Abstract
AIM: To examine whether visceral adipose tissue (VAT) serves as a risk factor for colorectal adenoma-early colorectal cancer (CRC) sequence.
METHODS: A retrospective case-control study was conducted with 153 patients with stage I CRC, age/sex-matched 554 patients with colorectal adenoma and 557 normal controls. All subjects underwent various laboratory tests, abdominal fat computed tomography (CT), and colonoscopy. VAT was defined as an intra-abdominal adipose tissue area measured by CT scan. Adipose tissue area was measured at the level of the umbilicus from CT scan. We used the lowest quartile of VAT and subcutaneous adipose tissue area as a reference group.
RESULTS: The body mass index (BMI), total cholesterol, fasting glucose and VAT areas were significantly different among normal, adenoma and CRC groups. The VAT area was 120.6 ± 49.0 cm2 in normal controls, 130.6 ± 58.4 cm2 in adenoma group and 117.6 ± 51.6 cm2 in CRC group (P = 0.002). In univariate analysis, increased BMI was a risk factor for CRC compared to control (P = 0.025). However, VAT area was not a risk factor for CRC compared to control. In multivariate analysis that adjusted for smoking, alcohol consumption and subcutaneous adipose tissue area, VAT area was inversely related to CRC, compared to the adenoma (OR = 0.53, 95%CI: 0.31-0.92, highest quartile vs lowest quartile).
CONCLUSION: Our study shows that visceral obesity is not a risk factor for early CRC. Visceral obesity might influence the normal-adenoma sequence but not the adenoma-early carcinoma sequence.
Keywords: Adipose tissue, Visceral fat, Obesity, Colorectal cancer, Colorectal adenoma, Abdominal computed tomography
Core tip: This study showed that visceral obesity is not a risk factor for early colorectal cancer, although it is an independent risk factor for colorectal adenoma in previous studies. Therefore, these data suggest that visceral obesity might influence the normal-adenoma sequence but not the adenoma-early carcinoma sequence.
INTRODUCTION
The prevalence of obesity has increased over the past few decades[1], and the prevalence of colorectal neoplasia has also increased in Asian countries, particularly in South Korea[2]. There is mounting evidence linking obesity to colorectal neoplasia[3]. Data from recent studies, including our previous research, have suggested that among the diverse methods that are used to define obesity, the visceral adipose tissue (VAT) area is a strong indicator of obesity as a risk factor for developing colorectal adenoma[4-7]. The natural course of adenoma is well known as the “adenoma-carcinoma sequence”[8]. Therefore, the role of VAT in developing colorectal cancer (CRC) should be interpreted at each step of this sequence. Several studies have assessed the association between the VAT area and CRC. For example, in a Japanese study[9], VAT was positively associated with developing early stage CRC but not adenoma. However, in this study, the number of CRC patients was small, and the control subjects were selected from the subjects with negative screening results but without colonoscopic exams, which may have resulted in including patients with colorectal adenomas. In a Turkish study[10], the VAT area did not differ between the CRC patients and controls. This study involved also a small number of cases, and the controls were consecutively collected, which means that they were not matched by age or gender.
The relationship between VAT and the colorectal adenoma-cancer sequence has not yet been completely documented. The aim of this study was to examine whether VAT serves as a risk factor for the colorectal adenoma-early CRC sequence.
MATERIALS AND METHODS
Study population
A retrospective case-controlled study was conducted to compare stage I, early CRC patients with an age- and sex-matched colorectal adenoma group and normal controls. From October 2004 to December 2008, 1206 CRC patients underwent colectomy at Seoul National University Hospital by an identical main operator. For preoperative evaluation, all patients had colonoscopic examination and abdominal computed tomography (CT) scan. To minimize the wasting effect of cancer itself, we included only the stage I CRC patients in our study. The cancer stage was determined using the American Joint Committee on Cancer criteria[11]. Stage I CRC includes the T1N0 and T2N0 on tumor node metastasis stages. There were 153 eligible patients after the following exclusion criteria were applied: preoperative neoadjuvant chemoradiation therapy, a history of colonic disease such as CRC, inflammatory bowel disease and a family history of CRC. The colon adenoma patients and normal controls were recruited at Seoul National University Hospital Healthcare System Gangnam Center during a routine health check-up over a similar time period. The inclusion criteria were those who underwent abdominal fat CT scan and colonoscopy on the same day. Patients with colorectal adenoma and normal controls (subjects with normal colonoscopic findings) followed the study design as previously described[4]. The following exclusion criteria were applied to the colorectal adenoma and normal control groups: a history of colonic disease, such as colorectal adenomatous polyps, cancer, inflammatory bowel disease, and bowel resection; a colonic examination including sigmoidoscopy, colonoscopy, or barium enema in the previous 10 years, a family history of CRC.
To adjust for age and sex, which are considered important confounders in CRC and adenoma studies, we formed three age- and sex-matched groups: the early CRC group, the adenoma group and the control group.
Ethics statement
The Institutional Review Board of Seoul National University Hospital approved the study protocol (IRB number H-1208-001-420), and the study was conducted in accord with the Helsinki Declaration. Informed consent was waived by the board.
