Abstract
Little is known regarding treatment choices of youth diagnosed with juvenile-onset fibromyalgia (JFM) as they move into young adulthood. Additionally, there is little empirical evidence to guide youth with FM into appropriate treatment options, leading to a variety of therapies used to manage FM symptoms. The purpose of this descriptive study was to examine all therapies used by individuals with JFM as they entered young adulthood and the perceived effectiveness of these treatments. As part of a larger follow-up study, participants completed a web-based survey of all current and past treatments received for FM symptoms 2 years after their initial presentation and diagnosis at a pediatric rheumatology clinic. One hundred ten out of 118 eligible patients participated in the follow-up assessment as young adults (mean age 18.97 years; 93.6% female). A majority of participants reported use of conventional medications (e.g., antidepressants, anti-convulsants) and nondrug therapies (e.g., psychotherapy). Currently and within the past 2 years, antidepressant medications were the most commonly used to manage FM. Complementary treatments were used less often, with massage being the most popular choice. Although currently used treatments were reported as being effective, past treatments, especially medications, were viewed as being more variably effective. This is a potential reason why young adults with JFM might try more complementary and alternative approaches to managing their symptoms. More controlled studies are needed to investigate the effectiveness of these complementary methods to assist treatment providers in giving evidence-based treatment recommendations.
Juvenile fibromyalgia (JFM) is a disorder characterized by widespread musculoskeletal pain, multiple painful tender points, sleep disturbance, fatigue, headaches, and other associated features, such as anxiety and irritable bowel symptoms (Yunus & Masi, 1985). JFM is primarily diagnosed in adolescent girls, and recent research suggests that symptoms tend to be chronic for many patients with JFM, with >60% of patients reporting persistent symptoms ~4 years after diagnosis (Kashikar-Zuck, Parkins, Ting, Verkamp, Lynch-Jordan, & Graham, 2010). Unfortunately, there is no known cure for JFM in youth or FM in adults, and treatments are focused primarily on symptom management (American Pain Society, 2005).
Usual clinical care for JFM in most pediatric rheumatology settings consists of medication management and recommendations for increased physical exercise. Also, psychologic referrals are often made for those patients who are having difficulty coping or may experience comorbid mood or anxiety problems (American Pain Society, 2005). After the initial referral, diagnosis, and stabilization of treatments, patients typically make a transition back to their primary care physician and little is known about their long-term care or subsequent treatment decisions as they move into young adulthood.
PHARMACOLOGY FOR ADULT FM
In adults with FM, there is evidence for the efficacy of a number of different classes of medications, including tricyclic antidepressants (TCAs; e.g., amitriptyline), selective serotonin reuptake inhibitors (SSRIs; e.g., sertraline), serotonin norepinephrine reuptake inhibitors (SNRIs; e.g., duloxetine), and anticonvulsants (e.g.; pregabalin). However, there is no strong evidence demonstrating the superiority of one medication compared to others (Straube, Derry, Moore, & McQuay, 2010). Most medications appear to have limited long-term effectiveness (Straube et al., 2010; Wahner-Roedler, Elkin, Vincent, Thompson, Oh, Loehrer, Mandrekar, & Bauer, 2005) and problems with tolerability and side effects (Stanford, 2009; Walitt, Katz, & Wolfe, 2010). Medication therapies have yet to be investigated in younger patients, resulting in relatively limited treatment options for youth with JFM. Owing to these limitations and the lack of evidence for medication efficacy/safety in children, there is an increasing interest in complementary approaches for JFM management, some of which have been well tested for adults with FM with promising results.
