Abstract
Background
The goal of the current study was to investigate asthma and mental health among youth in the community, and to consider the role of asthma severity and persistence in this link.
Method
Data were drawn from the Raine Study, a population-based birth cohort study in Western Australia. Logistic regression models and generalized estimating equations were used to examine the relationship between asthma at age 5 years and the range of internalizing and externalizing mental health problems at ages 5–17 years. Analyses were stratified by asthma severity and persistence, and adjusted for a range of potential confounders.
Results
More severe and persistent asthma at age 5 was associated with significantly increased odds of affective, anxiety, somatic, oppositional defiant and conduct problems at ages 5–17. Mild asthma and remitted asthma were not associated with heightened vulnerability to mental disorders.
Conclusions
Our results suggest that youth with symptomatic asthma are more likely to suffer from a wide range of mental health problems, and that the likelihood of mental health problems appears to increase as a function of asthma severity. Youth with poorly controlled and/or more severe and persistent asthma may be considered a vulnerable group who might benefit from mental health screening in clinical, school and community settings.
Keywords: ADHD, anxiety, asthma, depression, youth
Introduction
In recent years, there has been growing interest in the relationship between asthma and mental disorders. Data from several cross-sectional (McQuaid et al. 2001; Ortega et al. 2002, 2003, 2004; Goodwin et al. 2003b; Katon et al. 2007; Delmas et al. 2011) and longitudinal (Goodwin et al. 2004, 2005a; Alati et al. 2005; Feldman et al. 2006) community-based studies of youth show a consistent link between asthma and other respiratory symptoms and anxiety disorders among youth. Clinical data has also shown that psychiatric symptoms are associated with increased severity of asthma symptomatology, health service use, functional impairment and poorer asthma control, compared to that among youth without psychiatric symptoms (Morrison et al. 2002; Feldman et al. 2006; McCauley et al. 2007; Richardson et al. 2008).
While evidence of a link between childhood asthma and mental disorders is growing, several key questions remain. First, studies consistently find a link between asthma and anxiety disorders among youth (McQuaid et al. 2001; Morrison et al. 2002; Ortega et al. 2002, 2003, 2004; Goodwin et al. 2003a,b, 2004, 2005a,b; Alati et al. 2005; Feldman et al. 2006; Katon et al. 2007). Yet, relatively few studies have looked at whether and to what degree asthma is associated with mood disorders or with externalizing disorders and findings to date are inconsistent (Wamboldt et al. 2000; Ortega et al. 2004; Alati et al. 2005; Goodwin et al. 2005a). Second, several studies to date have primarily relied on retrospective reports of asthma attacks and/or on reports of asthma that are often grouped with other respiratory symptoms (e.g. ‘participant has bronchitis or asthma’) (Ortega et al. 2002; Alati et al. 2005; Goodwin et al. 2005a). This has resulted in lack of certainty that results are specific to asthma versus transient wheeze and/or bronchitis, which are very common in early childhood and are not interchangeable with asthma. Third, lack of specificity about the time-frame during which asthma occurred has made it difficult to understand the temporal relationship between asthma and mental disorders. Fourth, a substantial percentage of childhood asthma cases resolve by adulthood and it remains unclear whether these carry a risk similar to that associated with chronic and persistent asthma that continues into adulthood. Fifth, there has been little available information on the potential role of asthma severity or chronicity in the relationship between asthma and mental disorders. Previous studies have looked at asthma severity in relation to organic disease and pulmonary function (Federico et al. 2007), yet no previous study of the relationship between asthma and mental disorders has included this information. According to National Heart Blood and Lung Institute (NHBLI) guidelines (NHLBI, 2007), distinguishing asthma into mild, moderate or severe and intermittent or persistent is critical in evaluation and treatment planning.
Against this background, the current study addresses two main questions using a birth cohort study with well-measured asthma and well-defined mental health. First, the study investigates whether childhood asthma at age 5 years is associated with increased vulnerability to the range of internalizing and externalizing disorders up to age 17 years. Second, the study examines whether and to what degree asthma severity and/or persistence impact the relationship between asthma and mental health problems.
Method
The Western Australian Pregnancy Cohort (Raine) Study, initially established between 1989 and 1992, consists of 2868 children from Perth, Western Australia, who have been followed from birth. The study first began as a pregnancy cohort in which 2900 women were enrolled (representing 90% of eligible women approached to take part in the study), approximately 100 women per month for 3 years, at around week 18 of gestation (Newnham et al. 1993). The women were enrolled from the antenatal booking clinics at King Edward Memorial Hospital (KEMH), the principal tertiary obstetrics hospital in Perth, Western Australia. The criteria for enrolment were gestational age between 16 and 20 weeks, sufficient proficiency in English to understand the implications of participation, an expectation to deliver at the hospital, and an intention to remain in Western Australia so that follow-up through childhood would be possible. Mothers were not selected on the basis of any asthma or atopy criteria. As KEMH is the only specialist obstetric care center in Western Australia, the initial sample was at moderate obstetric risk, and the participating mothers reflect the population obtaining obstetrical care in this region. Thus this is a community-based cohort representing about 20% of all live births in Western Australia, with exclusions only for very low birthweight or birth defects. The population was 84% Caucasian, 4% Aboriginal and 12% other (primarily Asian); reflective of the population in Western Australia at the time. All children were examined at birth and extensive antenatal data were collected regarding maternal sociodemographic characteristics, including age and education. Informed consent was obtained at the time of enrolment in the study and at every subsequent follow-up and study protocols were approved by the Human Ethics Committees at KEMH and Princess Margaret Hospital for Children in Perth, Western Australia.
