Abstract
When replacing percutaneous endoscopic gastrostomy (PEG) tubes, an internal bolster may be retrieved either percutaneously or endoscopically. The aim of this study was to compare the complications of percutaneous and endoscopic method during PEG tube replacement. The medical records of 330 patients who received PEG tube replacement were retrospectively analyzed. According to the removal method of internal bolster, we categorized as endoscopic group and percutaneous group. Demographic data, procedure-related complications and risk factors were investigated. There were 176 cases (53.3%) in endoscopic group and 154 cases (46.7%) in percutaneous group. The overall immediate complication rate during PEG tube replacement was 4.8%. Bleeding from the stoma (1.3%) occurred in percutaneous group, whereas esophageal mucosal laceration (7.4%) and microperforation (0.6%) occurred in endoscopic group. The immediate complication rate was significantly lower in the percutaneous method (OR, 6.57; 95% CI, 1.47-29.38, P=0.014). In multivariate analysis, old age was a significant risk factor of esophageal laceration and microperforation during PEG tube replacement (OR, 3.83; 95% CI, 1.04-14.07, P=0.043). The percutaneous method may be more safe and feasible for replacing PEG tubes than the endoscopic method in old patients.
Keywords: Gastrostomy, Methods, Complications
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) is a relatively safe procedure to deliver enteral feedings to patients unable to feed by mouth (1). Since its introduction in the early 1980s, there has been a geometrical rise in the use of this technique among the elderly patients (2). While only 15,000 PEG tubes were placed in the year 1989, its placement frequency had increased significantly to more than 200,000 tubes annually; and this trend is projected to continue increasing, especially in elderly patient (3).
However, PEG is not a permanent device and requires periodic replacement because of degradation, infection, leakage and malfunction (4, 5). There are two replacement methods for the PEG tube (6, 7). The internal bumper can be removed percutaneous by pulling the PEG tube out through the abdominal wall, the "percutaneous method" (6). Alternatively, the PEG tube may be removed endoscopically by grasping the internal bumper with a snare or basket and extracting it via the oral cavity in a retrograde fashion, the "endoscopic method" (7).
The percutaneous method is advantageous for some patients who did not possible repeated endoscopic procedure; for example, patients with head and neck surgery or esophageal carcinomas (6). However, percutaneous method has the potential to injure the gastrocutaneous stoma or tract. Endoscopic method is preferred in patients who had abdominal surgery, the case of previously rigid internal bolster was inserted, and if there was any problem related to accessing the gastrostomy site (7).
Serious complications had been reported related to percutaneous method, such as massive bleeding, and tract disruption (5, 8). Complications of endoscopic removal of PEG tube has been also reported, such as upper airway obstruction and esophageal mucosal injury (7). However, there are no published data about direct compare the complication rate of PEG tube replacement by percutaneous and endoscopic method.
The aim of this study was to investigate the incidence and type of complications associated with the PEG replacement procedure between the percutaneous and endoscopic method. The risk factor associated with immediate complications such as bleeding and perforation during PEG tube replacement were also investigated.
MATERIALS AND METHODS
Study design
The medical records of patients who received PEG tubes replacement at the Dongguk University Ilsan Hospital from January 2008 through January 2012 were analyzed retrospectively. A total of 377 cases of PEG tube were replaced during the study period. Of these 47 cases were excluded due to young age (n=6), or self-removal (n=41). Final analyses were performed in 330 cases. We examined age, sex, comorbidity, mean interval of PEG tube replacement, indication for PEG tube replacement (routine, malfunction, leakage, and infection) and complications in both percutaneous and endoscopic method group.
Procedures
A bumper-type internal bolster (PEG-PULL-S, 24Fr, Cook Medical, Bloomington, IN, USA) was used for every case. All of the procedures were performed by four endoscopists with experiences of more than 10,000 cases of esophagogastroduodenoscopy (EGD) and 3,000 cases of colonoscopy.
Aspirin and antiplatelet agent did not routinely hold before PEG tube replacement. Warfarin was stopped for 5 days before the procedure. Then heparin was infused according to the prothrombin time or low molecular weight heparin was subcutaneously injected in patients with high risk of thromboembolism. In the cases of low risk, heparinization was not performed. If signs of bleeding were not observed, warfarin was resumed at 12 hr after the procedure.