COGNITIVE BEHAVIORAL THERAPY, EXERCISE, AND COMPLEMENTARY AND ALTERNATIVE MEDICINE STRATEGIES IN FM
Cognitive behavioral therapy (CBT) is the most well studied nondrug intervention for FM in adults (Bernardy, Fuber, Kollner, & Hauser, 2010; Glombiewski, Sawyer, Guterman, Koenig, Rief, & Hofmann, 2010) as well as in children (Degotardi, Klass, Rosenberg, Fox, Gallelli, & Gottlieb, 2006; Kashikar-Zuck, Swain, Jones, & Graham, 2005; Kashikar-Zuck, Ting, Arnold, Bean, Powers, Graham,….., & Lovell, 2012). CBT involves training in behavioral pain-coping skills to manage symptoms of FM. For children and adolescents with JFM, CBT is associated with improved physical functioning, ability to cope with pain, improved sleep, and decreased pain intensity and fatigue. In a randomized controlled trial (RCT) of 8 weeks of CBT (n = 57) versus FM education (n = 57) for those diagnosed with JFM, Kashikar-Zuck et al. (2012) found significantly greater reduction in functional disability in those who received CBT compared with FM education. Two other smaller-scale trials (Kashikar-Zuck et al., 2005; Degotardi et al., 2006) showed that 8 weeks of CBT resulted in significant decreases in depressive symptoms, functional disability, pain, somatic symptoms, and fatigue in adolescents with JFM.
In addition, exercise programs of low to moderate intensity have also been found to significantly improve physical function, FM symptoms, quality of life, and pain in adults and children with FM (Hauser et al., 2010; Jones, Clark, & Bennett, 2002; Stephens et al., 2008). Although exercise can be helpful in managing FM symptoms, long-term adherence can be difficult, especially in adolescents with JFM who are coping poorly with their symptoms, because a high level of motivation and consistent effort is needed (Gowans & deHueck, 2004).
Evidence for other nondrug complementary and alternative medicine (CAM)-based approaches, such as acupuncture, massage, yoga, and chiropractic treatment is emerging in the adult FM literature. In a metaanalytic review of seven randomized controlled trials of acupuncture in adults with FM (sample sizes of 20-86; age range 44-55 years; 95% female; 96% white), Langhorst, Klose, Musial, Irnich, and Hauser (2010) found evidence for pain reduction associated with acupuncture compared with sham or simulated acupuncture, but these positive results were found only in studies that had a potential risk of bias. In more well controlled studies, effects on pain, fatigue, sleep, and physical function were not significantly better than control conditions of sham acupuncture.
Barbour (2000) found that massage therapies are widely available and possibly one of the most sought-out therapies among FM patients: 75% of 60 patients with FM (90% female) reported utilizing massage. Of that 75%, three-fourths found it to be effective. In one study, women (n = 37; age range 21-65 years) who received Swedish massage for 24 weeks showed a trend toward improved mobility and reduced helplessness but no improvement in pain, depression, or well-being compared with a standard-care group and standard-care group with follow-up phone calls (Alnigenis, Bradley, Wallick, & Emsley, 2001). Also notable, that study had issues with attrition after the 4-week time point. Although massage is widely used and available, it is not well studied as a therapy for younger populations with FM.
In a recent trial of a yoga intervention for women with FM (n = 53; mean age 53.7 years), Carson et al. (2010), found that a comprehensive 8-week yoga program, including yoga poses, meditation, breathing, and yoga-based coping skills, led to a significant reduction in pain, fatigue, stiffness, depression, and other symptoms compared with a group receiving standard care.
One published small-scale trial investigating the effectiveness of chiropractic care for adult FM (n = 19; age range 25-70 years) (Blunt, Rajwani, & Guerriero, 1997) found that 4 weeks of chiropractic care was associated with a trend toward improvements in pain, strength, range of motion, and disability, but these were not significantly different from a wait-list control group.
Increased knowledge about the application of CAM approaches for the management of adult FM along with fewer concerns about troubling side effects may make these approaches more attractive to youth with JFM and their parents. At present, little is known about the choices that young patients with JFM make regarding their treatment choices as they grow older, a time when they are likely to be making more treatment decisions independently from their parents.
