Abstract
In intestinal helminth infections, Th2 immune respones are generally associated with mucin secretion for worm expulsion from the host intestine. In particular, IL-4 and IL-13 are the important cytokines related with intestinal mucus production via STAT6 signalling in nematode infections. However, this perspective has never been studied in Gymnophalloides seoi infection. The present study aimed to observe the STAT6 signalling and cytokine responses in C57BL/6 mice, a mouse strain resistant to infection with this trematode. The results showed that worm expulsion occurred actively during days 1-2 post-infection (PI), when goblet cells began to proliferate in the small intestine. The STAT6 gene expression in the mouse spleen became remarkable from day 2 PI. Moreover, G. seoi infection induced a significant increase of IL-13 from day 4 PI in the spleen of infected mice. Our results suggested that goblet cell hyperplasia and worm expulsion in G. seoi-infected mice should be induced by STAT6 signalling, in which IL-13 may be involved as a dominant triggering cytokine.
Keywords: Gymnophalloides seoi, intestinal trematode, goblet cell hyperplasia, worm expulsion, IL-13, STAT6
In intestinal helminth infections, increased expressions of IL-4 and IL-13 can directly affect cell populations that express IL-4R, and IL-4R signalling is largely dependent on the actions of the signal transducer and activator of transcription 6 (STAT6) [1]. In mouse models, intestinal nematodes induce a strong Th2-biased response, represented by an increase of IL-4 and IL-13 expressions and causing hyperplasia of mucin-secreting goblet cells [1-3]. IL-4Rα-deficient mice showed a delayed ability to resolve Nippostrongylus brasiliensis infection, with significantly prolonged fecal egg recovery and delayed worm expulsion [4]. The delayed worm expulsion was related to delayed intestinal goblet cell hyperplasia [4]. This result emphasized that the IL-13/IL-4Rα/STAT6 signalling pathway was essential in control of intestinal nematode infections.
During the infection period, STAT6 is also critical in the development of intestinal muscle hypercontractility, and both IL-4 and IL-13 influence the second message system of muscle cells by acting on the calcium channel or on the muscuranic receptor, either of which subsequently alters intestinal muscle contractility [1]. As increased contractility is associated with parasite expulsion [3], Th2-type immune response is an important mechanism behind worm expulsion from the intestine. A previous study in T. spiralis-infected mice has shown that both IL-4 and IL-13 induce hypercontractility of muscle cells via the STAT6 pathway, and this is a cellular mechanism for hypercontractility of the intestine [5].
The mechanisms of worm expulsion in intestinal trematode infections have been extensively studied in Metagonimus yokogawai, Echinostoma hortense, Neodiplostomum seoulense, and Gymnophalloides seoi [6]. In these models, several immune effector cells, including intestinal intraepithelial lymphocytes, mast cells, and goblet cells, were found in greater numbers along the villous epithelial layer of the small intestine in the respective definitive hosts [6]. Intestinal mastocytosis, goblet cell hyperplasia, eosinophilia, increase of mucosal IgA, and infiltration of macrophages into the small intestine have all been known to play important roles in the expulsion of intestinal trematodes [6,7]. However, trematode infections have generally not been the subject of study as much as nematode infections.
G. seoi is an intestinal trematode reported in patients with acute pancreatitis or diabetes mellitus [8], and was subsequently found to be transmitted by consumption of raw oysters, Crassostrea gigas [9]. In animal studies, mice experimentally infected with G. seoi exhibited villous atrophy, crypt hyperplasia, and goblet cell hyperplasia with inflammatory reactions in the villous stroma and crypt [6,10]. It was shown that CD4+ T-cells play an important role as a mediator of goblet cell hyperplasia but did not cause functional activation of goblet cells [10]. Because goblet cell hyperplasia is induced in the early phase of infection, there is little information regarding cellular events, such as STAT6 signalling. Thus, G. seoi provides a decent trematode model for a study.