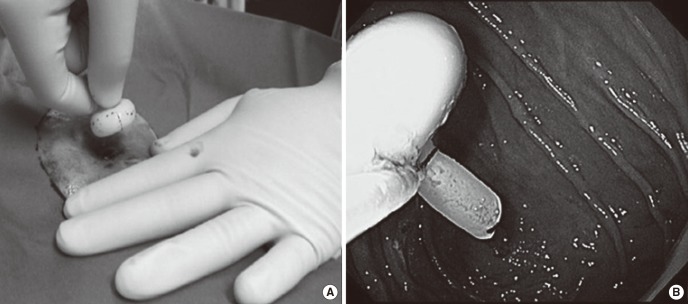
Percutaneous replacement was performed by removing the feeding device with external traction from the abdominal wall. The PEG tube was mobilized by pulling back and a mobilized tube moves freely in and out of the stoma. At this stage, the external tube was removed by traction by pulling. Then, endoscopic procedure was required to insertion new feeding device and to confirm appropriate positioning of the internal bolster (Fig. 1A).
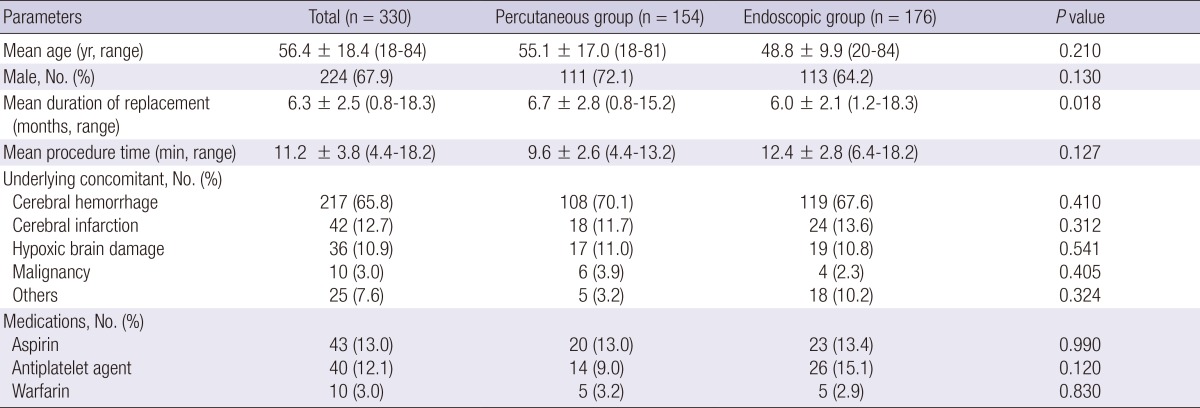
Fig. 1.
Photographs of removal. (A) Percutaneous method: PEG tube can be removed by pulling the PEG tube out of the abdominal wall. (B) Endoscopic method: Remnant tube adjacent to the bumper was captured the snare under endoscopic guide, then, it was retrieved out of the mouth.
For the endoscopic method, a video endoscope (GIF H260, Olympus Optical Co, Tokyo, Japan) was inserted into the oropharynx down the esophagus into the stomach. Tube replacement was done by cutting the old PEG tube bumper at skin level. A PEG bumper was removed by grasping it with a snare or basket and extracting it via the oral cavity in a retrograde method. A new PEG tube was inserted along the guide wire. Finally, endoscopic examination confirmed the appropriate position of the internal bumper and any procedure-related complications (Fig. 1B).
Definitions
Old age was defined an age as that was more than 65 year-old according to World Health Organizations definition. Short interval of PEG tube replacement was defined as less than 6 months.
Complication was categorized as immediate complication and late complication. Immediate complication was referred to the direct complication occurred during procedure. Late complication was defined occurring within 1 month after PEG tube replacement.
Immediate complication was divided in mechanical complication and peristomal bleeding. A laceration was defined as a linear or geographic tearing of esophageal mucosa or submucosa that was visible during the procedure. A microperforation was defined perforation as that was not visible during the procedure, however, that was identified as abnormal free air on a chest X-ray after procedure. Peristomal bleeding was categorized to external opening bleeding and stomach opening bleeding. External opening bleeding was defined significant complication for more than 3 min hemorrhage as that was oozing of blood by external compression of stoma. Stomach opening bleeding was defined when endoscopic intervention was required including epinephrine injection (1:10,000 dilutions).
