Abstract
Background
To establish, characterize and elucidate potential mechanisms of acquired bleomycin (BLM) resistance using human cancer cell lines. Seven BLM-resistant cell lines were established by exposure to escalating BLM concentrations over a period of 16-24 months. IC50 values and cell doubling times were quantified using a real time cytotoxicity assay. COMET and γ-H2AX assays, cell cycle analysis, and apoptosis assessment further investigated the mechanisms of BLM resistance in these cell lines.
Results
Compared with parental cell lines, real time cytotoxicity assays revealed 7 to 49 fold increases in IC50 and a mean doubling time increase of 147 % (range 64 %-352%) in BLM-resistant sub-clones (p<0.05 for both). Higher maintenance BLM concentrations were associated with higher IC50 and increased doubling times (p<0.05). Significantly reduced DNA damage (COMET and γ-H2AX assays), G2/M arrest, and apoptosis (p<0.05 for each set of comparison) following high-dose acute BLM exposure was observed in resistant sub-clones, compared with their BLM-sensitive parental counterparts. Three weeks of BLM-free culturing resulted in a partial return to BLM sensitivity in 3/7 BLM-resistant sub-clones (p<0.05).
Conclusion
Bleomycin resistance may be associated with reduced DNA damage after bleomycin exposure, resulting in reduced G2/M arrest, and reduced apoptosis.
Introduction
Bleomycin (BLM) is a glycopeptide antibiotic isolated from Streptomyces verticillis [1,2]. As a chemotherapeutic agent, it is used in the treatment of multiple tumors, including but not limited to testicular carcinomas, lymphomas, and head and neck cancers [3,4]. Although the full pathway of the drug’s mechanism of action has not been elucidated, BLM does bind to iron and oxygen to produce reactive oxygen species (ROS) [5] that induces single- and double-strand DNA breaks, with the latter being primarily responsible for its anti-tumor effects [6,7]. It also causes lipid peroxidation and mitochondrial DNA damage [8]. Extended cell-cycle arrest/senescence, apoptosis and mitotic cell death are the most common cellular responses to BLM treatment [9].
BLM was found to induce G2/M cell cycle arrest in cancer cell lines [10,11]. This may be explained by a G2/M checkpoint response to DNA damage. The G2/M checkpoint is important for genomic stability, for it ensures that chromosomes are intact and ready for separation before cells enter mitosis [12]. Unlike the G1 checkpoint, G2/M checkpoint genes are often not mutated in cancer cells [13].
Resistance to BLM is a clinical concern, and typically occurs during relapse in germ cell tumors, where BLM is most commonly used clinically. Although the mechanism of BLM-resistance is unclear, several possibilities have been put forward, including: (a) altered BLM intake and efflux [14,15]; (b) elevated antioxidant level [5,11]; (c) enhanced repair ability for BLM-induced DNA damage [14,16,17]; and (d) increased metabolism (inactivation) of BLM [17–19].
The development of BLM resistance serves as an important mechanism for the evasion of chemotherapeutic eradication in cancer cells. However, the mechanisms responsible for acquired BLM resistance in human tumor cells have not been well investigated. In this study, we established BLM-resistance in seven human cancer cell lines, including lines of tumor types currently treated with BLM and others known to be either sensitive or resistant to BLM. Moreover, we characterized these cell lines with regard to their level of BLM-resistance, BLM-induced DNA damage, doubling time, cell cycle distribution, and degree of apoptosis (before and after BLM treatment) to increase our understanding of the potential mechanisms of resistance.
Materials and Methods
Cells and cell culture
Seven commercially-available human cancer cell lines with wide differences in innate sensitivity/resistance to BLM (HOP62, ACHN, NT2/D1, SF-295, NCCIT, NCI-H322M, and MBA-MB-231) were chosen from National Cancer Institute (NCI) or American Type Culture Collection (ATCC) [20]. Two (NT2/D1, NCCIT) were testicular cell lines (Table 1).
Table 1. Description of Cell Lines.
| Cell line | Abbreviation (Parental/Resistant) | Derived from which cancer type | Parental IC50(µg /ml) * |
|---|---|---|---|
| ACHN | ACHN0 | Renal cell carcinoma | 0.009 |
| ACHN0.25 | |||
| HOP-62 | HOP0 | Lung adenocarcinoma | 0.11 |
| HOP0.05 | |||
| SF-295 | SF0 | CNS glioblastoma | 0.14 |
| SF0.4 | |||
| NT2/D1 | NT20 | Germ cell carcinoma | N/A |
| NT20.1 | |||
| NCCIT | NCCIT0 | Germ cell carcinoma | N/A |
| NCCIT1.5 | |||
| NCI-H322M | H322M0 | Lung adenocarcinoma | 25.8 |
| H322M2.5 | |||
| MDA-MB-231 | MB2310 | Breast adenocarcinoma | 27.9 |
| MB2313.0 |
Note: Cell lines with subscript “0” indicate parental (control) lines (e.g.,HOP0). The resistant sub-clones have a subscript identifying its maintenance BLM concentration, in µg/ml (e.g., HOP0.05). *Data obtained from NCI-60 drug screening panel [20].
NT2/D1 was maintained in Dulbecco’s Modified Eagle’s Medium (DMEM). Other lines were cultured in RPMI 1640. The conditions were 10% fetal bovine serum (FBS), 1% penicillin/streptomycin at 37°C in 5% CO2. Cells were grown as monolayers in 75 cm2 cell culture flasks unless otherwise stated. All cell lines tested negative for mycoplasma contamination by Polymer Chain Reaction (PCR) methods [21]. Cell lines were authenticated using Short Tandem Repeats (STR) testing [22].
Establishment of bleomycin-resistant sub-clones from parental (control) cell lines
To develop BLM-resistance, cells were continually exposed to stepwise increases in the concentration of BLM over a period of 16 to 24 months. Briefly, cells were seeded at a density of ~5 ×105/ml in a T75 cell culture flask with 10ml complete growth medium. After 4-6 hours of incubation, relatively low concentrations of BLM (ranging from 0.01 to 0.1µg/ml depending on the innate BLM-sensitivity), dissolved in phosphate-buffered saline (PBS) without Ca2+ and Mg2+, were added into the medium. Cells were left in BLM for 2 to 4 weeks or until a stable cell re-population formed. Regular medium replenishment was performed throughout this period. The BLM concentration was then increased by 0.5 to 2 fold. This stepwise dose escalation continued for 16 to 24 months until the BLM concentration reached at least ten times the starting concentration. Thereafter, all BLM-resistant cell lines (“BLM-resistant sub-clones”) were maintained in their highest achieved BLM concentration (“maintenance dose”). At the same time, regular passage of the parental cell lines were performed in parallel with the BLM-resistance establishment process.