In this study, we observed STAT6 expression in the spleen of C57BL/6 mice (a resistant mouse strain to infection with G. seoi), together with worm recoveries and goblet cell responses during days 0-7 post-infection (PI) with G. seoi. In addition, we also observed IL-4 and IL-13 levels in the spleen cell cultures during goblet cell hyperplasia and STAT6 expression in these mice.
Specific pathogen-free (SPF) female C57BL/6 mice were purchased from Koatech Laboratory Animal Center (Pyeongtaek-shi, Gyeonggi-do, Korea). After an acclimation period of 1 week, mice were housed in an animal facility equipped with SPF conditions at the Seoul National University College of Medicine [11]. Seven-week-old C57BL/6 mice were infected with G. seoi metacercariae. Animal experiments were carried out in accordance with the guidelines of Institutional Animal Care and User Committee, Seoul National University College of Medicine, Seoul, Korea.
For preparation of G. seoi metacercariae, oysters (Crassostrea gigas) were collected from Aphaedo, Shinan-gun, a known endemic area [9,10]. Each oyster shell was detached, and the oyster body was treated with artificial digestive solution containing 0.6% pepsin (1:10,000; Sigma-Aldrich, St. Louis, Missouri, USA) and 0.8% HCl at 37℃ for 10 min. The resulting product containing free metacercariae was washed several times with normal physiological saline. The solution was processed through Baermann's apparatus, and the presence of metacercariae was confirmed under a stereomicroscope. Each mouse was orally infected with 200 metacercariae in 0.2 ml of saline using a gavage needle (Cadence Science, Lake Sucess, New York, USA). Mice were euthanized under ether anesthesia to recover the worms and to collect the spleen for immunoassays. After incubation for 1 hr in Baermann's apparatus, the intestinal segments were returned to Petri dishes and examined under a stereomicroscope for residual flukes. The flukes were collected from the bottom of the tube equipped in the apparatus.
For the observation of goblet cells, 2-cm intestinal segments from the middle portion of the jejunum were washed with normal saline (0.9% sodium chloride) and fixed with 10% formalin. The tissues were embedded in paraffin and sectioned to a 5 µm thickness. The slides were deparaffinized serially with xylene and alcohol before staining, then oxidized by 1% periodic acid (Sigma Aldrich, Poole, UK) for 5 min, and reacted with Schiff's reagent to produce a colored end product. They were counterstained with hematoxylin (Sigma). Goblet cell (GC) numbers were counted per 10 villus-crypts units.
The mouse spleen was isolated aseptically, and single cell suspensions of splenocytes was prepared in cold Hank's balanced salt solution (HBSS) (Sigma) containing 2% FBS (Gibco BRL, Rockville, Maryland, USA). After splenocytes were washed with 2% FBS-HBSS and centrifuged at 1,500 rpm for 10 min, RBC in the cell pellet was lysed with the lysis buffer (NH4Cl 150 mM, KHCO3 1 mM, EDTA 0.01 mM) for 1 min. After further washing, the supernatant was decanted and splenocytes were resuspended in complete RPMI media containing 1% HEPES buffer, 10% FBS, 50 mM 2-ME, 2 mM L-glutamate, 1% glucose, 2% sodium bicarbonate, 1% sodium pyruvate, and 1% antibiotics. The resulting collection of splenocytes were divided into and incubated in 96-well plates (5×105 cells per well) (Nunc, Roskilde, Denmark) under 37℃ and 5% CO2 atmosphere. Culture supernatant was collected after 72 hr of incubation and stored at -80℃.
