Abstract
Purpose
Children with disabilities are two to three times more likely to become overweight or obese than typically developing children. Children with spina bifida (SB) are at particular risk, yet obesity prevalence and weight management with this population are under-researched. This retrospective chart review explored how weight is assessed and discussed in a children’s SB outpatient clinic.
Method
Height/weight data were extracted from records of children aged 2–18 with a diagnosis of SB attending an outpatient clinic at least once between June 2009–2011. Body mass index was calculated and classified using Centers for Disease Control and Prevention cut-offs. Notes around weight, diet and physical/sedentary activities were transcribed verbatim and analysed using descriptive thematic analysis.
Results
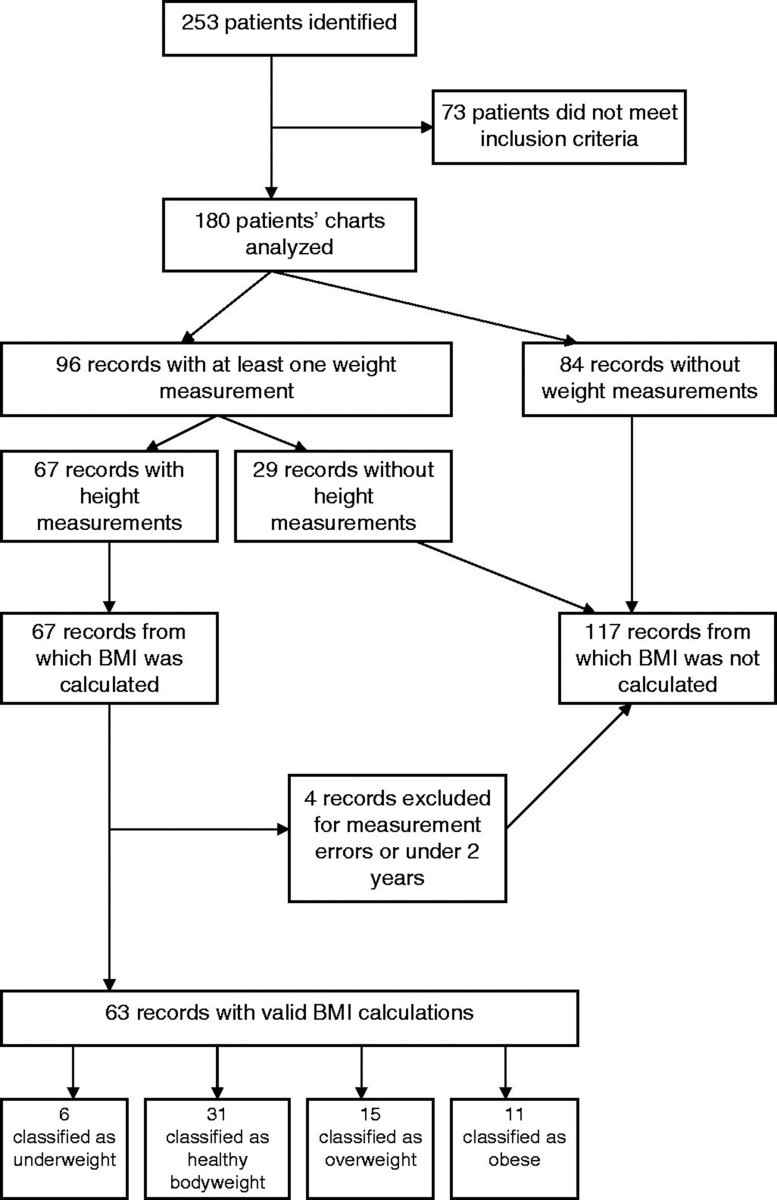
Of 180 eligible patients identified, only 63 records had sufficient data to calculate BMI; 15 patients were overweight (23.81%) and 11 obese (17.46%). Weight and physical activity discussions were typically related to function (e.g. mobility, pain). Diet discussions focused on bowel and bladder function and dietary challenges.
Conclusions
Anthropometrics were infrequently recorded, leaving an incomplete picture of weight status in children with SB and suggesting that weight is not prioritised. Bowel/bladder function was highlighted over other benefits of a healthy body weight, indicating that health promotion opportunities are being missed.
Implications for Rehabilitation
It is important to assess, categorise and record anthropometric data for children and youth with spina bifida as they may be at particular risk of excess weight.
Information around weight categorisation should be discussed openly and non-judgmentally with children and their families.
Health promotion opportunities may be missed by focusing solely on symptom management or function.
Healthcare professionals should emphasise the broad benefits of healthy eating and physical activity, offering strategies to enable the child to incorporate healthy lifestyle behaviours appropriate to their level of ability.
Keywords: Children, obesity, spina bifida
Introduction
Childhood obesity is a global concern [1] and has been called one of the greatest health problems of the twenty-first century [2]. Children with disabilities are particularly vulnerable, as estimates suggest that the prevalence of overweight and obesity is two to three times that of their typically developing peers [3–5]. Life expectancy for many children with disabilities has vastly increased in recent years [5–7], yet this progress may be compromised by the increasing prevalence of overweight and obesity [8].
Children with disabilities are at risk of the same negative consequences of obesity as typically developing children; high blood pressure, type 2 diabetes mellitus, atherosclerosis, non-alcoholic fatty liver disease and sleep apnoea are all potential short-term conditions with long-term health consequences [9–11]. Skin problems, respiratory difficulties, muscle and joint pain and gastrointestinal problems may also contribute to life-threatening conditions such as heart disease, stroke and respiratory disorders later in life [6,12,13]. However, these negative consequences are compounded for children with existing disabilities, as they are also at risk of secondary conditions and symptoms such as extreme muscle loss, pain, pressure sores, mobility limitations and depression [14,15], potentially hindering independence and participation in the community and limiting leisure and physical activities [3,5,16].
Despite the widespread use of folic acid supplements, spina bifida (SB) remains one of the most common congenital conditions [17], with a prevalence of 4.1 affected children per 10 000 births in Canada (8.6 per 10 000 births for all neural tube defects) [18]. The condition commonly causes lower body muscle weakness or paralysis as well as a degree of bladder/bowel dysfunction, depending upon the level of the lesion, and can result in significant morbidity [19]. The life-expectancy of people with SB has increased and it is now considered a non-progressive, life-long condition [17,20–24]. However, this brings new challenges around health promotion and providing optimal healthcare [23–25], particularly around weight management. Overweight and obesity can further reduce mobility, increase difficulties with catheterisation, toileting and other self-care activities, add pressure on skin already vulnerable to break-down/pressure sores and increase social isolation, which can all lead to decreased quality of life and low self-confidence [6,26–28]. This can then become a negative spiral where children are excluded from opportunities, which compounds low self-esteem, which acts as a barrier to participation and disables them further, exacerbating any weight-related issues [29].