The cohort attended follow-up visits at ages 1, 2, 3, 5, 8, 10, 14 and 17 years, consisting of comprehensive behavioral and physical health questionnaires completed by the primary caregiver (usually mother). At the 17-year follow-up, 1754 study adolescents and their families completed all or part of the follow-up (414 deferred participation, 184 were unable to be traced, 480 had withdrawn and 36 were deceased). There were complete mental health data available for 1368 adolescents at the 17-year follow-up, representing just over 47% of the original cohort.
Asthma
Current asthma at age 5 was defined by the presence of parental report of physician diagnosis of asthma, wheezing or a cough in the absence of a cold over the last 12 months, and taking asthma medication in the preceding 12 months by parental report (Joseph-Bowen et al. 2004). Asthma was categorized as mild, moderate, and severe on the basis of parental report of clinical symptoms throughout the year according to a schema adapted from the Asthma Management Handbook (National Asthma Council Australia, 2006). A mild case of asthma included 1–2 episodes of wheezing in the past 12 months. A moderate case of asthma included 3–12 wheezing episodes, and on average only one occasion of nocturnal wakening per week due to wheezing episodes over last 12 months. Severe asthma was defined as at least one of the following characteristics occurring over the past year: greater than 12 instances of wheeze, more than one episode of nocturnal wakening due to wheezing, or on average one or more episodes of acute asthma limiting speech. Finally, we examined active versus remitted asthma by analyzing those with asthma at age 5 compared to reports of wheezing in the last 12 months at the 8-year follow-up. From this data we created a four-level variable representing no asthma at age 5 and no recent wheezing at age 8 (reference category), asthma at age 5 but no recent wheezing at age 8 (‘remitted’), no asthma at age 5 but recent wheezing at age 8 (‘later onset’) and asthma at age 5 and wheezing at age 8 (‘persistent’). The diagnostic level of the severest level of symptoms reported was assigned.
Mental health problems
The 118-item Child Behavior Checklist for Ages 4–18 (CBCL/4–18) was administered at the 5-, 8-, 10-, 14- and 17-year follow-ups and completed by the primary caregiver (Achenbach, 1991). The CBCL demonstrated good sensitivity (83% overall) and specificity (67% overall) to a clinical psychiatric diagnosis and good test–retest reliability in a Western Australian clinical calibration (Zubrick et al. 1997). The CBCL/4–18 produces a raw score that was transformed into T scores (standardized by age and sex) for six problem scales using the CBCL DSM-Oriented Scales (Achenbach, 2001). The problem scales are considered to map well against the diagnostic criteria of DSM-IV for affective problems (e.g. major depression, dysthymia), anxiety problems (e.g. generalized anxiety disorder), somatic problems (e.g. somatization disorder), attention deficit hyperactivity problems (e.g. inattentive or hyperactive-impulsive type disorders), oppositional defiant problems (e.g. oppositional defiant disorder) and conduct problems (e.g. conduct disorder) (APA, 2000). For this study, we applied the recommended clinical cut-off scores (by age and sex) to obtain a binary variable indicative of clinically significant affective, anxiety, somatic, attention deficit hyperactivity disorder (ADHD), oppositional defiant and conduct problems. The clinical cut-offs were as specified by the CBCL DSM-Oriented Scales, and applied to raw scores normalized for age and sex (T≥65). The term ‘clinically significant’ refers to maladaptive behavior that falls within a defined clinical range for behavioral problems (Achenbach, 1991).
Maternal mental health and cigarette smoking
At 18 weeks’ gestation, women reported the number of cigarettes currently smoked per day and this was categorized into a dichotomous variable of ‘any’ and ‘no smoking’ in pregnancy. The classification was deliberately broad to account for social desirability factors in responding. The number of cigarettes smoked per day at 34 weeks’ gestation was strongly correlated with the number of cigarettes smoked at 18 weeks’ gestation (r=0.866, p<0.001), indicating few women quit smoking after 18 weeks’ gestation. At the 5-year follow-up interview, information on maternal smoking was obtained from the parent/caregiver, and this was categorized as no smoking compared to smoking one or more cigarettes per day. Information was retrospectively collected at the 8-year follow-up as to whether the mother had ever been treated for an emotional or mental health problem, and this was classified according to yes/no responses.
Family functioning
We used the parent-report General Functioning Scale (GFS) from the McMaster Family Assessment Device (FAD) administered at the 5-year follow-up as a measure of family functioning (Epstein et al. 1983). This short-form scale consists of 12 statements that were derived from an item-analysis of the complete 60-item scale, including questions on problem solving, family communication, affective responsiveness, and behavior control. The GFS has excellent reliability [r (Guttman’s split-half=0.83)] and internal consistency (Cronbach’s α=0.86) (Byles et al. 1988).