Late complications were divided in peristomal infection and PEG site leakage. Peristomal infection was evaluated in accordance with the Jain infection score (9). Individual scores for erythema, induration, and exudate were added up. If sum of the score was 8 or if a purulent exudate with bacteriological evidence was detected, a diagnosis of peristomal infection was made (9). PEG site leakage was defined leakage or oozing of feeding material out of peristomal site and required to new PEG tube replacement because of it.
Statistics analysis
Data were represented as mean±standard deviation for continuous variables or number (%) for categorical variables. Differences in the baseline continuous variables between the patients with age and mean duration of replacement were evaluated using t test. The chi-square test and Fisher's exact test were used to test for differences in the baseline categorical variables between patients with underlying concomitant disease, medication and complication.
After identifying the significant factors using univariate analysis, multiple logistic regression analysis was used to describe the association between variables and immediate complications of PEG tube replacement. All variables with P values <0.05 on univariate analysis were included in the multivariate analysis. A P value less than 0.05 was considered statistically significant. Data were analyzed using IBM SPSS Statistics version 20.0 (IBM Co., Amonk, NY, USA).
Ethics statement
The study protocol was approved by the institutional review board of Dongguk University Ilsan Hospital (IRB No. 2012-55). Informed consent was exempted by the board.
RESULTS
Baseline characteristics of PEG tube replacement
A total 330 cases of PEG tube were replaced. The mean age was 56.4±18.4 yr (range, 18 to 84) and 224 (67.9%) patients were male. Most common comorbid diseases were cerebral infarction (217 cases, 65.8%), followed by hypoxic brain damage (36 cases, 10.9%). When associated with bleeding, aspirin (43 cases, 13.0%) was the most frequently taken drug in both groups. The mean interval of PEG tube placement was 6.3±2.5 months (range, 0.8 to 18.3 months) and mean procedure time was 11.2±3.8 min (range, 4.4 to 18.2 min).
Routine replacement performed in 264 (79.8%) cases was the most common indication, followed by PEG site infection (n=37, 11.2%), and of persistent leakage around gastrostomy site (n=14, 4.2%).
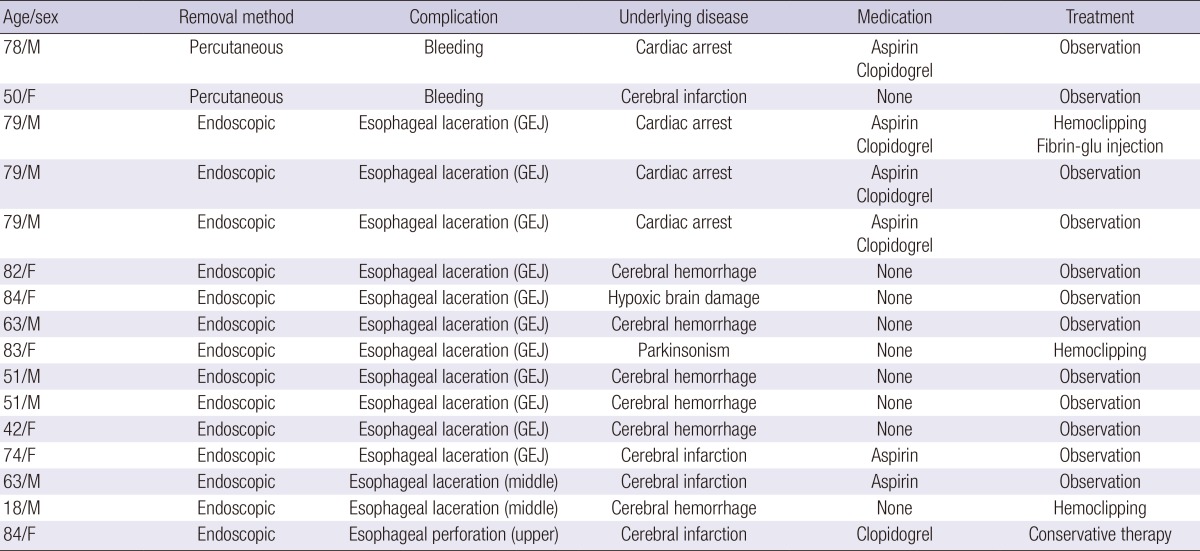
Of them, 176 cases (53.3%) were in endoscopic group and 154 cases (46.7%) were in percutaneous group. There were no patients in whom one method failed and switched to other procedure. There were no significant differences between two groups in baseline characteristics. However, the mean interval of PEG replacement was significantly longer in percutaneous group than in endoscopic group (6.7±2.8 months vs 6.0±2.1 months, P=0.018) (Table 1).