The prevalence of obesity in young people with SB has been estimated between 18 and 50% in children, and 34% and 64% in young people [26,30]. However, many of these figures have been taken from studies well over 15 years old [31–33]. Given the recent dramatic increase in obesity in typically developing children, these figures may under-estimate the magnitude of the problem in children with SB today. Children and young people with SB have physiological, environmental, psychosocial and physical factors which predispose them to overweight/obesity. For example, mobility impairments can result in sedentary lifestyles and reduced physical fitness [24,30]. Environmental and psychological factors, such as a lack of facilities, special equipment and trained fitness staff [11], and a lack of understanding regarding capabilities [2,4,15] may also play a role. Furthermore, awareness and attention to obesity in this population may be lacking; for example, issues such as bowel function may be more salient to children, parents and healthcare professionals [6,17,27,34]. Underlying brain malformations (e.g. Chiari II) can also cause problems with swallowing and gagging, limiting food intake to specific tastes or textures [26].
Both the Canadian Pediatric Society [35] and American Academy of Pediatrics [36] advocate that all typically developing children aged 2 years and older should have their growth monitored to screen for under-development, wasting, overweight and obesity. Current guidelines by the Centers for Disease Control and Prevention (CDC) use body mass index (BMI, calculated as kilograms per metre squared) as a proxy for body fat and consider a child 2–18 years between the 85–95th centile as overweight and above the 95th centile as obese [37]. Visits to healthcare professionals – whether or not for a weight-related matter – offer an ideal opportunity for such monitoring. However, evidence suggests that the assessment and recording of children’s weight and BMI by healthcare professionals varies enormously [38–41]. Furthermore, assessment of weight and growth alone is insufficient in improving children’s health if it is not discussed with the child and their family [35,42].
This issue is arguably even more important for children with SB, given their increased risk of obesity. Their regular interactions with a multidisciplinary healthcare team potentially provide great opportunities for weight assessment, monitoring and working with families to optimise their child’s health through healthy weight management [17,21].
Research gap
Children with SB may be particularly predisposed to overweight and obesity, yet there are gaps in the literature around the prevalence of obesity in paediatric SB populations. Little is known about how weight management and weight status are recorded and discussed in the outpatient clinic setting. The objectives of this study were to explore how the weight status of children attending an outpatient SB clinic in a paediatric rehabilitation hospital is recorded and how weight-related behaviours are discussed with children and their families. This is vital in order to understand the health promotion needs of a population vulnerable to developing serious secondary conditions which may limit their health and full participation in life.
Research questions
Are height and weight routinely recorded for children attending an outpatient SB clinic?
What proportion of clinic attendees are overweight or obese?
How are discussions of weight-related behaviours with children and families recorded?
Methods
Design
A retrospective medical records review (MRR) was used. Despite some concerns about the reliability of data extraction from medical records [43], MRRs can be advantageous as they do not influence clinical practice by observing the consultation [44] and it is a time-efficient method of collecting a large amount of data [45]. However, the researcher is reliant upon clinicians accurately recording the information in the medical records [45]. Despite these noted limitations, MRR methodology has been successfully used in reviewing how physicians both evaluate and manage obesity in typically developing children in primary care [46].
Sampling
The sample was drawn from the largest urban paediatric rehabilitation centre in Canada. The SB clinic consists of an inter-professional team with representation from orthopaedic surgery, urology, developmental behavioural paediatrics, nursing, physiotherapy, occupational therapy, speech therapy, psychology and social work. Members of the team assess the children individually and consult with other team members as needed; formal review of each patient is completed following the clinic. In addition, the clinic has access to consultation with separate services located within the centre, including recreational therapy specialists and registered dieticians.
Medical records were included in the review if children (1) had a coded diagnosis of SB (spina bifida aperta, occult spinal dysraphism); (2) had attended the clinic in the previous 24 months; and (3) were aged 2–18 years. Records were excluded if children had a diagnosis of spina bifida occulta or traumatic spinal cord injury or it was their first visit to the clinic, as they were unlikely to be representative of the target population.
All data available for an individual over the previous 36 months were examined. This time-frame allowed for seasonal and minor variations [47] and included children who visited the clinic infrequently. The age range of 2–18 years was selected due to published international cut-off points for BMI for that age range (albeit for able-bodied children) [37].
Data extraction
Ethical approval was obtained from the Hospital Research Ethics Board. As a standardised data extraction form was not available, one was designed for the purpose of this study and incorporated items from the literature wherever possible – this included questions on diet and physical activity that were taken from a previous MRR of obesity in children without disabilities [46]. Recording of lesion level, ambulatory and shunt status was taken from prospective studies of physical fitness in children and young people with SB [23,30,48]. Height and weight were also recorded on this form. Records were read carefully and all comments relating to weight, diet, physical and sedentary activities were transcribed verbatim. A “history” (e.g. diet, physical activity) was identified when a clinician recorded patients’ responses to open-ended questions about their usual dietary intakes, or the nature and extent of physical and sedentary activities. These were presented in narrative form. A copy of the extraction form is available from the first author upon request.
Reliability of data extraction
All data were extracted by a single member of the research team (EY). To evaluate the reliability of extraction, a second researcher (AM) independently extracted data from 10% (n = 18) randomly selected medical records. For quantitative data, Kappa co-efficients were calculated to assess agreement between extractors. Reliability of the qualitative data was calculated by the number of matching verbatim extracts identified by each of the two extractors for the same 18 records, expressed as a proportion of the total number of extracted sections. To guard against significant transcription errors [49], another randomly selected 10% records were checked by the second researcher for the accuracy of data entry, with an acceptable error rate considered to be <1% [50].
Data analysis
Descriptive statistics using SPSS Statistics 19.0 (SPSS, Chicago, IL) were used to summarise patient demographics and background details, such as age, gender and diagnosis. BMI was calculated as kilograms per metre squared (kg/m2) and children’s weight status classified using CDC cut-offs of <85th centile = healthy weight, 85–95th centile = overweight and >95th centile = obese [37]. Exploratory analysis was conducted using age, gender, weight status and the presence of documented weight-related discussions. Statistical significance was accepted as p < 0.05.
