Immigrants/Crowding (% Hispanic, % Asian, % foreign born, % crowded houses i.e. more than one person per room); 4) African American / Family Structure (% African American, % single parent households); and 5) Residential Instability (% not in the same house since 1995).
Statistical analyses
In descriptive analyses, the distributions of participant characteristics --including site, age, gender, race/ethnicity, education, income, marital status, employment, country of birth, primary language, insurance status, usual source of care, residential status, length of residence at current location and neighborhood SES-- were examined overall and stratified by residence in a primary care health professional shortage area. We then examined the prevalence, awareness, treatment and control of cardiovascular risk factors (diabetes, hypertension, hyperlipidemia, obesity and smoking) among PC-HPSA residents and non-residents. Chi-Square and t-tests were utilized as appropriate to determine statistical significance.
Prevalence ratios were calculated using a log-linear model. All analyses were done separately for each outcome (the prevalence, awareness, and control of each cardiovascular risk factor; cumulative risk factors). Analyses of awareness and control were restricted to participants with the condition of interest. The models were sequentially adjusted for participant characteristics: Model 1 – unadjusted; Model 2 – adjusted age, gender, race/ethnicity, site, marital status and education; Model 3 – added born in the US (y/n), English spoken in home; Model 4 – added income <$40,000, residential status, employment, insurance; Model 5 – added usual source of care, payment for usual care; Model 6 – added 5 neighborhood SES factors (included as continuous covariates
We conducted several sensitivity analyses to test the robustness of our findings. We used propensity score matching to investigate the robustness of our results with tighter control for confounders. HPSA residents were matched 1:1 with non-residents using a greedy matching algorithm set to match individuals with propensity scores ±0.005. We conducted further analyses among a subsample of participants who had lived at the same address for at least 20 years. Lastly, we used generalized estimating equations (GEE) models to account for any clustering of individuals within neighborhoods.
RESULTS
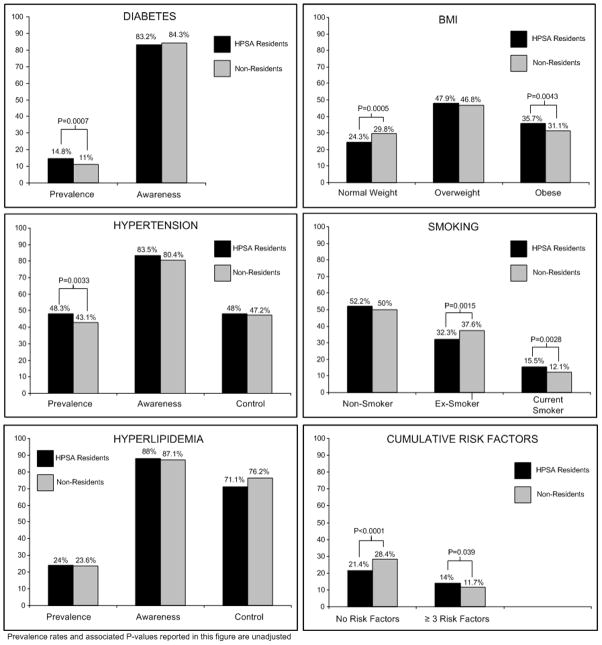
Similar to the national average, 16.7% of the MESA participants were residents of a primary care health professional shortage area. PC-HPSA residents were more likely to be African American or Hispanic, had less education with almost a quarter having less than a high school education, had a lower family income, and were less likely to speak English at home compared to non-residents (Table 1). The majority of MESA participants who were PC-HPSA residents lived in NYC, Los Angeles and Chicago. In unadjusted analyses, residence in an HPSA was associated with higher prevalence of individual risk factors including diabetes, hypertension, obesity, and smoking (Table 2; Figure 1). PC-HPSA residents were 25% less likely to have no risk factors and over 20% more likely to have 3 or more risk factors. In contrast, HPSA residence was not significantly associated with risk factor awareness or control.
Table 1.