Clinical and laboratory evaluations
All subjects were questioned regarding smoking, alcohol consumption, diabetes mellitus, hypertension, and medication histories. Height, weight and blood pressure were measured by trained nurses using a standardized protocol. Venous samples were drawn after an overnight 12-h fast to check serum total cholesterol and fasting glucose. All biochemical tests were performed using an automatic analyzer within the Department of Laboratory Medicine at Seoul National University Hospital.
Definitions and exposure measurements
Current smoking was defined as smoking at least one cigarette per day for the previous 12 mo, and alcohol consumption was defined as drinking over 140 g of alcohol per week. Hypertension was defined as a blood pressure of > 140/90 mmHg or taking an anti-hypertensive medication. Diabetes mellitus was defined as a fasting glucose of > 126 mg/dL or taking a diabetes mellitus medication. Body mass index (BMI) was calculated from the measured weight and height.
Measurement of adipose tissue areas by CT
All of the CRC patients had preoperative abdominal CT for staging work-up. The adipose tissue area was measure at the level of the umbilicus using a 16-detector row CT scanner (Somatom Sensation 16, Siemens medical Solutions, Forchheim, Germany), as previously described[12]. We defined VAT as an intra-abdominal adipose tissue area confined by the parietal peritoneum, excluding the paraspinal muscles and the vertebral column. Subcutaneous adipose tissue (SAT) areas were defined as adipose tissue areas external to the abdomen and the back muscles[4]. As there are no standard values for the definition of a normal amount of abdominal adipose tissue, we used the lowest quartile of SAT and VAT area in this study as a reference group. Same method was applied to the normal and adenoma groups from their abdominal fat CT. To minimize interpersonal variation, all measurements were performed by one experienced nurse who was blinded to the clinical and laboratory details of subject.
Colonoscopy and the detection of colorectal adenoma
The colonoscopies were performed by experienced gastroenterologists. The colonoscopists were blinded to the clinical findings and adipose tissue amounts. The bowel preparations were performed using four liters of colonlyte solution. Histopathologically, colorectal carcinoma was defined as colorectal adenocarcinoma, regardless of amount of the mucinous component or differentiation. Colorectal adenoma was defined as a colorectal adenoma, regardless of the grading and the amount of villous component.
Statistical analysis
The continuous variables are expressed as the mean ± SD. The χ2 test or Student’s t test and an analysis of variance (ANOVA) for independent samples were used to assess the differences in risk factors among the groups. The effect of obesity, as measured by SAT or VAT area, were estimated by calculating an OR and a 95%CI using conditional logistic regression analysis. In addition to the risk factors that were determined to be significant in a univariate analysis, we included additional variables that are known or reportedly have an association with CRC, such as smoking and alcohol consumption, for the multiple conditional logistic regression model to identify independent risk factors for CRC. All of the statistical analyses were performed using SPSS 19.0 (SPSS, Chicago, IL, United States) and SAS 9.2 (SAS institute, Cary, NC, United States). P < 0.05 was considered statistically significant.
RESULTS
Characteristics of participants
Of 1206 colorectal patients who had colectomies, 153 stage I patients met the inclusion criteria and were enrolled in the final analysis. The patients were matched by age and sex to produce 554 adenoma group members and 557 normal controls. The mean age of all 1264 subjects was 59.2 ± 8.5 years, and the male to female ratio was 842:422. The BMI, total cholesterol and fasting glucose levels, total adipose tissue, VAT and SAT areas were significantly different among the three groups. The VAT area was 120.6 ± 49.0 cm2 in normal controls, 130.6 ± 58.4 cm2 in the adenoma group, and 117.6 ± 51.6 cm2 in the early CRC group (P = 0.002). There were no differences in age, gender, smoking history, alcohol consumption, hypertension or diabetes (Table 1). The VAT areas in colorectal carcinoma patients were significantly lower than in the adenoma patients (P = 0.02), but not significantly lower than in the control group (P = 0.51). The VAT areas in colorectal adenoma patients were significantly higher than in the control group (P = 0.005) (Figure 1).
Table 1.