Qualitative data from the verbatim extracts in all records were subjected to descriptive thematic analysis, which aims to identify, analyse and describe patterns within qualitative data [51]. Extracts were initially grouped under “weight”, “diet” and “physical/sedentary activities”. Two of the authors (AM and EY) then independently used inductive coding with an interpretative perspective in order to create codes. Once common codes/themes were developed by each author, they were compared and contrasted, merged, relabeled or split as necessary. Negative cases, similarities and differences between codes were also discussed between the researchers.
Results
Reliability
When Kappa co-efficients were calculated for the two raters on 10% (n = 18) of cases in terms of extracting weight and height data from the records, values of 0.80 for weight and 0.83 for height were obtained. Verbatim extracts for the same 18 charts were also compared to assess consistency in the extraction of qualitative data. On average, the two extractors extracted the same excerpts 84.7% of the time relating to physical activity and 73.3% of the time for weight and diet, exceeding the co-efficient of ≥0.7 which indicates adequate reliability [52].
Sample characteristics
A total of 253 patients were identified, 73 of which did not meet the inclusion criteria, leaving 180 included in the analysis. Of these 180 medical records, approximately half were females (n = 94, 52.2%). A primary diagnosis for a large proportion of individuals was myelomeningocele (n = 133; 73.9%), followed by lipomyelomeningocele (n = 38; 21.1%) and 9 (5%) with other related conditions. Patients frequently had additional diagnoses recorded in their notes, which are summarised in Table 1. Patients ranged in age from 2 to 18 years (mean = 12.39 ± 4.79). The average length of time since the patient had registered at the SB outpatient clinic was 10.61 ± 5.41 years. The average number of visits to this clinic in the previous 36 months was 3.77 ± 2.01. Characteristics of the sample can be found in Table 1.
Table 1.
Sample characteristics.
| N (%) | |
|---|---|
| Lesion level [23] | |
| High level (L2 and above) | 49 (27.2%) |
| Middle (L3–L5) | 85 (47.2%) |
| Low (S1 and below) | 43 (23.9%) |
| Unknown | 3 (1.7%) |
| Ambulation* [48] | |
| Community ambulatory | 101 (56.1%) |
| Household ambulatory | 21 (11.7%) |
| Non-functional ambulatory | 2 (1.1%) |
| Non-ambulatory | 50 (27.8%) |
| Unknown | 6 (3.3%) |
| Hydrocephalus status | |
| Shunted hydrocephalus | 106 (58.9%) |
| Non-shunted hydrocephalus | 2 (1.1%) |
| No hydrocephalus | 71 (39.4%) |
| Primary diagnoses | |
| Myelomeningocele | 133 (73.9%) |
| Lipomeningocele | 38 (21.1%) |
| Other | 9 (5%) |
| Secondary diagnoses | |
| Neurogenic bladder | 108 (60.0%) |
| Neurogenic bowel | 56 (31.1%) |
| Arnold Chiari II malformation | 36 (20.0%) |
| Depression | 36 (20.0%) |
| Scoliosis | 43 (23.9%) |
| Tethered cord | 12 (6.7%) |
| Obesity/weight issues | 5 (2.8%) |
| Club foot | 23 (12.8%) |
| Developmental delay | 14 (7.8%) |
| Learning disability | 4 (2.2%) |
| ADHD | 15 (8.3%) |
| Medications | |
| None | 36 (20%) |
| Anti-cholinergic | 109 (60.6%) |
| Antibiotic (inc prophylaxis) | 68 (37.8%) |
| Stool softener/laxative | 58 (32.2%) |
| Anti-seizure | 10 (5.6%) |
| Other | 32 (17.8%) |
Community ambulatory = walks indoors and outdoors; household ambulatory = walk only indoors; non-functional ambulatory = only walks during therapy sessions; non-ambulatory = always in wheelchair [48].
Recording of weight, height and weight status
Of the 180 children included in this review, 96 had a weight recorded in their medical records at least once (53.3%). However, only 67 of the 180 children had both weight and height recorded in their notes at least once (37.2%), enabling calculation and classification of BMI. On average, these 67 children had weight and height recorded in under half of their visits they had made to the SB clinic (42.4%). There were no significant differences in whether both weight and height were recorded on at least occasion by gender or ambulatory status.
Of the 67 children with both weight and height measurements, 63 children (35%) could have their BMI categorised using the CDC-2000 classification system (2 children only had measurements taken under 2 years of age, while 2 other children had measurements with obvious errors such as a 5-year-old with a height of 1.5 m). From them, 15 (23.8%) were classified as overweight for at least one time point, while 11 (17.5%) could be classified as obese and 6 (9.5%) were classified as underweight (Figure 1).
Figure 1.
Flow of medical records.
Weight and height were recorded in half of the visits the overweight/obese children had made to the clinic (53.5%), but only 6 out of these 26 children classified as overweight or obese were explicitly identified as having excess weight in their notes (23.1%). Conversely, five children were described as overweight or obese in their records, but no data on weight and height were provided, including one described as being “morbidly obese” (#108). In addition, discussions specifically about weight and weight management were only recorded in the notes of 7 (26.9%) children classified as overweight or obese. Of those classified as overweight or obese, 46.2% were non-ambulatory, 23.1% household ambulatory and 30.8% were classified as community ambulatory (see Table 1 legend for definitions of ambulatory status).
Recording of diet, physical activities and sedentary behaviour
In the full sample (n = 180), a diet history had been recorded on at least one occasion in 113 of the charts (62.8%). A physical activity history was present in 115 (63.9%) charts whilst a sedentary behaviour history was recorded in only 30 charts (16.7%).
Discussions about diet and documentary advice were documented in 59 of the 180 records (32.8%) while 36 charts reported discussions around physical activity levels and advice given (20.0%). Advice about reducing sedentary behaviours – such as screen time – did not appear in any of the charts.
In the 26 children classified as overweight or obese, diet histories were frequently recorded (n = 22, 84.6%), while physical activity histories (n = 18, 69.2%) were more common than sedentary activity histories (n = 3, 11.5%).
Qualitative themes
Qualitative themes identified from the verbatim transcribed comments taken from the 180 charts were the following: (1) The importance of weight management in mitigating symptoms and optimising function; (2) dietary priorities and motivations; (3) physical and sedentary activities: friend or foe; (4) weight management, diet and physical activity: whose responsibility? The following quotes taken from the records illustrate each of the themes. The healthcare professional or discipline of the person recording the data, child ID number, child age and their weight status (if able to be calculated) are included in parentheses at the end of each quote.