BLM sensitivity test and doubling time analysis
Prior to the BLM resistance/sensitivity assessment (cytotoxicity assay), a cell proliferation assay was carried out on the xCELLigence system (Roche, USA) to identify the optimal conditions under which the real-time cytotoxicity assay should be running. Specifically, the proliferation assay was performed: a) to identify the optimal seeding density for the cytotoxicity assay for each of the cell lines; and b) to determine the duration of the cytotoxicity assay.
The proliferation assay was carried out by seeding various numbers of cells into a 96-well plate (E-plate 96, Roche, USA) in quadruplicate, followed by real time monitoring of cellular growth for up to 7 days. Twenty-four hours after the seeding, half of the wells on the plate were treated with BLM to determine the cellular response. The proliferation assay was repeated twice on each cell line. Optimal seeding densities for each line were selected on the basis of dramatic changes in proliferation at 72-96 hours after BLM treatment and small variations across replicate wells.
For cytotoxicity assays, the cell count was first performed, and cells were then seeded into triplicate wells with 180µl of BLM-free cell culture medium on a 96-well plate. Twenty-four hours after initial plating, 20µl of cell culture medium containing serially diluted BLM ranging from 0 to 800 µg/ml were added into each well. The number of viable live cells was monitored every 15 minutes, for a total of at least 120 hours. IC50 (integrated software, xCELLigence system) and fold differences in IC50 between BLM-resistant and parental (control) cell lines (IC50 BLM-resistant / IC50 control) were subsequently calculated. The fastest growth period observed for each of the cell lines in the proliferation assay was isolated for doubling time determination and its percentage change was calculated using xCELLigence system software.
Comet assay assessment of BLM-induced DNA damage
BLM is known to cause DNA damage in cells [6,7]. To determine initial (baseline) and DNA strand breaks after high dose BLM expose, alkaline Comet assays (single-cell gel electrophoresis) were performed [23] for each of the parental and resistant sub-clones. Olive Tail Moment (OTM) values of one hundred cells were scored at random per slide using fluorescence microscope with KOMET 5.0 software (Kinetic Imagine).
BLM-induced γ-H2AX foci formation
DNA double-strand breaks (DSBs) triggers the cellular formation of γ-H2AX foci (phosphorylated H2AX protein) [24]. To confirm the cellular DNA damage response to BLM through the Comet assay, quantitative analysis of γ-H2AX foci formation following high dose BLM exposure was performed on a subset of four parental/resistant pairs (HOP, ACHN, NCCIT, and H322M) [25] using Phospho-Histone H2AX pSer139 Monoclonal Antibody and Alexa Flour 488-conjugated anti-phospho-H2AX (BioLegend, San Diego, CA, USA). A minimum of 10000 events were counted on flow cytometer for each measurement; the intensity of γ-H2AX, which directly correlates with cytometry counts, was analyzed using Cell Quest software (BD, USA).
Cell cycle distribution analysis
Cell cycle distributions of each of pair of seven parental and resistant sub-clones were tested pre- and post- 24 hours of high dose BLM exposure at ten times the resistant sub-clones’ maintenance concentration. Then, cells in the mono-dispersed suspension were fixed with ethanol, followed by propidium iodide (PI) staining (PI, Sigma, USA) and analyzed using the FACScalibur flow cytometer (BD, USA). Percentages of cells resting in G1, S and G2/M phase were determined (CellQuest software, BD, USA and ModFit LT software, Verity Software House). Cell cycle distribution was measured in each parental/BLM-resistant pair at baseline and at different time points up to 24 hours of BLM treatment. Correlations between cell cycle distribution, IC50 values, and cell line doubling times were analyzed.
Annexin V/PI assay for BLM-induced apoptosis
To determine cell apoptosis pre- and post- BLM treatment, a representative subset of four parental/resistant pairs (HOP, ACHN, NCCIT, and H322M) was treated with 24 hours of high- dose BLM. The cells were then stained with Annexin V–FITC and PI, and evaluated for apoptosis by flow cytometry according to the manufacturer's protocol (BD PharMingen, San Diego, CA, USA). Both early (Annexin V-positive, PI-negative) and late apoptotic cells (Annexin V-positive, PI-positive) were counted as apoptotic cells.
Statistical Analysis
To assess treatment significance or difference, paired T-tests or unpaired T-tests (depending on the experimental specifications) were performed with a two-sided significance level of 0.05. Normality assumptions were assessed via Shapiro-Wilks tests. When the normality assumption could not be held, paired or unpaired Wilcoxon rank-sum tests were performed instead. For Comet assay assessment between parental and resistant sub-clones after high-dose BLM treatment, p-values were calculated using a t statistic for non-equal variances, testing the null hypothesis of equality on log ratios. Logistic regression was performed to assess baseline G2/M distribution differences between parental and resistant sub-clones. To investigate correlation between various measures (IC50 control, IC50 change following high-dose BLM treatment, doubling time, and cell cycle distribution), linear regression analyses were performed. All analyses were conducted using SAS version 9.2 or SPSS version 13.0.
Results
BLM-resistant cell lines maintained on BLM stably displayed higher IC50 values and prolonged doubling times
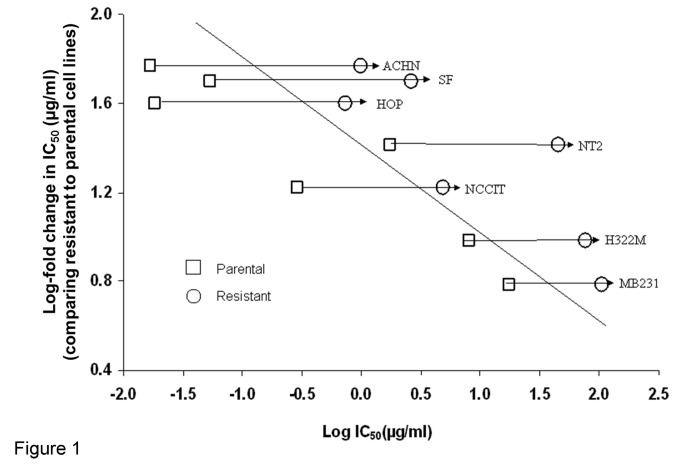
All seven BLM-resistant sub-clones demonstrated greater IC50 than their parental counterparts (Figure 1). Cytotoxicity assays showed between 7-49 fold increases of IC50 in BLM-resistant sub-clones. A positive correlation was observed between the maintenance BLM concentration and IC50 values (p<0.001, R2=0.58). After prolonged BLM exposure, cell lines with greater parental sensitivity to BLM (mean IC50, 0.1µg/ml) exhibited a greater increase in resistance (mean of 48 fold) compared to parental lines that were less sensitive (mean IC50, 9µg/ml, 15 fold; p<0.05 comparing parental sensitive to less sensitive lines).