Participant Characteristics by Residence in a Primary Care Shortage Area among MESA Participants, Baseline Exam (2000–2002)
| Total (n=6,047) | Residence in an PC-HPSA
|
|||
|---|---|---|---|---|
| Yes (n=1,008) | No (n=5,039) | P-value | ||
| Age, mean (SD), years | 61.9 (10.1) | 62.1 (10.3) | 61.9 (10.1) | 0.52 |
| Female, % | 52.4 | 55.1 | 51.9 | 0.07 |
| Race/Ethnicity, % | <0.0001 | |||
| Caucasian | 39.5 | 9.0 | 45.6 | |
| Chinese | 11.8 | 7.2 | 12.7 | |
| African American | 27.0 | 44.6 | 23.5 | |
| Hispanic | 21.7 | 39.1 | 18.2 | |
| Education, % | ||||
| Less than High School | 16.9 | 28.9 | 14.5 | <0.0001 |
| High School Graduate | 18.2 | 18.6 | 18.2 | 0.78 |
| Some College | 28.5 | 29.4 | 28.4 | 0.53 |
| College Graduate | 17.9 | 12.4 | 19.0 | <0.0001 |
| Graduate School | 18.4 | 10.8 | 20.0 | <0.0001 |
| Site, % | <0.0001 | |||
| Forsyth County, North Carolina | 15.7 | 0.1 | 18.8 | |
| New York City, New York | 16.1 | 56.1 | 8.1 | |
| Baltimore, Maryland | 15.7 | 2.2 | 18.4 | |
| St. Paul, Minnesota | 16.0 | 1.1 | 19.0 | |
| Chicago, Illinois | 17.5 | 29.1 | 15.2 | |
| Los Angeles, California | 19.0 | 11.5 | 20.5 | |
| Family Income < $40,000 | 49.0 | 63.2 | 46.1 | <0.0001 |
| Time Lived in Neighborhood, median, years | 16.0 | 21.6 | 15.0 | <0.0001 |
| Health Insurance, % | ||||
| HMO/Private Insurance | 70.6 | 65.7 | 71.6 | 0.0002 |
| Medicaid | 6.7 | 12.6 | 5.5 | <0.0001 |
| Medicare | 35.1 | 34.5 | 35.2 | 0.66 |
| Military or Veterans Affairs | 3.6 | 4.3 | 3.5 | 0.21 |
| Other | 6.5 | 5.3 | 6.8 | 0.08 |
| No Health Insurance | 8.3 | 8.4 | 8.3 | 0.91 |
| Married, % | 61.7 | 52.1 | 63.6 | <0.0001 |
| Usual Source of Care, % | 0.16 | |||
| Doctor’s Office / Clinic | 93.3 | 93.2 | 93.4 | |
| Hospital or Emergency Room | 2.8 | 3.5 | 2.6 | |
| Other | 3.9 | 3.3 | 4.0 | |
| Birthplace, % | <0.0001 | |||
| US | 69.1 | 51.8 | 72.6 | |
| Puerto Rico | 2.2 | 7.4 | 1.2 | |
| Other Country | 28.7 | 40.8 | 26.2 | |
| English Spoken at Home, % | 75.9 | 50.8 | 79.7 | <0.0001 |
| Employment, % | <0.0001 | |||
| Homemaker | 10.9 | 9.1 | 11.3 | |
| Employed Full-Time | 39.6 | 38.3 | 39.8 | |
| Employed Part-Time | 8.9 | 6.4 | 9.4 | |
| Employed, On Leave | 1.0 | 1.9 | 0.9 | |
| Unemployed | 2.1 | 3.2 | 1.9 | |
| Retired | 37.5 | 41.2 | 36.8 | |
| Residential Status, % | <0.0001 | |||
| Rent | 27.7 | 57.6 | 21.7 | |
| Paying Mortgage | 40.4 | 21.5 | 44.2 | |
| Own | 28.3 | 16.8 | 30.6 | |
| Other | 3.6 | 4.1 | 3.6 | |
| Family History of Heart Attack, % Neighborhood SES Scores, mean (SD) | 33.3 | 29.8 | 34.0 | 0.0019 |
| Score 1 – Poverty | 0.22 (1.03) | 1.38 (0.76) | −0.01 (0.92) | <0.0001 |
| Score 2 – Education / Occupation | −0.37 (1.26) | 0.42 (0.82) | −0.52 (1.28) | <0.0001 |
| Score 3 – Immigrants / Crowding | 0.79 (1.09) | 1.39 (1.16) | 0.67 (1.03) | <0.0001 |
| Score 4 – African American / | 0.57 (0.93) | 1.41 (0.74) | 0.40 (0.87) | <0.0001 |
| Score 5 – Residential Instability | 0.41 (0.96) | 0.97 (0.82) | 0.29 (0.94) | <0.0001 |
Abbreviations: MESA, Multi-Ethnic Study of Atherosclerosis; PC-HPSA, Primary Care Health Professional Shortage Area; SD, standard deviation; HMO, Health Maintenance Organization; SES, socioeconomic status
Table 2.