The importance of weight management in mitigating symptoms and optimising function
Healthcare professionals discussed the immediate impact of the person’s weight with the patient and family. This was often in terms of mobility or ambulation, usually that a reduction of weight would improve functional difficulties they were currently experiencing: “Patient’s mobility has become a little more laboured, likely from her weight gain as she has gotten older” (Physiotherapist, #169, 14 years, healthy weight).
This emphasis on function was also reflected in discussions around continence, discussing the importance of a healthy weight in order to reduce unpleasant symptoms and improve surgical options:
In terms of her urinary leakage, we had a long discussion on the impact of patient’s weight on the pelvic floor function. I discussed with mother that this in of itself may be a contributing factor to some of this… I think weight loss will be critical to her overall function. (Paediatrician, #106, 15 years, no Height & Weight [H&W])
Similarly, weight loss was linked to positive improvements in symptoms:
Her symptoms have improved dramatically with an 8-pound weight loss… Physical exam reveals a moderately obese young woman but she does appear to have lost weight…From a medical standpoint, I am very pleased to hear that her symptoms are improving with weight loss. (Paediatrician, #106, 15 years, no H&W)
The future implications of excess weight were also highlighted, for example:
I am more concerned about the future rather than in the immediate year or two, but it is important that he loses weight. (Nutrition clinic, #16, 13 years, obese [OB])
Its contribution to caregiver burden was noted, especially as many patients required assistance with activities of daily living involving significant physical exertion:
We addressed that patient is somewhat overweight … he is getting bigger and heavier and more difficult to deal with in terms of daily activities for his mother. (Orthopaedist, #54, 14 years, overweight [OW])
The most common weight management strategy discussed was physical activity, for example:
We encouraged Mom to increase physical activity as much as possible, even if she should continue using her wheelchair at school, which is the manual wheelchair, which still allows her to do some exercise. (Nutrition clinic, #151, 7 years, OB)
Occasionally, this was discussed in conjunction with diet, such as: “Adding more fruits and vegetables to her diet may help her feel full without adding many calories, and increasing her activity as tolerated may also be helpful” (Nursing, #145, 18 years, no H&W).
Dietary priorities and motivations
Diet was most commonly discussed with respect to bowel and bladder functioning as opposed to weight management. Conversely, bowel and (to a lesser extent) bladder function was also considered as an indicator of the quality of the child’s diet. For example, these two extracts illustrate how bowel movements were discussed in relation to what the patient ate and drank:
Patient has a bowel movement every 2 days. This is an improvement since her last visit, and Mom reports that this is due to her increase in fiber and fluids, as well as the use of probiotics. (Nursing, #69, 13 years, healthy weight) From a bowel standpoint, he is continent and this is all through diet control. There are no problems. He is able to identify dietary exacerbants. (Paediatrician, #31, 14, no H&W)
It was apparent that parents and children used diet to manage the child’s bowel and bladder function, for example, using specific foods to prevent and “treat” constipation:
Mom reports that they have noticed softer, more frequent bowel movements with patient when he has eaten fruits and vegetables. Conversely, candy and chocolate produces constipation. (Nursing, #129, 14 years, underweight)
The discussions about improving dietary habits predominantly surrounded fiber and water intake. One record addressed the broad benefits of water to health: “We encouraged patient to increase her water intake to keep her overall health at an optimum level, as well as to keep her bladder and bowel status healthy” (Nursing, #126, 16 years, no H&W), but it was more usual for healthcare professionals to use bowel and bladder function as the sole motivator to follow a balanced diet, rather than promoting nutritional balance or a healthy bodyweight:
Writer tried to explain that if patient could drink more water and try to eat some apples and vegetables, that it would possibly help him go to the bathroom and it would not be so painful. (Nursing, #10, 9 years, OW)
While diet was emphasised for bowel health, fluid intake was linked to bladder function. Fluid intake by children was consistently reported as being poor, so practical and creative ways were suggested to improve the patients’ fluid intake, such as adding pieces of fruit to improve the taste of water:
I encouraged patient to try to replace his huge intake of apple juice with more water, even if this involves having to dilute the apple juice on a sliding scale over time to increase water intake. (Nursing, #116, 3 years, no H&W)
Physical and sedentary activities: friend or foe?
The majority of the records which referred to physical activity focused upon its relation to function and mobility. Most commonly, discussions of physical activity were related to its negative effects, e.g. the experience of pain and/or fatigue in relation to different activity levels. Examples included increased fatigue when engaging in activities such as walking and running, and reports of worsening stamina and back pain associated with physical activities. This restricted children’s participation and could prompt withdrawal from even functional activity:
She reports that she walks minimally so that she doesn’t regress and develop more pain. (Physiotherapist, #7, 18 years, no H&W)
This may have led to parents setting limitations and restrictions on their child’s engagement in daily activities and they were encouraged to be a little less restrictive, such as: “Mother was encouraged to allow her to stand in the stander and to continue to walk at home” (Orthopaedist, #102, 17 years, no H&W).
A smaller proportion of records associated positive outcomes with physical activity:
She’s physically very active – she’s been playing flag football, volleyball, basketball, she’s on the high-level soccer team – and really is doing very well. (Paediatrician, #166, 15 years, no H&W)
For some with mobility or functional impairments, participation in sports was made possible with modified activities and adaptive equipment, such as hand-propelled bikes and adapted gym programmes. However, we did not find any discussions recorded around how an inactive child could undertake physical activities within the constraints of their disability or how adaptive equipment could be accessed or modified activities learned. Additionally, no discussions pertaining to how a child might obtain the social benefits of physical activities – such as making friends and improving psychological well-being [53] – were recorded in the medical charts. Formal sedentary activity histories were infrequently recorded. We found no record of discussions about appropriate levels of sedentary behaviours such as screen time.
Weight management, diet and physical activity: whose responsibility?
