Abstract
The current study examined utilization of cognitive-behavioral therapy (CBT) by individuals receiving treatment for obsessive-compulsive disorder (OCD). Participants were 202 adults with primary DSM-IV OCD who enrolled in a longitudinal, observational study of the course of OCD and completed 2 years of annual follow-up interviews using the Longitudinal Interval Follow-Up Evaluation. One hundred twenty participants reported that a mental health professional recommended CBT for their OCD symptoms at some point during the 2-year follow-up period. One quarter (n = 31) of these participants did not initiate CBT despite receiving a treatment recommendation. Thirty-one percent of the 89 participants who entered CBT endorsed dropping out of CBT prematurely and less than one third received an adequate “dose” of CBT sessions. Self-reported CBT drop-out rates were significantly greater than attrition rates reported in clinical trials using intensive schedules of exposure and ritual prevention (EX/RP). Perceived environmental barriers and fears regarding treatment participation were the most frequently endorsed reasons for not participating or dropping out of CBT. Despite its efficacy for OCD, many individuals with clinically significant symptoms fail to initiate CBT when recommended by a mental health professional, receive treatments that are less intensive than those used in clinical trials, or drop out of treatment prematurely. Financial costs of CBT, difficulty attending sessions, and fears regarding treatment are significant barriers to initiating and completing therapy.
Acute treatment efficacy of cognitive–behavioral therapy (CBT) for obsessive–compulsive disorder (OCD) is well established. Results from randomized controlled trials (RCTs) indicate that two thirds of patients who enter CBT and as many as 77–86% of those who complete “gold standard” exposure and ritual prevention (EX/RP) show clinically significant improvement (Foa et al. 2005; Freeston et al., 1997). Results from several meta-analyses have documented high effect sizes for OCD treatments and low rates of placebo responses (Eddy, Dutra, Bradley, & Westen, 2004; Huppert et al., 2004). However, treatment attrition rates across EX/RP studies are variable suggesting that many individuals may not be able to tolerate or comply with treatment demands. RCTs examining twice-weekly sessions of EX/RP report attrition rates ranging from 8 to 19% of participants who enter treatment (Fals-Stewart, Marks, & Schafer, 1993; Simpson, Foa, et al., 2008; Tolin et al., 2007). An RCT comparing an intensive schedule of EX/RP (five times per week) with or without clomipramine (CMI) to CMI alone or pill placebo reported that one third of participants who entered the EX/RP conditions dropped out before completing treatment (Foa et al., 2005).
Observational studies (also referred to as “naturalistic treatment studies”) provide a unique opportunity to complement efficacy data and understand what happens when these treatments are delivered in routine clinical practice (Seligman, 1996). To increase generalizability of efficacy trials, these studies include broad inclusion/exclusion criteria, allow clinicians to deliver treatments as usual, and allow patients to choose their treatments. The few observational studies of OCD treatment to date suggest that EX/RP delivered outside of controlled trials is effective for diverse patients and settings including (a) individuals who were excluded or chose not to participate in RCTs (Franklin, Abramowitz, Kozak, Levitt, & Foa, 2000), (b) a private practice setting (Warren & Thomas, 2001), and (c) African American and Carribean American patients treated in a university-based anxiety clinic (Friedman et al., 2003). Drop-out rates in these studies were similar to RCTs, ranging from 8 to 9% for individuals receiving treatment in university-based anxiety clinics (Franklin et al., 2000; Friedman et al., 2003) to 27% for those who received treatment in private practice (Warren & Thomas, 2001). However, these studies are limited to small sample sizes (Friedman et al., 2003; Warren & Thomas) or were delivered by psychologists or trainees in academic specialty clinics (Franklin et al., 2000; Friedman et al., 2003).
Observational studies of OCD also suggest that CBT may be underutilized among patients who seek treatment, even in anxiety specialty clinics. Results of a chart review study of 85 patients receiving treatment at an OCD specialty clinic indicated that almost all received a serotonin reuptake inhibitor (SRI) for at least 10 weeks but only 45% received EX/RP (Orloff et al., 1994). Another study by Goisman and colleagues (1993) found that only 28% of patients receiving treatment in anxiety specialty clinics received EX/RP. Similarly, Denys, VanMegen, and Westenberg (2002) reported that only 6% of patients seeking treatment at an OCD specialty clinic in The Netherlands had received CBT. In a large survey of the treatment practices of psychiatrists in the United States, Blanco and colleagues (2006) found that only 7.5% of 132 OCD patients were receiving CBT. In the only study to use a longitudinal, observational design to assess use of CBT for OCD in a sample of 66 patients, Eisen and colleagues (1999) found that only 18% received at least 20 sessions of CBT over a 2-year follow-up. However, rates of CBT dropout or refusal were not examined in these studies and reasons for CBT underutilization remain unclear. Given the high drop-out rates reported in RCTs, one reason for CBT underutilization may be that patients are unwilling to enter or complete CBT treatment. Lack of providers trained in EX/RP and patient’s unwillingness to endure distress associated with EX/RP have been hypothesized to be barriers to treatment but have not been systematically studied in OCD samples (Kozak & Coles, 2005; Tolin & Hannan, 2005). Further, all of these studies specifically examined patients in treatment at medical centers and treatments delivered in the 1990s prior to several movements aimed at increasing use of evidence-based treatments among psychologists (Chambless & Hollon, 1998; Chambless & Ollendick, 2001), as well as psychiatrists (Mellman & Beresin, 2003).
The Brown Longitudinal Obsessive Compulsive Study (BLOCS) is an ongoing, observational follow-up study of treatment-seeking individuals who self-identified OCD as their primary psychiatric disorder (defined as the most problematic psychiatric disorder lifetime). Participants were recruited from mental health specialty sites in Rhode Island and southeastern Massachusetts. Data collected at intake indicated that only 24% of participants reported receiving a recommended dose of CBT (i.e., at least 13 sessions scheduled weekly or more frequently) prior to study entry (Mancebo et al., 2006). In a small pilot study assessing CBT history prior to study entry among a subset of the intake sample (n = 80), anxiety regarding treatment and perceived environmental barriers were the most frequently endorsed reasons for not receiving or not completing CBT in the past (Mancebo, Pinto, Rasmussen, & Eisen, 2008). However, these data were retrospective and recall bias may have influenced participant responses.
The current study focuses on understanding reasons for CBT underutilization by examining prospective data collected during the first 2 years of follow-up. The main aims of the current study are to describe patient perceptions of CBT utilization, compare self-reported dropout rates to those reported in clinical trials, and identify patient perceptions of barriers to CBT in a large sample of treatment-seeking individuals with primary OCD. Exploratory aims were to examine perceived use of evidence-based techniques for OCD (e.g., exposure and response prevention) among participants who endorsed receiving CBT and to identify potential patient characteristics affecting adherence to CBT recommendations. Based on the literature cited above, we hypothesized that (a) a substantial number of participants who continued to meet DSM-IV criteria for OCD would report receiving CBT treatment recommendations but would fail to initiate CBT, (b) self-reported CBT drop-out rates in our study would be significantly greater than those reported in clinical trials of intensive EX/RP for OCD, and (c) perceived environmental barriers and fears regarding treatment would be the most frequently endorsed reasons for not initiating CBT and dropping out of CBT.