Culture supernatants of splenocytes were assayed for IL-4 and IL-13 using ELISA kits (BD Pharmingen, San Diego, California, USA). G. seoi antigen for in vitro stimulation of splenocytes was prepared from metacercariae (GMAg) and adult worms (GAAg). The worms were homogenized using a glass-teflon homogenizer and were spun down at 13,200 rpm at 4℃ for 20 min. Each resulting supernatant was filtered through a 0.45 µm disposable syringe filter (MFS Inc., Pleasanton, California, USA) and stored at -80℃ until required. Protein concentrations were determined using Nanodrop 2000 spectrophotometer (Thermo Scientific, Wilmington, Delaware, USA). GMAg and GAAg were added 100 µg/ml per well for cell stimulation. To examine STAT6 expression, the splenocytes were lysed using radioimmunoprecipitation assay (RIPA) buffer (1×PBS, 1% NP-40, 0.05% sodium deoxycholate, and 0.1% sodium dodecyl sulfate) with 10% protease and phosphatase inhibitor cocktail (Pierce, Rockford, Illinois, USA), and kept for 30 min on ice. The lysate was obtained by centrifugation at 13,200 rpm for 30 min at 4℃. The protein concentration was assessed by BCA protein assay kit (Pierce) using bovine plasma globulin as the standard and was read at 562 nm of spectrophotometer. The determined protein samples were boiled with sample buffer for 3 min at 99℃. Equal amounts of protein were loaded on each lane of 10% SDS-PAGE gel, and were separated in the running buffer at 100 V. After the gel was transferred onto a PVDF membrane (BioRad, Richmond, California, USA), the PVDF membrane was blocked with 1× TBS-T containing 5% skim milk for 2 hr at room temperature. Subsequently, the membrane was incubated with anti-STAT6 (Santa Cruz, California, USA) and anti-β-actin antibodies (Santa Cruz) for overnight at 4℃. The membrane was washed 3 times for 10 min with TBS-T (1× TBS, 0.01% Tween-20), and then incubated with HRP-conjugated secondary antibody (1:2,000) in blocking buffer with 5% skim milk for 1 hr at room temperature. After washing, the protein band on the membrane was visualized by LAS-4000 system (Fujifilm, Tokyo, Japan). Data are presented as mean±SEM. Statistical significance of data was analyzed using the Student's t-test. A P-value of <0.05 was considered statistically significant.