Data analysis
Frequency data were compared for all control variables according to asthma diagnosis at age 5 (predictor variable). We used a logistic regression model to examine the ability of our predictor variable to effect changes in T scores reflecting clinically meaningful differences in affective, anxiety, somatic, ADHD, oppositional defiant and conduct problems from ages 5–17 years (i.e. a score above the relevant clinical cutoff point for age and sex). The logistic regression model accounted for loss of independence due to repeated observations of the same individuals over time by incorporating generalized estimating equations (GEE) with a first-order autoregressive [AR(1)] working correlation matrix structure. Our model first examined univariate relationships, followed by the inclusion of all potentially confounding and intermediate variables (maternal age at 18 weeks’ gestation, maternal completion of high school education, maternal smoking at age 5, maternal mental health history at age 8, family functioning at age 5). Given that the GEE model may hide age-specific effects, we examined age interaction effects in all three of our logistic regression with GEE models. We then performed a similar logistic regression model analysis examining the effect of different levels of severity of asthma on CBCL DSM-IV-oriented problem scales, comparing mild, moderate and severe asthma to no asthma diagnosis with adjustment for the confounding and mediating variables outlined above, and then performed the same analysis again for our remitted versus persistent asthma variable. SPSS v. 15.0 (SPSS Inc., USA) was used for the analyses.
Results
At age 5 years, 390 (18%) children had a diagnosis of asthma, with approximately 9% classified in severity as mild, 4% moderate and 5% severe. Male children were more likely (two-tailed p<0.005) to have an asthma diagnosis at age 5 than female children (21% v. 15%), and children whose mothers had completed high school were less likely to have asthma at age 5 than the children whose mothers had not finished high school (15% v. 20%; Table 1). Children whose mothers reported a history of mental health problems at the 8-year follow-up were more likely to have previously had an asthma diagnosis at age 5 compared to children whose mothers did not report ever having an emotional or mental health problem (21% v. 16%). There were no significant differences between children who had asthma and those who did not have asthma at age 5 and maternal age or current smoking status at age 5.
Table 1.
Frequency data by asthma diagnosis at age 5 (N=2193)
| N | No asthma (N=1803) n (%)a |
Asthma (N=390) n (%)a |
pb | |
|---|---|---|---|---|
| Gender of child | 2193 | <0.001* | ||
| Male | 896 (79.4) | 232 (20.6) | ||
| Female | 907 (85.2) | 158 (14.8) | ||
| Maternal age at conception | 2140 | 0.087 | ||
| <20 years | 126 (77.3) | 37 (22.7) | ||
| 20–24.9 years | 335 (81.9) | 74 (18.1) | ||
| 25–29.9 years | 540 (81.9) | 119 (18.1) | ||
| 30–34.9 years | 497 (83.8) | 96 (16.2) | ||
| ≥35 years | 264 (83.5) | 52 (16.5) | ||
| Maternal education | 2141 | 0.004* | ||
| <High school completion | 994 (80.4) | 242 (19.6) | ||
| High school completion | 769 (85.0) | 136 (15.0) | ||
| Maternal smoking at age 5 years | 2188 | 0.113 | ||
| Non-smoker | 1271 (82.9) | 263 (17.1) | ||
| Smoker | 527 (80.6) | 127 (19.4) | ||
| Maternal history of mental health problems | 1945 | 0.014 | ||
| No | 1278 (84.0) | 243 (16.0) | ||
| Yes | 336 (79.2) | 88 (20.8) | ||
| Family functioning at age 5 years | 2048 | 0.460 | ||
| Poor | 279 (17.6) | 83 (17.9) | ||
| Good | 1306 (82.4) | 380 (82.1) |
Row percentages presented, missing data not presented.
χ2p value for linear by linear trend.
p<0.05.
The prevalence of anxiety, oppositional defiant and conduct problems were highest at age 5 (see Table 2). Affective problems showed a peak prevalence of 11% at age 8, and somatic problems had a high prevalence at ages 5 (14%) and 8 (14%) with a peak at age 10 (17%). ADHD problems were the least common with around 2% meeting the clinical criteria at ages 5–14 and only 1% (n=13) meeting the criteria at age 17.
Table 2.
Percentage of participants with DSM-IV scale problems at each follow-upa
| Year 5 (N=2179) n (%) |
Year 8 (N=2088) n (%) |
Year 10 (N=2019) n (%) |
Year 14 (N=1787) n (%) |
Year 17 (N=1368) n (%) |
|
|---|---|---|---|---|---|
| Affective problems | 207 (9.5) | 225 (10.8) | 190 (9.4) | 122 (6.8) | 105 (7.7) |
| Anxiety problems | 180 (8.3) | 143 (6.9) | 120 (5.9) | 87 (4.9) | 39 (2.9) |
| Somatic problems | 292 (13.5) | 295 (14.2) | 336 (16.7) | 127 (7.1) | 76 (5.6) |
| ADHD problems | 51 (2.3) | 50 (2.4) | 36 (1.8) | 36 (2.0) | 13 (1.0) |
| Oppositional defiant problems | 264 (12.1) | 230 (11.0) | 188 (9.3) | 166 (9.3) | 84 (6.1) |
| Conduct problems | 290 (13.3) | 245 (11.7) | 187 (9.3) | 111 (6.2) | 70 (5.1) |
ADHD, Attention deficit hyperactivity disorder.
Percentages represent those participants with problems compared with those without problems at each follow-up.