Comparison of the baseline characteristics of the colorectal cancer, adenoma, and control groups n (%)
| Characteristics | Control (n = 557) | Adenoma (n = 554) | Cancer (n = 153) | P value |
| Age (yr) | 59.1 ± 8.7 | 59.1 ± 8.2 | 60.3 ± 9.1 | 0.278 |
| Male | 370 (66.4) | 372 (67.1) | 100 (65.4) | 0.910 |
| Alcohol consumption | 77 (13.8) | 86 (15.5) | 31 (20.3) | 0.146 |
| Current smoking | 86 (15.4) | 106 (19.1) | 28 (18.3) | 0.255 |
| Hypertension | 195 (35.0) | 217 (39.2) | 63 (41.2) | 0.222 |
| Diabetes | 70 (12.6) | 70 (12.6) | 19 (12.4) | 0.997 |
| Body mass index (kg/m2) | 23.80 ± 2.48 | 24.34 ± 2.56 | 24.25 ± 2.51 | 0.001 |
| ≤ 22.9 | 194 (34.8) | 150 (27.1) | 46 (30.1) | 0.011 |
| 23.0-24.9 | 197 (35.4) | 188 (33.9) | 51 (33.3) | |
| 25.0-29.9 | 161 (28.9) | 202 (36.5) | 55 (35.9) | |
| ≥ 30.0 | 5 (0.9) | 14 (2.5) | 1 (0.7) | |
| Total cholesterol (mg/dL) | 197.7 ± 35.5 | 193.1 ± 35.4 | 179.9 ± 45.5 | < 0.001 |
| Fasting glucose (mg/dL) | 100.7 ± 21.2 | 100.7 ± 20.0 | 107.3 ± 26.4 | 0.002 |
| Total adipose tissue area (cm2) | 262.4 ± 81.3 | 281.3 ± 90.1 | 264.1 ± 86.0 | 0.001 |
| Visceral adipose tissue area (cm2) | 120.6 ± 49.0 | 130.6 ± 58.4 | 117.6 ± 51.6 | 0.002 |
| Subcutaneous adipose tissue area (cm2) | 141.9 ± 55.0 | 150.7 ± 59.8 | 146.5 ± 56.6 | 0.040 |
Results are expressed as mean ± SD.
Figure 1.
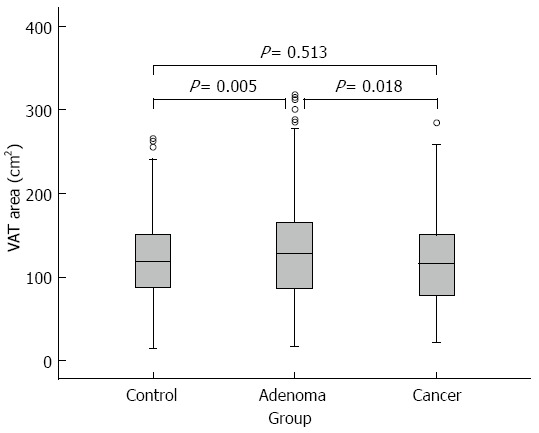
Comparison of visceral adipose tissue area (cm2) among patients with colorectal carcinoma, those with colorectal adenoma, and controls. Visceral adipose tissue (VAT) area in colorectal carcinoma patients was significantly lower than in adenoma patients (P = 0.018), but it was not significantly lower than in control group (P = 0.513).
Adiposity in stage I CRC vs normal group
In a prior paper from our research group, the VAT area was an independent risk factor for colorectal adenoma compared to normal controls[4]. In this study, according to a univariate analysis, the VAT and SAT area were not risk factors for early CRC. However, BMI was found to be significantly associated with the presence of CRC (P = 0.021). Conditional logistic regression models adjusting for smoking and alcohol consumption showed that CRC was not associated with VAT area. Including the SAT area in the multivariate analysis provided the same result. Increased BMI, as a surrogate marker for general obesity, was an independent risk factor for CRC (P for trend = 0.025) (Table 2).
Table 2.
Body measure index, adipose tissue area and the risk of colorectal cancer vs control
|
Univariate |
Multivariate 11 |
Multivariate 22 |
||||
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | |
| BMI | ||||||
| Quartile I | 1 | 0.0213 | 1 | 0.0253 | ||
| Quartile II | 0.82 (0.49-1.40) | 0.471 | 0.81 (0.48-1.38) | 0.446 | ||
| Quartile III | 1.33 (0.81-2.20) | 0.262 | 1.32 (0.80-2.19) | 0.279 | ||
| Quartile IV | 1.61 (0.97-2.66) | 0.066 | 1.58 (0.95-2.63) | 0.077 | ||
| VAT | ||||||
| Quartile I | 1 | 0.4783 | 1 | 0.5013 | 1 | 0.3783 |
| Quartile II | 0.80 (0.49-1.31) | 0.376 | 0.79 (0.48-1.29) | 0.341 | 0.73 (0.43-1.23) | 0.235 |
| Quartile III | 0.65 (0.40-1.07) | 0.089 | 0.65 (0.40-1.07) | 0.089 | 0.59 (0.35-1.02) | 0.057 |
| Quartile IV | 0.92 (0.56-1.53) | 0.758 | 0.93 (0.56-1.54) | 0.776 | 0.82 (0.47-1.46) | 0.507 |
| SAT | ||||||
| Quartile I | 1 | 0.7163 | 1 | 0.7703 | 1 | 0.5223 |
| Quartile II | 1.10 (0.67-1.82) | 0.708 | 1.10 (0.66-1.82) | 0.726 | 1.25 (0.73-2.13) | 0.426 |
| Quartile III | 1.10 (0.62-1.68) | 0.940 | 1.00 (0.60-1.66) | 0.993 | 1.15 (0.66-1.99) | 0.623 |
| Quartile IV | 1.14 (0.68-1.89) | 0.625 | 1.12 (0.67-1.87) | 0.664 | 1.31 (0.73-2.34) | 0.362 |
Multivariate model 1 was adjusted for current smoking status, and alcohol consumption;
Multivariate model 2 was adjusted for subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT), in addition. Since body mass index (BMI) showed co-linearity to adipose tissue amount, it was not included in the analysis;
P value for test of trend of odds.