More information is needed about these transitional years from adolescence to young adulthood in individuals who have a chronic condition such as FM. Not only are these youth making more decisions on their own, they are in need of uninterrupted and developmentally appropriate coordinated care (White, 1996). Therefore, the age of the study sample is important to represent the transition period between pediatric care to adult care.
The primary objective of the present paper is to present descriptive findings on the diverse therapies pursued by youth with JFM to examine treatment utilization patterns for a condition with few standard treatment recommendations.
METHOD
Design and Setting
The study was a quantitative, single-group, descriptive design, in which a follow-up survey was administered to former patients seen at a large tertiary-care midwestern children’s hospital. The primary research questions were: 1) What therapies did youth with JFM utilize ≥2 years after they were seen in a pediatric subspecialty rheumatology treatment center? and 2) What therapies did they see as effective? Recruitment was completed in a pediatric rheumatology clinic, where patients with widespread chronic pain are referred by primary care providers to rule out inflammatory disorders such as juvenile arthritis and to make a definitive diagnosis.
Participants
As part of our longitudinal research into the outcomes of patients initially diagnosed with FM in adolescence, we collected information via online survey about the treatments they are currently using and used in the past 2 years, as well as whether they perceived these treatments to be helpful. All participants previously received routine medical care at a pediatric rheumatology clinic. At the time of this 2-year follow-up survey, participants were in their late adolescent–early adult years and none were being actively followed by the pediatric clinic. One hundred eighteen youth were contacted by phone ≥2 years after their initial assessment in the clinic to participate in an online follow-up survey as part of a longitudinal study of with JFM. A multidisciplinary team of rheumatologists, psychologists, nurse specialists, and research staff identified potential participants for the study. Participants met classification criteria for JFM as determined by a pediatric rheumatologist based on the Yunus and Masi (1985) criteria for JFM, i.e., generalized musculoskeletal aching at three or more sites for ≥3 months in the absence of other underlying conditions, laboratory tests within normal limits, severe pain in five out of 18 tender point sites, and at least three associated criteria, such as fatigue, irritable bowel, and sleep disturbance. Participants received a gift card through certified mail as reimbursement for their time and effort.
Procedure
A trained research assistant contacted eligible youth (or their parents if <18 years old) by telephone to request their participation in a web-based follow-up study. If they agreed, written informed consent was obtained (with parental permission and written assent if the participant was <18 years old) by mail. After the signed consent forms were returned, the research assistant called participants to inform them how to access a secure website and provided them with a unique log-in name and password. If participants did not have access to a computer, or expressed a preference for manual completion of measures, they were offered the option of receiving the questionnaires by mail.
Ethics
This study was approved by the hospital site’s Institutional Review Board and conducted in accordance with current ethical standards for human subjects research.
Follow-Up Survey
Items assessing the use and perceived effectiveness of drug and nondrug treatments were part of a larger follow-up survey of current health and physical and emotional functioning. Information was collected regarding all current and past treatments (in the past 2 years) including medications (antidepressants, anticonvulsants, pain analgesics, antimigraine/triptans, muscle relaxants, nonsteroidal antiinflammatory drugs), physical therapy, psychotherapy, and CAM treatments (massage, acupuncture, chiropractic, vitamins/herbal supplements), as well as the perceived helpfulness of each of these treatments. The survey allowed participants to list the therapies by group (medications, physical therapy, and other treatments [e.g., CAM therapies]) that they were currently using or had used in the past for JFM. Then they selected whether this treatment was helpful or not (“yes” or “no”). The participants were able to complete the entire set of questionnaires within ~30-45 minutes.
Statistical Analysis
All data from the online survey were converted to a Microsoft Excel spreadsheet, which was then exported to an SPSS (version 15.0; SPSS, Chicago, IL) database for further analysis. Descriptive data were computed on demographic information and percentages of patients using each type of medication and nonmedication intervention currently and in the past 2 years.