The unadjusted logistic regression model showed that an asthma diagnosis at age 5 was significantly associated (two-tailed p<0.05) with clinically significant scores on all six DSM-IV-oriented problem scales (Table 3). Following adjustment for control variables there was a significantly increased odds from ages 5–17 years for affective, anxiety, somatic, ADHD, oppositional defiant and conduct problems for children with asthma at age 5 compared to those without asthma. The effect size was similar across disorders. The interactions with age were not significant for the relationship between asthma diagnosis at age 5 and CBCL-DSM diagnoses indicating that the summarizing of scores for each age into the GEE model did not hide specific age effects.
Table 3.
Relationship between asthma at age 5 and CBCL/DSM-IV problems from ages 5–17
| Multivariate logistic GEE model (years 5–17 inclusive) |
||||||
|---|---|---|---|---|---|---|
| Asthma age 5 years |
Affective problems |
Anxiety problems |
Somatic problems |
ADHD problems |
Oppositional defiant problems |
Conduct problems |
| Unadjusted | ||||||
| OR | 1.57** | 1.72** | 1.75** | 1.72* | 1.66** | 1.72** |
| 95% CI | 1.24–1.98 | 1.31–2.26 | 1.44–2.12 | 1.10–2.70 | 1.30–2.10 | 1.36–2.18 |
| p value | <0.001 | <0.001 | <0.001 | 0.017 | <0.001 | <0.001 |
| Adjusteda | ||||||
| OR | 1.47* | 1.64** | 1.62** | 1.84* | 1.51** | 1.53** |
| 95% CI | 1.11–1.95 | 1.21–2.23 | 1.31–2.02 | 1.11–3.02 | 1.15–1.98 | 1.18–2.00 |
| p value | 0.007 | 0.002 | <0.001 | 0.017 | 0.003 | 0.002 |
CBCL, Child Behavior Checklist; GEE, generalized estimating equations; ADHD, attention deficit hyperactivity disorder ; OR, odds ratio; CI, confidence interval.
Adjusted for maternal age, maternal education, maternal smoking in pregnancy, maternal smoking at age 5, maternal history of mental health problems at age 8 and family functioning at age 5 years.
p<0.05
p<0.005.
In assessing severity of asthma at age 5 and vulnerability to mental health problems, we found that across all disorders, mild asthma was not associated with an increased likelihood of problems from ages 5–17, when compared to those who did not have asthma (Table 4). However, moderate asthma was significantly associated with an increased odds for somatic and ADHD problems (p<0.05) and relationships were in the same direction though they did not reach statistical significance for other problems. Severe asthma was associated with increased odds of all disorders; these associations were just below statistical significance for severe asthma. Once again there were no significant interactions with age.
Table 4.
Relationship between severity and persistence of asthma and CBCL/DSM-IV problems from age 5–17
| Multivariate logistic GEE model (years 5–17 inclusivea) |
|||||||
|---|---|---|---|---|---|---|---|
| Affective problems |
Anxiety problems |
Somatic problems |
ADHD problems |
Oppositional defiant problems |
Conduct problems |
||
| Severity of asthma age 5 years | |||||||
| No asthma | |||||||
| OR | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |
| Mild asthma | |||||||
| OR | 0.91 | 1.22 | 1.16 | 1.52 | 1.18 | 1.32 | |
| 95% CI | 0.58–1.44 | 0.75–1.98 | 0.84–1.62 | 0.73–3.16 | 0.78–1.81 | 0.89–1.96 | |
| p value | 0.692 | 0.427 | 0.369 | 0.262 | 0.434 | 0.163 | |
| Moderate asthma | |||||||
| OR | 1.43 | 1.59 | 1.90** | 2.54* | 1.46 | 1.57 | |
| 95% CI | 0.85–2.41 | 0.90–2.79 | 1.30–2.77 | 1.16–5.58 | 0.87–2.44 | 0.94–2.62 | |
| p value | 0.179 | 0.108 | 0.001 | 0.020 | 0.151 | 0.086 | |
| Severe asthma | |||||||
| OR | 3.42** | 3.13** | 2.70** | 1.89 | 2.38** | 2.24** | |
| 95% CI | 2.29–5.10 | 1.98–4.95 | 1.93–3.79 | 0.84–4.27 | 1.56–3.64 | 1.48–3.39 | |
| p value | <0.001 | <0.001 | <0.001 | 0.126 | <0.001 | <0.001 | |
| Persistence of asthma age 5 years | |||||||
| No asthma | |||||||
| OR | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |
| Remitted asthma | |||||||
| OR | 1.20 | 1.45 | 1.06 | 2.34* | 1.34 | 1.29 | |
| 95% CI | 0.76–1.89 | 0.87–2.42 | 0.71–1.59 | 1.21–4.51 | 0.84–2.13 | 0.80–2.09 | |
| p value | 0.431 | 0.156 | 0.775 | 0.011 | 0.220 | 0.300 | |
| Later onset asthma | |||||||
| OR | 1.97** | 1.67* | 1.42* | 2.26* | 0.95 | 1.11 | |
| 95% CI | 1.38–2.81 | 1.05–2.65 | 1.04–1.94 | 1.11–4.62 | 0.61–1.49 | 0.76–1.62 | |
| p value | <0.001 | 0.030 | 0.030 | 0.025 | 0.822 | 0.583 | |
| Persistent asthma | |||||||
| OR | 2.26** | 2.64** | 2.41** | 2.63** | 1.92** | 1.91** | |
| 95% CI | 1.65–3.10 | 1.84–3.79 | 1.86–3.13 | 1.38–5.03 | 1.37–2.69 | 1.39–2.62 | |
| p value | <0.001 | <0.001 | <0.001 | 0.003 | <0.001 | <0.001 | |
CBCL, Child Behavior Checklist; GEE, generalized estimating equations; ADHD, attention deficit hyperactivity disorder ; OR, odds ratio; CI, confidence interval.