Table 1.
Characteristics of the patients
Others included cerebral palsy, multiple sclerosis, Parkinsonism and dementia.
Immediate complications
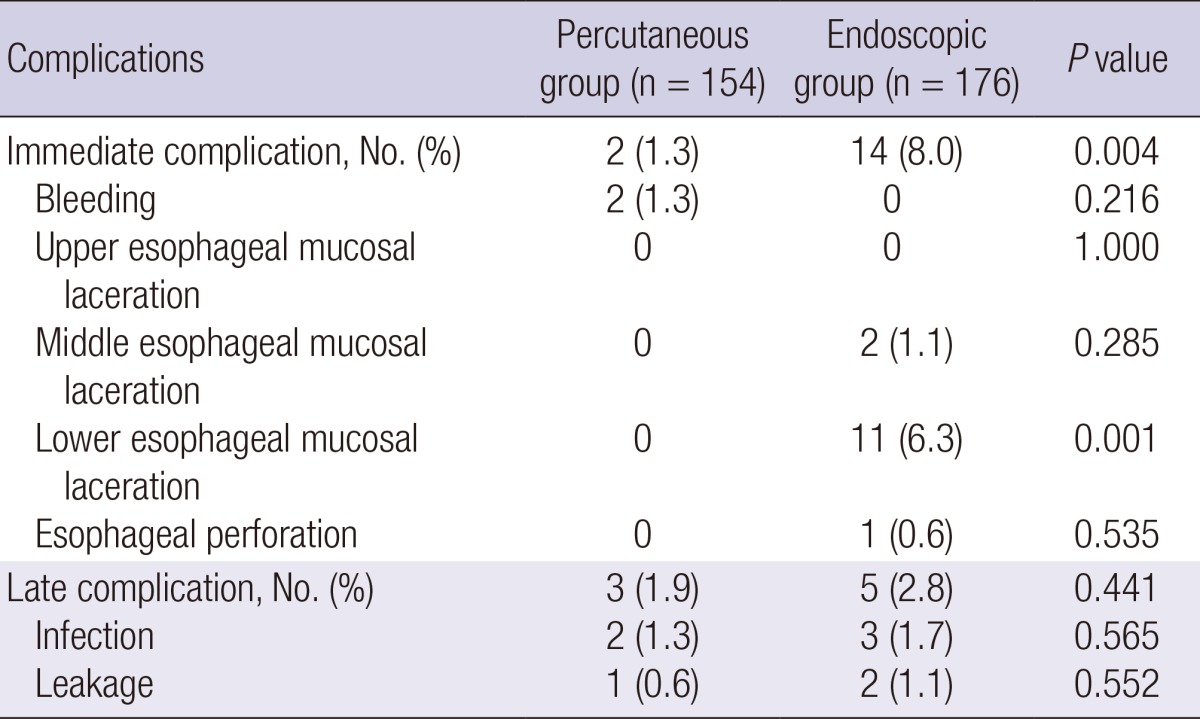
The overall immediate complications rate was 4.8% (16/330). All immediate complications during PEG tube replacement are described in Table 2. In percutaneous group, peristomal bleeding occurred in 2 cases (1.3%). Both bleedings were occurred in stomach opening and well controlled by endoscopic epinephrine injection. All two cases did not require new stoma or transfusion after hemostasis. In endoscopic group, esophageal laceration occurred in 13 cases (7.4%) and esophageal microperforation occurred in 1 case (0.6%). The lower esophagus was the most common injury site (5.7%) and mid-esophageal was affected in 2 cases (1.1%). Ten cases were treated by epinephrine spray through endoscopy to control oozing. Hemoclips were applied at both edges of laceration in the 3 cases. One case of the microperforation occurred in the upper esophagus of a patient who cooperated poorly during the procedure which was successfully treated with antibiotics and food fasting. There was no procedure-related death in both groups.