A benchmarking strategy was used to evaluate self-reported CBT drop-out rates in patients receiving treatment for OCD in outpatient mental health settings. Specifically, self-reported drop-out rates in this study were compared with those reported in three clinical trials of CBT (Abramowitz, Foa, & Franklin, 2003; Franklin et al., 2000; Storch et al., 2008). These studies defined dropouts as individuals who enrolled in the study and discontinued before completing the EX/RP protocol. We chose these three trials based on their generalizability to patients (broad inclusion criteria) and treatment characteristics (no random assignment, used weekly or twice-weekly therapy sessions) delivered in outpatient mental health settings. Two studies compared intensive EX/RP to twice-weekly sessions and the third was an open trial of intensive EX/RP (see treatment characteristics for all three studies in Table 1).
Table 1.
Comparison of BLOCS Sample and Treatment Characteristics to Clinical Trial Benchmark Studies
| Study | Franklin et al., 2000 (N = 110) | Abramowitz et al., 2003 (N = 40)a | Storch et al., 2008 (N = 62)b | BLOCS (N = 202) |
|---|---|---|---|---|
| Sample Demographics | ||||
| Male (%) | 52.7 | 57.5 | 53.0 | 43.0 |
| Caucasian (%) | 98.0 | NR | NR | 96.0 |
| Age (Mn ± SD) | 34.2 ± 13.1 | I = 36.2 ± 15.6; TW = 38.7 ± 3.6 | I = 35.6 ± 14.7; W = 27.6 ± 7.9 | 39.7 ± 12.5 |
| College educatedc (%) | 46.0 | NRd | NR | 46.0 |
| Married (%) | 31.0 | NR | NR | 44.0 |
|
| ||||
| Clinical Characteristics | ||||
| OCD duration, yrs (Mn ± SD) | NR | I = 14.5 ± 11.3; TW = 20.4 ± 12.8 | NR | 22.1 ± 13.5 |
| 54.0 | 45.0 | NRe | 63.8 f | |
| Comorbid Axis I (%) | 56.0 | 45.0 | 79.0 f | 83.7f |
| On SRI (%) | 26.7 ± 4.8 | I = 25.7 ± 3.9; | I = 28.5 ± 4.7; | 23.3 ± 5.8 |
| YBOCS (Mn ± SD) | TW = 25.5 ± 4.5 | W = 24.9 ± 6.0 | ||
| MHRSD (Mn ± SD) | 12.9 ± 5.8 | N/A | N/A | 11.8 ± 8.9 |
|
| ||||
| Treatment Characteristics | ||||
| Number of sessions per week | 5 | I = 5; TW = 2 | I = 5; W = 1 | 1–2 or less |
| Total number of sessions | 18 | 15 | 14 | 22 (median) |
| CBT characteristicsg | Individual EX/RP | Individual EX/RP | Individual EX/RP | Individual CBT N/A |
| Treatment setting | Anxiety clinic, university medical center | Anxiety clinic, university medical center | University- based OCD clinic | |
| Therapist Characteristics | Ph.D.s or psychology interns | Ph.D.s | Ph.D.s or psychology interns | Ph.D.s = 82% MA = 10% |
|
| ||||
| Percent Did Not Initiate CBT | NR | NR | 1.5 | 26% of 120 who endorsed CBT recommendation |
|
| ||||
| Percent Dropped Out of CBT | 9.0 | I = 20.0; TW = 20.0 | I = 3.0; W = 16.6 | 31% of 89 participants who initiated CBT |
Note. Abbreviations: N/A = not administered; NR = not reported.
Twenty participants received intensive (I) sessions and 20 participants received twice-weekly (TW) sessions.
Thirty-two participants received intensive (I) sessions and 30 participants received weekly (W) sessions.
College educated defined as having a 4-year undergraduate or graduate degree.
Mean number of years of schooling = 17.
Excluded history or current psychosis or bipolar, current suicidality, or substance use disorder.
Rates are significantly greater (p <. 05).
Participants in benchmarking studies received standard EX/RP, but BLOCS participants may have received a variety of CBT techniques.
Method
Participants
Participants were enrolled in the BLOCS between June 2001 and October 2004. Two hundred and fifty-two participants (78% of the 325 adults who completed intake interviews) had completed an intake interview and 2 years of follow-up assessments in an ongoing, longitudinal study course of OCD in a clinical sample. The remaining 73 participants (22% of the original sample) had not yet completed two annual interviews (n = 68), were deceased (n = 2), or dropped out of the study (n = 3). This report is limited to the 202 who met full DSM-IV criteria at study intake (the 50 adult participants who were in remission at study intake were excluded from analyses).
Participants were individuals with DSM-IV OCD who had sought treatment for OCD within the past 5 years. We included participants with comorbid disorders if they identified OCD as the most problematic disorder lifetime (primary OCD). The only other inclusion criteria were willingness/ability to participate in annual interviews and no evidence of an organic mental disorder.
Table 1 compares sample characteristics for the BLOCS and the three benchmarking clinical trials. Chi-square analyses indicated that demographic and clinical characteristics of our sample were similar to the three studies with two exceptions. Comorbidity rates in our sample were similar to those reported by Franklin et al. (2000) but significantly greater than rates reported by Abramowitz and colleagues (2003), χ2 = 6.46, df = 2, p = .039. Major comorbid Axis I disorders in our sample were social phobia (18%), major depressive disorder (15%), and specific phobia (14%). Most common personality disorders were obsessive compulsive personality (24%) and avoidant personality (15%). Participants in our sample were also more likely to be on an SRI at study entry than participants in two (the Franklin and Abramowitz studies) of the three benchmarking studies, χ2 = 42.93, df = 3, p < .001.
Procedures
Participants were recruited from consecutive admissions to one of several psychiatric treatment settings in the Rhode Island/southeastern Massachussetts area including a hospital-based outpatient OCD clinic, inpatient and partial hospitalization units of a private psychiatric hospital, two community mental health centers, a general outpatient psychiatric group practice, and three private practice psychotherapy sites known for their expertise in providing CBT for OCD. Seventy-percent of the intake sample was obtained from the OCD specialty clinic that provided pharmacotherapy and referrals to CBT therapists in the community. Thus, all participants had initiated some form of treatment for OCD at study intake. A total of 653 individuals were screened for the study: 127 did not meet inclusion/exclsuion criteria (85 identified another psychiatric disorder as primary, 24 did not live locally, 9 were not in treatment for OCD, and 3 were unable to provide informed consent), 127 refused to participate in the study, and 4 withrew from the study before completing the intake interview. Thus, the final intake sample consisted of 395 participants (75% of eligible screens) who completed the intake interview (325 adults and 70 children). As stated above, this report is limited to the 202 adults who met full DSM-IV criteria at study intake and completed the first 2 years of follow-up.
The Butler Hospital and Brown University Institutional Review Boards approved the study. After providing written informed consent to participate in annual interviews, participants were interviewed in person by trained clinical interviewers at study intake and were contacted annually for an in-person or telephone follow-up interview. There were no study restrictions on treatments received during the follow-up phase of the study and this observational study consisted only of annual interviews assessing changes in symptoms, functioning, and treatments received since the previous interview. For ethical reasons, study staff were allowed to provide standard referrals to an appropriate clinician or agency to participants who expressed interest in restarting mental health treatment or reported serious psychiatric symptoms (e.g., suicidal ideation). However, the actual referrals by study staff were rare, only for participants who expressed suicidal ideation, and no participant specifically requested a CBT referral from study staff. Therefore, participants received naturalistic treatments and treatment recommendations were provided by community clinicians.