RESULTS
One hundred ten out of 118 contacted youth (93.2%) agreed to participate in the follow-up assessment. Participants were contacted if it had been ≥2 years since their initial diagnosis of JFM in the clinic (mean 40.44 months, SD 21.04 months). Study enrollment was completed from June 2007 to December 2010 with >90% of participants completing the survey within 1-2 weeks of the survey being sent. Participants were primarily female (93.6%) and white (87.3%). The average age of the sample was 18.97 years (range14-25 years, SD 2.37). The average number of years of education was 11.98 years (SD 2.93). For further demographic information, see Table 1. The reasons for the eight individuals not participating in the survey were: unable to establish contact (n = 5), passed away (n = 2), and (n = 1).
TABLE 1. Demographic Characteristics of Study Participants at Follow-Up (n = 110).
| Characteristic | ||
|---|---|---|
|
| ||
| Mean | SD | |
| Age | 18.97 | 2.37 |
| Average length of follow-up (mo) | 40.44 | 21.04 |
| n | % | |
|---|---|---|
| Sex | ||
| Male | 7 | 6.4 |
| Female | 103 | 93.6 |
| Race | ||
| White | 96 | 87.3 |
| Black | 10 | 9.1 |
| Asian | 1 | .9 |
| American Indian/Alaskan Native | 2 | 1.8 |
| Years of education | 11.98 | 2.93 |
Current Treatments
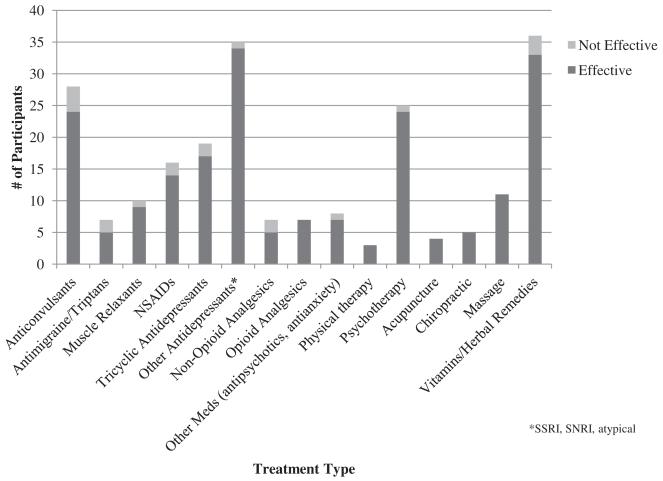
At the time of the follow-up assessment, participants reported using mostly conventional medical and nondrug (i.e, psychotherapy) treatments. Antidepressant medications (e.g., SSRIs, SNRIs, TCAs, atypical antidepressants) were the most commonly used current medications, followed by anticonvulsants. Of the 54 participants (49%) currently using antidepressant medications, 19 (35.2%) used TCAs and 34 (62.9%) used an SSRI, SNRI, or atypical antidepressant.
Twenty-five participants (23%) were active in psychotherapy. Only 3 participants (2.7%) currently participated in physical therapy. For those using CAM treatments (n = 20), four participants (3.6%) received acupuncture, five (4.5%) chiropractic care, and 11 (10%) massage therapy. In addition, a number of participants (n = 36; 32.7%) reported taking vitamin supplements or herbal remedies. For details on all currently used medications and other treatments, see Figure 1.
Figure 1.
■ Frequencies of currently used therapies by youth for juvenile-onset fibromyalgia symptoms and the perceived effectiveness of the therapy.