Table 2.
Immediate complications associated with PEG replacement (n=16)
GEJ, gastroesophageal junction.
Late complication
The overall late complication rate was 2.4% (8/330). All of the late complications were peristomal site infection or PEG site leakage. In the percutaneous group, 3 late complications (1.9%) were noted, which was peristomal infection in 2 cases (1.3%) and PEG site leakage in 1 case (0.6%). In endoscopic group, 5 late complications (2.8%) were noted, which was peristomal infection in 3 cases (1.7%) and PEG site leakage in 2 cases (1.1%). All cases of peristomal site infection were well treated by antibiotics therapy; and PEG site leakage was also well controlled after new feeding device.
Comparison of complication rate between percutaneous and endoscopic method
The immediate complication rate was significantly lower with the percutaneous group than the endoscopic group (1.3% vs 8.0%, P=0.004) (Table 3). Adjustment for the interval of PEG tube replacement strengthened the association of the immediate complication rate with method, with the percutaneous method being significantly lower than the endoscopic method (odds ratio [OR], 6.57; 95% Confidence Interval [CI], 1.47-29.38, P=0.014). On the other hands, there was no significant difference between percutaneous group and endoscopic group in terms of late complication. (1.9% vs 2.8%, P=0.441 )
Table 3.
Complications of percutaneous group and endoscopic group
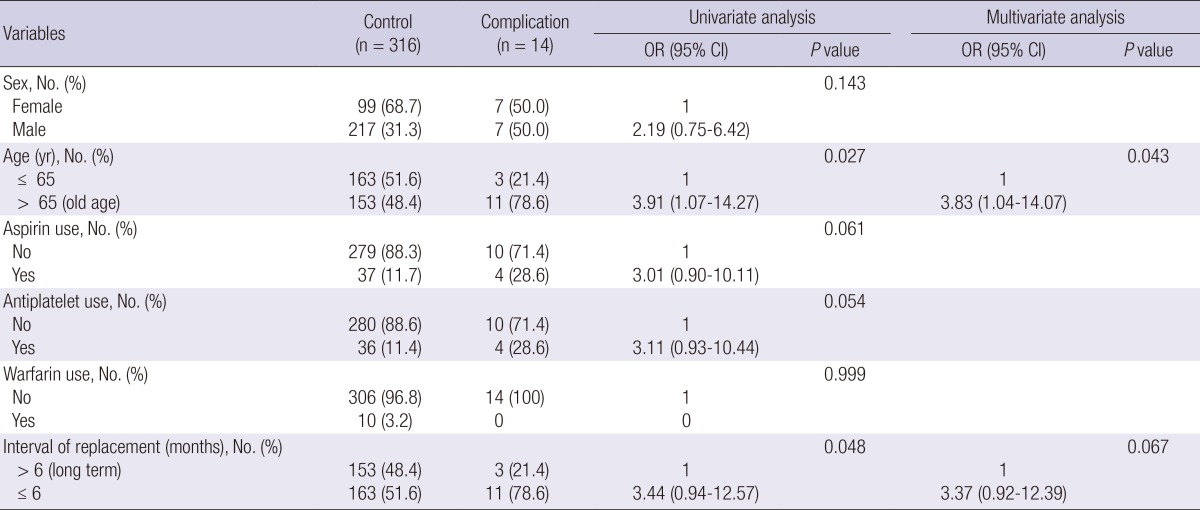
Risk factors of complications during PEG tube replacement
We investigated the risk factors associated with the immediate complications, such as peristomal bleeding and mechanical complications. From the univariate analysis, peristomal bleeding was not associated with all variables, including aspirin use (P=0.113), antiplatelet use (P=0.100), warfarin use (P=0.802), old age (P=0.993), short interval of tube replacement (P=0.193) and male gender (P=0.587).
However, significant increased risk was associated with mechanical complication (esophageal laceration and microperforation) included old age (P=0.027) and short interval of PEG tube replacement (P=0.048). However, other variables, such as aspirin use, antiplatelet use, warfarin use and male gender were not significant associated (Table 4). In multivariate analysis, old age (OR, 3.83; 95% CI, 1.04-14.07, P=0.043) was a significant risk factor of mechanical complication during PEG tube replacement. However, short interval of tube replacement was not statistically significant (Table 4).