Measures
Intake diagnoses were established using the Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition (SCID/IP; First, Spitzer, Gibbon, & Williams, 1996) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997). Newly trained interviewers were required to demonstrate a high degree of interrater reliability (intraclass correlation coefficients > .85) with both SCID trainers and other raters. All interviews were audiotaped and raters presented cases at weekly meetings attended by a psychiatrist and a clinical psychologist (MCM and JE, respectively), both with expertise in OCD. More details regarding interviewer training are described elsewhere (Eisen et al., 2010; Pinto et al., 2006). In an effort to avoid rater drift, interviewers continued to submit randomly selected tapes on a regular basis for interrater reliability ratings (IRR). All interviewers listened to tapes and submitted IRRs for the main outcome measures (including OCD diagnosis and Yale-Brown Obsessive Compulsive Scale [YBOCS] scores). Raters who did not meet the standards underwent retraining. Shrout-Fleiss interrater reliabilities for OCD diagnoses were 0.97 and for total YBOCS scores were 0.95, indicating excellent interrater reliability.
Follow-up interviews were conducted yearly with the Longitudinal Interval Follow-up Evaluation (LIFE), a semistructured interview designed to assess the longitudinal course of Axis I disorders and psychosocial functioning (Keller et al., 1987). The LIFE also assesses weekly medication usage as well as psychosocial treatments received in each follow-up interval. Whenever possible, clinical records were consulted to verify participant reports of treatments received. The LIFE has been shown to yield good interrater reliability, long-term test–retest reliability and convergent validity (Warshaw, Keller, & Stout, 1994). Current (past-week) OCD symptom severity was assessed at each interview using the YBOCS, a reliable and valid 10-item rater-administered scale (Goodman, Price, Rasmussen, Mazure, Delgado, et al., 1989; Goodman, Price, Rasmussen, Mazure, Fleischman, et al., 1989).
The 25-item version of the rater-administered Modified Hamilton Rating Scale for Depression (MHRSD) was used to assess current (past-week) severity of depressive symptoms (Miller, Bishop, Norman, & Maddever, 1985). Reliability of the MHRSD is excellent (intraclass correlation = 0.93) and validity has been established by comparing it with the original Hamilton Depression Rating Scale (Hamilton, 1960).
The Treatment Adherence Survey–Patient Version (Mancebo et al., 2008) is a rater-administered measure designed to assess the types of treatments recommended to participants (CBT and/or medications) and whether participants followed through with treatment recommendations. The following definition of CBT is provided to participants who endorse receiving any psychotherapy: “CBT for OCD focuses on learning techniques to manage your obsessions and compulsions. Most often it involves facing the situations that you avoid because of the anxiety associated with your obsessions (exposure) without doing your rituals (response prevention). You also learn to change the way you think about intrusive, obsessive thoughts, which will decrease your anxiety and lead to more realistic thinking.” Participants who pursued CBT and/or medication treatments are asked whether they dropped out of treatment prematurely. Specifically, participants who endorsed attending CBT during follow-up were asked “Did you stop attending CBT before completing therapy?” Participants who endorsed “yes” on this item were considered to be self-identified CBT dropouts. The interviewer also asks participants to check off as many reasons as apply from a list of 14 possible reasons and one open-ended item for not participating in CBT and/or dropping out of CBT prematurely, and then to select the reason that most influenced their decision not to adhere to treatment recommendations. The instrument has demonstrated excellent test–retest reliability and excellent agreement with medical chart documentation (Mancebo et al., 2008).
The Behavioral Therapy Inventory (BTI) was used to assess perceived frequency of specific CBT techniques known to be effective for OCD. The BTI was adapted from the Psychosocial Treatment Inventory (PTI), an interview designed to assess frequency of different types of psychosocial treatment methods (Steketee et al., 1997). We modified the original PTI by including only behavioral and cognitive methods known to be effective for OCD. The first section of the BTI is an inventory of 15 types of CBT techniques known to be effective for OCD. All participants who endorsed seeing a therapist for their OCD were asked whether they used specific CBT techniques during their treatment. Participants were asked to rate the frequency of 15 CBT techniques stating whether it was used 0 (never or rarely), 1 (sometimes), or 2 (frequently/a lot) during their therapy sessions.
Data Analysis
This report presents data for the first 202 adults who met DSM-IV criteria for OCD (based on the SCID-P) and completed 2 years of follow-up assessments. SAS version 9.13 (SAS Institute, 2007) was used for data analyses. We used the American Psychiatric Association Practice Guidelines for OCD (American Psychiatric Association, 2007) to define the recommended minimum “dose” of CBT (13 weekly sessions) and SRIs (at least 8 weeks). Descriptive analyses consisted of frequencies, percentages, means, and standard deviations. Between-group differences were examined with the chi-square tests for categorical variables and ANOVAs for continuous variables. McNemar’s tests were used to examine rates of treatment utilization across time. Statistical t tests were two-tailed and an alpha level of 0.05 was used to determine statistical significance.
A series of three logistic regression analyses were used to identify patient characteristics at intake that were uniquely associated with CBT utilization and adherence during the 2-year follow-up. Outcome variables were (a) receiving a CBT recommendation, (b) initiating CBT when it was recommended, and (c) prematurely dropping out of CBT. We excluded participants who were attending CBT at study intake from the first two analyses as these participants had already initiated CBT. The following intake variables were entered simultaneously as predictors: age, gender, education (college degree), OCD severity (YBOCS score), duration of OCD, severity of depression (MHRSD score), number of comorbid Axis I diagnoses, and previous history of CBT. A best-subsets approach was used to examine all possible subsets of these predictor variables. We examined the score statistic for all possible models and selected the smallest set of variables that yielded a meaningful increment in explained variance over competing models (Furnival & Wilson, 1974; Hosmer & Lemeshow, 2000).
Results
Treatments Received for OCD During Follow-up
Treatments received prior to study entry and during each of the 2 years of follow-up are described in Table 2. Most of the sample (83%) was on an SRI at study intake and continued on an SRI throughout the 2-year observational period. Ninety percent of participants (n = 167) receiving psychotropic medications for OCD reported receiving treatment from a psychiatrist, 9% (n = 17) from their primary care physician, and 1% (n = 2) from another type of clinician (e.g., nurse practitioner).
Table 2.
Treatments Received for OCD at Intake, During 2 Years of Follow-Up, and Lifetime (N = 202)
| Prior to Intake | Year 1a | Year 2a | |
|---|---|---|---|
| Any Psychotherapy, n (%) | 152 (75.2) | 106 (52.5) | 74 (36.6) |
| Cognitive–Behavioral Therapy, n (%) | 119 (59.2)b | 83c (41.1) | 68c (33.7) |
| Received 13+ weekly sessions, n (%)d | 53 (26.2) | 19 (9.4) | 17 (8.4) |
| Total number of sessions, Mean (±SD) | 36.9 (45.2) | 19.7 (19.4) | 19.7 (18.0) |
| Median | 21 | 15 | 14.5 |
| Range | 1–250 | 1–134 | 1–88 |
| Non-CBT Psychotherapy, n (%)e | 38 (18.8) | 34 (16.8) | 20 (9.9) |
| Total number of sessions, Mean (±SD) | N/A | 15.5 (14.4) | 18.4 (19.7) |
| Median (Range) | N/A | 12 (1–52) | 12.5(1–63) |
| Any Psychotropic Medications, n (%) | 184 (91.1) | 186 (92.1) | 174 (86.1) |
| Serotonin Reuptake Inhibitors (SRIs), n (%) | 169 (83.7) | 181 (89.6) | 165 (81.7) |
| Received for at least 8 consecutive weeks, n (%)d | 123 (60.8) | 175 (86.6) | 162 (80.2) |
| Number of wks on drug, Mean (±SD) | 173.8 (±236.6) | 46.9 (±11.9) | 43.8 (±11.9) |
| Number of wks on drug, Median | 52 | 52 | 52 |
Note. N/A = data not available.