Adjusted for maternal age, maternal education, maternal smoking in pregnancy, maternal smoking at age 5, maternal history of mental health problems at age 8 and family functioning at age 5 years.
p<0.05
p<0.005.
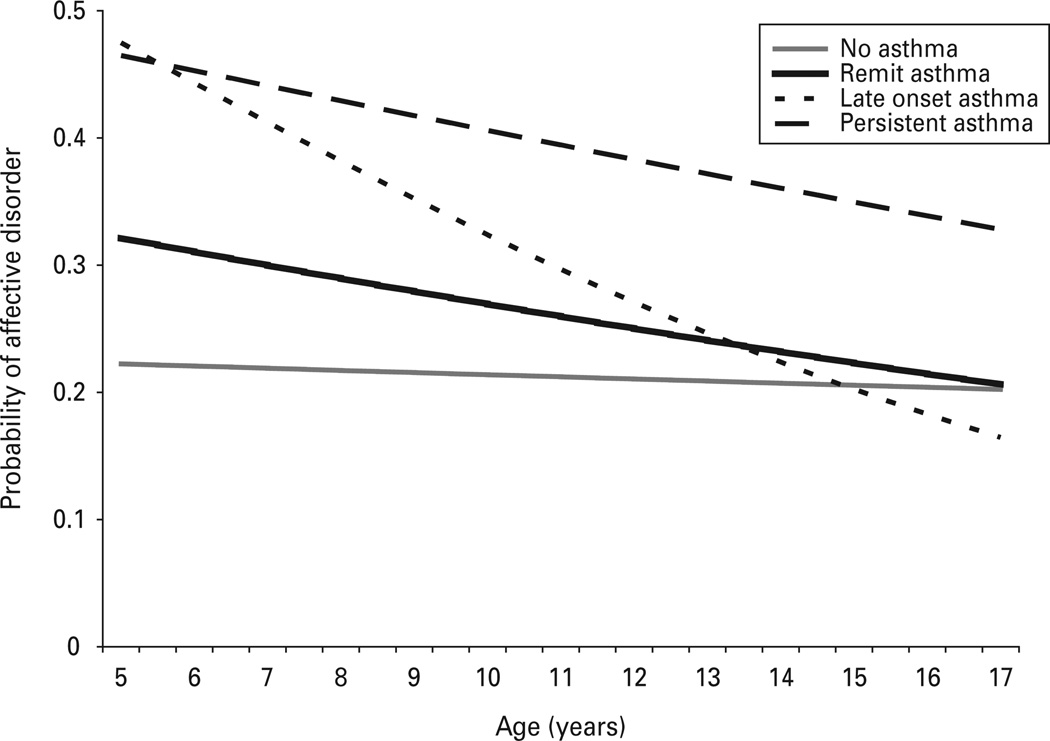
Our final analysis examined the impact of remitting versus later onset and persistent asthma, compared to no asthma at age 5 or wheezing at age 8 (Table 5). We found that with the exception of ADHD problems, there were no significant relationships between asthma at age 5 that had remitted by age 8 and vulnerability to mental health problems. There was a significant association between later onset asthma (i.e. recent wheezing at age 8) and internalizing problems (affective, anxiety and somatic problems), as well as ADHD but no significant relationships were observed between externalizing problems (oppositional defiant and conduct problems) following later onset asthma. There was a significant relationship between persistent asthma and all problem scales. We tested for age interaction effects and found a significant age interaction [adjusted for maternal age of 28 years (mean)] for the outcomes of affective, anxiety and ADHD problems, representing a decreasing likelihood of scoring above the clinical cut-point as age increased. Those with persistent asthma had around 33% probability of scoring above the cut-point by age 17 compared to 20% of participants with no asthma (Fig. 1; affective problems only, data for anxiety and ADHD problems not presented).
Fig. 1.
The probability of affective problems at each age for asthma onset and persistence groups.
Discussion
This study investigated the relationship between asthma at age 5 and vulnerability to the range of mental health problems from ages 5–17 among youth in Western Australia. We found that asthma at age 5 is significantly associated with both internalizing-type (e.g. affective, anxiety and somatic problems) and externalizing-type (e.g. ADHD, oppositional defiant and conduct problems) disorders among young persons. To our knowledge, this study is the first to examine the impact of asthma severity and persistence on mental health over time from ages 5–17 in a representative, population-based sample. Our findings suggest that likelihood of mental health problems among youth with asthma increases as the severity of asthma increases. The relationship does not appear to be statistically significant among those with mild asthma. Further, the relationship between persistent asthma and mental health problems is strong while asthma at age 5 that has remitted by age 8 does not appear to be associated with any greater vulnerability to mental health problems, compared to those who never had asthma. This vulnerability appears to be most prominent earlier in childhood but decreases with age.