Table 4.
Risk factors of mechanical complication during PEG tube replacement
OR, odds ratio; CI, confidence interval.
DISCUSSION
The aim of this study was to compare the complication rate of PEG tube replacement by percutaneous and endoscopic method. In this study, overall immediate complication rate during PEG tube replacement was 4.8%, and late complication rate was 2.4%. Although PEG replacement procedure is relatively safe, it may be complicated by bleeding, mucosal laceration, perforation, fistula disruption, pneumoperitoneum, peritonitis and injury to adjacent organs (10-12). Although most of cases are minor complications which can usually be treated spontaneously, a few cases of major complication may requiring endoscopic or surgical intervention (13).
The immediate complication rate of the percutaneous group was significantly lower than that of the endoscopic group. In the percutaneous group, bleeding from the stomach opening occurred in 2 cases (1.3%). Bleeding is the most serious complication of the percutaneous group, which can be protected by applying proper degree of tension when pulling out a bolster (14). PEG systems of previous generation had a rigid mushroom shaped head which was prone to result in tissue injury when it removed percutaneously (15). However, currently used tubes and bolsters with softness, deformability and malleability are allowed the percutaneous method to be performed more safely.
In endoscopic group, immediate complications occurred in 14 cases (8.0%) and esophageal mucosal laceration, especially the lower esophagus, was most common complication. The lower esophagus encompassing the gastroesophageal junction is the most vulnerable to be damaged from a passing sharp-edged internal bolster (16). A number of patients indicated for placement of PEG have abnormal contracture and spinal deformity that undoubtedly contributes to an abnormal position of the esophagus, which may be responsible for the increased risk of esophageal injury (16-18). Moreover, gastric distension by infused air during an endoscopic procedure evokes retching which increases the risk of esophageal injury (19).
Our study demonstrated that old age was a significant risk factor of esophageal laceration and microperforation. Most of PEG tube placed patients are unable to ambulate, which leads to degeneration and increased stiffness in the joints, leading to contracture and abnormal posture. By aging process, the decrease in muscle fibers in the body, whereas the relative increase in the proportion of connective tissue, may promote contracture of joints and abnormal esophageal anatomy. Because of sharp-edged bump was passed out through esophagus by endoscopic method, anatomical variation might be the most important factor to increase mechanical complications. Recent other studies showed that aspirin and other antiplatelet agent use did not contribute to increase the bleeding during PEG placement (20, 21). Our study also showed that PEG tube replacement related-peristomal bleeding was rare (1.3%, 2/154), even with use of aspirin or antiplatelet agents despite of the methodological differences (PEG replacement vs PEG placement). Generally, PEG tube exchanged regularly every 6 months. Therefore, less than 6 months of PEG tube exchange implicated any problem of previous feeding tube, such as self-removal, malfunction, infection and leakage. We also found out this study short duration of PEG tube replacement (≤6 months) did not significant associated immediate complication.
Planning of preventive strategy could be important considering our results. To reduce the immediate complications in both methods, percutaneous methods should be performed to replace the PEG tube for the old patients to prevent the lower esophagus injury. A recent case report showed that fluoroscopy-guided removal of PEG tubes might be an alternative method in situations where endoscopic attempts fail (22). Moreover, PEG tube should be gently removed with holding around the stoma to prevent from stretching by percutaneous methods. When endoscopic methods were applied to old age patients, a soft-latex protective hood might be protective to esophageal injury (23).
Most of reported studies were focused on the PEG tube placement, but there were few studies about the PEG tube replacement. About percutaneous method, the complication rate of our study (1.3%) is consistent with that previous study (6). One case of stoma tract disruption occurred in total 87 patients (1.2%), resulting in dehiscence of the stoma tract from the abdominal wall (6). A gastrostomy tube was endoscopically placed and the patient's stoma tract healed after 2 weeks without further treatment. On the other hands, there were limited data about endoscopic replacement of PEG tube. There was a case report of distal esophageal perforation by endoscopic method in Korea (24). The patient was successfully treated with primary surgical repair and 2 weeks of antibiotics and food fasting.