Rates refer to treatments received from intake to year 1 (year 1) and from year 1 to year 2 (year 2).
Sixty-two participants were attending CBT at the time of the intake interview.
Some participants received CBT in year 1 and 2. Total of 89 participants received CBT during the 2-year follow-up period.
Recommended doses of CBT and SRIs for OCD were based on the American Psychological Association Practice Guidelines (2007).
Number of non-CBT counseling sessions received prior to study entry was not collected at intake.
Rates of CBT and non-CBT decreased from year 1 to year 2 (McNemar’s test = 6.53, p = .01). All but five CBT participants reported concurrent use of SRIs during CBT. A total of 89 participants (44% of the sample) received CBT during the follow-up period: 53 participants were participating in CBT at study intake and continued to attend CBT sessions, 23 participants entered CBT for the first time (i.e., no history of CBT prior to study entry), and 13 participants restarted CBT (i.e., had attended CBT more than 1 year prior to study entry and entered CBT again during follow-up). The mean number of CBT sessions received over 2 years was 33.1 (SD = 33.3). Participants who endorsed CBT were more likely to be seeing a doctoral-level clinician (χ2 = 59.23, df = 2, p < .001): 82% of CBT participants (n = 73) reported receiving treatment from a doctoral-level therapist (psychologist or social worker), 12% (n = 11) from a non-Ph.D. therapist, and 6% (n = 5) from a psychiatrist. In contrast, 68% (n = 24) of non-CBT psychotherapy was provided by a psychiatrist, 17% (n = 6) from a doctoral-level clinician, and 14% (n = 5) from a master’s-level clinician.
Only 38 (19% of the sample and 43% of the 89 CBT participants) attended CBT sessions that were scheduled at a frequency of once or twice per week and 26 (13% of the sample and 14 29% of CBT participants) endorsed receiving a recommended “dose” of at least 13 weekly sessions of CBT during follow-up. All but three participants denied attending intensive outpatient (defined as at least three times per week) or residential CBT. Participants who reported attending CBT for the first time were as likely to receive a recommended “dose” of CBT as those who reported attending CBT prior to study intake (46 vs. 35%, respectively, χ2 = 1.19, df = 1, p = .27).
Adherence to CBT Recommendations
As shown in Figure 1, more than half of the sample (n = 120) reported that a clinician recommended CBT for their OCD at some point during the 2 years of follow-up. Among these 120 participants who received CBT recommendations, 26% (n = 31) failed to initiate therapy.
FIGURE 1.
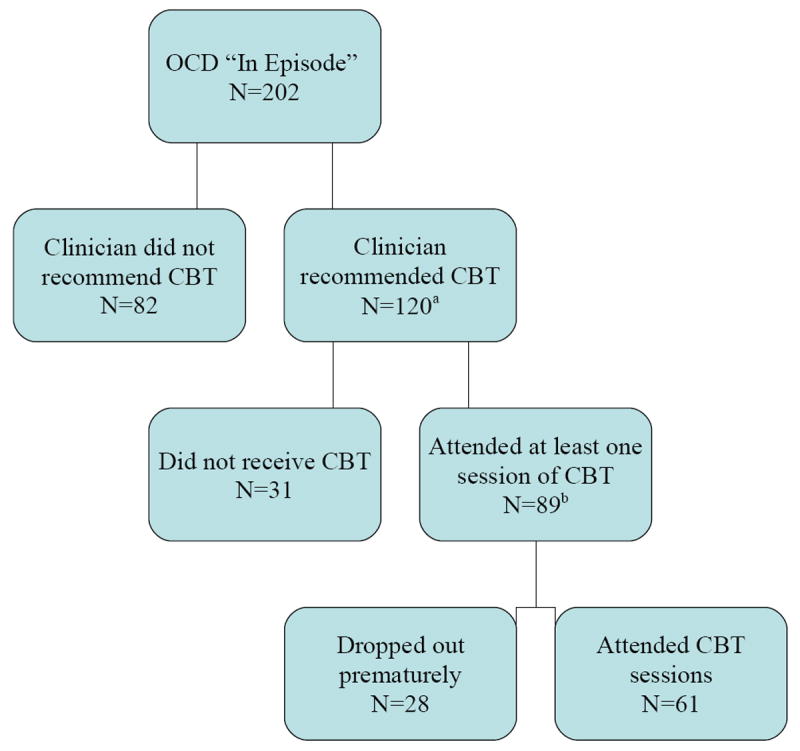
Adherence to CBT recommendations received during 2 years of follow-up among 202 participants with DSM-IV OCD.
Note. aForty participants had no history of CBT and 80 reported attending at least one session of CBT prior to intake. bIncludes 18 participants who did not initiate CBT when first recommended but entered CBT after a second recommendation. Therefore, these participants were categorized as attending CBT during the follow-up period.
Self-Reported Versus Clinical Trial Drop-Out Rates
As described in Figure 1, 31% of the 89 participants who entered CBT during follow-up reported dropping out before completing therapy. Intake YBOCS scores for participants who denied dropping out of CBT (Mn = 24.2, SD = 5.9) were similar to those of self-identified CBT drop-outs (Mn = 24.4, SD =4.5; t = 0.14, df = 87, p = .885). Table 1 compares self-reported drop-out rates from our sample to the rates reported in the three benchmarking clinical trials. Chi-squared analyses showed that the attrition rate in our study was significantly greater than the rates reported for intensive EX/RP conditions in the Franklin et al. (2000) and Storch et al. (2008) studies but not significantly different from the Abramowitz study (χ2 = 18.5, df = 3, p < . 01). Rates in our study were also similar to attrition rates reported for participants who entered weekly or twice-weekly EX/RP.
Reasons for Not Initiating CBT or Dropping Out of Treatment
Reasons endorsed for not following through with CBT recommendations are listed in Table 3. The most frequently endorsed reasons for not initiating CBT were environmental barriers to participating in treatment (e.g., could not find a CBT provider, could not afford treatment, difficulty scheduling appointments) and most participants also selected these items as the main reason that they failed to initiate CBT. Beliefs about utility of treatment (e.g., would not be helpful, would not learn anything new) and severity of illness were also frequently endorsed but few participants identified these beliefs as the main reason for not participating in CBT. Thirty percent reported fear/anxiety regarding treatment as a reason for not pursuing CBT and 20% endorsed this as the main reason for not initiating.
Table 3.