Figure 1. Correlation between IC50 fold increase and IC50 values of control cell lines.
Linear regression models determined that higher values of IC50 were associated with lower values of fold change (logarithm scale slope of: -0.11 (standard error: 0.02), P < 0.0001, R2= 0.58). Each IC50 value is the mean of experiments performed in triplicate.
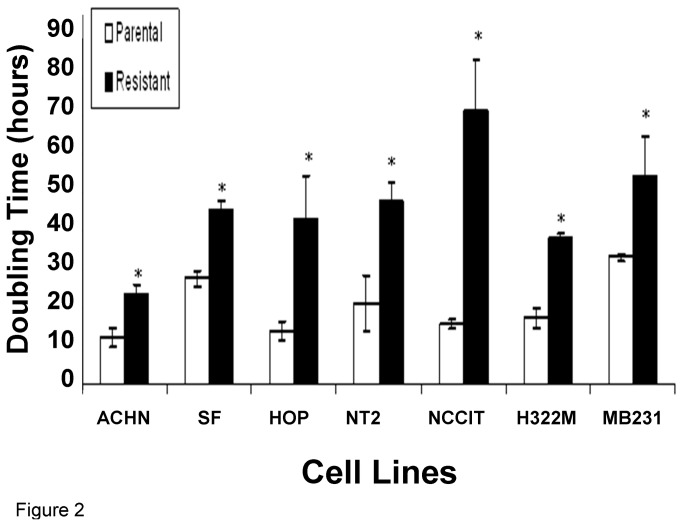
It was observed that BLM-resistant sub-clones grew slower than their parental cell lines. Two cell lines, when maintained in higher concentrations of BLM, such as MB2313.0 and H322M2.5 (subscripts denote maintenance BLM concentration), also exhibited enlarged and flattened cell morphology resembling that of cell senescence compared to their parental lines, but only after many generations. In contrast, acute exposure to high doses of BLM did not result in morphological changes. The slower cellular growth was confirmed by cell doubling time calculated with the xCELLigence system. All BLM-resistant sub-clones displayed statistically significant doubling time prolongation with a mean doubling time increase of 147% (range: 64%-352%) when compared with their parental cell lines (Figure 2, p<0.05). There was no correlation between cell doubling time and IC50 values, and none between the percentage increase in doubling time and fold increase in IC50.
Figure 2. Average doubling time of parental (control) and BLM-resistant sub-clones.
Mean doubling time ± standard error of the mean (SEM, n=3) was reported. The mean doubling time (measured in hours) of the parental lines was shorter than that of BLM-resistant sub-clones in all seven cell lines. * P<0.05 compared to parental.
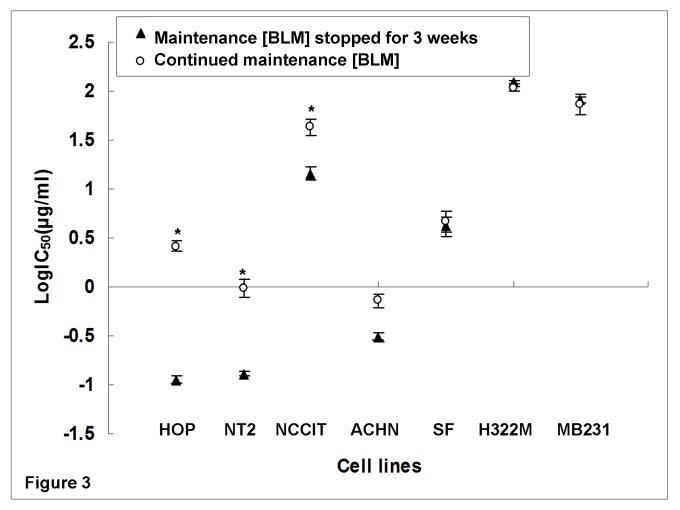
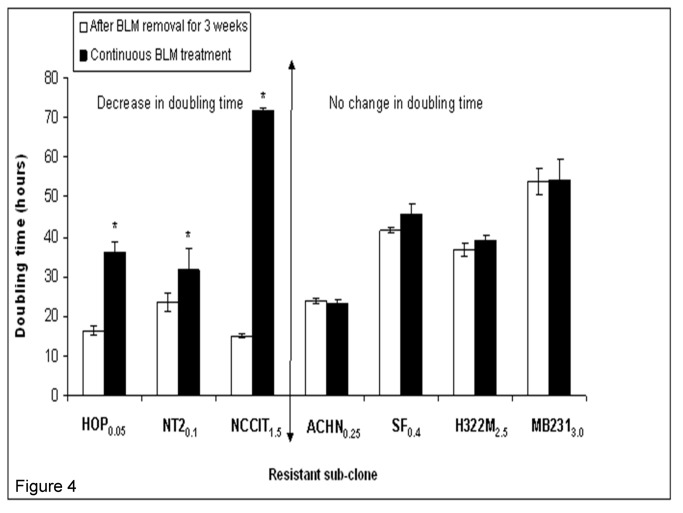
To test the stability of BLM resistance in BLM-resistant sub-clones, comparisons in IC50 values and doubling times were made between normally maintained BLM-resistant sub-clones and the same resistant sub-clones which were subsequently cultured in BLM-free medium for three weeks. After three weeks of BLM-free culturing, three of the originally resistant sub-clones (including both testicular cell lines NT20.1, NCCIT1.5 and the lung cancer cell line HOP0.05) exhibited a significant IC50 reduction (Figure 3) and doubling time reduction (Figure 4), when compared to regularly maintained BLM-resistant sub-clones. There were no statistically significant changes in IC50 and doubling time in the remaining four lines.