Our results confirm and extend previous findings of a link between asthma and anxiety disorders among youth by demonstrating a relationship between asthma and both internalizing and externalizing problems into adolescence. Specifically, we found a significant relationship between asthma and conduct problems and oppositional defiant problems. Findings in the literature have been inconsistent on this association: Ortega et al. (2004) detected an association between parent-reported lifetime diagnosis of asthma and any disruptive disorder (OR 1.6, 95% CI 1.1–2.3) and asthma attack and oppositional defiant disorder [odds ratio (OR) 1.9, 95% confidence interval (CI) 1.2–3.0] among Puerto Rican children. Yet, the same study found no association between hospitalization for asthma and disruptive disorders (Ortega et al. 2004) and Ortega et al. (2003) found no significant association between parent-reported lifetime asthma and disruptive disorders among youth in US community samples. Further, Alati et al. (2005) found no relationship between asthma at age 5 and externalizing disorders in a birth cohort in Brisbane, Australia. The reason for these discrepancies is not clear. It could be due to differences in sample size, sample composition and/or measurement of asthma. We also found an association between asthma and ADHD, which is consistent with several previous studies (Ortega et al. 2004; Goodwin et al. 2005a). The association was not statistically significant in the severe range, although it was in all others and this may have been due to low sample size as we had a very small number of participants with ADHD, potentially due to the stringent cut-off points for ADHD problems using DSM-IV-oriented scales. Remitted asthma was not associated with any mental disorders with the exception of ADHD. The reason for this specific association is not known but should be investigated further. Previous clinical studies have also found relationships between asthma and other externalizing-type/disruptive behaviors (McQuaid et al. 2001) suggesting that the overall weight of evidence to date supports an association between asthma and both internalizing and externalizing problems.
To our knowledge, this is the first study to examine the relationship between asthma and mental disorders among youth using both detailed report on the severity and persistence of asthma and standardized, well-validated measures of mental health. Several previous population-based studies have been performed using data from surveys that were designed primarily to study mental health, and as such included comparatively weaker and/or vague measures of physical health. Therefore, findings from the current study add to the literature in this area by providing new evidence indicating that it does not appear to be the case that any asthma in youth is associated with increased risk of mental health problems. Instead, the extent to which youth with asthma are vulnerable to mental health problems appears closely related to the severity and persistence of asthma. One major limitation, however, with this finding is that ‘severe’ asthma cannot necessarily be distinguished from ‘poorly controlled’ asthma. Rather, they are potentially interchangeable here as we do not have measures of physical severity of asthma (versus the degree to which asthma is well controlled), nor do we have detailed data on asthma medicine use. As such, it is conceivable that the relationship between severe asthma and mental health problem emerges because youth with mental health problems do not manage their asthma well, potentially in part, because of mental health problems. Therefore, asthma of the same level of physiological severity – when it occurs in a young person who has depression – may be poorly controlled and therefore present as severe asthma while in a young person who does not have depression, the asthma is well managed and may appear mild. Another possibility is that a third variable, such as childhood abuse or neglect could lead to the co-occurrence of mental disorders and asthma, as it is independently associated with each (Goodwin et al. 2004); however, there is some evidence that childhood adversity alone does not account for the association between asthma and depression/anxiety in adults (Scott et al. 2008). Future studies aimed at untangling the relationship between mental health problems and asthma control/asthma morbidity over time are needed.
As results of previous studies have suggested that asthma early in life is associated with increased vulnerability to mental health problems in young persons, a common question has been whether this increased risk applies to youth who ‘outgrow’ asthma. Childhood asthma remits by early adulthood in a substantial percentage of those who have been diagnosed early in childhood (Martinez et al. 1998; Morgan et al. 2005; Stern et al. 2008). Our findings suggest that indeed youth with asthma that remits in childhood do not appear to be at any greater risk for mental health problems, with the exception of ADHD, than those who never had asthma. The finding that ADHD is the only disorder elevated among those with remitted asthma deserves further study. Yet, overall, this result suggests that contrary to what the bulk of studies have concluded based on the available data in these studies (i.e. that youth with any lifetime asthma are at risk for mental disorders), this is not the case. Therefore, screening or special attention to all youth with any lifetime asthma is not necessarily warranted. Rather, those with persistent asthma (at least as best we could measure this that persists from ages 5–8) do indeed seem somewhat more vulnerable to a range of mental health problems and therefore it is this group who should be watched closely and screened. This information may be useful to clinicians who treat children with asthma in general and specialty pediatric settings because these data provide somewhat compelling evidence that youth with persistent asthma may be more vulnerable to mental health problems. Of interest, we found that the probability of affective problems decreased with age for youth with any asthma – potentially suggesting that risk of affective problems may in some way be related to asthma at earlier ages. Although at older ages (late adolescence), the risk of affective disorders (but not anxiety or ADHD) was still comparatively elevated among those with persistent asthma.
In addition to those already mentioned, there are several limitations to our study that should be considered when interpreting the results. First, though detailed and validated measures were used, we relied on parental report for both asthma and mental health problems. It is conceivable that this could bias findings as separate reporters for each is preferable. Yet, it has been demonstrated that with children of this age, parental report of behavior should be fairly robust (Warnick et al. 2008) and in a large-scale community-based study, parental response to detailed questions regarding physician-diagnosed asthma is the most robust criteria. Second, measurement of asthma for age 8 included wheeze at one time point and asthma at another. While it is true that current wheezing (at least one episode in the past 12 months) is more common that current asthma as children get older, the likelihood that those with current wheeze have asthma and most likely persistent asthma increases. As such, the difference in assessment at the two ages is unlikely to make a major difference to our findings. Third, Western Australia is a westernized country similar in many ways to Western Europe and the USA, yet it is possible that the results may have limited generalizability to other countries. Replication of these findings with youth from diverse settings would be useful. Fourth, we were not able to control for all possible confounding factors in the relationship between asthma and mental health problems.