The medical records demonstrated that healthcare professionals had differing views on where the responsibility for diet, physical activity and weight management lay. Some comments suggested that healthcare professionals believed weight management to be under the control of the child and/or family, in terms of becoming, or continuing to be overweight/obese. For example, in the notes of one young man described as “morbidly obese” (but with no height and weight data), the responsibility was firmly placed onto the child when discussing future treatment of his condition:
They will not perform the surgery until patient shows considerable effort towards changing his lifestyle and eating habits. (Nursing, #108, 17 years, no H&W)
This was also demonstrated through the frequent description of children as “challenging themselves” to eat more fruits and vegetables and maintain sufficient water intake:
Patient has been working hard to improve his diet, which now includes salads and some fruits. He will continue to challenge himself with this, as well as increasing his water intake. (Nursing, #135, 13 years, OB)
Given the emphasis on self-management, the records suggested that healthcare professionals felt that it was essential for children to understand that obesity was an issue for them, with associated negative consequences:
He has grown 4 cm since last October, but he gained unfortunately 4.1 kg as well. I explained to patient the importance of losing weight and hopefully ‘he will get it’. (Nutrition clinic, #16, 13 years, OB)
The involvement of family members, especially the mother, was also seen as playing an important guiding role in both diet and fluid intake, and their attentiveness to maintaining a healthy diet was consistently noted:
Patient’s parents make sure she gets proper nutrition and is well hydrated. She gets lots of fruits and vegetables along with proper protein and whole grain breads. (Nursing, #149, 7 years, OB)
Certainly, co-operation between the child and his/her parents was seen to facilitate healthy nutrition and was used as a strategy to improve nutritional intake. A supportive family environment where parents actively encouraged children to eat a range of nutritious food appeared to play a key role in maintaining a well-balanced diet. The impact on parents was also recognised, for example, in this comment about the challenges experienced by a mother:
Mom and patient are going to work together to make a list of the healthy food patient is willing to eat, or at least try. Hopefully this will make mom’s grocery shopping easier, and give patient more variety in her diet. (Nursing, #138, 13 years, no H&W)
Similarly, parents were tasked with encouraging their children to “stay active” although notably with little specific guidance: “Mom is encouraged to keep patient very active which is benefiting her strength” (Physiotherapist, #103, 4 years, no H&W).
The medical records also indicated that responsibility was often expanded to other healthcare professionals. Children were frequently referred (formally and informally) to dieticians and paediatricians, as well as physiotherapists and nurses, for advice on reducing their weight, for example:
My suggestion for [patient] is that she receives some counseling from her paediatrician in terms of nutrition and diet as I suspect weight-loss would be very beneficial to her… (Surgeon, #139, 17 years, no H&W).
Discussion
Key findings
1. Height and weight are not routinely recorded for children attending an outpatient SB clinic.
Despite both the Canadian Pediatric Society [35] and American Academy of Pediatrics [36] recommendations, our examination of the medical records showed that weight and height were not routinely assessed at clinic visits. This was evident even in instances where children’s excess weight was explicitly mentioned in the notes (n = 8). We were only able to calculate a BMI for 35% of the 180 cases, of which almost 24% were classified as overweight and almost 18% as obese (41.3% in total). This markedly exceeds the prevalence of overweight and obesity found in typically developing Canadian children, which was 26% in 2009 [54] and is comparable to the higher end of previous estimates of obesity in children with SB cited as between 18 and 50% [26]. However, reporting bias cannot be ignored. For example, it is possible that clinicians measured weight and height more often, but only recorded their assessments if a particular problem was identified.
Of particular note is the finding that in less than a quarter (23.1%) of instances where BMIs fell in the overweight/obese range was the child’s excess weight mentioned in the notes. If a lack of reporting mirrors reality, this suggests that for the majority of overweight and obese children, excess bodyweight is not being considered as a priority topic during consultations. Given that the identification of obesity is associated with improved weight management [41,42], further research could usefully be targeted at identifying the barriers to weight management discussions in SB clinics. Reasons for this may include a lack of awareness among clinicians, a lack of confidence to tackle a notoriously sensitive issue or an unwillingness to overburden families who face many challenges already, such as intense therapy schedules [3,55] and socio-economic pressures [11]. It is not known whether the family members accompanying children in this study were themselves overweight, although it has been noted in the literature that overweight children frequently have overweight parents [56]. Clinicians have reported this factor to be an additional barrier to discussing weight with families [57], but weighing and measuring children at clinic appointments may provide an opportunity to raise the topic in a sensitive manner and perhaps discuss the broader family lifestyle, even where visits to HCPs are initiated for reasons other than body weight [58].
2. Discussions of weight-related behaviours with children and families were incompletely recorded and related mostly to symptom management as opposed to healthy lifestyle.
Discussions in the records around a healthy body weight were mostly related to physical function (e.g. mobility, pain, continence) and this was used to motivate the child to tackle overweight/obesity. There was, however, little discussion recorded on practical advice as how to achieve weight control, for example, whether the children were involved in appropriate and sufficient levels of physical activity. It was notable that sedentary activities such as playing video games or being on the computer were often recorded, yet we found no instances of advice given on minimising them, even though recent research has shown that sedentary behaviours are strongly associated with negative health outcomes, irrespective of physical activity levels [59,60]. Dietary quality was almost universally associated with bowel function rather than promoting diet in terms of nutritional balance and good overall health. It is possible that clinicians were attempting to tackle their clients’ body weight indirectly rather than discussing body weight explicitly. This is perhaps understandable as previous evidence has suggested that many paediatric clinicians are uncomfortable broaching the subject of obesity [61,62]. However, children deserve to be appropriately informed about their health and care [63,64], so further research could usefully be targeted at exploring clinicians’ motivations behind their approach to these discussions, thereby identifying training needs.
Recommendations
This study suggests that important health promotion opportunities are being missed. In addition to weight management and bowel and bladder function, the wider benefits of a good diet should be emphasised to children (and for the whole family), as it is crucial for children to develop good eating patterns and nutritious food preferences from an early age [10,65], given that childhood food preferences and eating patterns often track into adulthood [66]. Furthermore, emphasising the wider benefits of physical activity to children, such as making friends, increasing participation and improving psychological well-being [53] may be helpful, although some children and families may need assistance to find rewarding activities within their abilities [67].
However, it must be acknowledged that weight management is very complex and influenced by many environmental, personal and contextual factors [68]. In addition, SB is a multifaceted condition that often includes multiple health issues at any one time [69], which must be taken into account when planning weight management or health promotion strategies for this client group. Parents of children with disabilities have previously reported that therapy sessions often took priority over mealtimes [55], so working with families to identify strategies that are most useful and meaningful for them is paramount. Additionally, children and youth may need disability-specific assistance and counseling in order to achieve a healthier lifestyle, for instance, to establish strategies (e.g. pre-voiding) to deal with issues such as activity-induced incontinence. Integrating disability-specific counseling may foster greater participation and success. The obesogenic environment is a powerful influence upon weight-related behaviours [70], requiring clinicians to work closely with their patients and families – over and above merely providing information – to increase the likelihood that positive health behaviours are adopted. However, the impact of this on limited clinical resources also needs addressing, especially in smaller clinics which may not have access to specialist nutritional support.