Adiposity in stage I CRC vs adenoma group
In the univariate analysis, VAT area, SAT area and BMI were not risk factors for early CRC compared to colorectal adenoma. The conditional logistic regression models (adjusted for smoking and alcohol consumption) showed that overall obesity, which is indicated by BMI, was not different between the adenoma and CRC groups. Contrary to expectations, an inverse relationship of the VAT area to early CRC was observed, compared with colorectal adenoma (OR = 0.53, 95%CI: 0.31-0.92, P = 0.02, highest quartile vs lowest quartile of the VAT area) (Table 3).
Table 3.
Body measure index, adipose tissue area and the risk of colorectal cancer vs colorectal adenoma
|
Univariate |
Multivariate 11 |
Multivariate 22 |
||||
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | |
| BMI | ||||||
| Quartile I | 1 | 0.9373 | 1 | 0.8873 | ||
| Quartile II | 0.87 (0.51-1.48) | 0.600 | 0.86 (0.50-1.48) | 0.595 | ||
| Quartile III | 0.96 (0.58-1.58) | 0.875 | 0.96 (0.58-1.58) | 0.857 | ||
| Quartile IV | 0.95 (0.58-1.55) | 0.824 | 0.93 (0.57-1.53) | 0.777 | ||
| VAT | ||||||
| Quartile I | 1 | 0.0323 | 1 | 0.0243 | 1 | 0.0283 |
| Quartile II | 0.74 (0.45-1.21) | 0.227 | 0.74 (0.45-1.20) | 0.224 | 0.70 (0.42-1.18) | 0.182 |
| Quartile III | 0.71 (0.43-1.17) | 0.182 | 0.68 (0.41-1.13) | 0.141 | 0.65 (0.38-1.12) | 0.118 |
| Quartile IV | 0.57 (0.35-0.94) | 0.028 | 0.56 (0.34-0.92) | 0.023 | 0.53 (0.31-0.92) | 0.024 |
| SAT | ||||||
| Quartile I | 1 | 0.5503 | 1 | 0.5563 | 1 | 0.7293 |
| Quartile II | 0.90 (0.55-1.49) | 0.686 | 0.91 (0.55-1.50) | 0.697 | 1.08 (0.63-1.83) | 0.786 |
| Quartile III | 1.03 (0.62-1.71) | 0.898 | 1.02 (0.62-1.70) | 0.933 | 1.26 (0.73-2.17) | 0.407 |
| Quartile IV | 0.82 (0.49-1.35) | 0.427 | 0.82 (0.50-1.36) | 0.443 | 1.09 (0.62-1.91) | 0.362 |
Multivariate model 1 was adjusted for current smoking status, and alcohol consumption;
Multivariate model 2 was adjusted for subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT), in addition. Since body mass index (BMI) showed co-linearity to adipose tissue amount, it was not included in the analysis;
P value for test of trend of odds.
DISCUSSION
In this study of 153 stage I CRC patients, age- and sex-matched 554 colorectal adenoma patients and 557 normal controls, we found that visceral obesity was not a risk factor for early CRC. Overall obesity (measured by BMI) was a significant risk factor for CRC compared with normal controls. This was consistent with previous findings[13].
Recently, the prevalence of obesity has increased rapidly and is becoming a major public health problem. At present, more than 300 million people worldwide are obese[14]. There is mounting evidence relating obesity to colorectal neoplasia. However, the relationship between obesity and colorectal neoplasia differs depending on the methodology used to measure obesity. Whole body fat area is distributed into two main compartments with different metabolic characteristics: SAT and VAT[15]. BMI and body weight reflects the whole body fat amount. Waist circumference (WC) and waist to hip ratio (WHR) implies the visceral fat area. Visceral obesity is also referred to as abdominal or central obesity. In several reports, BMI and body weight were not consistently related to the development of colorectal neoplasia, an association which is strongly influenced by gender[6,10,16-18]. WC and WHR have shown a stronger positive relationship[18-21]; however, several studies of WC and WHR suggested a greater risk for CRC in men than women, thus providing inconclusive results regarding their relationship[22,23]. The visceral fat area can be assessed most objectively by CT scanning at the umbilical level[12]. Therefore, our study assessed the relationship of visceral obesity with colorectal adenoma and cancer based on CT analysis instead of WC and WHR. The technique we used for visceral adipose tissue area measurements in CT scan has been standardized and validated in previous studies[24-28]. Note that many studies have related visceral obesity to colorectal adenoma[7,17,19,29,30]. Our institute reported a similar result[4]. Results assessing the relationship between abdominal obesity and colorectal neoplasia are inconclusive. Studies have proven positive[9], negative[10] or no association[31]. In the paper showing a positive relationship, the number of case subjects with CRC was small, and the authors did not confirm with colonoscopy that the control groups were polyp-free[31]. In the study showing an inverse relationship, the number of cases was small, and the authors included overall CRC stages, which resulted in the weight loss over the course of cancer development influencing the result. Studies that evaluate the effect of abdominal obesity in a large number CRC cases and define the control and adenoma groups clearly by colonoscopic examination are sparse. Colorectal neoplasia follows the “adenoma-carcinoma sequence”[8], which is characterized by the progression from precancerous adenoma to carcinoma. Because adenomatous polyps are common and only a small portion progress to cancer[32], the association of visceral obesity with colorectal neoplasia should be explored at each step. However, studies assessing their association with cancer (separately) are sparse. In our study, we assessed the effect of visceral obesity on the “normal to cancer” and “adenoma to cancer” progression. Contrary to the effect of visceral obesity on the “normal to colorectal adenoma sequence”, visceral obesity was not a risk factor for developing CRC. Every step of the “adenoma-carcinoma sequence” is affected by multiple factors[33-37], such as genetic instability, cell cycle, apoptosis and other environmental factors, including inflammatory cells and dietary carcinogens. Therefore, the association between visceral fat and these multiple factors may be step-specific over the progression of this sequence. The role of visceral fat in the progression of the “adenoma-carcinoma sequence” is complex and has not been thoroughly explored. From the previous research and our paper, it appears that visceral obesity is a risk factor for colorectal adenoma formation but does not have an additional effect on its further progress to colorectal carcinoma.