Risk Factor Prevalence, Awareness and Control by Residence in a Primary Care Shortage Area among MESA participants, Baseline Exam (2000–2002)
| Residence in an PC-HPSA
|
||||||
|---|---|---|---|---|---|---|
| Total | Yes | No | P-value | Prevalence Ratio | 95% CI | |
| Diabetes, % | ||||||
| Prevalence | 11.6 | 14.8 | 11.0 | <0.001 | 1.34 | 1.12, 1.61 |
| Awareness* | 84.1 | 83.2 | 84.3 | 0.74 | 0.99 | 0.81, 1.20 |
| Hypertension, % | ||||||
| Prevalence | 44.0 | 48.2 | 43.1 | 0.003 | 1.12 | 1.01, 1.23 |
| Awareness* | 81.0 | 83.5 | 80.4 | 0.12 | 1.04 | 0.93, 1.16 |
| Control* | 43.7 | 42.8 | 44.0 | 0.73 | 0.97 | 0.84, 1.13 |
| Hyperlipidemia, % | ||||||
| Prevalence | 23.6 | 24.0 | 23.6 | 0.76 | 1.02 | 0.89, 1.17 |
| Awareness* | 87.3 | 88.0 | 87.1 | 0.70 | 1.01 | 0.87, 1.17 |
| Control* | 54.6 | 51.2 | 55.3 | 0.44 | 0.93 | 0.77, 1.12 |
| BMI, % | ||||||
| Normal Weight | 28.9 | 24.3 | 29.8 | <0.001 | 0.82 | 0.71, 0.93 |
| Overweight | 47.0 | 47.9 | 46.8 | 0.53 | 1.02 | 0.93, 1.13 |
| Obese | 31.9 | 35.7 | 31.1 | 0.004 | 1.15 | 1.02, 1.29 |
| Smoking, % | ||||||
| Never Smoked | 50.4 | 52.2 | 50.0 | 0.20 | 1.04 | 0.95, 1.15 |
| Previously Smoked | 36.8 | 32.3 | 37.6 | 0.001 | 0.86 | 0.76, 0.97 |
| Current Smoker | 12.6 | 15.5 | 12.1 | 0.003 | 1.28 | 1.08, 1.53 |
| Cumulative Number of Risk Factors, % | ||||||
| None | 27.3 | 21.4 | 28.4 | <0.0001 | 0.75 | 0.65, 0.87 |
| 3 or More Risk Factors | 12.1 | 14.0 | 11.7 | 0.04 | 1.20 | 1.00, 1.44 |
Abbreviations: MESA, Multi-Ethnic Study of Atherosclerosis; PC-HPSA, Primary Care Health Professional Shortage Areas; CI, confidence interval; BMI, body mass index *Among prevalent cases (hypertension, n=2656; hyperlipidemia, n=1429; diabetes, n=704)
Figure 1.
Cardiovascular Risk Factors by Residence in a Primary Care Health Professional Shortage Area among MESA Participants, Baseline Exam (2000–2002).
In risk-adjusted results PC-HPSA residence was not independently associated with any risk factor prevalence, awareness or control (Table 3). Participant demographic and socioeconomic characteristics, particularly race/ethnicity and site, explained most of the association between cardiovascular risk factors and residence in a PC-HPSA. For example, in an unadjusted model, residents of HPSAs had a 34% greater likelihood of having prevalent diabetes. The excess risk of diabetes dropped by approximately 65% when participant demographics were included in the model. An additional 1.4%, 9.1%, 6.4% and 6.3% decrease in excess risk was seen with the addition of acculturation, socioeconomic status, access to health care, and neighborhood SES, respectively.