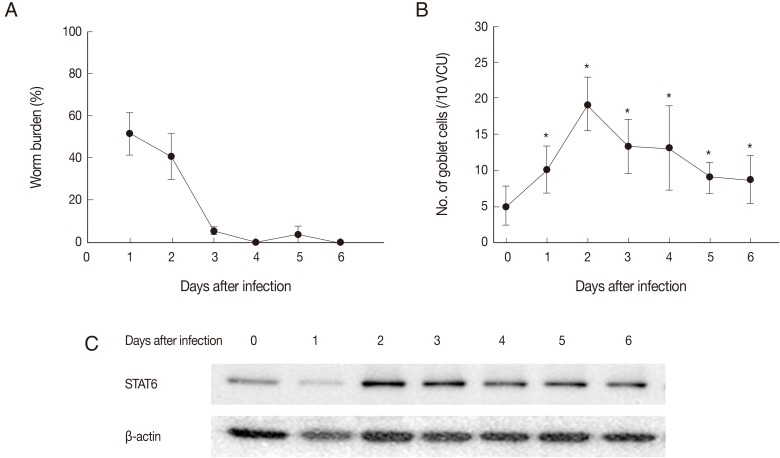
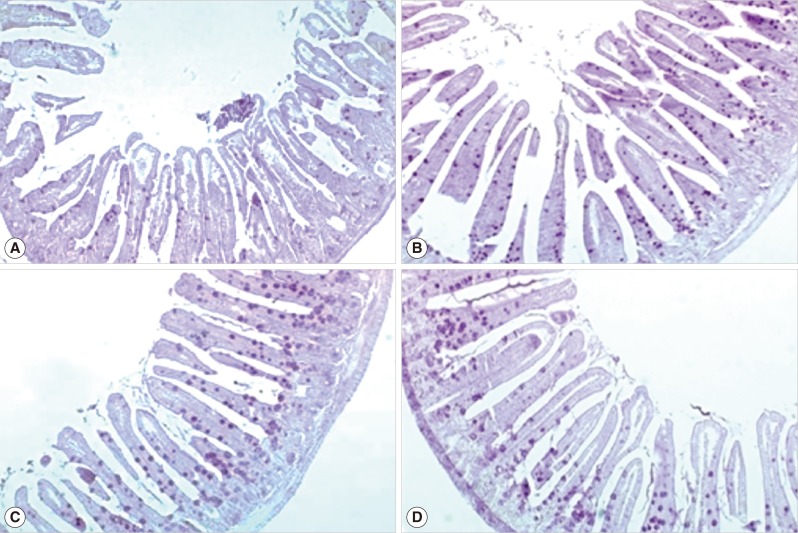
C57BL/6 mice were infected with 200 metacercariae of G. seoi, and the worm burden in the small intestine was examined everyday for 6 days PI (Fig. 1). G. seoi worms were rapidly expelled from the small intestine, and were found with rare frequency on day 6 PI. The worm recovery was 51.8%, 5.7%, and 4.0% on days 1, 3, and 5 PI, respectively (Fig. 1A). The proliferation of goblet cells in G. seoi-infected mice was remarkable (Fig. 2), when compared to uninfected mice. The goblet cell count was highest on day 2 PI. The counts per 10 villus-crypt units (VCU) were 5.1±2.7 (day 0 PI), 10.1±3.2 (day 1 PI), 19.2±3.7 (day 2 PI), 13.3±3.7 (day 3 PI), 13.1±5.8 (day 4 PI), 9.0±2.2 (day 5 PI), and 8.7±3.3 (day 6 PI) (Fig. 1B). Goblet cell hyperplasia continued during those 6 days, until the worms were expulsed.
Fig. 1.
Worm recovery, goblet cell responses, and STAT6 expression in C57BL/6 mice infected with 200 metacercariae of G. seoi and sacrificed every day after infection. (A) Chronological worm recovery (%) in mice infected with G. seoi. Each value represents mean±SD from 3 mice. (B) Goblet cell numbers per 10 villus-crypt unit (VCU) in the small intestine of mice infected with G. seoi. *P<0.05. (C) STAT6 expression in the spleen of mice infected with G. seoi. Splenocytes were harvested from mice during experimental period and lysed using RIPA buffer. STAT6 concentration in the cell lysate was determined by Western blot analysis. β-actin was used as the housekeeping protein.
Fig. 2.
Intestinal sections showing goblet cell hyperplasia in the jejunum of a normal (A) and G. seoi-infected C57BL/6 mice (B, day 2 PI; C, day 3 PI; D, day 4 PI). Periodic acid Schiff (PAS) stain. ×100.
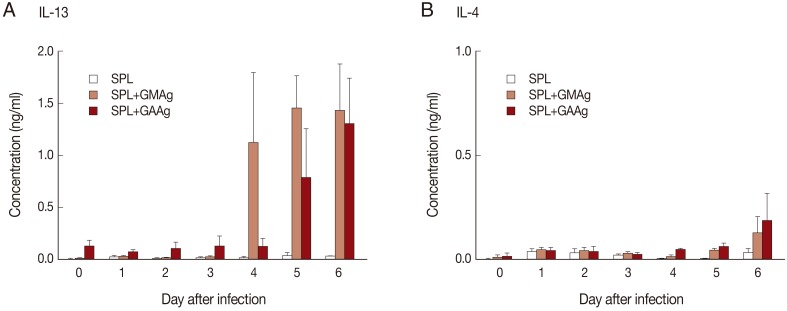
From day 2 PI, STAT6 was highly expressed (Fig. 1C). To determine cytokines associated with STAT6 expression, the in vitro-cultured splenocytes were assayed for IL-4 and IL-13. When splenocytes were cultured with GMAg, these cells produced significantly high levels of IL-13 from day 4 PI (P<0.05), suggesting that IL-13 might be triggering IL-4Rα in G. seoi infection (Fig. 3A). IL-4 was not significantly increased during G. seoi infection (Fig. 3B).