Strengths and limitations
A number of limitations, as well as strengths must be noted. MRR is retrospective by nature and therefore the data were not collected for research purposes. As such, there may be inaccuracies in the data as they rely on the recorder [45]. Furthermore, we can only comment upon what was recorded in the records; we do not know what (if any) discussions occurred during consultations that were not recorded in the charts. It is possible that healthcare professionals discussed weight, diet and activities with patients and their families without recording them, although the structured and comprehensive nature of medical records makes this unlikely.
Our prevalence rates are based on a potentially skewed sample, given that we were only able to calculate BMI for 63 of the 180 eligible cases. It is possible that children who were considered at risk of obesity were more likely to be weighed and thus overweight/obesity is over-represented in our prevalence of 41.3%. However, it is likely that this is an underestimation of the true prevalence of overweight/obesity in children with SB, given that we found evidence of children being described as having excess weight in their notes but without height and weight data recorded. This highlights the benefit of taking a mixed methods approach to MRRs such as in this study, as this discrepancy would not have been detected had solely quantitative data been recorded.
The reliability of data extraction from medical records is a noted concern [43]. Reliability was, therefore, enhanced by following the principles advocated by a number of researchers experienced in this method [45,71,72]. The primary data extractor (EY) was not told the specific research objective, only that an audit of weight and height in medical records was being conducted. There were also clear inclusion and exclusion criteria. Inter-rater reliability was conducted by a randomly selected sample of 10% of the medical records extracted by a second person (AM), which exceeded accepted reliability limits [52]. Data entry accuracy was also verified.
Lastly, it is important to acknowledge that the use of BMI and cut-offs developed for typically developing children (such as those produced by the CDC) in the SB population has been criticised [73,74], which may contribute to inconsistent practice. Young people with SB frequently have a higher percentage of body fat and lower lean body mass [75,76] and are also usually shorter than their typically developing peers [69,74]. Alternative methods of assessing the weight and body composition of children with SB exist, such as dual-energy X-ray absorptiometry (“DXA scanning”) [73,74] or total body potassium (TBK) [77], but require costly, specialised equipment unavailable in most ambulatory clinics. Therefore, in the absence of a gold standard method of assessing and classifying the weight of children with SB, BMI may be used an indicator of excess weight, but it is important to also gather information on other health behaviours to provide a more holistic picture of the child’s lifestyle.
Future work
Clinicians who work with typically developing children are encouraged to assess, monitor and discuss weight-related issues regularly with children and their families [35,36], yet we know that this does not always occur in clinical practice [38–41]. It is unclear whether the variation in practice detected in this study is merely reflecting wider clinical practice, or whether there are specific barriers in this population. Therefore, further research could usefully explore these issues in a wider sample and start to identify the barriers and facilitators associated with weight assessment and management practices. An ethnographic study of an SB clinic may provide useful insight to this, providing the opportunity to observe clinical practice in context. In-depth interviews with clinicians from a wide range of disciplines may also be fruitful.
Acknowledgements
We would like to thank all the staff of Health Records at Holland Bloorview Kids Rehabilitation Hospital.
Declaration of interest
None of the authors have any conflict of interest to declare. We wish to thank the Ward Family Foundation Summer Student Endowment Program. Funding was also provided by a Bloorview Research Institute start-up grant.
References
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Childhood overweight and obesity. World Health Organization. 2009. Available from: http://www.who.int/dietphysicalactivity/childhood/en/index.html [last accessed 23 Aug 2012]
- 3.Rimmer JH, Rowland JL, Yamaki K. Obesity and secondary conditions in adolescents with disabilities: addressing the needs of an underserved population. J Adolesc Health. 2007;41:224–9. doi: 10.1016/j.jadohealth.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Reinehr T, Dobe M, Winkel K, et al. Obesity in disabled children and adolescents: an overlooked group of patients. Dtsch Ärztebl Int. 2010;107:268–75. doi: 10.3238/arztebl.2010.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neter JE, Schokker DF, de Jong E, et al. The prevalence of overweight and obesity and its determinants in children with and without disabilities. J Pediatr. 2011;158:735–9. doi: 10.1016/j.jpeds.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 6.Simeonsson RJ, McMillen JS, Huntington GS. Secondary conditions in children with disabilities: spina bifida as an example. Ment Retard Dev Disabil Res Rev. 2002;8:198–205. doi: 10.1002/mrdd.10038. [DOI] [PubMed] [Google Scholar]
- 7.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303:623–30. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 8.Yamaki K, Rimmer JH, Lowry BD, Vogel LC. Prevalence of obesity-related chronic health conditions in overweight adolescents with disabilities. Res Dev Disabil. 2011;32:280–8. doi: 10.1016/j.ridd.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Daniels SR, Jacobson MS, McCrindle BW, et al. American Heart Association childhood obesity research summit report. Circulation. 2009;119:e489–517. doi: 10.1161/CIRCULATIONAHA.109.192216. [DOI] [PubMed] [Google Scholar]
- 10.Lanigan JD. The substance and sources of young children’s healthy eating and physical activity knowledge: implications for obesity prevention. Child Care Health Dev. 2011;37:368–76. doi: 10.1111/j.1365-2214.2010.01191.x. [DOI] [PubMed] [Google Scholar]
- 11.Leitch KK. Reaching for the top: a report by the advisor on healthy children and youth. Ottawa: Health Canada; 2007. [Google Scholar]