Table 3.
Prevalence Ratios from Multivariate Models of Risk Factor Prevalence, Awareness and Control for Residence in a Primary Care Shortage Area among MESA participants, Baseline Exam (2000–2002)
| Model 1: Unadjusted | Model 2: Plus Demographics§ | Model 3: Plus Acculturation|| | Model 4: Plus Socio-Economic Variables# | Model 5: Plus Access to Health Care** | Model 6: Plus Neighborhood SES§§ | |
|---|---|---|---|---|---|---|
| Diabetes | ||||||
| Prevalence | 1.34† | 1.12 | 1.11 | 1.08 | 1.06 | 1.04 |
| Awareness* | 0.99 | 1.03 | 1.03 | 1.03 | 1.00 | 1.01 |
| Hypertension | ||||||
| Prevalence | 1.12† | 1.03 | 1.03 | 1.02 | 1.02 | 0.97 |
| Awareness * | 1.04 | 0.97 | 0.96 | 0.96 | 0.96 | 0.93 |
| Control * | 0.97 | 0.88 | 0.88 | 0.88 | 0.87 | 0.86 |
| Hyperlipidemia | ||||||
| Prevalence | 1.02 | 1.12 | 1.11 | 1.12 | 1.09 | 1.13 |
| Awareness * | 1.01 | 1.00 | 1.00 | 0.99 | 0.99 | 1.01 |
| Control* | 0.93 | 1.00 | 1.00 | 0.98 | 0.98 | 0.96 |
| BMI | ||||||
| Normal Weight | 0.82† | 0.96 | 0.97 | 0.96 | 0.96 | 0.99 |
| Overweight | 1.02 | 1.05 | 1.05 | 1.06 | 1.06 | 1.08 |
| Obese | 1.15† | 1.09 | 1.08 | 1.08 | 1.08 | 1.00 |
| Smoking | ||||||
| Never Smoked | 1.04 | 1.05 | 1.05 | 1.05 | 1.05 | 1.07 |
| Previously Smoked | 0.86† | 0.89 | 0.89 | 0.90 | 0.89 | 0.91 |
| Current Smoker | 1.28† | 1.16 | 1.16 | 1.13 | 1.14 | 1.00 |
| Cumulative Number of Risk Factors | ||||||
| None | 0.75‡ | 0.90 | 0.90 | 0.91 | 0.91 | 0.97 |
| 3 or More Risk Factors | 1.20 | 1.07 | 1.06 | 1.03 | 1.02 | 0.94 |
Abbreviations: MESA, Multi-Ethnic Study of Atherosclerosis; SES, socioeconomic status; BMI, body mass index
Among prevalent cases (hypertension, n=2656; hyperlipidemia, n=1429; diabetes, n=704)
P<0.05;
P<0.001
Model includeddemographic covariates including age, gender, race/ethnicity, site, marital status and education.
Model included demographics plus measures of acculturation covariates including born in the US and English spoken in home.
Model included demographics, acculturation plus socioeconomic covariates including income <$40,000, residential status, employment and health insurance.
Model included demographics, acculturation, socioeconomic and health care access covariates including usual source of care and source of payment for usual care.
Model included demographics, acculturation, socioeconomic, health care access and neighborhood SES covariates including neighborhood poverty, education/occupation, immigrants/crowding, percentage African American/family structure and residential stability.
Findings were similar in sensitivity analyses using propensity score matching, restricted to individuals living at the same address for at least 20 years and controlled for neighborhood clustering. In exporatory analyses, six interaction terms were examined for each outcome. No consistently significant interaction terms were identified across outcomes. There were some significant interaction terms for specific outcomes (hpsa*age for smoking; hpsa*gender for obesity, normal weight, no risk factors and all controlled; HPSA*no insurance for hyperlipidemia awareness), potentially due to the large number interactions tested. When we conducted stratified risk-adjusted analyses, the association of the outcomes with PC-HPSA remained non-significant in all strata.