Fig. 3.
IL-13 and IL-4 expressions in the spleen of mice infected with G. seoi. (A) IL-13 concentrations in the spleen after infection, as determined from the supernatant of cultured cells stimulated with G. seoi antigen, using an IL-13 ELISA kit. (B) IL-4 concentrations in the spleen after infection, as determined from the supernatant of cultured cells stimulated with G. seoi antigen, using an IL-4 ELISA kit. SPL, spleen cells; GMAg, G. seoi metacercaria antigen; GAAg, G. seoi adult antigen.
In our previous study which investigated the role of CD4+ T-helper cells in C57BL/6 (resistant) and ICR (susceptible) mice, C57BL/6 showed high numbers of mucosal goblet cells and increased mRNA expressions of IL-4 and IL-5 in mesenteric lymph node (MLN) cells during the early stage of infection [10]. In addition, when CD4+ T-cells from G. seoi-infected mice were adoptively transferred to other infected mice, these mice showed increased worm expulsion and goblet cell hyperplasia [10]. However, alteration of the terminal sugar of mucins, which is indicative of functional activation of goblet cells, was independent from CD4+ T-cells in G. seoi infection [10]. This implied that goblet cell hyperplasia should be regulated by CD4+-T cells but alteration of the terminal sugar chain of mucins may be probably induced by a non-CD4+ T-cell-dependent process [10].
In general, Th2 immune responses in intestinal helminth infection can be represented by goblet cell hyperplasia, increased mucin secretion, mast cell hyperplasia, and increased intestinal muscle contractility [2,5,12-16]. These immune responses have been well studied in nematode infections [1-5,13-16]. IL-4 and IL-13 play an important role in generation of intestinal muscle contractility in mice infected with Heligmosomoides polygyrus and N. brasiliensis, partly dependent on STAT6 expression [17]. Also in T. spiralis infection, the enteric muscle function was important in worm expulsion, and STAT6 activated by IL-4 and IL-13 was critical in the development of intestinal muscle hypercontractility [18]. Thus, IL-4 and IL-13 have multiple effects on induction of mastocytosis, mucin secretion, and smooth muscle contractility [19]. Since IL-4 and IL-13 share the receptor IL-4Rα for mediating STAT6 signalling pathway, a dominant expression of either IL-4 or IL-13 can contribute to the host defense [16,17].
However, the role of IL-4 and IL-13 is quite different from each other as reported in intestinal nematode and cestode infections [14-17,19]. It has been shown that mast cell hyperplasia is strongly influenced by IL-4, wherease goblet cell hyperplasia is apparently much more dependent on IL-13 [15]. However, the roles of IL-4 and IL-13 are not well-known in trematode infections. In particular, very little is known about the STAT6 signalling mechanism during an intestinal trematode infection.
In a trematode infection, it was reported that G. seoi induced intestinal inflammation characterized by marked mucin hypersecretion and goblet cell hyperplasia in rodent models, which emphasized the role of goblet cell hyperplsia on parasite expulsion [6,10]. In our study, the number of goblet cells was the highest on day 2 PI, and subsequently, the worm expulsion occurred maximum by day 3 PI. Meanwhile, the expression of STAT6 was increased from day 2 PI in the spleen. This suggests that G. seoi infection may be controlled by STAT6-based Th2 immune responses, as was previously reported in intestinal nematode infections [1-6,16-18].