Contrary to Western population, carcinogenesis is different in the Asian population, which develops CRC more often directly in normal colonic mucosa without adenoma stage. Our results might be compatible to this de novo pathway hypothesis. Further studies were needed to prove this hypothesis[38].
Diabetes, one of the factors comprising metabolic syndrome, is also considered a risk factor for CRC. Some studies have shown positive[39-41] association between diabetes and CRC while others have shown inconclusive[39,41,42]. There are reports that the association is affected by ethnicity, gender and the duration of treatment[43,44]. In our study, diabetes showed no relationship with CRC. Recent study demonstrated that colon cancer risk is increased in diabetic men before diabetes onset[45]. Diabetes did not alter colon cancer risk in men or women after clinical diabetes onset[45]. Because we only included patients with early CRC, we thought abnormal glucose metabolism, including impaired fasting glucose and diabetes all together, was a risk factor for early CRC. Multivariable analysis showed impaired fasting glucose/diabetes is an independent risk factor of early colon cancer (data was not shown). Future studies with objective measurement of diabetes (insulin level, C-peptide) and incorporating ethnicity, gender and medication difference might help elucidate the risk of CRC in diabetes.
Our study has some superiority over previous studies. Although several studies have assessed the effect of visceral obesity on colorectal neoplasia using CT scanning, few studies that analyzed its respective effect on the normal to adenoma and the adenoma to carcinoma sequences[7,9,10,19,31,46]. In our study, we included only the stage I CRC patients to minimize the wasting characteristics of the cancer itself. Because we perform more than 500 cases CRC surgery in a year, the total number of early CRC cases that were included was sufficiently larger. In our study, we benefited from utilizing a control group that was selected by performing a complete; therefore, definite comparisons among the control, adenoma and CRC groups were feasible.
Several limitations of the study also warrant mentioning. First, because this study had a cross-sectional design, we could not evaluate the effect of the duration of visceral obesity and could not consider recent weight changes. Second, we did not adjust healthcare, socioeconomic status, dietary factors or physical activity factors, which affect the visceral fat amount and the CRC development. Third, as the control and adenoma groups were selected from the health screening population, there might be a socioeconomic difference in the CRC groups. However, several variables such as diabetes, hypertension, smoking, and alcohol consumption were not different from three groups. Fourth, information of previous adenoma before surgery was not available, which might affect the development of CRC. Fifth, since we did not analyze the genetic data in each group, de novo pathway, which is comprise some portion for CRC development[47], was not taken into consideration to explain CRC development. Sixth, volumetric measure of VAT was more accurate than visceral adipose tissue area measurement[48,49]. However, the technique we used for VAT area measurements has been standardized and validated in previous studies[24-28]. Finally, since our study was designed retrospectively, we could not take into consideration in the relationship of metabolic syndromes for analysis because data such as triglyceride, high-density lipoprotein-cholesterol and insulin level, were not available. In addition, we did not have data such as WC or WHR in patients with CRC due to our retrospective study design.
In conclusion, although visceral obesity is an independent risk factor for colorectal adenoma in previous studies, it is not a risk factor for early CRC. Visceral obesity might not influence the adenoma-early carcinoma sequence, but it does influence the normal-adenoma sequence. In addition, role of visceral obesity which might be explained de novo pathway for CRC development in Asian population need to be studied in future.
COMMENTS
Background
Recently, several studies have addressed the association between colorectal adenoma and visceral adipose tissue (VAT) area as measured by abdominal computed tomography (CT). In addition, it has been well documented that most colorectal cancers (CRC) stem from colorectal adenoma in a process referred to as the adenoma-carcinoma sequence. However, the relationship between VAT and early CRC has not been thoroughly documented.
Research frontiers
Although several studies have assessed the effect of visceral obesity on colorectal neoplasia using CT scanning, few studies that analyzed its respective effect on the normal to adenoma and the adenoma to carcinoma sequences. The authors investigated the role of VAT in developing CRC at each step of this sequence
Innovations and breakthroughs
This study showed that visceral obesity is not a risk factor for early CRC, although it is an independent risk factor for colorectal adenoma in previous studies. Therefore, these data suggest that visceral obesity might influence the normal-adenoma sequence but not the adenoma-early carcinoma sequence. All of these observations are original and provide new information between visceral obesity and colorectal neoplasia above and beyond CT-measured visceral adiposity.