DISCUSSION
We examined the association between residence in a primary care health professional shortage area and cardiovascular risk factor prevalence, awareness and control among MESA participants, a large diverse, population-based cohort. Residents of PC-HPSAs had a higher prevalence of individual risk factors as well as a greater cumulative number of risk factors. The increase in CVD risk factors among residents of PC-HPSAs was primarily due to the higher proportion of African American and Hispanic individuals as well as the lower socioeconomic status of the residents. Residents of areas in which primary care physicians were more readily available did not have better cardiovascular risk factor awareness or control.
This study is one of the first to report on the association between residence in PC-HPSAs and cardiovascular risk factors. Our findings of a higher prevalence of CVD risk factors and a greater cumulative number of CVD risk factors among PC-HPSA residents are consistent with prior studies that found poorer general health among residents of PC-HPSAs. Previous studies have reported conflicting findings as to whether associations of health with PC-HPSA residence remain significant after adjustment for factors such as demographic characteristics, health care availability, health insurance, and clinical characteristics. In our study, higher prevalence of CVD risk factors among PC-HPSA residents was primarily due to racial/ethnic and SES disparities and did not remain significant in multivariate analyses adjusting for factors such as age, race/ethnicity, sex, site, marital status and education. Previous reports have found associations of PC-HPSA residence with decreased health care utilization including cancer screening, mammography and pap smears, in bivariate analyses.3, 12 However, after adjustment for demographic characteristics, health insurance, cost of care, and health care access, women who lived in PC-HPSAs were equally likely to have received a mammogram in the past 2 years or a pap smear in the last 3 years as compared with women not living a PC-HPSA;3, 12 although, women who lived in PC-HPSA remained more likely to have adhered to mammography guidelines and received the appropriate lifetime number of exams.3
Upon examination of health outcomes, Parchman and colleagues found that elderly adults in poor health who live in PC-HPSAs are 70% more likely to experience a preventable hospitalization even after adjustment demographic and socioeconomic characteristics.5 Similarly, among two state-based studies including almost 500 Kentucky4 and 10,940 West Virginian residents2, respectively, residents of PC-HPSAs were found to have significantly poorer general health (as defined by a 5-point Likert scale and the Medical Outcomes Study Short form, respectively) even after risk adjustment. Importantly, both of these studies were conducted on the county level and therefore excluded residents of counties with only partial HPSA designation. Only about half of all HPSAs include the entire county, the other half include only parts of counties such as specific census tracts.13 This exclusion resulted in all HPSA residents being mostly White and from rural counties and thus limits their generalizability to more diverse, urban populations.
The findings from this study suggest that residence in a federally-designated primary care health professional shortage area is not independently associated with cardiovascular risk factors. Instead, health care quality and continuity of care may be more important predictors of CVD risk. In other studies, patients with congestive heart failure or coronary heart disease who received care at community health centers, often located in low-income HPSA areas (as compared to hospital-based practices) were found to be less likely to get a cardiology consultation, a marker of better quality of care, and had 20% fewer follow-up consultations, a measure of continuity of care.14 Further study is needed to identify how differences in the quality and continuity of care may mediate the relationship between availability of care and health.
The Multi-Ethnic Study of Atherosclerosis study is a prospective, diverse, population-based study which includes detailed information on participants’ residence over the past 20 years. An additional strength of this study includes the detailed assessment of cardiovascular risk factors.6 Unlike previous research, in this study we conducted the analyses at the census tract level, and adjusted for participants’ neighborhood socioeconomic status. However, our study has several limitations. MESA is a large population-based cohort that recruited from geographically diverse sites across the country; however it is not nationally representative nor was it designed to be geographically representative of its sites. In addition, MESA participants may not reflect average PC-HPSA residents, as the study recruited from urban centers. Although in MESA a random sample was selected, those who chose to participate may have had more familiarity or comfort with the healthcare system; for example, only about 8% of the MESA participants included in this study were uninsured, compared with the national average of 14%.15 In addition the proportion of MESA residents who lived in a PC-HPSA was 16% as compared to the national average of approximately 20%.1 We used the federal PC-HPSA designation as a marker for physician availability. However, HPSA designation is not automatic and requires effort on the part of state and government officials in pursing a designation. This may result in some eligible counties not receiving the designation and thereby cause us to underestimate the relationship between PC-HPSA and CVD risk factors. Lastly, this study was cross-sectional and thus temporality could not be established. We did however, have similar findings even when we restricted the analyses to individuals who had lived in the same residence for 20 years or more. In addition, survival bias may have explained our failure to find adjusted associations. The focus of this study was to examine the association with cardiovascular risk factors, therefore we did not determine whether residence in a PC-HPSA was associated with increased healthcare costs, utilization or outcomes. Future studies are needed to examine these associations.