Reasons for Not Initiating or Dropping Out of CBT for OCD
| Did Not Initiate When Recommendeda (N = 49) | Dropped Out of CBT (N = 28) | |||
|---|---|---|---|---|
|
| ||||
| Endorsed Reasonb | Main Reason | Endorsed Reasonc | Main Reason | |
| TASP Item | N (%) | N (%) | N (%) | N (%) |
| Perceived Environmental Barriers | 34 (69.3) | 27 (55.1) | 15 (53.5) | 13 (46.4) |
| CBT not available | 5 (10.2) | 1 (2.0) | 0 (0.0) | 0 (0.0) |
| Could not afford cost of CBT | 12 (24.4) | 3 (6.1) | 5 (17.8) | 3 (10.7) |
| Health insurance did not cover CBT | 16 (32.6) | 10 (20.4) | 2 (7.1) | 1 (3.5) |
| Too busy or treatment was inconvenient | 20 (40.8) | 13 (26.5) | 12 (42.8) | 9 (32.1) |
| Perceived Utility of CBT | 16 (32.6) | 3 (6.1) | 9 (32.1) | 4 (14.2) |
| CBT not helpful in the past | 4 (8.1) | 2 (4.1) | 1 (3.5) | 1 (3.5) |
| Did not think CBT would work for my OCD | 9 (18.3) | 1 (2.0) | 5 (17.8) | 1 (3.5) |
| CBT would not teach me anything new | 6 (12.2) | 0 (0.0) | 4 (14.2) | 2 (7.1) |
| Too Anxious or Fearful to Participate in CBT | 15 (30.6) | 10 (20.4) | 8 (28.5) | 6 (21.4) |
| Beliefs Regarding Severity of Illness | 15 (30.6) | 5 (10.2) | 3 (10.7) | 2 (7.1) |
| OCD not severe enough to justify CBT | 7 (14.2) | 3 (6.1) | 2 (7.1) | 1 (3.5) |
| OCD was too severe to participate in CBT | 8 (16.3) | 2 (4.1) | 1 (3.5) | 1 (3.5) |
| Relationship With Clinician | 6 (12.2) | 2 (4.1) | 2 (7.1) | 1 (3.5) |
| Did not think CBT provider was good | 2 (4.0) | 2 (4.1) | 1 (3.5) | 1 (3.5) |
| OCD symptoms too personal too discuss | 4 (8.1) | 0 (0.0) | 1 (3.5) | 0 (0.0) |
| Stigma/Confidentiality | 4 (8.1) | 2 (4.1) | 1 (3.5) | 0 (0.0) |
| Did not want a “record” of treatment for OCD | 2 (4.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Worried about stigma of mental illness | 3 (6.1) | 0 (0.0) | 1 (3.5) | 0 (0.0) |
| Embarrassed others would find out | 3 (6.1) | 2 (4.1) | 0 (0.0) | 0 (0.0) |
| Other Reasons | 5 (10.2) | 0 (0.0) | 4 (14.2) | 2 (7.1) |
Note.
Thirty-one participants endorsed not attending CBT and an additional 18 participants did not receive CBT when first recommended but entered CBT after a second recommendation (n = 49). These participants were categorized as attending CBT but also reported reasons for not attending CBT when it was originally recommended.
Column does not sum to 49 because participants were allowed to endorse multiple reasons for not initiating CBT when recommended.
Column does not sum to 28 because participants endorsed multiple reasons for dropping out of CBT.
The reasons endorsed for dropping out of CBT were similar to those cited by participants who did not initiate treatment and chi-square analyses revealed no significant differences (all p values greater than .05). Perceived environmental barriers were the most common reasons for dropping out of CBT and 46% of self-identified CBT dropouts reported this as the main reason for terminating treatment. Specifically, most participants endorsed difficulty attending regular sessions (i.e., “too busy” or “treatment was inconvenient”) versus financial costs of treatment. More than one quarter of CBT dropouts identified fear/anxiety regarding treatment as a reason for terminating treatment and all but two cited this as the most influential reason for terminating treatment.
Patient Characteristics Associated With CBT Recommendations and Adherence
We used best-subsets logistic regression modeling to identify potential predictors of receiving a CBT treatment recommendation, initiating CBT during the 2-year follow-up, and dropping out of CBT. Participants who were already attending CBT at intake (n = 62) were excluded from the analyses predicting CBT recommendations or initiating CBT as we could not assess pretreatment characteristics such as symptom severity or comorbid disorders. The first model significantly predicted likelihood of receiving a CBT recommendation during the 2-year follow-up (χ2 = 9.54, df = 1, p = .002, −2 log likelihood = 177.55) and correctly classified 64% of the sample. Significantly increased odds of receiving a CBT recommendation were associated with increased YBOCS score at intake (OR = 1.09, p =.003, CI = 1.03–1.17). The second model found that increased OCD severity at intake also predicted likelihood of initiating CBT during follow-up (χ2 = 11.27, df = 4, p = .023, −2 log likelihood = 141.106) and correctly classified 68% of the sample (OR = 1.10, p =.013, CI = 1.02–1.19). These results suggest that for every 1-point increase in YBOCS at intake, there was a 9% increase in likelihood of endorsing a CBT recommendation and a 10% increase in likelihood of initiating CBT. None of the other variables (age, gender, education, OCD duration, MHRSD, comorbid disorders, or CBT history) made a significant contribution to the first two models. Finally, a third model found no significant predictors of dropping out of CBT among the 89 participants who attended CBT during follow-up.
Perceived Use of Specific CBT Techniques
Table 4 lists the specific techniques endorsed as “frequently” used during CBT. The majority (86%) of CBT participants reported that their therapist encouraged them to use self-directed EX/RP (practice EX/RP and/or decrease avoidance behaviors outside of therapy sessions). More than half of CBT participants also reported using direct (in vivo) EX/RP, imaginal EX/RP, and/or cognitive restructuring during therapy sessions. Techniques that were the least frequently endorsed were making an audiotape of obsessions (12%) or completing cognitive challenge records such as a thought record or a downward arrow (22%).
Table 4.
Number and Percentage of CBT Participants Who Endorsed “Frequent” Use of Technique During Psychotherapy (N = 89)
| How often did your doctor, counselor, or therapist … | CBT Participants (n = 89) | |
|---|---|---|
| Exposure and Response Prevention (EX/RP) Methods | ||
| Ask you to imagine having prolonged contact with things that make you anxious (exposure)? | 57 (64.0) | |
| Ask you to actually have prolonged contact with things that make you anxious during a session (exposure)? | 45 (51.6) | |
| Ask you to imagine deliberately refraining from performing compulsions (response prevention)? | 54 (60.6) | |
| Ask you to actually deliberately refrain from performing compulsions during a session (response prevention)? | 48 (53.9) | |
| Ask you to practice exposure between sessions? | 77 (86.5) | |
| Ask you to practice response prevention between sessions? | 77 (86.5) | |
| Refuse to give you reassurance regarding your obsessions? | 39 (43.8) | |
| Encourage you not to avoid situations that trigger your OCD symptoms? | 77 (86.5) | |
| Make an audiotape of your obsessions and ask you to practice listening to it? | 11 (12.3) | |
| Cognitive Methods | ||
| Ask you to deliberately exaggerate your fears in order to neutralize them? | 41 (46.0) | |
| Ask you to rate on a scale how strongly you believe these thoughts or beliefs to be true? | 41 (46.0) | |
| Ask you to substitute different, more rational thoughts or beliefs for your erroneous ones or otherwise help you restructure your thinking? | 53 (59.5) | |
| Ask you to use a thought record, downward arrow, or pie chart to challenge the unreasonableness of your worries? | 20 (22.4) | |
| Homework Exercises | ||
| Ask you how often you deliberately exposed yourself to situations that triggered your OCD symptoms and try to refrain from performing compulsions (exposure and response prevention homework)? | 56 (62.9) | |
| Ask you to track the distress your OCD symptoms caused between sessions? | 39 (43.8) | |
Discussion
To our knowledge, this is the first longitudinal, observational study to assess adherence to CBT (or any psychotherapy) recommendations in a large clinical sample of patients receiving treatment for OCD. Results suggest that more than half of patients with clinically significant OCD symptoms endorsed receiving CBT recommendations suggesting that clinicians are making specific referrals for CBT to individuals with OCD. Our hypothesis that a substantial number of participants who were recommended CBT would fail to initiate treatment was not supported: 74% of the 120 participants who endorsed receiving CBT recommendations stated that they attended at least one session of CBT during the 2 years of follow-up. Although the mean number of CBT sessions over 2 years of follow-up was 33, less than one third of CBT participants reported receiving a “dose” of CBT sessions consistent with the APA Practice Guidelines (2007) for OCD (at least 13 weekly sessions), suggesting that the intensity of CBT delivered in outpatient mental health settings may be strikingly different from treatments delivered in clinical trials that have largely consisted of intensive (daily) EX/RP sessions or twice-weekly CBT sessions (Abramowitz et al., 2003; Foa et al., 2005; Freeston et al., 1997; Koran, Hanna, Hollander, Nestadt, & Simpson, 2007; Simpson, Foa, et al., 2008). These results are even more striking given the fact that our sample consisted of individuals who were already in treatment at mental health specialty centers and the fact that 70% of our sample was recruited from a hospital-based OCD specialty clinic that provided pharmacotherapy and routinely refers patients to experienced CBT therapists in the community. It is likely that study participants had greater access to CBT than individuals who live in rural areas or are not in close proximity to anxiety specialty centers. Thus, our findings may overestimate rates of CBT recommendations for OCD and access to CBT providers.