Applications
The role of visceral fat in the progression of the “adenoma-carcinoma sequence” is complex and has not been thoroughly explored. From the previous research and our paper, it appears that visceral obesity is a risk factor for colorectal adenoma formation but does not have an additional effect on its further progress to colorectal carcinoma. These findings will be valuable data to understand the role of adipose tissue in the progression of “adenoma-carcinoma sequence”.
Terminology
VAT is defined as an intra-abdominal adipose tissue area confined by the parietal peritoneum, excluding the paraspinal muscles and the vertebral column. Subcutaneous adipose tissue areas were defined as adipose tissue areas external to the abdomen and the back muscles.
Peer review
Although there are some limitations due to its retrospective study design, this article is a nice and well written case controlled study showing the role of adipose tissue in the progression of colorectal adenoma-carcinoma sequence.
Footnotes
Supported by Grant from the Seoul National University Hospital Research Fund, No. 0420100610 (2010-1086)
P- Reviewers: Chang ST, Nash GF, Tarantino G S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Korea Centers for Disease Control. Korea health statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3) Seoul: Ministry of Health and Welfare;; 2010. p. (Korean). [Google Scholar]
- 2.Choe JW, Chang HS, Yang SK, Myung SJ, Byeon JS, Lee D, Song HK, Lee HJ, Chung EJ, Kim SY, et al. Screening colonoscopy in asymptomatic average-risk Koreans: analysis in relation to age and sex. J Gastroenterol Hepatol. 2007;22:1003–1008. doi: 10.1111/j.1440-1746.2006.04774.x. [DOI] [PubMed] [Google Scholar]
- 3.Dai Z, Xu YC, Niu L. Obesity and colorectal cancer risk: a meta-analysis of cohort studies. World J Gastroenterol. 2007;13:4199–4206. doi: 10.3748/wjg.v13.i31.4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang HW, Kim D, Kim HJ, Kim CH, Kim YS, Park MJ, Kim JS, Cho SH, Sung MW, Jung HC, et al. Visceral obesity and insulin resistance as risk factors for colorectal adenoma: a cross-sectional, case-control study. Am J Gastroenterol. 2010;105:178–187. doi: 10.1038/ajg.2009.541. [DOI] [PubMed] [Google Scholar]
- 5.MacInnis RJ, English DR, Hopper JL, Gertig DM, Haydon AM, Giles GG. Body size and composition and colon cancer risk in women. Int J Cancer. 2006;118:1496–1500. doi: 10.1002/ijc.21508. [DOI] [PubMed] [Google Scholar]
- 6.Pischon T, Lahmann PH, Boeing H, Friedenreich C, Norat T, Tjønneland A, Halkjaer J, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC, et al. Body size and risk of colon and rectal cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC) J Natl Cancer Inst. 2006;98:920–931. doi: 10.1093/jnci/djj246. [DOI] [PubMed] [Google Scholar]
- 7.Oh TH, Byeon JS, Myung SJ, Yang SK, Choi KS, Chung JW, Kim B, Lee D, Byun JH, Jang SJ, et al. Visceral obesity as a risk factor for colorectal neoplasm. J Gastroenterol Hepatol. 2008;23:411–417. doi: 10.1111/j.1440-1746.2007.05125.x. [DOI] [PubMed] [Google Scholar]
- 8.Hill MJ, Morson BC, Bussey HJ. Aetiology of adenoma--carcinoma sequence in large bowel. Lancet. 1978;1:245–247. doi: 10.1016/s0140-6736(78)90487-7. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto S, Nakagawa T, Matsushita Y, Kusano S, Hayashi T, Irokawa M, Aoki T, Korogi Y, Mizoue T. Visceral fat area and markers of insulin resistance in relation to colorectal neoplasia. Diabetes Care. 2010;33:184–189. doi: 10.2337/dc09-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erarslan E, Turkay C, Koktener A, Koca C, Uz B, Bavbek N. Association of visceral fat accumulation and adiponectin levels with colorectal neoplasia. Dig Dis Sci. 2009;54:862–868. doi: 10.1007/s10620-008-0440-6. [DOI] [PubMed] [Google Scholar]
- 11.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene F, Trotti A. AJCC Cancer Staging Manual. 6th ed. New York: Springer; 2010. [Google Scholar]
- 12.Chung SJ, Kim D, Park MJ, Kim YS, Kim JS, Jung HC, Song IS. Metabolic syndrome and visceral obesity as risk factors for reflux oesophagitis: a cross-sectional case-control study of 7078 Koreans undergoing health check-ups. Gut. 2008;57:1360–1365. doi: 10.1136/gut.2007.147090. [DOI] [PubMed] [Google Scholar]