Our results showed that, in the presence of G. seoi infection, the cytokine which was directly associated with STAT6-related immune response was IL-13 but not IL-4. This suggests that IL-13 may be associated with goblet cell hyperplasia and worm expulsion. However, IL-13 production was significantly increased on days 4-6 PI rather than in an earlier course of infection. In comparison, IL-4 production in splenocytes stimulated with GMAg or GAAg never increased during the infection period. In our previous study, C57BL/6 mice infected with G. seoi induced cytokines related with Th2- as well as Th1-type immune responses in MLN [10]. Both Th1 cytokines (IL-1α, IL-1β, IL-2, IFN-γ, and TNF-α) and Th2 cytokines (IL-4, IL-5, and IL-13) increased on day 2 PI [10]. Therefore, it is suggested that IL-4 may be induced in the early stage of infection within day 3 PI in the regional MLN and but not in the spleen. In the case of IL-13, it may become induced in the early stage in MLN and reach the peak in later stages in the spleen.
IL-4 and IL-13 have been found to mediate specific functions during Th2 immune responses, with IL-4 facilitating humoral IgG1 and IgE production and IL-13 contributing to epithelial hyperplasia and eosinophil recruitment in peripheral tissues [12,20]. In G. seoi infection in C57BL/6 mice, IL-13 production, together with STAT6 expression, may contribute to goblet cell hyperplasia and worm expulsion.
ACKNOWLEDGMENTS
This study was supported by a grant no. 02-2008-023 from the Seoul National University Bundang Hospital (SNUBH) Research Fund and by a grant no. 04-2011-0520 from the Seoul National University Hospital (SNUH) Research Fund.
Footnotes
We have no conflict of interest related to this work.
References
- 1.Anthony RM, Rutitzky LI, Urban JF, Jr, Stadecker MJ, Gause WC. Protective immune mechanisms in helminth infection. Nat Rev Immunol. 2007;7:975–987. doi: 10.1038/nri2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maizels RM, Holland MJ. Parasite immunology: pathways for expelling intestinal helminths. Curr Biol. 1998;8:R711–R714. doi: 10.1016/s0960-9822(98)70455-5. [DOI] [PubMed] [Google Scholar]
- 3.Khan WI, Collins SM. Immune-mediated alteration in gut physiology and its role in host defence in nematode infection. Parasite Immunol. 2004;26:319–326. doi: 10.1111/j.0141-9838.2004.00715.x. [DOI] [PubMed] [Google Scholar]
- 4.Horsnell WG, Cutler AJ, Hoving JC, Mearns H, Myburgh E, Arendse B, Finkelman FD, Owens GK, Erle D, Brombacher F. Delayed goblet cell hyperplasia, acetylcholine receptor expression, and worm expulsion in SMC-specific IL-4Rα-deficient mice. PLoS Pathog. 2007;3:e1. doi: 10.1371/journal.ppat.0030001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akiho H, Blennerhassett P, Deng Y, Collins SM. Role of IL-4, IL-13, and STAT6 in inflammation-induced hypercontractility of murine smooth muscle cells. Am J Physiol Gastrointest Liver Physiol. 2002;282:G226–G232. doi: 10.1152/ajpgi.2002.282.2.G226. [DOI] [PubMed] [Google Scholar]
- 6.Toledo R, Esteban JG, Fried B. Immunology and pathology of intestinal trematodes in their definitive hosts. Adv Parasitol. 2006;63:285–365. doi: 10.1016/S0065-308X(06)63004-2. [DOI] [PubMed] [Google Scholar]
- 7.Shin EH, Lee SH, Kim JL, Chai JY. T-helper-1 and T-helper-2 immune responses in mice infected with the intestinal fluke Neodiplostomum seoulense: their possible roles in worm expulsion and host fatality. J Parasitol. 2007;93:1036–1045. doi: 10.1645/GE-1203R.1. [DOI] [PubMed] [Google Scholar]