Figure 3. Effects of 3-week discontinuation of maintenance BLM treatment on IC50 (µg/ml).
Experiments were performed in triplicate. Log IC50 comparisons were performed. Three (HOP0.05, NT20.1, and NCCIT1.5) of the seven cell lines had significant reductions in IC50 values following three weeks of BLM-free maintenance. * P<0.05 for comparisons between BLM resistant sub-clones and their corresponding counterparts with three weeks of treatment break.
Figure 4. Effects of 3-week discontinuation of maintenance BLM treatment on doubling time.
Experiment was performed in triplicate. Three (HOP0.05, NT20.1, NCCIT1.5) of the seven cell BLM-resistant lines exhibited significant decrease in doubling time following three weeks of BLM-free treatment. * P<0.05 compared to after removal BLM for 3 weeks cell lines.
BLM resistance may be dose-dependent
Given that a general correlation exists between IC50 values and the maintenance BLM concentrations across 7 cell lines (Figure 1), the possibility of dose-dependent BLM resistance was tested. For the single cell line ACHN, IC50 values were obtained from ACHN0 (parental line), and its two resistant sub-clones, ACHN0.1 and ACHN0.25. A positive correlation was found between the maintenance BLM concentrations (0, 0.1 and 0.25µg/ml) and their IC50 values (0.01, 0.29, and 0.74µg/ml respectively, p<0.05). Moreover, a positive correlation was also observed between BLM maintenance concentrations and doubling times (0µg/ml-12hrs, 0.1µg/ml-16.5hrs, 0.25µg/ml-23.5hrs, p<0.05). This finding was not tested or confirmed in any of the other cell lines.
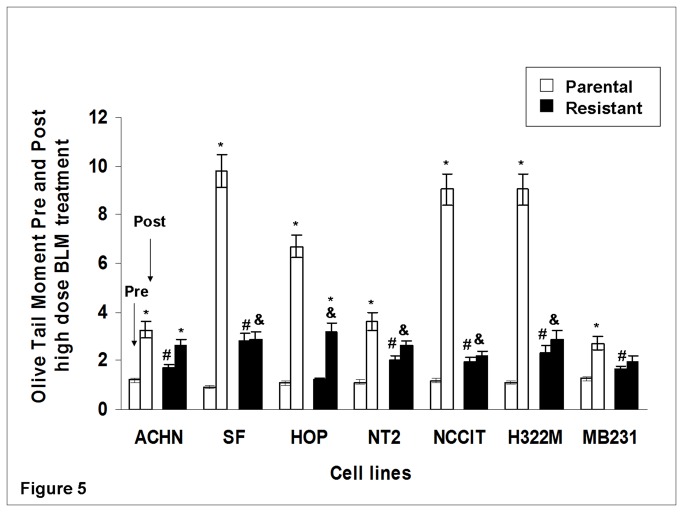
BLM-resistant sub-clones had less BLM-induced DNA damage in Comet assays
Quantification of DNA damage in all seven parental/resistant pairs using Comet assay (measured in OTM) showed that prior to BLM treatment, six of the seven resistant cell lines had higher basal DNA damage compared with control (the exception was HOP0.05, p<0.05). This generally correlated with the prolonged basal cell doubling time observed in these resistant sub-clones. Following high dose BLM treatment, five of seven resistant sub-clones (SF0.4, HOP0.1, NT20.1, NCCIT1.5, and H322M2.5) had lower DNA damage than their parental lines. No increase in DNA damage after BLM exposure was observed in five of seven resistant lines (SF0.4, NT20.1, NCCIT1.5, H322M2.5, and MB2313.0). In contrast, all parental cell lines had greater DNA damage post- BLM than pre- BLM (p<0.05 for each comparison; Figure 5). Further, all seven parental lines displayed significantly greater DNA damage increase post- BLM treatment when compared to their resistant counterparts (p<0.05).
Figure 5. DNA damage in Olive Tail Moment (OTM) pre- and post- high dose BLM treatment assessed by comet assay.
Experiments were run in triplicates. Cells were subject to high dose BLM exposure (corresponding to ten times their respective maintenance concentrations) for 24 hours. OTM was used for DNA fragmentation (damage) quantification, and was calculated as: OTM = (Tail.mean - Head.mean) × (Tail %DNA)/100. Comet assay revealed greater increase in DNA fragmentation (expressed in OTM levels) after BLM treatment in all parental lines.* P<0.05 for comparison between cell lines prior and after high dose BLM treatment. All parental lines exhibited significant increase in DNA damage. # P<0.05 for comparison between parental and resistant cell lines at baseline (pre-treatment). All BLM-resistant lines except for HOP0.05 exhibited increased DNA damage at baseline compared to their parental lines. & P<0.05 for comparison between resistant cell lines and parental cell line post BLM treatment. Less DNA damage (compared to their parental lines) post- BLM treatment was found in five of seven BLM-resistant cell lines (SF0.4, HOP0.1, NT20.1, NCCIT1.5, and H322M2.5).
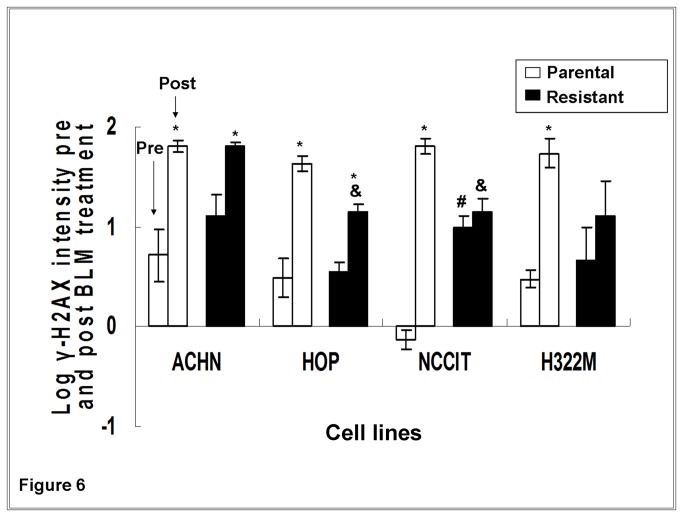
BLM-resistant sub-clones had reduced γ-H2AX levels compared to their parental lines following high dose BLM treatment
As a second measure of cellular response to DNA damage, γ-H2AX was also assessed in a subset of four cell lines (HOP, ACHN, NCCIT and H322M). Following 24 hours of high dose BLM treatment, γ-H2AX intensities increased in all parental cell lines. In the resistant sub-clones, increased γ-H2AX intensities were only observed in two of four lines (ACHN0.25 and HOP0.05,Figure 6). This is in agreement with the Comet assays. Three (HOP0.05, NCCIT1.5, and H322M2.5) of the four resistant sub-clones exhibited significantly less change in γ-H2AX intensity (γ-H2AX intensity post-treatment minus pre-treatment) compared with their parental sub-clones post- BLM treatment (p<0.05). This trend was borderline significant in the fourth line (H322M2.5, p=0.054).