The present study has several limitations. It was a retrospective study at single center and removal methods were not randomly assigned. Another limitation is that there was no case of "cut and push method" which is another variant of percutaneous method performed by cutting a tube at skin level and allowing an internal bolster to pass spontaneously via alimentary tract (15). However, the cut and push method might result in intestinal obstruction in patients with underlying gastrointestinal disease. Therefore, disconnected internal PEG flanges were retrieved endoscopically in preference to allow spontaneous passage (25).
In conclusion, overall immediate complication rate during PEG tube replacement was 4.8%, and late complication rate was 2.4%. The immediate complication rate was significantly lower in the percutaneous method. The percutaneous method may be more safe and feasible for replacing PEG tubes in old patients to prevent the mechanical complication such as esophageal injury. Further prospective study would be required to evaluate a tailored method for PEG replacement in high risk patients.
Footnotes
This study was supported by Dongguk University Research Fund of 2013.
The authors have no conflicts of interest to disclose.
References
- 1.Safadi BY, Marks JM, Ponsky JL. Percutaneous endoscopic gastrostomy: an update. Endoscopy. 1998;30:781–789. doi: 10.1055/s-2007-1001422. [DOI] [PubMed] [Google Scholar]
- 2.Mendiratta P, Tilford JM, Prodhan P, Curseen K, Azhar G, Wei JY. Trends in percutaneous endoscopic gastrostomy placement in the elderly from 1993 to 2003. Am J Alzheimers Dis Other Demen. 2012;27:609–613. doi: 10.1177/1533317512460563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roche V. Percutaneous endoscopic gastrostomy: clinical care of PEG tubes in older adults. Geriatrics. 2003;58:22–29. [PubMed] [Google Scholar]
- 4.Turner JK, Berrill JW, Dolwani S, Green JT, Swift G. Percutaneous endoscopic gastrostomy tube replacement. Endoscopy. 2010;42:E146–E147. doi: 10.1055/s-0029-1244102. [DOI] [PubMed] [Google Scholar]
- 5.Schrag SP, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, Martin ND, Hoey BA, Stawicki SP. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes: a comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407–418. [PubMed] [Google Scholar]
- 6.Cass OW, Rowland K, Bartram B, Ross JR, Choe Y, Hall JD. Insertion, efficacy, and removal of a nonendoscopically removable percutaneous endoscopic gastrostomy (PEG) tube. Surg Endosc. 1999;13:516–519. doi: 10.1007/s004649901025. [DOI] [PubMed] [Google Scholar]
- 7.Palmer GM, Frawley GP, Heine RG, Oliver MR. Complications associated with endoscopic removal of percutaneous endoscopic gastrostomy (PEG) tubes in children. J Pediatr Gastroenterol Nutr. 2006;42:443–445. doi: 10.1097/01.mpg.0000189361.61298.9f. [DOI] [PubMed] [Google Scholar]
- 8.Delatore J, Boylan JJ. Bleeding gastric ulcer: a complication from gastrostomy tube replacement. Gastrointest Endosc. 2000;51:482–484. doi: 10.1016/s0016-5107(00)70452-4. [DOI] [PubMed] [Google Scholar]
- 9.Jain NK, Larson DE, Schroeder KW, Burton DD, Cannon KP, Thompson RL, DiMagno EP. Antibiotic prophylaxis for percutaneous endoscopic gastrostomy: a prospective, randomized, double-blind clinical trial. Ann Intern Med. 1987;107:824–828. doi: 10.7326/0003-4819-107-6-824. [DOI] [PubMed] [Google Scholar]
- 10.Nicholson FB, Korman MG, Richardson MA. Percutaneous endoscopic gastrostomy: a review of indications, complications and outcome. J Gastroenterol Hepatol. 2000;15:21–25. doi: 10.1046/j.1440-1746.2000.02004.x. [DOI] [PubMed] [Google Scholar]