- 13.Moghaddam AA, Woodward M, Huxley R. Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomarkers Prev. 2007;16:2533–2547. doi: 10.1158/1055-9965.EPI-07-0708. [DOI] [PubMed] [Google Scholar]
- 14.Giovannucci E. Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr. 2001;131:3109S–3120S. doi: 10.1093/jn/131.11.3109S. [DOI] [PubMed] [Google Scholar]
- 15.Shuster A, Patlas M, Pinthus JH, Mourtzakis M. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85:1–10. doi: 10.1259/bjr/38447238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacInnis RJ, English DR, Haydon AM, Hopper JL, Gertig DM, Giles GG. Body size and composition and risk of rectal cancer (Australia) Cancer Causes Control. 2006;17:1291–1297. doi: 10.1007/s10552-006-0074-y. [DOI] [PubMed] [Google Scholar]
- 17.Gunter MJ, Leitzmann MF. Obesity and colorectal cancer: epidemiology, mechanisms and candidate genes. J Nutr Biochem. 2006;17:145–156. doi: 10.1016/j.jnutbio.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 18.Larsson SC, Wolk A. Obesity and colon and rectal cancer risk: a meta-analysis of prospective studies. Am J Clin Nutr. 2007;86:556–565. doi: 10.1093/ajcn/86.3.556. [DOI] [PubMed] [Google Scholar]
- 19.Otake S, Takeda H, Suzuki Y, Fukui T, Watanabe S, Ishihama K, Saito T, Togashi H, Nakamura T, Matsuzawa Y, et al. Association of visceral fat accumulation and plasma adiponectin with colorectal adenoma: evidence for participation of insulin resistance. Clin Cancer Res. 2005;11:3642–3646. doi: 10.1158/1078-0432.CCR-04-1868. [DOI] [PubMed] [Google Scholar]
- 20.Kim JH, Lim YJ, Kim YH, Sung IK, Shim SG, Oh SO, Park SS, Yang S, Son HJ, Rhee PL, et al. Is metabolic syndrome a risk factor for colorectal adenoma? Cancer Epidemiol Biomarkers Prev. 2007;16:1543–1546. doi: 10.1158/1055-9965.EPI-07-0199. [DOI] [PubMed] [Google Scholar]
- 21.Moore LL, Bradlee ML, Singer MR, Splansky GL, Proctor MH, Ellison RC, Kreger BE. BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham Study adults. Int J Obes Relat Metab Disord. 2004;28:559–567. doi: 10.1038/sj.ijo.0802606. [DOI] [PubMed] [Google Scholar]
- 22.Frezza EE, Wachtel MS, Chiriva-Internati M. Influence of obesity on the risk of developing colon cancer. Gut. 2006;55:285–291. doi: 10.1136/gut.2005.073163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed RL, Schmitz KH, Anderson KE, Rosamond WD, Folsom AR. The metabolic syndrome and risk of incident colorectal cancer. Cancer. 2006;107:28–36. doi: 10.1002/cncr.21950. [DOI] [PubMed] [Google Scholar]
- 24.Thaete FL, Colberg SR, Burke T, Kelley DE. Reproducibility of computed tomography measurement of visceral adipose tissue area. Int J Obes Relat Metab Disord. 1995;19:464–467. [PubMed] [Google Scholar]
- 25.Kvist H, Chowdhury B, Grangård U, Tylén U, Sjöström L. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48:1351–1361. doi: 10.1093/ajcn/48.6.1351. [DOI] [PubMed] [Google Scholar]
- 26.Goodpaster BH. Measuring body fat distribution and content in humans. Curr Opin Clin Nutr Metab Care. 2002;5:481–487. doi: 10.1097/00075197-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Baumgartner RN, Heymsfield SB, Roche AF, Bernardino M. Abdominal composition quantified by computed tomography. Am J Clin Nutr. 1988;48:936–945. doi: 10.1093/ajcn/48.4.936. [DOI] [PubMed] [Google Scholar]
- 28.Borkan GA, Gerzof SG, Robbins AH, Hults DE, Silbert CK, Silbert JE. Assessment of abdominal fat content by computed tomography. Am J Clin Nutr. 1982;36:172–177. doi: 10.1093/ajcn/36.1.172. [DOI] [PubMed] [Google Scholar]
- 29.Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122:327–334. doi: 10.7326/0003-4819-122-5-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 30.Terry MB, Neugut AI, Bostick RM, Sandler RS, Haile RW, Jacobson JS, Fenoglio-Preiser CM, Potter JD. Risk factors for advanced colorectal adenomas: a pooled analysis. Cancer Epidemiol Biomarkers Prev. 2002;11:622–629. [PubMed] [Google Scholar]
- 31.Schoen RE, Weissfeld JL, Kuller LH, Thaete FL, Evans RW, Hayes RB, Rosen CJ. Insulin-like growth factor-I and insulin are associated with the presence and advancement of adenomatous polyps. Gastroenterology. 2005;129:464–475. doi: 10.1016/j.gastro.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 32.Stryker SJ, Wolff BG, Culp CE, Libbe SD, Ilstrup DM, MacCarty RL. Natural history of untreated colonic polyps. Gastroenterology. 1987;93:1009–1013. doi: 10.1016/0016-5085(87)90563-4. [DOI] [PubMed] [Google Scholar]