Treatments in the Past 2 Years
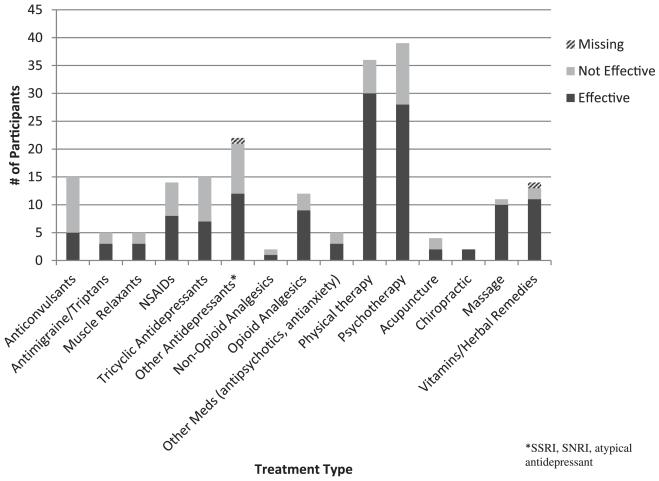
In the past 2 years, participants also reported using primarily conventional medical treatments as well as nondrug therapies. Again, antidepressant medications were the most commonly used treatment, followed by anticonvulsants. Of the 37 participants (33.6%) currently using antidepressant medications, 22 (59.4%) used an SSRI, SNRI, or atypical antidepressant and 15 (40.5%) used TCAs.
Thirty-nine participants (35.4%) reported psychotherapy and 36 (33%) physical therapy. For past complementary treatments, four participants (3.6%) received acupuncture, two (1.8%) chiropractic care, 11 (10%) massage, and 14 (12.7%) vitamins or herbal remedies. All other past medications and treatments are represented in Figure 2.
Figure 2.
■ Frequencies of therapies used in the past by youth for juvenile-onset fibromyalgia symptoms and the perceived effectiveness of the therapy.
Perceived Effectiveness
For current treatments, almost all of the treatments reported were seen as being helpful. There was more variability in the perceived effectiveness of past treatments, especially medications, which were seen as effective by about one-half (54.7%) of the participants, and psychotherapy, which was seen as effective by 71.7%. Physical therapy was seen as being helpful by 83.3%. Massage was the most used CAM therapy (10% of participants) and was seen as being useful by the majority (91%) of those who received this treatment.
DISCUSSION
The findings of this descriptive study reinforce results from our previously published study (Kashikar-Zuck et al., 2010) which found that adolescents with JFM experience long-term FM symptoms and continue to seek out medications and other treatments to manage their condition. Conventional medication and psychotherapy-based approaches were utilized to a greater extent than complementary treatments and may reflect provider recommendations as much as patient choice. Interestingly, participants reported greater use of medications and CAM therapies at the time of the current assessment than in the past 2 years. This pattern might indicate continuing or worsening symptoms, greater knowledge about treatment options, or a greater willingness to try varied therapies as they move into adulthood and make more independent health care decisions. The increase in medications from those reported in the past could also be because the participants were now able to take a variety of medications approved by the FDA for adult FM. Another explanation may be that many parents and health care providers prefer to limit the number and type of medications prescribed at younger ages.
Along with greater use of medications, there was a large increase (12.7% in the past to 32.7% currently) in the number of participants currently taking vitamins and herbal remedies (e.g., multivitamins, melatonin). Additionally, a large decrease in participants utilizing physical therapy was observed despite the high perceived effectiveness of this approach. This may have occurred because as individuals’ move into young adulthood they become more sedentary (CDC, 2009) and may also believe that a “dose” of physical therapy sessions is sufficient for obtaining the necessary knowledge of a home exercise program. However, this survey did not inquire whether the participant was directed or expected to practice exercises at home and whether or not they complied with a home exercise plan. This decrease could also be due to the cost of physical therapy, especially if it is not covered by health insurance or if the amount of physical therapy sessions is limited by an insurance plan.
CAM therapies were not as commonly used by the youth with JFM. The three CAM therapies that emerged as more popular were massage, acupuncture, and chiropractic care. These were more likely to be reported as a current treatment than in the past, indicating that there might be an increasing openness to try these treatments as the individuals become older and/ or more financially able to pursue them. This increase of CAM treatments in adulthood also coincides with findings from a 2007 National Health Interview Survey by the National Center for Complementary and Alternative Medicine (≥18 years old: n = 23,393; ≤17 years old: n = 9,417) that ~38% of adults use a form of CAM and ~12% of children use one (National Center for Complementary and Alternative Medicine, 2008). Nevertheless, the low utilization of CAM treatments in youth with JFM indicates a real need for greater evidence-based work in this area to increase potential nondrug treatment options for this chronic condition.