- 12.Hogan A, McLellan L, Bauman A. Health promotion needs of young people with disabilities: a population study. Disabil Rehabil. 2000;22:352–7. doi: 10.1080/096382800296593. [DOI] [PubMed] [Google Scholar]
- 13.Antle BJ, Mills W, Steele C, et al. An exploratory study of parents’ approaches to health promotion in families of adolescents with physical disabilities. Child Care Health Dev. 2007;34:185–93. doi: 10.1111/j.1365-2214.2007.00782.x. [DOI] [PubMed] [Google Scholar]
- 14.Liou TH, Pi-Sunyer FX, Laferrere B. Physical disability and obesity. Nutr Rev. 2005;63:321–31. doi: 10.1111/j.1753-4887.2005.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 15.Buffart LM, Westendorp T, Erasmus MC, et al. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J Rehabil Med. 2009;41:881–5. doi: 10.2340/16501977-0420. [DOI] [PubMed] [Google Scholar]
- 16.Skär L, Prellwitz M. Participation in play activities: a single-case study focusing on a child with obesity experiences. Scand J Caring Sci. 2008;22:211–19. doi: 10.1111/j.1471-6712.2007.00515.x. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell LE, Adzick NS, Melchionne PS, et al. Spina bifida. Lancet. 2004;364:1885–95. doi: 10.1016/S0140-6736(04)17445-X. [DOI] [PubMed] [Google Scholar]
- 18.De Wals P, Tairou F, Van Allen MI, et al. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med. 2007;357:135–42. doi: 10.1056/NEJMoa067103. [DOI] [PubMed] [Google Scholar]
- 19.Pit-ten Cate IM, Kennedy C, Stevenson J. Disability and quality of life in spina bifida and hydrocephalus. Dev Med Child Neurol. 2002;44:317–22. doi: 10.1017/s0012162201002146. [DOI] [PubMed] [Google Scholar]
- 20.Bellin MH, Sawin KJ, Roux G, et al. The experience of adolescent women living with spina bifida Part I: self-concept and family relationships. Rehabil Nurs. 2007;32:57–67. doi: 10.1002/j.2048-7940.2007.tb00153.x. [DOI] [PubMed] [Google Scholar]
- 21.Buran CF, McDaniel AM, Brei TJ. Needs assessment in a spina bifida program. Clin Nurse Spec. 2002;16:256–62. doi: 10.1097/00002800-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Buran CF, Sawin KJ, Brei TJ, Fastenau PS. Adolescents with myelomeningocele: activities, beliefs, expectations and perceptions. Dev Med Child Neurol. 2004;46:244–52. doi: 10.1017/s0012162204000404. [DOI] [PubMed] [Google Scholar]
- 23.Verhoef M, Post MWM, Barf HA, et al. Perceived health in young adults with spina bifida. Dev Med Child Neurol. 2007;49:192–7. doi: 10.1111/j.1469-8749.2007.00192.x. [DOI] [PubMed] [Google Scholar]
- 24.Buffart LM, van den Berg-Emons HJG, van Wijien-Hempel MS, et al. Health-related physical fitness of adolescents and young adults with myelomeningocele. Eur J Appl Physiol. 2008;108:181–8. doi: 10.1007/s00421-008-0684-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buffart LM, van den Berg-Emons HJG, Van Meeteren J, et al. Lifestyle, participation, and health-related quality of life in adolescents and young adults with myelomeningocele. Dev Med Child Neurol. 2009;51:886–94. doi: 10.1111/j.1469-8749.2009.03293.x. [DOI] [PubMed] [Google Scholar]
- 26.Dosa NP, Foley JT, Eckrich M, et al. Obesity across the lifespan among persons with spina bifida. Disabil Rehabil. 2009;31:914–20. doi: 10.1080/09638280802356476. [DOI] [PubMed] [Google Scholar]
- 27. Spina Bifida Association. Fact sheets – obesity. Available from: http://www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2700287/k.C25F/Obesity.htm 2009 [last accessed 28 Jan 2011]
- 28.Danielsson A, Bartonek A, Levey E, et al. Associations between orthopaedic findings, ambulation and health-related quality of life in children with myelomeningocele. J Child Orthop. 2008;2:45–54. doi: 10.1007/s11832-007-0069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy NA, Carbone PS American Academy of Pediatrics Council on Children with Disabilities. Promoting the participation of children with disabilities in sports, recreation and physical activities. Pediatrics. 2008;121:1057–61. doi: 10.1542/peds.2008-0566. [DOI] [PubMed] [Google Scholar]
- 30.Buffart LM, Roebroeck ME, Rol M, et al. Triad of physical activity, aerobic fitness and obesity in adolescents and young adults with myelomeningocele. J Rehabil Med. 2008;40:70–5. doi: 10.2340/16501977-0135. [DOI] [PubMed] [Google Scholar]
- 31.Mita K, Akataki K, Itoh K, et al. Assessment of obesity of children with spina bifida. Dev Med Child Neurol. 1993;35:305–11. doi: 10.1111/j.1469-8749.1993.tb11642.x. [DOI] [PubMed] [Google Scholar]
- 32.Hayes-Allen MC. Obesity and short stature in children with myelomeningocele. Dev Med Child Neurol. 1972;S27:59–64. doi: 10.1111/j.1469-8749.1972.tb09775.x. [DOI] [PubMed] [Google Scholar]
- 33.Charney EB, Rosenbaum M, Finegold D. Linear growth in a population of children with myelomeningocele. Eur J Pediatr Surg. 1981;34:415–19. doi: 10.1055/s-2008-1063385. [DOI] [PubMed] [Google Scholar]
- 34.Antle BJ, Montgomery G, Stapleford C. The many layers of social support: capturing the voices of young people with spina bifida and their parents. Health Soc Work. 2009;34:97–106. doi: 10.1093/hsw/34.2.97. [DOI] [PubMed] [Google Scholar]
- 35.Dieticians of Canada and Canadian Paediatric Society. Promoting optimal monitoring of child growth in Canada: using the new who growth charts. Paediatr Child Health. 2010;15:77–9. doi: 10.1093/pch/15.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 37.Ogden C, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Rep. 2010;25:1–5. [PubMed] [Google Scholar]
- 38.Huang J, Donohue M, Golnari G, et al. Pediatricians’ weight assessment and obesity management practices. BMC Pediatr. 2009;9:19. doi: 10.1186/1471-2431-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dorsey KB, Wells C, Krumholz HM, Concato JC. Diagnosis, evaluation, and treatment of childhood obesity in pediatric practice. Arch Pediatr Adolesc Med. 2005;159:632–8. doi: 10.1001/archpedi.159.7.632. [DOI] [PubMed] [Google Scholar]
- 40.McLean K, Wake M, McCallum Z. Overweight in medical paediatric inpatients: detection and parent expectations. J Paediatr Child Health. 2007;43:256–61. doi: 10.1111/j.1440-1754.2007.01056.x. [DOI] [PubMed] [Google Scholar]
- 41.Patel AI, Madsen KA, Maselli JH, et al. Underdiagnosis of pediatric obesity during outpatient preventive care visits. Acad Pediatr. 2010;10:405–9. doi: 10.1016/j.acap.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perrin EM, Skinner AC, Steiner MJ. Parental recall of doctor communication of weight status: national trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2012;166:317–22. doi: 10.1001/archpediatrics.2011.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Labelle J, Swaine BR. Reliability associated with the abstraction of data from medical records for inclusion in an information system for persons with a traumatic brain injury. Brain Inj. 2002;16:713–27. doi: 10.1080/02699050110119880. [DOI] [PubMed] [Google Scholar]