Recent findings suggest that youth with asthma may have specific, unique needs for social/emotional support to cope effectively with the demands of their illness and their limitations, and that these are not routinely considered in clinical practice (Stewart et al. 2011). These findings suggest it would be important to examine whether and to what degree specific interventions aimed at supporting youth in their management of chronic illness, especially among those with severe and persistent disease, may help to reduce mental health problems in this population. Such randomized clinical trials will also help to establish causality. Recent studies in adults show that effective control of asthma is associated with fewer mental health problems in clinical settings (Kardos et al. 2011; Vieira et al. 2011), compared to uncontrolled asthma. It is therefore possible that screening and provision of mental health services for youth with asthma – as appropriate – could lead to better asthma control over the long term. It may also be that interventions that help children and families to better control the child’s asthma may assist in reducing a child’s future risk of mental health problems.
Acknowledgments
We acknowledge the support via core funding from the Raine Medical Research Foundation, The University of Western Australia (UWA), the Telethon Institute for Child Health Research, the UWA Faculty of Medicine, Dentistry and Health Science, the Women and Infants Research Foundation and Curtin University. The Raine Study is also funded by the National Health and Medical Research Council of Australia (NHMRC; grant nos. 963209, 211912, 003209 and 353514), Australian Health Management, the Telstra Foundation, the Western Australian Health Promotion Foundation, the National Heart Foundation of Australia and Beyond Blue. Dr Robinson is funded by Australian Rotary Health. Work was supported in part by NIH grant nos. MH64736 and DA20892 to Dr Goodwin. We are extremely grateful to all the families who took part in this study and the Raine Study team, which includes data collectors, cohort managers, data managers, clerical staff, research scientists and volunteers.
Footnotes
Declaration of Interest
None.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM. CBCL DSM-Oriented Scales. Burlington, VT: ASEBA; 2001. [Google Scholar]
- Alati R, O’Callaghan M, Najman JM, Williams GM, Bor W, Lawlor DA. Asthma and internalizing behavior problems in adolescence: a longitudinal study. Psychosomatic Medicine. 2005;67:462–470. doi: 10.1097/01.psy.0000161524.37575.42. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders – Revised (DSM-IV-R) Washington: American Psychiatric Association; 2000. [Google Scholar]
- Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: reliability and validity of the General Functioning subscale of the McMaster Family Assessment Device. Family Process. 1988;27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- Delmas MC, Guignon N, Chan Chee C, Fuhrman C, Herbet JB, Gonzalez L. Asthma and major depressive episode in adolescents in france. Journal of Asthma. 2011;48:640–646. doi: 10.3109/02770903.2011.585410. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital & Family Therapy. 1983;9:171–180. [Google Scholar]
- Federico MJ, Wamboldt FS, Carter R, Mansell A, Wamboldt MZ. History of serious asthma exacerbations should be included in guidelines of asthma severity. Journal of Allergy and Clinical Immunology. 2007;119:50–56. doi: 10.1016/j.jaci.2006.10.019. [DOI] [PubMed] [Google Scholar]
- Feldman JM, Ortega AN, McQuaid EL, Canino G. Comorbidity between asthma attacks and internalizing disorders among Puerto Rican children at one-year follow-up. Psychosomatics. 2006;47:333–339. doi: 10.1176/appi.psy.47.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Asthma and depressive and anxiety disorders among young persons in the community. Psychological Medicine. 2004;34:1465–1474. doi: 10.1017/s0033291704002739. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Archives of General Psychiatry. 2003a;60:1125–1130. doi: 10.1001/archpsyc.60.11.1125. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Lewinsohn PM, Seeley JR. Cigarette smoking and panic attacks among young adults in the community: the role of parental smoking and anxiety disorders. Biological Psychiatry. 2005a;58:686–693. doi: 10.1016/j.biopsych.2005.04.042. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Messineo K, Bregante A, Hoven CW, Kairam R. Prevalence of probable mental disorders among pediatric asthma patients in an inner-city clinic. Journal of Asthma. 2005b;42:643–647. doi: 10.1080/02770900500264770. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Pine DS, Hoven CW. Asthma and panic attacks among youth in the community. Journal of Asthma. 2003b;40:139–145. doi: 10.1081/jas-120017984. [DOI] [PubMed] [Google Scholar]
- Joseph-Bowen J, de Klerk NH, Firth MJ, Kendall GE, Holt PG, Sly PD. Lung function, bronchial responsiveness, and asthma in a community cohort of 6-year-old children. American Journal of Respiratory and Critical Care Medicine. 2004;169:850–854. doi: 10.1164/rccm.200304-556OC. [DOI] [PubMed] [Google Scholar]