One notable issue regarding CAM therapies is the out-of-pocket cost of these therapies, because the majority of them are not covered by health insurance. It is currently not feasible for many people to utilize these therapies, which is a key reason that we need more evidence regarding the benefits for adults and youth with FM. More scientific evidence for these therapies increases the potential for them to be adopted in standard care and easier access for patients with FM and other chronic pain conditions.
Study Limitations
It is recognized that this descriptive study has some limitations. First, using self-report surveys of current and past treatments may be influenced by potential recall bias. Additionally, we did not have information about participants’ current treatment providers or access to medical records to corroborate their reports.
CONCLUSIONS AND CLINICAL IMPLICATIONS
This study provides preliminary evidence about the diverse FM treatment choices as individuals with JFM diagnosed in adolescence move into adulthood. Many of the treatments used by participants lack a strong evidence base and clear evidence-based guidelines that would help providers treating FM to offer their patients improved treatment recommendations. In addition, this study brings awareness to treatment providers regarding treatments used and found to be effective by this sample of youth with JFM.
Through greater awareness of the types of therapies, particularly CAM approaches, being used by patients, it is hoped that more controlled studies will be designed to rigorously test the efficacy of these treatments in JFM, to assist treatment providers in giving evidence-based treatment recommendations.
REFERENCES
- Alnigenis MNY, Bradley JD, Wallick J, Emsley CL. Massage therapy in the management of fibromyalgia: A pilot study. Journal of Musculoskeletal Pain. 2001;9(2):55–67. [Google Scholar]
- American Pain Society . Guideline for the management of fibromyaglia syndrome pain in adults and children. American Pain Society; Glenview, IL: 2005. [Google Scholar]
- Barbour C. Use of complementary and alternative treatments by individuals with fibromyalgia syndrome. Journal of the American Academy of Nurse Practitioners. 2000;12(8):311–316. doi: 10.1111/j.1745-7599.2000.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Bernardy K, Fuber N, Kollner V, Hauser W. Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome—A systematic review and metaanalysis of randomized controlled trials. The Journal of Rheumatology. 2010;37(10):1991–2005. doi: 10.3899/jrheum.100104. [DOI] [PubMed] [Google Scholar]
- Blunt KL, Rajwani MH, Guerriero RC. The effectiveness of chiropractic management of fibromyalgia patients: A pilot study. Journal of Manipulative and Physiological Therapeutics. 1997;20(6):389–399. [PubMed] [Google Scholar]
- Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151(2):530–539. doi: 10.1016/j.pain.2010.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report. Youth Risk Behavior Surveillance–United States, 2009. 2009 Retrieved February 6, 2012 from. http://www.cdc.gov/mmwr/pdf/ss/ss5905.pdf. [PubMed]
- Degotardi PJ, Klass ES, Rosenberg BS, Fox DG, Gallelli KA, Gottlieb BS. Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. Journal of Pediatric Psychology. 2006;31(7):714–723. doi: 10.1093/jpepsy/jsj064. [DOI] [PubMed] [Google Scholar]
- Glombiewski JA, Sawyer AT, Gutermann J, Koenig K, Rief W, Hofmann SG. Psychological treatments for fibromyalgia: A meta-analysis. Pain. 2010;151(2):280–295. doi: 10.1016/j.pain.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Gowans SE, deHueck A. Effectiveness of exercise in management of fibromyalgia. Current Opinion in Rheumatology. 2004;16(2):138–142. doi: 10.1097/00002281-200403000-00012. [DOI] [PubMed] [Google Scholar]