Figure 6. γ-H2AX formation pre- and post- high dose BLM treatment assessed by flow cytometry.
Experiments were run in triplicate. Cells were subject to high dose BLM exposure (corresponding to ten times their respective maintenance concentrations) for 24 hours. Flow cytometric detection of BLM-induced γ-H2AX foci formation were then obtained in a subset of four cell lines (ACHN, HOP, NCCIT and H322M). * P<0.05 for comparison between cell lines prior and after high dose BLM treatment. All parental lines exhibited significant increase in formation of γ-H2AX. # P<0.05 for comparison between parental and resistant cell lines at baseline (pre-treatment). One of four BLM-resistant cell lines (NCCIT1.5) had greater γ-H2AX formation than its parental counterpart at baseline. & P<0.05 for comparison between resistant and parental cell lines following BLM treatment. Two of four BLM-resistant cell lines (HOP0.1 and NCCIT1.5.) revealed significantly less γ-H2AX formation than their parental counterparts post BLM treatment, with a third line (H322M2.5) being borderline significant (p=0.054).
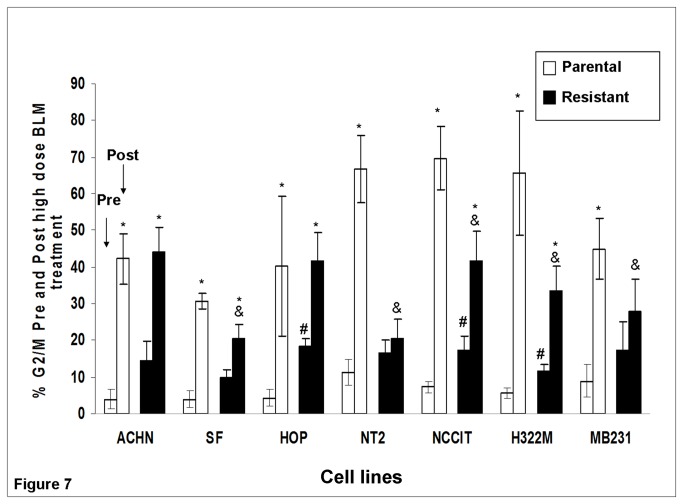
BLM-resistant cell lines had a lower percentage of G2/M arrest following high dose BLM exposure
Since cell cycle arrest at G2/M phase was a characteristic general cellular response to BLM exposure, the ability of BLM-resistant sub-clones to suppress BLM-induced G2/M arrest was evaluated. As shown in Figure 7, three of seven BLM-resistant sub-clones (HOP0.05, NCCIT1.5, and H322M2.5) exhibited greater G2/M phase distribution at baseline, compared with their parental lines (p<0.05). Similarly, for the other four cell lines, the resistant sub-clones also exhibited greater G2/M phase distribution at baseline, though non-significantly. After 24 hours of high dose BLM exposure, five (SF0.4, NT20.1, NCCIT1.5, H322M2.5, and MB2313.0) of seven BLM-resistant sub-clones exhibited a lower G2/M distribution than their corresponding parental lines (p<0.05). Comparing the % G2/M distribution before and after 24 hours of high dose BLM treatment, all parental cell lines exhibited increases in G2/M distribution following the treatment (p<0.05).The same trend was seen in all resistant sub-clones, although two (NT20.1 and MB2313.0) were non-significant. The extent of % G2/M distribution increase (calculated as % G2/Mpost-treatment minus % G2/Mpre-treatment) was smaller for all resistant sub-clones than their corresponding parental lines (p<0.05).
Figure 7. Summary of % G2/M phase distribution pre- and post- high dose BLM treatment in all 7 parental/resistant pairs.
High dose BLM treatment corresponds to ten times the corresponding maintenance concentration for each cell line. Mean ± SEM (n=3) values are reported. * P<0.05 for the comparison between cell lines prior to and after high dose BLM treatment. All parental lines exhibited significant increases in G2/M cell cycle distribution. # P<0.05 for comparison between parental and resistant cell lines at baseline (pre-treatment). Three of seven BLM-resistant cell lines (HOP0.05, NCCIT1.5, and H322M2.5) exhibited increased % G2/M distribution at baseline compared to their parental cell lines. & P<0.05 for comparison of % G2/M distribution between parental and resistant cell lines after BLM treatment. Less % G2/M distribution than parental lines was found in five out of seven BLM-resistant cell lines (SF0.4, NT20.1, NCCIT1.5, H322M2.5, and MB2313.0) after BLM treatment.
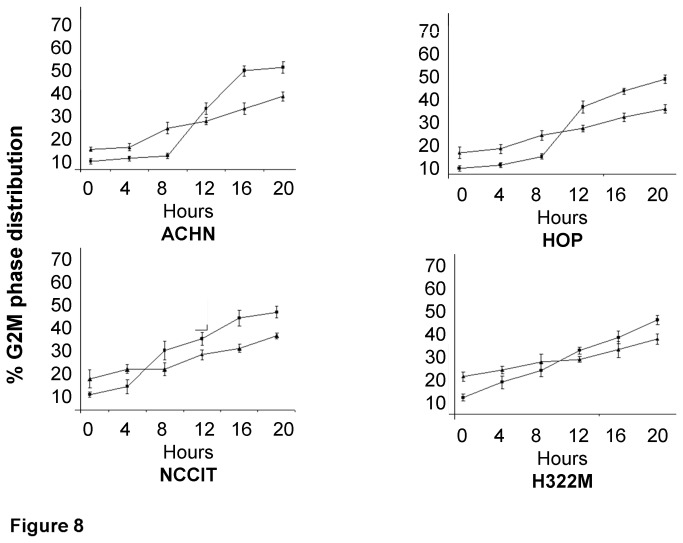
G2/M arrest becomes prominent after 8 hours of high dose BLM treatment
To evaluate the timing of G2/M arrest after high dose BLM exposure, four cell lines (the innately BLM sensitive HOP and ACHN lines, the NCCIT testicular line and the innately BLM resistant H322M, the same lines evaluated for the γ-H2AX experiment) underwent a time course analysis. Although there was increasing G2/M arrest in both parental and BLM-resistant sub-clones (Figure 8), this arrest was most prominently seen between 8 and 12 hours after BLM treatment in parental cells.