- Kardos P, Wittchen HU, Muhlig S, Ritz T, Buhl R, Rabe K, Klotsche J, Riedel O. Controlled and uncontrolled allergic asthma in routine respiratory specialist care – a clinical-epidemiological study in Germany. Current Medical Research and Opinion. 2011;27:1835–1847. doi: 10.1185/03007995.2011.606805. [DOI] [PubMed] [Google Scholar]
- Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. Journal of Adolescent Health. 2007;41:455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez FD, Stern DA, Wright AL, Taussig LM, Halonen M. Differential immune responses to acute lower respiratory illness in early life and subsequent development of persistent wheezing and asthma. Journal of Allergy and Clinical Immunology. 1998;102:915–920. doi: 10.1016/s0091-6749(98)70328-8. [DOI] [PubMed] [Google Scholar]
- McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. General Hospital Psychiatry. 2007;29:214–222. doi: 10.1016/j.genhosppsych.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. Journal of Developmental & Behavioral Pediatrics. 2001;22:430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- Morgan WJ, Stern DA, Sherrill DL, Guerra S, Holberg CJ, Guilbert TW, Taussig LM, Wright AL, Martinez FD. Outcome of asthma and wheezing in the first 6 years of life: follow-up through adolescence. American Journal of Respiratory and Critical Care Medicine. 2005;172:1253–1258. doi: 10.1164/rccm.200504-525OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison KM, Goli A, Van Wagoner J, Brown ES, Khan DA. Depressive symptoms in inner-city children with asthma. Prim Care Companion to the Journal of Clinical Psychiatry. 2002;4:174–177. doi: 10.4088/pcc.v04n0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Asthma Council Australia. Asthma Management Handbook 2006. Melbourne: National Asthma Council Australia; 2006. [Google Scholar]
- Newnham JP, Evans SF, Michael CA, Stanley FJ, Landau LI. Effects of frequent ultrasound during pregnancy: A randomised controlled trial. Lancet. 1993;342:887–891. doi: 10.1016/0140-6736(93)91944-h. [DOI] [PubMed] [Google Scholar]
- NHLBI. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. National Heart, Lung and Blood Institute: National Institutes of Health; 2007. [Google Scholar]
- Ortega AN, Huertas SE, Canino G, Ramirez R, Rubio-Stipec M. Childhood asthma, chronic illness, and psychiatric disorders. Journal of Nervous and Mental Disease. 2002;190:275–281. doi: 10.1097/00005053-200205000-00001. [DOI] [PubMed] [Google Scholar]
- Ortega AN, McQuaid EL, Canino G, Goodwin RD, Fritz GK. Comorbidity of asthma and anxiety and depression in Puerto Rican children. Psychosomatics. 2004;45:93–99. doi: 10.1176/appi.psy.45.2.93. [DOI] [PubMed] [Google Scholar]
- Ortega AN, McQuaid EL, Canino G, Ramirez R, Fritz GK, Klein RB. Association of psychiatric disorders and different indicators of asthma in island Puerto Rican children. Social Psychiatry and Psychiatric Epidemiology. 2003;38:220–226. doi: 10.1007/s00127-003-0623-6. [DOI] [PubMed] [Google Scholar]
- Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. General Hospital Psychiatry. 2008;30:398–406. doi: 10.1016/j.genhosppsych.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KM, Von Korff M, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, Haro JM, Kessler RC, Kovess V, Ono Y, Ormel J, Posada-Villa J. Childhood adversity, early-onset depressive/anxiety disorders, and adult-onset asthma. Psychosomatic Medicine. 2008;70:1035–1043. doi: 10.1097/PSY.0b013e318187a2fb. [DOI] [PubMed] [Google Scholar]
- Stern DA, Morgan WJ, Halonen M, Wright AL, Martinez FD. Wheezing and bronchial hyper-responsiveness in early childhood as predictors of newly diagnosed asthma in early adulthood: a longitudinal birth-cohort study. Lancet. 2008;372:1058–1064. doi: 10.1016/S0140-6736(08)61447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart M, Masuda JR, Letourneau N, Anderson S, McGhan S. ‘I want to meet other kids like me’: support needs of children with asthma and allergies. Issues in Comprehensive Pediatric Nursing. 2011;34:62–78. doi: 10.3109/01460862.2011.572638. [DOI] [PubMed] [Google Scholar]
- Vieira AA, Santoro IL, Dracoulakis S, Caetano LB, Fernandes AL. Anxiety and depression in asthma patients: impact on asthma control. Jornal Brasileiro de Pneumologia. 2011;37:13–18. doi: 10.1590/s1806-37132011000100004. [DOI] [PubMed] [Google Scholar]
- Wamboldt MZ, Hewitt JK, Schmitz S, Wamboldt FS, Rasanen M, Koskenvuo M, Romanov K, Varjonen J, Kaprio J. Familial association between allergic disorders and depression in adult Finnish twins. American Journal of Medical Genetics. 2000;96:146–153. doi: 10.1002/(sici)1096-8628(20000403)96:2<146::aid-ajmg4>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Warnick EM, Bracken MB, Kasl S. Screening efficiency of the Child Behavior Checklist and Strengths and Difficulties Questionnaire: a systematic review. Child and Adolescent Mental Health. 2008;13:140–147. doi: 10.1111/j.1475-3588.2007.00461.x. [DOI] [PubMed] [Google Scholar]
- Zubrick S, Silburn S, Gurrin L, Teoh H, Shepherd C, Carlton J, Lawrence D. Australian Bureau of Statistics and the Telethon Institute for Child Health Research. Perth, Western Australia: 1997. Western Australian Child Health Survey: education, health and competence. [Google Scholar]