It is unclear why many patients, despite being symptomatic, reported attending sessions at less intensive schedules than what is recommended by the APA guidelines (at least weekly). Frequency of visits was similar for patients with a CBT history and patients who entered CBT for the first time suggesting that some patients may begin CBT with infrequent visits that is in contrast to the structure of CBT in clinical trials. One difference between clinical trials and treatment in naturalistic clinical settings is the structured schedule of visits (e.g., twice weekly) and specific time-limited protocol for EX/RP (e.g., 15 sessions) versus open-ended treatment duration. Clinicians in naturalistic settings may not typically start EX/RP treatment by informing patients that they need to attend weekly/twice-weekly sessions of EX/RP sessions for a specific number of sessions and may accept patients who are less motivated to enter consistent treatment. Given that the efficacy of less than weekly sessions of EX/RP is unknown, future studies examining the acute and long-term impact of less frequent EX/RP would be useful data for clinicians and patients.
Our hypothesis that self-reported CBT drop-out rates would be greater than attrition rates reported in clinical trials using intensive schedules of EX/RP was supported. In this study, 31% of individuals who endorsed initiating CBT treatment reported that they dropped out of CBT before completing therapy. Our rates were significantly greater than the attrition rates of two of the three clinical trials using intensive (five times per week) sessions of EX/RP but were not significantly greater than the attrition rate reported by Abramowitz and colleagues (2003). One reason for the discrepancy may be that individuals who chose to enter intensive sessions may be more motivated for treatment as they are willing to dedicate a significant time commitment and tolerate massed sessions of EX/RP.
Our study is also the first to systematically evaluate patient perceptions of barriers to initiating CBT treatments for OCD. Our hypothesis that environmental barriers and fears regarding treatment would be the reasons most endorsed for not initiating CBT or dropping out of CBT was partially supported. Environmental barriers were the most frequently endorsed reasons for CBT nonadherence and the majority of participants also identified this reason as being the most influential in their decisions. Specifically, lack of health insurance coverage (this included not being able to find an “in-network” CBT provider) or difficulty scheduling appointments (e.g., unable to get time off from work) were frequently cited as reasons for not initiating CBT but financial costs were less frequently cited by self-identified CBT dropouts suggesting that once individuals make it in the door, the costs are manageable. These findings are consistent with surveys that suggest as many as 16% of the U.S. population lack health insurance, and mental health coverage is often limited even for the insured (Frank & McGuire, 1994; Kessler et al. 1997). In the United States, psychotherapy benefits typically vary across health insurance plans (e.g., limited number of sessions per year, higher copayments than medication visits). Studying the impact of health reform initiatives on utilization of psychotherapy or comparing utilization of psychotherapy under different health care systems (e.g., European vs. United States) are potential areas for future research.
We were surprised to find that approximately one quarter of participants who did not initiate CBT and one third of those who reported dropping out of CBT reported difficulty attending CBT sessions as the main reason for nonadherence (i.e., they were “too busy” to attend CBT sessions, could not find child care, too far to travel, conflicted with work schedule). While it is possible that participants may report inconvenience as a more acceptable excuse than other reasons (e.g., fear of CBT), these findings, coupled with the finding that most patients were on psychotropic medications, nonetheless highlight the differences in time commitments and out-of-pocket financial costs required for CBT and for pharmacological treatments. In this study, participants were recruited from a small geographical area where availability of CBT and pharmacological providers may have been similar. However, committing to attending sessions (typically scheduled during business hours) a few times per year versus once per week may yield different cost–benefit appraisals or be impractical for some individuals. Other potentially useful augmenting strategies for patients who have difficulty attending sessions regularly may be to use computerized telephone administration systems (e.g., BT-STEPS; Bachofen et al., 1999) or web-based CBT programs for patients who have difficulty attending sessions. Although data from open trials suggest that this treatment is acceptable and efficacious for OCD, controlled data suggest it may be less potent than therapist-administered CBT (Bachofen et al., 1999; Baer & Greist, 1997; Greist et al., 2002). However, some patients (e.g., highly motivated, less severe symptoms) may benefit from computer-based treatments and some clinicians may find these programs to be useful methods to extend to therapy sessions (e.g., to increase frequency of EX/RP in-between sessions).
Fear of engaging in CBT was endorsed by more than one quarter of participants who failed to initiate CBT and those who prematurely terminated CBT. In addition, most individuals who endorsed this as a reason for nonadherence also selected this reason as the most influential in their decision, making it the second most frequently endorsed “main reason” for dropping out of CBT. Possible explanations for this finding may be related to the nature of CBT for OCD, as well as the way treatment is described by the referral source. We believe these results highlight significant barriers to treatment that need to be targeted to improve CBT adherence and that such research may yield valuable information for the development of alternative or adjunctive treatment strategies (e.g., improving distress tolerance skills). For example, the manner in which the treatment is described to OCD patients by referees is likely related to the fear of engaging in CBT. In addition, other referee characteristics such as familiarity with CBT techniques, knowledge regarding efficacy literature, and attitudes regarding medications for OCD are likely to affect how the treatment is described to the prospective patient, and therefore the degree of confidence and anxiety the patient experiences. Finally, studies examining different methods (e.g., written, verbal, video) of prescribing CBT and their effects on treatment initiation may also yield valuable information for clinicians who recommend CBT to their clients.
For many patients, engaging in exposure therapy may prove too daunting (Kozak & Coles, 2005; Tolin & Hannan, 2005). Although in this study only 27% of CBT attendees endorsed using formal cognitive therapy (CT) techniques (thought records, downward arrows, or pie charts to challenge distorted thinking) during their CBT sessions, CT protocols that incorporate behavioral experiments have been shown to be efficacious for OCD and may be more acceptable to patients who are fearful of standard EX/RP (Abramowitz, Franklin, & Foa, 2002; Salkovskis, 1989; van Oppen & Arntz, 1994; Wilhelm & Steketee, 2006). In contrast, more than three quarters of CBT attendees endorsed self-administered EX/RP (i.e., being asked to practice EX/RP in-between sessions or encouraged to decrease avoidance of situations that triggered OCD symptoms). This data is in contrast to results from a survey study that two thirds of a sample of psychologists endorsed frequent use of cognitive restructuring techniques for OCD, 40% endorsed frequent use of relaxation training, and only 37% reported frequent use of EX/RP (Freihet, Vye, Swan, & Cady, 2004). As our data is based on patient reports of techniques used in treatment, it is unclear whether CT techniques are actually used less frequently in CBT sessions or whether it is easier for patients to identify exposure techniques. Future studies exploring therapist perspectives as well as patient perspectives of CBT techniques used in therapy would help clarify whether community therapists use systematic CT techniques less frequently than self-administered EX/RP or whether CT techniques are more susceptible to recall bias.