Figure 8. Time course measurement of % G2/M distribution in four parental/resistant cell line pairs at 0 (baseline) 4, 8, 12, 20, and 24 hours following high dose BLM treatment.
Experiments were run in triplicate. G2/M distribution was found to be higher in parental lines (compared to resistant sub-clones) 8 hours after BLM treatment.
Reduced apoptosis was found in BLM-resistant sub-clones
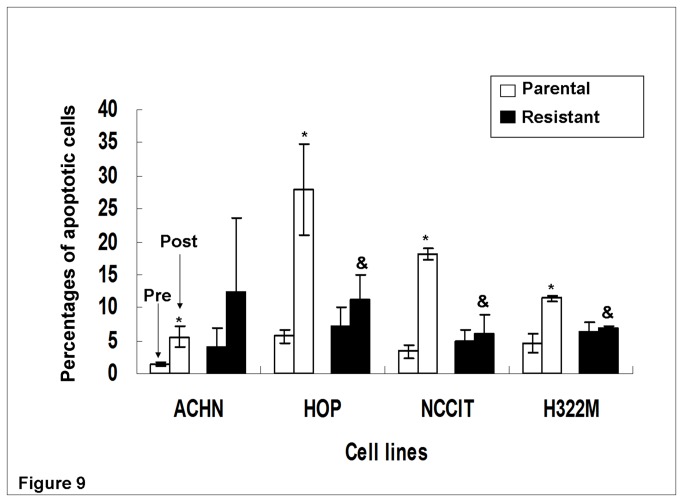
Using the same four paired sub-clones, we examined whether cells underwent apoptosis after high dose BLM treatment. After 24 hours of BLM treatment, the percentage of apoptotic cells increased in all four parental lines tested (Figure 9). In contrast, no resistant sub-clones exhibited statistically significant increases in apoptosis following BLM treatment. This was in agreement with the Comet assay (DNA damage) analysis. Moreover, three of four resistant sub-clones (HOP0.05, NCCIT1.5, and H322M2.5) exhibited significantly less increase in apoptosis (% apoptosis after minus % apoptosis before BLM treatment) compared with their parental lines following BLM treatment (p<0.05). This generally correlated with the reduced DNA damage and G2/M cell cycle arrest in BLM-resistant sub-clones (compared with parental lines, post-treatment) as observed previously.
Figure 9. Percent cell apoptosis pre- and post- high dose BLM exposure in four parental/resistant cell line pairs.
* P<0.05 for comparison between cell lines prior to and after high dose BLM treatment. All parental lines but no resistant lines exhibited significant increases in apoptosis post- BLM treatment. & P<0.05 for comparison between resistant and parental cell line following BLM treatment. Less cell apoptosis was found in three (HOP0.05, NCCIT1.5, and H322M2.5) of four BLM-resistant lines, when compared to their parental lines.
Discussion
In this study, we successfully established seven BLM-resistant human cancer cell lines from commercially available cancer cell lines of various organ origins (lung, testicle, breast, kidney, as well as the central nervous system). After sudden acute, short-term exposure to BLM, these BLM-resistant sub-clones exhibited less DNA damage, had longer doubling times, had a lower proportion of cells in G2/M arrest, and had reduced apoptosis, when compared to their more BLM-sensitive parental cell lines. BLM-resistant cell lines were developed by progressively increasing the incubating BLM concentration over an extended period of 16-24 months. Previous studies may have utilized similar methods in cultivating BLM resistant sub-clones. However, few of them reached the high level of BLM-resistance observed in this study (which was 7-49 fold increase in IC50 between resistant and parental sub-clones, when compared to a 3-20 fold increase in another study [15]). Moreover, through analysis of BLM-induced DNA damage, cell cycle distribution, and percentages of apoptosis, several putative mechanisms of BLM resistance/sensitivity were evaluated.
BLM is known to cause extended G2/M arrest and/or cell apoptosis [9] in BLM sensitive cells. This can be mediated by ATM/ATR [26,27], the upstream proteins of a DNA repair and signaling pathway that triggers G2/M arrest or cell apoptosis via a range of downstream gene products such as chk1/2, cdc 25 [28], p53, and p21WAF1/CIP1 , where the latter two are critical for sustaining G2/M cycle arrest [29]. Moreover, histone H2AX was found to be necessary for the activation of the G2/M check point [30].
Comet and γ-H2AX results revealed less BLM-induced DNA damage in the resistant lines, suggesting that the resistant sub-clones may have an enhanced ability to prevent and/or reduce DNA damage caused by BLM. This may be due to reduced cellular uptake of BLM, and/or enhanced BLM elimination/detoxification, mediated by cell surface receptors or transporters [31], antioxidant molecules/enzymes that reduce BLM-generated ROS [11,32]; or enzymes that inactivate BLM [33,34]. Future studies need to further study these mechanisms.
In this study, BLM resistance also resulted in less G2/M arrest and cell apoptosis, consistent with results from a previous study on a single BLM-resistant line [11]. The slight increase in G2/M arrest at baseline (prior to high dose BLM treatment) for these BLM resistant sub-clones could be explained by chronic exposure to BLM. The fact that BLM-resistant cells were able to proliferate at a BLM concentration that was not viable for their parental lines suggests that evasion of cell cycle blockage could be another mechanism of resistance. Taken together, our results suggest that BLM resistant cells may have acquired enhanced ability to prevent/reduce DNA damage caused by BLM. This in turn, may have led to the reduced G2/M arrest and apoptosis.
A stepwise dose escalating method for BLM resistance development may result in a dose-response relationship among BLM maintenance concentrations, IC50 values and doubling times observed in ACHN0, AHCN0.1 and AHCN0.25 cells. However, until these findings are confirmed in other sets of sub-clones, this will remain an interesting finding in need of validation.