- 8.Chai JY, Shin EH, Lee SH, Rim HJ. Two cases of Gymnophalloides seoi infection accompanied by diabetes mellitus. Korean J Parasitol. 1995;33:61–64. doi: 10.3347/kjp.1995.33.1.61. [DOI] [PubMed] [Google Scholar]
- 9.Chai JY, Shin EH, Lee SH, Rim HJ. Foodborne intestinal flukes in Southeast Asia. Korean J Parasitol. 2009;47:S69–S102. doi: 10.3347/kjp.2009.47.S.S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guk SM, Lee JH, Kim HJ, Kim WH, Shin EH, Chai JY. CD4+ T-cell-dependent goblet cell proliferation and expulsion of Gymnophalloides seoi from the intestine of C57BL/6 mice. J Parasitol. 2009;95:581–590. doi: 10.1645/GE-1807.1. [DOI] [PubMed] [Google Scholar]
- 11.Moon JH, Pyo KH, Jung BK, Chun HS, Chai JY, Shin EH. Resistance to Toxoplasma gondii infection in mice treated with silk protein by enhanced immune responses. Korean J Parasitol. 2011;49:303–308. doi: 10.3347/kjp.2011.49.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wynn TA. IL-13 Effector functions. Annu Rev Immunol. 2003;21:425–456. doi: 10.1146/annurev.immunol.21.120601.141142. [DOI] [PubMed] [Google Scholar]
- 13.McKenzie GJ, Fallon PG, Emson CL, Grencis RK, McKenzie AN. Simultaneous disruption of interleukin (IL)-4 and IL-13 defines individual roles in T helper cell type 2-mediated responses. J Exp Med. 1999;189:1565–1572. doi: 10.1084/jem.189.10.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bancroft AJ, McKenzie AN, Grencis RK. A critical role for IL-13 in resistance to intestinal nematode infection. J Immunol. 1998;160:3453–3461. [PubMed] [Google Scholar]
- 15.Knight PA, Brown JK, Pemberton AD. Innate immune response mechanisms in the intestinal epithelium: potential roles for mast cells and goblet cells in the expulsion of adult Trichinella spiralis. Parasitology. 2008;135:655–670. doi: 10.1017/S0031182008004319. [DOI] [PubMed] [Google Scholar]
- 16.Khan WI, Blennerhasset P, Ma C, Matthaei KI, Collins SM. Stat6 dependent goblet cell hyperplasia during intestinal nematode infection. Parasite Immunol. 2001;23:39–42. doi: 10.1046/j.1365-3024.2001.00353.x. [DOI] [PubMed] [Google Scholar]
- 17.Zhao A, McDermott J, Urban JF, Jr, Gause W, Madden KB, Yeung KA, Morris SC, Finkelman FD, Shea-Donohue T. Dependence of IL-4, IL-13, and nematode-induced alterations in murine small intestinal smooth muscle contractility on Stat6 and enteric nerves. J Immunol. 2003;171:948–954. doi: 10.4049/jimmunol.171.2.948. [DOI] [PubMed] [Google Scholar]
- 18.Khan WI. Physiological changes in the gastrointestinal tract and host protective immunity: learning from the mouse-Trichinella spiralis model. Parasitology. 2008;135:671–682. doi: 10.1017/S0031182008004381. [DOI] [PubMed] [Google Scholar]
- 19.Webb RA, Hoque T, Dimas S. Expulsion of the gastrointestinal cestode, Hymenolepis diminuta by tolerant rats: evidence for mediation by a Th2 type immune enhanced goblet cell hyperplasia, increased mucin production and secretion. Parasite Immunol. 2007;29:11–21. doi: 10.1111/j.1365-3024.2006.00908.x. [DOI] [PubMed] [Google Scholar]
- 20.Price AE, Liang HE, Sullivan BM, Reinhardt RL, Eisley CJ, Erle DJ, Locksley RM. Systemically dispersed innate IL-13-expressing cells in type 2 immunity. Proc Natl Acad Sci USA. 2010;107:11489–11494. doi: 10.1073/pnas.1003988107. [DOI] [PMC free article] [PubMed] [Google Scholar]