- Hauser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, Busch A. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: A systematic review and meta-analysis of randomised controlled trials. Arthritis Research and Therapy. 2010;2(3):R79. doi: 10.1186/ar3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KD, Clark SR, Bennett RM. Prescribing exercise for people with fibromyalgia. AACN Clinical Issues. 2002;13(2):277–293. doi: 10.1097/00044067-200205000-00012. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S, Swain NF, Jones BA, Graham TB. Efficacy of cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. Journal of Rheumatology. 2005;32(8):1594–1602. [PubMed] [Google Scholar]
- Kashikar-Zuck S, Parkins IS, Ting TV, Verkamp E, Lynch-Jordan A, Graham TB. Controlled follow-up study of physical and psychosocial functioning of adolescents with juvenile primary fibromyalgia syndrome. Rheumatology (Oxford) 2010;49(11):2204–2209. doi: 10.1093/rheumatology/keq254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S, Ting TV, Arnold LM, Bean J, Powers SW, Graham TB, Passo MH, Schikler KN, Hashkes PJ, Spalding S, Lynch-Jordan AM, Banez G, Richards MM, Lovell DJ. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: a multisite, single-blind, randomized, controlled clinical trial. Arthritis and Rheumatism. 2012;64(1):297–305. doi: 10.1002/art.30644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhorst J, Klose P, Musial F, Irnich D, Hauser W. Efficacy of acupuncture in fibromyalgia syndrome—A systematic review with a meta-analysis of controlled clinical trials. Rheumatology (Oxford) 2010;49(4):778–788. doi: 10.1093/rheumatology/kep439. [DOI] [PubMed] [Google Scholar]
- National Center for Complementary and Alternative Medicine . The use of complementary and alternative medicine in the United States. National Institutes of Health; Bethesda, MD: 2008. [Google Scholar]
- Stanford SB. Fibromyalgia: Psychiatric drugs target CNS-linked symptoms. Current Psychiatry. 2009;8(3):37–50. [Google Scholar]
- Stephens S, Feldman BM, Bradley N, Schneiderman J, Wright V, Singh-Grewal D, Lefebvre A, Benseler SM, Cameron B, Laxer R, O’Brien C, Schneider R, Silverman E, Spiegel L, Stinson J, Tyrrell PN, Whitney K, Tse SM. Feasibility and effectiveness of an aerobic exercise program in children with fibromyalgia: results of a randomized controlled pilot trial. Arthritis and Rheumatism. 2008;59(10):1399–1406. doi: 10.1002/art.24115. [DOI] [PubMed] [Google Scholar]
- Straube S, Derry S, Moore RA, McQuay HJ. Pregabalin in fibromyalgia: Meta-analysis of efficacy and safety from company clinical trial reports. Rheumatology (Oxford) 2010;49(4):706–715. doi: 10.1093/rheumatology/kep432. [DOI] [PubMed] [Google Scholar]
- Wahner-Roedler DL, Elkin PL, Vincent A, Thompson JM, Oh TH, Loehrer LL, Mandrekar JN, Bauer BA. Use of complementary and alternative medical therapies by patients referred to a fibromyalgia treatment program at a tertiary care center. Mayo Clinic Proceedings. 2005;80(1):55–60. doi: 10.1016/S0025-6196(11)62958-3. [DOI] [PubMed] [Google Scholar]
- Walitt BT, Katz RS, Wolfe F. Treatment with FDA approved therapies in patients with fibromyalgia; Poster presented at the American College of Rheumatology Conference; Atlanta, GA. 2010. [Google Scholar]
- White PH. Future expectations: Adolescents with rheumatic diseases and their transition into adulthood[editorial] British Journal of Rheumatology. 1996;35:80–83. doi: 10.1093/rheumatology/35.1.80. [DOI] [PubMed] [Google Scholar]
- Yunus MB, Masi AT. Juvenile primary fibromyalgia syndrome. A clinical study of thirty-three patients and matched normal controls. Arthritis & Rheumatism. 1985;28(2):138–145. doi: 10.1002/art.1780280205. 10.1002/art.1780280205. [DOI] [PubMed] [Google Scholar]