After removing maintenance BLM concentrations from all seven resistant sub-clones, there was partial reversal of IC50 values and doubling time in three of seven cell lines. The absence of reversibility in the other four cell lines could be the result of individual cell line differences, or perhaps these cell lines needed longer breaks from BLM exposure to develop BLM sensitivity again. To our knowledge, the literature on reversing BLM-resistance in cancer cell lines has been extremely limited. This observation speaks to the potential importance of continued BLM exposure when developing resistant sub-clones. Moreover, the result suggests that reversible mechanisms such as epigenetic rather than (permanent) genetic changes may be playing a role in maintaining some of the BLM-resistance.
This study has limitations. Firstly, an in vitro model may not explain resistance in patients, but remains a critical first step in studying BLM resistance mechanism. Secondly, the amount of BLM treatment for each cell line corresponded to ten times the maintenance concentration for each BLM resistant sub-clone. There is the possibility that the treatment is not “acute” or high enough to elicit significant cellular response following the treatment. However, significant responses were seen in parental cells. Thirdly, individual cell line differences were not well-accounted, given the range of cell line origins. Since each cell line may have unique mechanisms that contribute to BLM resistance, this may explain some of the variations observed across experiments in this study. Fourthly, the cells used were not monoclonal. This may result in cells behaving differently upon BLM treatment. Yet, given that it was technically difficult to repopulate cells from a single cell that survived the dose escalation, we adopted this conventional approach of resistance development.
In summary, this study described some of the relationships between BLM resistance, BLM-induced DNA damage, cell growth rate, cell cycle distribution, and apoptosis. The reduced DNA damage, reduced G2/M arrest, and reduced apoptosis observed in BLM-resistant sub-clones following high dose BLM exposure suggest that acquired BLM resistance involves effective DNA damage reduction and G2/M cell cycle evasion. The seemingly reversible resistance observed in at least some of the BLM resistant sub-clones suggests that some of the BLM- resistance in our cell lines models may have utilized non-permanent mechanisms such as epigenetic changes to cope with chronic BLM exposure. Our results provide the foundation for future research in biomarkers of BLM resistance, which may ultimately lead to an improved rationale for personalized chemotherapy selection.
Acknowledgments
We thank the laboratories of M. Tsao, F.F. Liu, and A.D. Schimmer for providing suggestions on cell culturing techniques and automatic cell counting equipments.
Funding Statement
This study was supported by the Princess Margaret Hospital Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Umezawa H (1965) Bleomycin and other antitumor antibiotics of high molecular weight. Antimicrob Agents Chemother (Bethesda) 5: 1079–1085. PubMed: 5883403. [PubMed] [Google Scholar]
- 2. Umezawa H, Maeda K, Takeuchi T, Okami Y (1996) New anti-biotics, bleomycin A and B. J Antibiot 19: 200–209. [PubMed] [Google Scholar]
- 3. Lazo JS (1999) Bleomycin. Cancer Chemother Biol Response Modif 18: 39-45. PubMed: 10800476. [PubMed] [Google Scholar]
- 4. Chen J, Stubbe J (2005) Bleomycins: towards better therapeutics. Nat Rev Cancer 5 (2): 102-112. doi: 10.1038/nrc1547. PubMed: 15685195. [DOI] [PubMed] [Google Scholar]
- 5. Yen HC, Chang HM, Majima HJ, Chen FY, Li SH (2005) Levels of reactive oxygen species and primary antioxidant enzymes in WI38 versus transformed WI38 cells following bleomcyin treatment. Free Radic Biol Med 38: 950-959. doi: 10.1016/j.freeradbiomed.2004.12.022. PubMed: 15749391. [DOI] [PubMed] [Google Scholar]
- 6. Povirk LF (1996) DNA damage and mutagenesis by radiomimetic DNA-cleaving agents: bleomycin, neocarzinostatin and other enediynes. Mutat Res 355: 71-89. doi: 10.1016/0027-5107(96)00023-1. PubMed: 8781578. [DOI] [PubMed] [Google Scholar]
- 7. Chen J, Ghorai MK, Kenney G, Stubbe J (2008) Mechanistic studies on bleomycin-mediated DNA damage: multiple binding modes can result in double-stranded DNA cleavage. Nucleic Acids Res 36: 3781-3790. doi: 10.1093/nar/gkn302. PubMed: 18492718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khaidakov M, Manjanatha MG, Aidoo A (2002) Molecular analysis of mitochondrial DNA mutations from bleomycin-treated rats. Mutat Res 500: 1-8. doi: 10.1016/S0027-5107(01)00270-6. PubMed: 11890929. [DOI] [PubMed] [Google Scholar]
- 9. Cloos J, Temmink O, Ceelen M, Snel MH, Leemans CR et al. (2002) Involvement of cell cycle control in bleomycin-induced mutagen sensitivity. Environ Mol Mutagen 40(2): 79-84. doi: 10.1002/em.10093. PubMed: 12203399. [DOI] [PubMed] [Google Scholar]
- 10. Kaneko M, Matsuda D, Ohtawa M (2012) Potentiation of bleomycin in jurkat cells by fungal pycnidione. Biol Pharm Bull 35(1): 18-28. doi: 10.1248/bpb.35.18. PubMed: 22223332. [DOI] [PubMed] [Google Scholar]
- 11. Yen HC, Li SH, Majima HJ (2011) Up-regulation of antioxidant enzymes and coenzyme Q (10) in a human oral cancer cell line with acquired bleomycin resistance. Free Radic Res 45 (6): 707-716. doi: 10.3109/10715762.2011.572969. PubMed: 21486114. [DOI] [PubMed] [Google Scholar]
- 12. Hagimori K, Fukuda T, Hasegawa Y, Omura S, Tomoda H (2007) Fungal malformins inhibit bleomycin-induced G2 checkpoint in Jurkat cells. Biol Pharm Bull 30: 1379-1383. doi: 10.1248/bpb.30.1379. PubMed: 17666789. [DOI] [PubMed] [Google Scholar]