In summary, we found that although CVD risk factor prevalence is higher among residents of primary care health professional shortage areas, these findings were primarily due to a high proportion of individuals with low SES and from minority ethnic groups. Availabililty of primary care physicians was not independently associated with CVD risk factor prevalence, awareness or control. These findings suggest that attempts to improve health care access by ensuring adequate numbers of primary care physicians or assigning more resources without also addressing other factors underlying healthcare disparities (SES, cultural norms, acculturation, community education, etc) may not be effective; rather all factors need to be addressed simultaneously. Further research is needed to take a closer look at specific factors underlying health disparities among minority groups and how these can be effectively addressed.
Supplementary Material
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Funding Sources: This research was supported by an NHLBI Training Grant in Cardiovascular Epidemiology and Prevention (grant T32HL069771) and contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute.
Footnotes
Conflict of Interest Disclosures: None
References
- 1.US Department of Health and Human Services Health Resources and Services Administration. [Accessed 6/29/2009];Shortage Designation: HPSAs, MUAs & MUPs. 2009 http://bhpr.hrsa.gov/shortage/
- 2.Liu JJ. Health professional shortage and health status and health care access. J Health Care Poor Underserved. 2007;18:590–598. doi: 10.1353/hpu.2007.0062. [DOI] [PubMed] [Google Scholar]
- 3.Phillips KA, Kerlikowske K, Baker LC, Chang SW, Brown ML. Factors associated with women's adherence to mammography screening guidelines. Health Serv Res. 1998;33:29–53. [PMC free article] [PubMed] [Google Scholar]
- 4.Kohrs FP, Mainous AG. The relationship of health professional shortage areas to health status. Implications for health manpower policy. Arch Fam Med. 1995;4:681–685. doi: 10.1001/archfami.4.8.681. [DOI] [PubMed] [Google Scholar]
- 5.Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas. An analysis of vulnerable Medicare beneficiaries. Arch Fam Med. 1999;8:487–491. doi: 10.1001/archfami.8.6.487. [DOI] [PubMed] [Google Scholar]
- 6.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 9.Daviglus ML, Pirzada A, Liu K, Yan LL, Garside DB, Dyer AR, Hoff JA, Kondos GT, Greenland P, Stamler J. Comparison of low risk and higher risk profiles in middle age to frequency and quantity of coronary artery calcium years later. Am J Cardiol. 2004;94:367–369. doi: 10.1016/j.amjcard.2004.04.038. [DOI] [PubMed] [Google Scholar]
- 10.WHO Consultancy on Obesity. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 2000. [PubMed] [Google Scholar]
- 11.NHLBI Expert Panel on the Identification Evaluation and Treatment of Overweight and Obesity in Adults. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Obesity Research. 1998;6:51S–209S. [PubMed] [Google Scholar]
- 12.Coughlin SS, Leadbetter S, Richards T, Sabatino SA. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Soc Sci Med. 2008;66:260–275. doi: 10.1016/j.socscimed.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 13.GAO. Health Care Shortage Areas: Designations Not a Useful Tool for Directing Resources to the Underserved. GAO/HEHS-92-200. 1995. [Google Scholar]
- 14.Cook NL, Ayanian JZ, Orav EJ, Hicks LS. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation. 2009;119:2463–2470. doi: 10.1161/CIRCULATIONAHA.108.825133. [DOI] [PubMed] [Google Scholar]
- 15.US Census Bureau. Health Insurance Coverage: 2000. 2001. pp. 60–215. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.