- 33.Millan A, Huerta S. Apoptosis-inducing factor and colon cancer. J Surg Res. 2009;151:163–170. doi: 10.1016/j.jss.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 34.Paraskeva C, Corfield AP, Harper S, Hague A, Audcent K, Williams AC. Colorectal carcinogenesis: sequential steps in the in vitro immortalization and transformation of human colonic epithelial cells (review) Anticancer Res. 1990;10:1189–1200. [PubMed] [Google Scholar]
- 35.Gryfe R, Swallow C, Bapat B, Redston M, Gallinger S, Couture J. Molecular biology of colorectal cancer. Curr Probl Cancer. 1997;21:233–300. doi: 10.1016/s0147-0272(97)80003-7. [DOI] [PubMed] [Google Scholar]
- 36.Takayama T, Miyanishi K, Hayashi T, Kukitsu T, Takanashi K, Ishiwatari H, Kogawa T, Abe T, Niitsu Y. Aberrant crypt foci: detection, gene abnormalities, and clinical usefulness. Clin Gastroenterol Hepatol. 2005;3:S42–S45. doi: 10.1016/s1542-3565(05)00257-0. [DOI] [PubMed] [Google Scholar]
- 37.Matsubara N. Epigenetic regulation and colorectal cancer. Dis Colon Rectum. 2012;55:96–104. doi: 10.1097/DCR.0b013e318233a1ef. [DOI] [PubMed] [Google Scholar]
- 38.Sung JJ, Lau JY, Goh KL, Leung WK. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005;6:871–876. doi: 10.1016/S1470-2045(05)70422-8. [DOI] [PubMed] [Google Scholar]
- 39.Yang YX, Hennessy S, Lewis JD. Type 2 diabetes mellitus and the risk of colorectal cancer. Clin Gastroenterol Hepatol. 2005;3:587–594. doi: 10.1016/s1542-3565(05)00152-7. [DOI] [PubMed] [Google Scholar]
- 40.Larsson SC, Orsini N, Wolk A. Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst. 2005;97:1679–1687. doi: 10.1093/jnci/dji375. [DOI] [PubMed] [Google Scholar]
- 41.Limburg PJ, Vierkant RA, Fredericksen ZS, Leibson CL, Rizza RA, Gupta AK, Ahlquist DA, Melton LJ, Sellers TA, Cerhan JR. Clinically confirmed type 2 diabetes mellitus and colorectal cancer risk: a population-based, retrospective cohort study. Am J Gastroenterol. 2006;101:1872–1879. doi: 10.1111/j.1572-0241.2006.00725.x. [DOI] [PubMed] [Google Scholar]
- 42.Campbell PT, Deka A, Jacobs EJ, Newton CC, Hildebrand JS, McCullough ML, Limburg PJ, Gapstur SM. Prospective study reveals associations between colorectal cancer and type 2 diabetes mellitus or insulin use in men. Gastroenterology. 2010;139:1138–1146. doi: 10.1053/j.gastro.2010.06.072. [DOI] [PubMed] [Google Scholar]
- 43.La Vecchia C, Negri E, Decarli A, Franceschi S. Diabetes mellitus and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 1997;6:1007–1010. [PubMed] [Google Scholar]
- 44.Krämer HU, Müller H, Stegmaier C, Rothenbacher D, Raum E, Brenner H. Type 2 diabetes mellitus and gender-specific risk for colorectal neoplasia. Eur J Epidemiol. 2012;27:341–347. doi: 10.1007/s10654-012-9686-6. [DOI] [PubMed] [Google Scholar]
- 45.Onitilo AA, Berg RL, Engel JM, Glurich I, Stankowski RV, Williams G, Doi SA. Increased risk of colon cancer in men in the pre-diabetes phase. PLoS One. 2013;8:e70426. doi: 10.1371/journal.pone.0070426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sass DA, Schoen RE, Weissfeld JL, Weissfeld L, Thaete FL, Kuller LH, McAdams M, Lanza E, Schatzkin A. Relationship of visceral adipose tissue to recurrence of adenomatous polyps. Am J Gastroenterol. 2004;99:687–693. doi: 10.1111/j.1572-0241.2004.04136.x. [DOI] [PubMed] [Google Scholar]
- 47.Chen CD, Yen MF, Wang WM, Wong JM, Chen TH. A case-cohort study for the disease natural history of adenoma-carcinoma and de novo carcinoma and surveillance of colon and rectum after polypectomy: implication for efficacy of colonoscopy. Br J Cancer. 2003;88:1866–1873. doi: 10.1038/sj.bjc.6601007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuk JL, Church TS, Blair SN, Ross R. Measurement site and the association between visceral and abdominal subcutaneous adipose tissue with metabolic risk in women. Obesity (Silver Spring) 2010;18:1336–1340. doi: 10.1038/oby.2009.414. [DOI] [PubMed] [Google Scholar]
- 49.Kuk JL, Church TS, Blair SN, Ross R. Does measurement site for visceral and abdominal subcutaneous adipose tissue alter associations with the metabolic syndrome? Diabetes Care. 2006;29:679–684. doi: 10.2337/diacare.29.03.06.dc05-1500. [DOI] [PubMed] [Google Scholar]