- 13. Kuntz K, O’Connell MJ (2009) The G2 DNA damage checkpoint: Could this ancient regulator be the Achilles heel of cancer? Cancer Biol Ther 8(15): 1433-1439. doi: 10.4161/cbt.8.15.9081. PubMed: 19574738. [DOI] [PubMed] [Google Scholar]
- 14. Bokemeyer C (2008) Bleomycin in testicular cancer: will pharmacogenomics improve treatment regimens? J Clin_Oncol 26(11): 1817-1823. doi: 10.1200/JCO.2007.14.1606. PubMed: 18398143. [DOI] [PubMed] [Google Scholar]
- 15. Pron G, Belehradek J Jr, Orlowski S, Mir LM (1994) Involvement of membrane bleomycin-binding sites in bleomycin cytotoxicity. Biochem Pharmacol 48 (2): 3001-3010. PubMed: 7519854. [DOI] [PubMed] [Google Scholar]
- 16. Pron G, Mahrour N, Orlowski S (1999) Internalisation of the bleomycin molecules responsible for bleomycin toxicity: a receptor-mediated endocytosis mechanism. Biochem Pharmacol 57(1): 45-56. doi: 10.1016/S0006-2952(98)00282-2. PubMed: 9920284. [DOI] [PubMed] [Google Scholar]
- 17. Tuimala J, Szekely G, Gundy S, Hirvonen A, Norppa H (2002) Genetic polymorphisms of DNA repair and xenobiotic-metabolizing enzymes: role in mutagen sensitivity. Carcinogenesis 23(6): 1003-1008. doi: 10.1093/carcin/23.6.1003. PubMed: 12082022. [DOI] [PubMed] [Google Scholar]
- 18. Robertson KA, Bullock HA, Xu Y (2001) Altered expression of Ape1/ref-1 in germ cell tumors and overexpression in NT2 cells confers resistance to bleomycin and radiation. Cancer Res 61(5): 2220-2225. PubMed: 11280790. [PubMed] [Google Scholar]
- 19. Liu S, Lai Y, Zhao W, Wu M, Zhang Z (2011) Links between DNA polymerase beta expression and sensitivity to bleomycin. Toxicology 281(1-3): 63-69. doi: 10.1016/j.tox.2011.01.008. PubMed: 21251944. [DOI] [PubMed] [Google Scholar]
- 20. Genomics and Bioinformatics Group, LMP, CCR, National Cancer Institute. CellMinerTM (2012) Available online at: http://discover.nci.nih.gov/cellminer/drugHtmlPage.do
- 21. Uphoff CC, Drexler HG (2011) Detecting mycoplasma contamination in cell cultures by polymerase chain reaction. Methods Mol Biol 731: 93-103. doi: 10.1007/978-1-61779-080-5_8. PubMed: 21516400. [DOI] [PubMed] [Google Scholar]
- 22. Lorenzi PL, Reinhold WC, Varma S (2009) DNA fingerprinting of the NCI-60 cell line panel. Mol Cancer Ther 8(4): 713-724. doi: 10.1158/1535-7163.MCT-08-0921. PubMed: 19372543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tice RR, Agurell E, Anderson D (2000) Single cell gel/comet assay: guidelines for in vitro and in vivo genetic toxicology testing. Environ Mol Mutagen 35(3): 206-221. doi: 10.1002/(SICI)1098-2280(2000)35:3. PubMed: 10737956. [DOI] [PubMed] [Google Scholar]
- 24. Ivashkevich A, Redon CE, Nakamura AJ, Martin RF, Martin OA (2012) Use of the γ-H2AX assay to monitor DNA damage and repair in translational cancer research. Cancer Lett 327(1-2): 123-133. doi: 10.1016/j.canlet.2011.12.025. PubMed: 22198208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muslimovic A, Ismail IH, Gao Y, Hammarsten O (2008) An optimized method for measurement of gamma-H2AX in blood mononuclear and cultured cells. Nat Protoc 3(7): 1187-1193. doi: 10.1038/nprot.2008.93. PubMed: 18600224. [DOI] [PubMed] [Google Scholar]
- 26. Nakayama Y, Igarashi A, Kikuchi I, Obata Y, Fukumoto Y et al. (2009) Bleomycin-induced over-replication involves sustained inhibition of mitotic entry through the ATM/ATR pathway. Exp Cell Res 315(15): 2515-2528. doi: 10.1016/j.yexcr.2009.06.007. PubMed: 19527713. [DOI] [PubMed] [Google Scholar]
- 27. Sun Y, Jiang X, Chen S, Fernandes N, Price BD (2005) A role for the Tip60 histone acetyltransferase in the acetylation and activation of ATM. Proc Natl Acad Sci U S A 102(37): 13182-13187. doi: 10.1073/pnas.0504211102. PubMed: 16141325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bartek J, Lukas J (2003) Chk1 and Chk2 kinases in checkpoint control and cancer. Cancer Cell 3(5): 421–429. doi: 10.1016/S1535-6108(03)00110-7. PubMed: 12781359. [DOI] [PubMed] [Google Scholar]
- 29. Bunz F, Dutriaux A, Lengauer C (1998) Requirement for p53 and p21 to sustain G2 arrest after DNA damage. Science 282(5393): 1497-1501. doi: 10.1126/science.282.5393.1497. PubMed: 9822382. [DOI] [PubMed] [Google Scholar]
- 30. Fernandez-Capetillo O, Chen HT, Celeste A, Ward I, Romanienko PJ et al. (2002) DNA damage-induced G2-M checkpoint activation by histone H2AX and 53BP1. Nat Cell Biol 4(12): 993-997. doi: 10.1038/ncb884. PubMed: 12447390. [DOI] [PubMed] [Google Scholar]
- 31. Aouida M, Poulin R, Ramotar D (2010) The human carnitin transporter SLC22A16 mediates high affinity uptake of the anticancer polyamine analoguebleomycin-A5. J Biol Chem 285: 6275-6284. doi: 10.1074/jbc.M109.046151. PubMed: 20037140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cort A, Timur M, Dursun E, Kucuksayan E, Aslan M et al. (2012) Effects of N-acetylcystein on bleomycin-induced apoptosis in malignant testicular germ cell tumors. J Physiol Biochem 68(4): 555-562. doi: 10.1007/s13105-012-0173-z. PubMed: 22562160. [DOI] [PubMed] [Google Scholar]
- 33. Schwartz DR, Homanics GE, Hoyt DG, Klein E, Abernethy J et al. (1999) The neutral cysteine protease bleomycin hydrolase is essential for epidermal integrity and bleomycin resistance. Proc Natl Acad Sci U S A 96(8): 4680-4685. doi: 10.1073/pnas.96.8.4680. PubMed: 10200322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen J, Chen Y, He Q (2012) Action of bleomycin is affected by bleomycin hydrolase but not by caveolin-1. Int J Oncol 41(6): 2245-2252. PubMed: 23076812. [DOI] [PubMed] [Google Scholar]