Emphasizing CT as an option prior to initiating EX/RP may be one way to improve adherence to CBT recommendations. Motivational interventions (MIs) may be a way for clinicians to improve adherence to treatment recommendations as well as CBT retention (Maltby & Tolin, 2005; Simpson, Zuckoff, Page, Franklin, & Foa, 2008), as these techniques have shown promise for facilitating treatment for other anxiety disorders (e.g., Buckner, 2009). In a recent open trial of MI integrated with EX/RP in six patients with OCD, Simpson and colleagues (Simpson, Zuckoff, et al., 2008) reported that four of six OCD patients who entered an open trial of MI integrated with standard EX/RP (18 sessions) completed treatment and a fifth patient reported minimal OCD symptoms at her last session (completed 13 sessions). More research is needed to characterize the individuals who are fearful of engaging in CBT, and such research may yield valuable information for the development of alternative or adjunctive treatment strategies (e.g., improving distress tolerance skills). The manner in which the treatment is described to OCD patients by referees may also be related to the fear of engaging in CBT. For example, the degree to which a referral source is familiar with the techniques of CBT, as well as the literature establishing its efficacy, is likely to have consequences for how the treatment is described to the prospective patient, and therefore the degree of confidence and anxiety he or she experiences. In order to minimize the possible negative effects of increased trepidation about undergoing CBT for OCD, we recommend that referees adopt a description similar to that proposed in the American Psychiatric Association’s Practice Guidelines for OCD (American Psychiatric Association, 2007), which state that “In describing CBT, the clinician should note that it involves confronting feared thoughts and situations, but at a tolerable rate. The therapist is a supportive coach, not a disciplinarian, and encourages behavior change and praises successes while validating the difficulty of confronting the OCD symptoms” (p. 22).
Results need to be interpreted within the context of study limitations. First, 70% of participants were recruited from an OCD specialty clinic specializing in pharmacotherapy and the majority were on SRIs for OCD; thus it is likely that the treatment preferences of participants in this study may lean toward medication. Patient preferences are likely to affect adherence rates and thus may have impacted our adherence rates. Although beliefs regarding utility of CBT were infrequently endorsed as “main” reasons for not initiating CBT, one third of participants who did not initiate CBT and one third of those who dropped out of CBT endorsed these reasons. Thus, it would be worthwhile to replicate our study at other sites that are known for their expertise in psychotherapy for anxiety disorders. Second, more than half of our sample endorsed attending at least one session of CBT for OCD prior to study entry but only 26% endorsed receiving at least 13 weekly sessions. Therefore, it is unclear whether these participants were CBT resistant and results may not generalize to “CBT-naïve” individuals. Third, patient adherence to CBT recommendations and utilization of CBT were based on self-reports and it is possible that data is influenced by social desirability or recall bias as participants were asked to recall the number and frequency of sessions over the past year. Thus, inferences regarding use of specific CBT techniques by CBT completers and dropouts are beyond the scope of this study and the collected data. An additional limitation is the fact that reports of actual techniques utilized during therapy were based on patient reports and we did not directly assess the quality of CBT provided, and limited data were collected on practitioners’ adherence to empirically supported treatment techniques. Therefore our results may be biased by participant report, and also failed to capture the use of other therapeutic techniques that have been demonstrated to be ineffective for OCD, such as relaxation training and thought stopping. Future work should incorporate clinician perspectives and objective measures of adherence to replicate our findings. Finally, due to the observational design of the study, we could not control when participants received a CBT referral and therefore excluded participants who were in CBT at study entry from the predictor analyses. Therefore, we may have missed predictors of CBT recommendations or initiating CBT as those participants who may have been more willing to enter CBT may have initiated CBT prior to study entry. We believe our results support the need for an experimental study to identify patient and provider characteristics that increase CBT adherence.
Acknowledgments
Supported by a grant (R01 MH060218) to Dr. Steven A. Rasmussen from the National Institute of Mental Health, Bethesda, MD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Maria C. Mancebo, Butler Hospital, Brown University Medical School
Jane L. Eisen, Brown University Medical School
Nicholas Sibrava, Butler Hospital, Brown University Medical School.
Ingrid R. Dyck, Brown University Medical School
Steven A. Rasmussen, Butler Hospital, Brown University Medical School
References
- Abramowitz JS, Foa EB, Franklin ME. Exposure and ritual prevention for obsessive–compulsive disorders: Effects of intensive versus twice-weekly sessions. Journal of Consulting and Clinical Psychology. 2003;71(2):394–398. doi: 10.1037/0022-006x.71.2.394. [DOI] [PubMed] [Google Scholar]
- Abramowitz JS, Franklin ME, Foa EB. Empirical status of cognitive–behavioral therapy for obsessive–compulsive disorder: A meta-analytic review. Romanian Journal of Cognitive and Behavioral Psychotherapy. 2002;2:89–104. [Google Scholar]
- American Psychiatric Association. Practice guideline for the treatment of patients with obsessive–compulsive disorder. American Journal of Psychiatry. 2007;164(Suppl):1–56. [PubMed] [Google Scholar]
- Bachofen M, Nakagawa A, Marks IM, Park JM, Greist JH, Baer L. Home self-assessment and self-treatment of obsessive–compulsive disorder using a manual and a computer-conducted telephone interview: Replication of a U.K.–U.S. study. Journal of Clinical Psychiatry. 1999;60:545–549. doi: 10.4088/jcp.v60n0807. [DOI] [PubMed] [Google Scholar]
- Baer L, Greist JH. An interactive computer-administered self-assessment and self-help program for behavior therapy. Journal of Clinical Psychiatry. 1997;58(Suppl. 12):23–28. [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66(1):7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Denys D, Van Megen H, Westenberg H. The adequacy of pharmacotherapy in outpatients with obsessive–compulsive disorder. International Clinical Psychopharmacology. 2002;17(3):109–114. doi: 10.1097/00004850-200205000-00003. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Dutra L, Bradley R, Westen D. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive–compulsive disorder. Clinical Psychology Review. 2004;24(8):1011–1030. doi: 10.1016/j.cpr.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Goodman WK, Keller MB, Warshaw M, DeMarco LM, Luce DD, et al. Patterns of remission and relapse in obsessive–compulsive disorder: A 2-year prospective study. Journal of Clinical Psychiatry. 1999;60(5):346–351. doi: 10.4088/jcp.v60n0514. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Marks AP, Schafer J. A comparison of behavioral group therapy and individual behavior therapy in treating obsessive–compulsive disorder. Journal of Nervous and Mental Disease. 1993;181(3):189–193. doi: 10.1097/00005053-199303000-00007. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured clinical interview for DSM-IV axis II personality disorders (SCID-II) New York: Biometrics Research Department, New York State Psychiatric Institute; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, et al. Structured clinical interview for DSM-IV axis I disorders–Patient edition (SCID/IP Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive–compulsive disorder. American Journal of Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Franklin ME, Abramowitz JS, Kozak MJ, Levitt JT, Foa EB. Effectiveness of exposure and ritual prevention for obsessive–compulsive disorder: Randomized compared with nonrandomized samples. Journal of Consulting and Clinical Psychology. 2000;68(4):594–602. [PubMed] [Google Scholar]