- 44.Stange KC, Zyzanski SJ, Fedirko Smith T, et al. How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patient visits. Med Care. 1998;36:851–67. doi: 10.1097/00005650-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Worster A, Haines T. Medical record review studies: an overview. Isr J Trauma, Intensive Care Emerg Med. 2002;2:18–23. [Google Scholar]
- 46.Mabry IR, Clark SJ, Kemper A, et al. Variation in establishing a diagnosis of obesity in children. Clin Pediatr. 2005;44:221–7. doi: 10.1177/000992280504400305. [DOI] [PubMed] [Google Scholar]
- 47.Hulley SB, Cummings SR, Browner WS, et al. Designing clinical research. Philadelphia (PA): Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 48.Verhoef M, Barf HA, Post MWM, et al. Functional independence among young adults with spina bifida, in relation to hyrocephalus and level of lesion. Dev Med Child Neurol. 2006;48:114–19. doi: 10.1017/S0012162206000259. [DOI] [PubMed] [Google Scholar]
- 49.Horowitz RI, Yu EC. Assessing the reliability of epidemiological data obtained from medical records. J Chronic Dis. 1984;37:825–31. doi: 10.1016/0021-9681(84)90015-8. [DOI] [PubMed] [Google Scholar]
- 50.Day S, Fayers P, Harvey D. Double data entry: what value, what price? Control Clin Trials. 1998;19:15–24. doi: 10.1016/s0197-2456(97)00096-2. [DOI] [PubMed] [Google Scholar]
- 51.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 52.Oppenheim AN. Questionnaire design, interviewing and attitude measurement. London: Continuum; 2005. [Google Scholar]
- 53.Oriel KN, George CL, Blatt PJ. The impact of a community based exercise program in children and adolescents with disabilities: a pilot study. Phys Disabil Educ Relat Serv. 2008;27:5–20. [PubMed] [Google Scholar]
- 54. Statistics Canada. Body mass index (BMI) for children and youth 2007–2009; 2010. Report no. 2010001; 1–5.
- 55.Pocock M, Trivedi D, Wills W, et al. Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev. 2009;11:338–53. doi: 10.1111/j.1467-789X.2009.00648.x. [DOI] [PubMed] [Google Scholar]
- 56.Eneli IU, Kalogiros ID, McDonald KA, Todem D. Parental preferences on addressing weight-related issues in children. Clin Pediatr. 2007;46:612–18. doi: 10.1177/0009922807299941. [DOI] [PubMed] [Google Scholar]
- 57.Edvardsson K, Edvardsson D, Hörnsten Å. Raising issues about children’s overweight- maternal and child health nurses’ experiences. J Adv Nurs. 2009;65:2542–51. doi: 10.1111/j.1365-2648.2009.05127.x. [DOI] [PubMed] [Google Scholar]
- 58. National Institute for Health and Clinical Excellence. Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children; 2006. Available from: http://www.nice.org.uk/nicemedia/pdf/CG43NICEGuideline.pdf [last accessed 12 Jul 2012]
- 59.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Colley RC, Wong SL, Garriguet D, et al. Physical activity, sedentary behaviour and sleep in Canadian children: parent-report versus direct measures and relative associations with health risk. Health Rep. 2012;23:1–8. [PubMed] [Google Scholar]
- 61.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–14. [PubMed] [Google Scholar]
- 62.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5:150–6. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 63.United Nations. Convention on the Rights of the Child. Geneva: United Nations; 1989. [Google Scholar]
- 64.Alderson P. Children’s decisions in health care and research. London: Institute of Education; 2004. [Google Scholar]
- 65.Scaglioni S, Salvioni M, Galimberti C. Influence of parental attitudes in the development of eating behaviour. Br J Nutr. 2008;99:S22–5. doi: 10.1017/S0007114508892471. [DOI] [PubMed] [Google Scholar]
- 66.Kelder SH, Perry CL, Klepp K-I, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity and food choice behaviours. Am J Public Health. 1994;84:1121–6. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McPherson AC, Lindsay S. How do children with disabilities view “healthy living”? A descriptive pilot study. Disabil Health J. 2012;5:201–9. doi: 10.1016/j.dhjo.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 68.Mikhailovich K, Morrison P. Discussing childhood overweight a obesity with parents: a health communication dilemma. J Health Care. 2007;11:311–22. doi: 10.1177/1367493507082757. [DOI] [PubMed] [Google Scholar]
- 69.Liptak GS, Samra AE. Optimizing health care for children with spina bifida. Dev Disabil Res Rev. 2010;16:66–75. doi: 10.1002/ddrr.91. [DOI] [PubMed] [Google Scholar]
- 70.Freeman M, Stern JS. The role of optimal healing environments in the management of childhood obesity. J Altern Complement Med. 2004;10:S231–44. [PubMed] [Google Scholar]
- 71.Badcock D, Kelly A-M, Kerr D, Reade T. The quality of medical record review studies in the international emergency medicine literature. Ann Emerg Med. 2005;45:444–7. doi: 10.1016/j.annemergmed.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 72.Gilbert EH, Lowenstein SR, Koziol-McLian J. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–8. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 73.McDonald CM, Abresch-Meyer AL, Dopler Nelson M, Widman LM. Body mass index and body composition measures by dual X-ray absorptiometry in patients aged 10 to 21 years with spinal cord injury. J Spinal Cord Med. 2007;30:S97–104. doi: 10.1080/10790268.2007.11754612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liusuwan RA, Widman LM, Abresch RT, et al. Body composition and resting energy expenditure in patients aged 11 to 21 years with spinal cord dysfunction compared to controls: comparisons and relationships among the groups. J Spinal Cord Med. 2007;30:S105–11. doi: 10.1080/10790268.2007.11754613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wittenbrook W. Best practices in nutrition for children with myelomeningocele. Infant Child Adolesc Nutr. 2010;2:237–45. [Google Scholar]
- 76.Grogan CB, Ekvall SM. Body composition of children with myelomeningocele, determined by 40K, urinary creatinine and anthropometric measures. J Am Coll Nutr. 1999;18:316–23. doi: 10.1080/07315724.1999.10718870. [DOI] [PubMed] [Google Scholar]
- 77.Littlewood RA, Trocki O, Cleghorn G. Measured and predicted total body water in children with myelimeningocele. J Paediatr Child Health. 2003;39:278–81. doi: 10.1046/j.1440-1754.2003.00137.x. [DOI] [PubMed] [Google Scholar]