- 11.Berger SA, Zarling EJ. Colocutaneous fistula following migration of PEG tube. Gastrointest Endosc. 1991;37:86–88. doi: 10.1016/s0016-5107(91)70634-2. [DOI] [PubMed] [Google Scholar]
- 12.Fox VL, Abel SD, Malas S, Duggan C, Leichtner AM. Complications following percutaneous endoscopic gastrostomy and subsequent catheter replacement in children and young adults. Gastrointest Endosc. 1997;45:64–71. doi: 10.1016/s0016-5107(97)70304-3. [DOI] [PubMed] [Google Scholar]
- 13.Fang JC. Minimizing endoscopic complications in enteral access. Gastrointest Endosc Clin N Am. 2007;17:179–196. doi: 10.1016/j.giec.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Yaseen M, Steele MI, Grunow JE. Nonendoscopic removal of percutaneous endoscopic gastrostomy tubes: morbidity and mortality in children. Gastrointest Endosc. 1996;44:235–238. doi: 10.1016/s0016-5107(96)70157-8. [DOI] [PubMed] [Google Scholar]
- 15.Pearce CB, Goggin PM, Collett J, Smith L, Duncan HD. The 'cut and push' method of percutaneous endoscopic gastrostomy tube removal. Clin Nutr. 2000;19:133–135. doi: 10.1054/clnu.2000.0100. [DOI] [PubMed] [Google Scholar]
- 16.Bertoni G, Pacchione D, Conigliaro R, Sassatelli R, Pedrazzoli C, Bedogni G. Endoscopic protector hood for safe removal of sharp-pointed gastroesophageal foreign bodies. Surg Endosc. 1992;6:255–258. doi: 10.1007/BF02498816. [DOI] [PubMed] [Google Scholar]
- 17.Papakonstantinou K, Karagiannis A, Tsirantonaki M, Konstantinidis A, Spirou S, Skottis I, Karabinis A. Mediastinitis complicating a percutaneous endoscopic gastrostomy: a case report. BMC Gastroenterol. 2003;3:11. doi: 10.1186/1471-230X-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kilic D, Findikcioglu A, Ates U, Hekimoglu K, Hatipoglu A. Management of descending mediastinal infections with an unusual cause: a report of 3 cases. Ann Thorac Cardiovasc Surg. 2010;16:198–202. [PubMed] [Google Scholar]
- 19.Cappell MS. Esophageal bleeding after percutaneous endoscopic gastrostomy. J Clin Gastroenterol. 1988;10:383–385. doi: 10.1097/00004836-198808000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Richter JA, Patrie JT, Richter RP, Henry ZH, Pop GH, Regan KA, Peura DA, Sawyer RG, Northup PG, Wang AY. Bleeding after percutaneous endoscopic gastrostomy is linked to serotonin reuptake inhibitors, not aspirin or clopidogrel. Gastrointest Endosc. 2011;74:22–34. doi: 10.1016/j.gie.2011.03.1258. [DOI] [PubMed] [Google Scholar]
- 21.Singh D, Laya AS, Vaidya OU, Ahmed SA, Bonham AJ, Clarkston WK. Risk of bleeding after percutaneous endoscopic gastrostomy (PEG) Dig Dis Sci. 2012;57:973–980. doi: 10.1007/s10620-011-1965-7. [DOI] [PubMed] [Google Scholar]
- 22.Ahlers CM, Schneider J, Lachmann R, Herber S, Düber C, Pitton MB. Fluoroscopy-guided removal of pull-type gastrostomy tubes. Cardiovasc Intervent Radiol. 2008;31:1252–1254. doi: 10.1007/s00270-008-9335-3. [DOI] [PubMed] [Google Scholar]
- 23.Bertoni G, Sassatelli R, Conigliaro R, Bedogni G. A simple latex protector hood for safe endoscopic removal of sharp-pointed gastroesophageal foreign bodies. Gastrointest Endosc. 1996;44:458–461. doi: 10.1016/s0016-5107(96)70099-8. [DOI] [PubMed] [Google Scholar]
- 24.Heo SW, Kwon JG, Park KC, Ryu JI, Ju DU, Ha KH, Jung JT, Kim HG. Esophageal perforation after change of a percutaneous endoscopic gastrostomy tube. Korean J Gastrointest Endosc. 2011;43:1–4. [Google Scholar]
- 25.Khan S, Gatt M, Petty D, Stojkovic S. Intestinal obstruction after PEG tube replacement: implications to daily clinical practice. Surg Laparosc Endosc Percutan Tech. 2008;18:80–81. doi: 10.1097/SLE.0b013e31815842d6. [DOI] [PubMed] [Google Scholar]