- Freeston MH, Ladouceur R, Gagnon F, Thibodeau N, Rheaume J, Letarte H, Bujold A. Cognitive–behavioral treatment of obsessive thoughts: A controlled study. Journal of Consulting and Clinical Psychology. 1997;65(3):405–413. doi: 10.1037//0022-006x.65.3.405. [DOI] [PubMed] [Google Scholar]
- Freiheit SR, Vye C, Swan R, Cady M. Cognitive–behavioral therapy for anxiety: Is dissemination working? The Behavior Therapist. 2004;27(2):25–32. [Google Scholar]
- Friedman S, Smith LC, Levine C, Paradis C, Viswanathan R, Trappler B, Ackerman R. Obsessive–compulsive disorder in a multi-ethnic urban outpatient clinic: Initial presentation and treatment outcome with exposure and ritual prevention. Behavior Therapy. 2003;34:397–410. [Google Scholar]
- Furnival GM, Wilson RW. Regressions by leaps and bounds. Technometrics. 1974;16:499–511. [Google Scholar]
- Goisman RM, Rogers MP, Steketee G, Warshaw M, Cuneo P, Keller MB. Utilization of behavioral methods in a multicenter anxiety disorders study. Journal of Clinical Psychiatry. 1993;54(6):213–218. [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown obsessive compulsive scale. II. Validity. Archives of General Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, et al. The Yale-Brown obsessive-compulsive scale: I. Development, use and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, Clary CM, et al. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63(2):138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression: Second edition. New York: Wiley; 2000. [Google Scholar]
- Huppert JD, Schultz LT, Foa EB, Barlow DH, Davidson JR, Gorman JM, Woods SW. Differential response to placebo among patients with social phobia, panic disorder, and obsessive–compulsive disorder. American Journal of Psychiatry. 2004;161(8):1485–1487. doi: 10.1176/appi.ajp.161.8.1485. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kessler R, Frank R, Edlund B, Katz S, Lin E, Leaf P. Differences in the use of psychiatric outpatient services between the United States and Ontario. New England Journal of Medicine. 1997;336:551–557. doi: 10.1056/NEJM199702203360806. [DOI] [PubMed] [Google Scholar]
- Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB. Practice guideline for the treatment of patients with obsessive–compulsive disorder. American Journal of Psychiatry. 2007;164(Suppl. 7):5–53. [PubMed] [Google Scholar]
- Kozak MJ, Coles ME. Treatment for OCD: Unleashing the power of exposure. In: Abramowitz JS, Houts AC, editors. Concepts and controversies in obsessive–compulsive disorder. New York: Springer; 2005. pp. 283–304. [Google Scholar]
- Maltby N, Tolin DF. A brief motivational intervention for treatment-refusing OCD patients. Cognitive Behavior Therapy. 2005;34(3):176–184. doi: 10.1080/16506070510043741. [DOI] [PubMed] [Google Scholar]
- Mancebo MC, Eisen JL, Pinto A, Greenberg BD, Dyck IR, Rasmussen SA. The Brown longitudinal obsessive compulsive study: Treatments received and patient impressions of improvement. Journal of Clinical Psychiatry. 2006;67(11):1713–1720. doi: 10.4088/jcp.v67n1107. [DOI] [PubMed] [Google Scholar]
- Mancebo MC, Pinto A, Rasmussen SA, Eisen JL. Development of the treatment adherence survey–Patient version (TAS-P) for OCD. Journal of Anxiety Disorders. 2008;22(1):32–43. doi: 10.1016/j.janxdis.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellman LA, Beresin E. Psychotherapy competencies: Development and implementation. Academic Psychiatry. 2003;27(3):149–153. doi: 10.1176/appi.ap.27.3.149. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman WH, Maddever H. The modified Hamilton rating scale for depression: Reliability and validity. Psychiatry Research. 1985;14(2):131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Orloff LM, Battle MA, Baer L, Ivanjack L, Pettit AR, Buttolph L, Jenike MA. Long-term follow-up of 85 patients with obsessive–compulsive disorder. American Journal of Psychiatry. 1994;151:441–442. doi: 10.1176/ajp.151.3.441. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. Behaviour therapy and obsessional ruminations: Can failure be turned into success? Behaviour Research and Therapy. 1989;27:149–160. doi: 10.1016/0005-7967(89)90073-9. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS version 9.13 (Version 9.13) Cary, NC: Author; 2007. [Google Scholar]
- Seligman ME. Science as an ally of practice. American Psychologist. 1996;51(10):1072–1079. doi: 10.1037//0003-066x.51.10.1072. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Foa EB, Liebowitz MR, Ledley DR, Huppert JD, Cahill S, Hembree E, et al. A randomized, controlled trial of cognitive–behavioral therapy for augmenting pharmacotherapy in obsessive–compulsive disorder. American Journal of Psychiatry. 2008;165(5):621–630. doi: 10.1176/appi.ajp.2007.07091440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding motivational interviewing to exposure and ritual prevention for obsessive–compulsive disorder: An open pilot trial. Cognitive Behavior Therapy. 2008;37(1):38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Keller MB. The psychosocial treatments interview for anxiety disorders. A method for assessing psychotherapeutic procedures in anxiety disorders. Journal of Psychotherapy Practice and Research. 1997;6(3):194–210. [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Merlo LJ, Lehmkuhl H, Geffken GR, Jacob M, Ricketts E, Goodman WK, et al. Cognitive–behavioral therapy for obsessive–compulsive disorder: A non-randomized comparison of intensive and weekly approaches. Journal of Anxiety Disorders. 2008;22(7):1146–1158. doi: 10.1016/j.janxdis.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Hannan S. What is in a name? The distinction between self-directed and self-conducted treatment. In: Abramowitz JS, editor. Concepts and controversies in obsessive compulsive disorder. New York: Springer; 2005. pp. 347–351. [Google Scholar]
- Tolin DF, Hannan S, Maltby N, Diefenbach GJ, Worhunsky P, Brady RE. A randomized controlled trial of self-directed versus therapist-directed cognitive–behavioral therapy for obsessive–compulsive disorder patients with prior medication trials. Behavior Therapy. 2007;38(2):179–191. doi: 10.1016/j.beth.2006.07.001. [DOI] [PubMed] [Google Scholar]
- van Oppen P, Arntz A. Cognitive therapy for obsessive–compulsive disorder. Behaviour Research and Therapy. 1994;32:79–97. doi: 10.1016/0005-7967(94)90086-8. [DOI] [PubMed] [Google Scholar]
- van Oppen P, van Balkom AJ, de Haan E, van Dyck R. Cognitive therapy and exposure in vivo alone and in combination with fluvoxamine in obsessive–compulsive disorder: A 5-year follow-up. Journal of Clinical Psychiatry. 2005;66(11):1415–1422. doi: 10.4088/jcp.v66n1111. [DOI] [PubMed] [Google Scholar]
- Warren R, Thomas JC. Cognitive–behavior therapy of obsessive–compulsive disorder in private practice: An effectiveness study. Journal of Anxiety Disorders. 2001;15(4):277–285. doi: 10.1016/s0887-6185(01)00063-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28(6):531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Wilhelm S, Steketee G. Cognitive therapy for obsessive–compulsive disorder: A guide for practitioners. Oakland, CA: New Harbinger; 2006. [Google Scholar]


